Abstract
Background
No studies investigating the effect of midfoot (talonavicular joint) position on clinical outcomes following flatfoot reconstruction have been performed. The purpose of our study was to determine whether a postoperative abducted or adducted forefoot alignment, as determined from AP radiographs, was associated with a difference in outcomes using the Foot and Ankle Outcome Score (FAOS).
Methods
Midfoot abduction was defined on postoperative AP radiographs, evaluated at a mean of 1.9 years in 55 patients from the authors’ institution that underwent flatfoot reconstruction for stage II adult acquired flatfoot deformity (AAFD), as a lateral incongruency angle greater than 5 degrees, a talonavicular uncoverage angle greater than 8 degrees, and a talo-first metatarsal angle greater than 8 degrees based on previously reported measurements. Patients with two or more measurements in the abduction category were classified as the abduction group (n=30); those with one or fewer measurements in the abduction category were placed in the adduction group (n=25). Preoperative FAOS and postoperative FAOS with a mean follow-up of 3.1 years were compared using Wilcoxon rank-sum tests.
Results
Patients corrected to a position of adduction showed a significantly lower improvement in the FAOS daily activities (p=0.012) and quality of life subscales (p=0.046). Mean improvement in subscale score for the adducted group was lower for pain (p=0.052) and sports activities (p=0.085) but did not reach statistical significance. No significant difference in the FAOS symptoms subscale (p=0.372) between groups was found.
Conclusions
Correction of the talonavicular joint to a position of adduction following stage II AAFD is associated with decreased patient outcomes in daily activities and quality of life compared with an abducted position. These results suggest that overcorrection to a position of midfoot adduction leads to a lesser amount of individual patient improvement in the reconstruction of stage II AAFD.
Level of Evidence
Therapeutic Level III
Keywords: Adult acquired flatfoot deformity, Reconstruction, Midfoot abduction, Clinical outcomes, Talonavicular joint
INTRODUCTION
Adult acquired flatfoot deformity (AAFD) results from dysfunction of the tibialis posterior tendon with gradual insufficiency of the ligaments that support the medial longitudinal arch of the foot4. In addition to collapse of the medial arch, stage II AAFD is characterized by numerous passively correctible deformities including forefoot abduction through the talonavicular joint and hindfoot valgus4,12. Although there is significant debate over the proper operative treatment of stage II AAFD, reconstructions commonly comprise of a number of bony and soft tissue procedures such as the medializing calcaneal osteotomy (MCO), lateral column lengthening (LCL), Cotton osteotomy, first tarsometatarsal fusion, and less commonly spring ligament reconstruction; these procedures may be performed separately or in combination4.
The severity of the abduction deformity varies widely between patients in stage II AAFD4. As a consequence, some patients require minimal operative correction of the AP talonavicular deformity while those with a greater amount of talonavicular uncoverage may be treated with an LCL4. LCL corrects the forefoot abduction deformity and decreases talonavicular uncoverage7,13,16. However, correction of the preoperative abduction deformity with an LCL has been associated with increased lateral plantar pressures, stress fractures of the fifth metatarsal, and postoperative rigidity of the foot2,3,5,18.
In current practice, the amount of LCL to be performed intraoperatively is determined based on clinical and radiographic assessment, and the use of trial wedges has been shown to reduce postoperative stiffness and pain 5. Adequate correction reduces talonavicular uncoverage while not leading to excessive stiffness of the lateral aspect of the forefoot4. Oh et al. (2013) demonstrated that small increments in LCL can lead to substantial changes in talonavicular abduction and lateral plantar pressures15. The surgeon must therefore carefully select the amount of lengthening of the lateral column to prevent complications.
In regards to postoperative clinical outcomes, there have been no studies in the literature that identify an appropriate radiographic midfoot (talonavicular) alignment for stage II AAFD patients following reconstruction. The goal of our work was to quantify an optimal postoperative radiographic midfoot position following reconstruction of the stage II AAFD. In particular, we wanted to determine whether a mild postoperative abducted or a mild adducted forefoot alignment, as determined from AP radiographs, was associated with a difference in outcomes using the Foot and Ankle Outcome Score (FAOS), previously validated for AAFD11. Our hypothesis was that stage II AAFD patients corrected to a mild abducted midfoot position would have the best outcomes.
MATERIALS AND METHODS
This retrospective study identified all patients who underwent a flatfoot reconstruction for stage II AAFD between January, 2008 and March, 2011. Two surgeons fellowship-trained in foot and ankle surgery performed all reconstructions. Data, including demographic information, postoperative anteroposterior (AP) radiographs, preoperative FAOS, and postoperative FAOS, was collected from an Institutional Review Board-approved foot and ankle registry. The protocol was approved by the registry’s steering committee. The use of a medializing calcaneal osteotomy (MCO), lateral column lengthening (LCL), first tarsometatarsal fusion (TMT fusion), Cotton osteotomy, and spring ligament reconstruction as part of a flatfoot reconstruction was determined using operative notes.
Inclusion and Exclusion Criteria
Patients were eligible to be included in this study if they had (1) a diagnosis of stage II AAFD at the time of flatfoot reconstruction, (2) an MCO performed as part of the flatfoot reconstruction, (3) an FAOS preoperatively and greater than 22 months postoperatively, and (4) AP radiographs taken at least 45 weeks postoperatively. Patients who had (1) a contralateral flatfoot reconstruction and/or (2) talonavicular, calcaneocuboid, or subtalar fusions were excluded from the study as they were possible confounders. Sixty patients initially met all inclusion criteria. One patient was excluded due to a subsequent contralateral triple arthrodesis, and four patients were excluded due to subsequent contralateral flatfoot reconstructions. This left 55 patients who met all inclusion and exclusion criteria.
Clinical Outcome Evaluation
Clinical outcomes were evaluated using the Foot and Ankle Outcome Score (FAOS), which has been validated for AAFD11. The FAOS is a self-administered questionnaire that is specific for foot and ankle pathology. It consists of 42 questions divided into five separate subscales including pain, symptoms, quality of life, daily activities, and sports activities. Patients evaluate the magnitude of their symptoms as none, mild, moderate, severe, or extreme. They similarly choose the frequency of their symptoms from the options: (1) never, rarely, sometimes, often, or always or (2) never, monthly, weekly, daily, or always. Each subscale is independently scored from 0 to 100 with 100 representing the best clinical outcomes. However, because patients are not required to answer every question in the questionnaire if they feel a question is not applicable, the number of subjects for each subscale may vary (Table 1). The reason we chose to look at the change in FAOS subscale rather than postoperative subscale value alone was to avoid variability between patients so that patients could act as their own control (i.e. to control for within-subject variability). If multiple preoperative FAOS questionnaires were available, the FAOS closest to the time of surgery was used. In order to ensure adequate follow-up time, the most recent postoperative FAOS questionnaire at least 22 months after the patient’s flatfoot reconstruction was selected from the registry.
Table 1.
Number of patients by postoperative midfoot position group who answered a sufficient number of questions in each FAOS subscale. Patients are not required to respond to all of the questions in the FAOS survey, and consequently, some patients may not have a score in every subscale.
| Midfoot Position Group | Total no. (patients) | Pain no. | Symptoms no. | Daily Activities no. | Sports Activities no. | Quality of Life no. |
|---|---|---|---|---|---|---|
| Abduction | 30 | 28 (93.3%) | 29 (96.7%) | 27 (90.0%) | 21 (70.0%) | 30 (100.0%) |
| Adduction | 25 | 23 (92.0%) | 24 (96%) | 25 (100.0%) | 17 (68.0%) | 25 (100.0%) |
Radiographic Evaluation
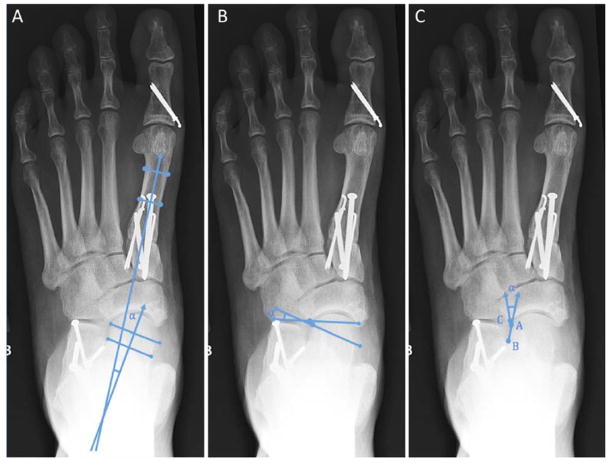
Postoperative AP radiographs were collected from the registry database. All radiographs were taken at least 45 weeks postoperatively. There is evidence in the literature to suggest that radiographic measurements of deformity do not change after 3 months14, but our measurements were taken at nearly 1 year or more after surgery. AP radiographs were taken in a standardized fashion in which patients stood with their weight equally distributed between both feet, the feet shoulder-width apart, and the arch relaxed. The x-ray beam was directed 15 degrees posteriorly towards the heel and was moved 37 inches from the digital cassette. For each patient, lateral incongruency angle, talonavicular uncoverage (TUC) angle, and first talo-first metatarsal (1TMT) angle on AP radiographs were measured to assess postoperative midfoot alignment. The AP 1TMT angle was reported as positive in patients whose first metatarsal axis was abducted compared to the axis of the talus (Figure 1a). The TUC angle was considered positive when the line connecting the edges of the navicular articular surface intersected the line connecting the edges of the talar head articular surface lateral to the talonavicular joint (Figure 1b). Lateral incongruency angle was measured as described previously by Ellis et al. (2009) (Figure 1c) 6. The incongruency angle is determined from the intersection of a line beginning at the lateral most aspect of the talar articular surface (Point A) and extending to the most lateral extent of the navicular articular surface (Point C) with a line drawn from the lateral most aspect of the narrowest part of the talar neck (Point B) to Point A 6. The incongruency angle was positive when the most lateral aspect of the navicular articular surface (Point C) was located laterally to the most lateral aspect of the talar articular surface (Point A).
Figure 1.
- 1TMT angle
- TUC angle
- Incongruency angle
Patients were then divided into either the midfoot abduction or adduction group based on a combination of their lateral incongruency angle, TUC angle, and 1TMT angle on AP radiographs. Abduction was defined as a lateral incongruency angle greater than 5 degrees, a TUC angle greater than 8 degrees, and a 1TMT angle greater than 8 degrees based on previously reported measurements6,10. Because no one angle has been shown to provide the best assessment of abduction versus adduction, patients with two or more measurements in the abduction category were classified as the abduction group; those with one or fewer measurements in the abduction category were placed in the adduction group.
A three-group secondary analysis was performed to provide additional information about talonavicular position. For this analysis, patients were divided into three groups based on postoperative talonavicular position. The normal group was specified as a talonavicular within 10 degrees of the average measurement for a foot with no pathology. Thus, the normal group was defined as a lateral incongruency angle greater than or equal to −5 degrees and less than or equal to 15 degrees, a TUC angle greater than or equal to −2 degrees and less than or equal to 18 degrees, and a 1TMT angle greater than or equal to −2 degrees and less than or equal to 18 degrees based on previously reported measurements6,10. Similarly, the mildy abducted group was defined as a lateral incongruency angle greater than 15 degrees, a TUC angle greater than 18 degrees, and a 1TMT angle greater than 18 degrees based on previously reported measurements6,10. All other angles were considered mildly adducted. Patients with 2 or more angles in one group were placed into that group. Patients with 1 angle in each of the three groups were placed into the normal group.
Operative Technique
All flatfoot reconstructions were performed by two surgeons fellowship-trained in foot and ankle surgery at the investigators’ institution. Patients underwent either an MCO alone (n=16) or a combination of MCO with an LCL (n=39). The MCO was accomplished via an incision on the lateral aspect of the heel followed by a transverse cut of the calcaneus. 4.5, 6.5, or 7.3 cannulated screws were used to secure the osteotomy. If an LCL was performed, the site was accessed through a lateral incision over the anterior calcaneus, and the surgeon utilized either a Griend (step-cut)- or Evans-type osteotomy technique7,8. The osteotomy site was packed with autograft and bone marrow aspirate from the iliac crest and anchored with two fully threaded, cortical screws or a claw plate.
As part of a flatfoot reconstruction, some patients also underwent a Cotton osteotomy (n=24), first tarsometatarsal (1TMT) fusion (n=28), and spring ligament reconstruction (n=5) depending on their deformity (Table 2). The surgeons utilized a dorsal approach to access the Cotton osteotomy site, filled the osteotomy site with autogenous or allograft bone, and then fixed it with a small plate and screws. A modified Lapidus technique in which the joint surfaces are prepared and then fixed with a combination of fully threaded, cortical cross screws was used to complete the 1TMT fusion. Spring ligament reconstructions employed allograft tendons placed through drill holes in the navicular, tibia, and/or calcaneus and secured to 3.5 mm screw posts in the dorsal navicular and lateral fibular bones. The attending surgeons determined the amount of MCO, LCL, and Cotton osteotomy intraoperatively in order to provide the appropriate correction of the underlying deformity. Postoperatively, all patients were placed in a cast or removable boot and were nonweightbearing for 6 to 8 weeks before progressing to full weightbearing by 10 to 12 weeks.
Table 2.
Patient demographics and number of patients undergoing different procedures by postoperative midfoot position group.
| Midfoot Position Group | Total no. (patients) | BMI | Age | Male / Female | LCL | 1 TMT Fusion | Cotton Osteotomy | Spring Ligament Reconstruction |
|---|---|---|---|---|---|---|---|---|
| Abduction | 30 | 28.3 | 60.9 | 12 / 18 (40.0% / 60.0%) | 19 (63.3%) | 17 (56.7%) | 11 (36.7%) | 3 (12.0%) |
| Adduction | 25 | 28.0 | 62.4 | 8 / 17 (32.0% / 68.0%) | 20 (80.0%) | 11 (44.0%) | 13 (52.0%) | 2 (8.0%) |
Statistical Analysis
Wilcoxon rank-sum tests were used to compare the change in FAOS subscales between patients in postoperative adduction (n=25) and abduction (n=30). This method allowed us to identify significant differences in the mean change in FAOS subscales between the two midfoot groups. Wilcoxon rank-sum tests were also utilized to determine if there were any significant differences in the mean amount of LCL performed or average postoperative hindfoot moment arm between patients in the two groups though this data was not available for all patients. Seventeen postoperatively abducted patients and 16 postoperatively adducted patients had the amount of LCL performed recorded. All patients had the amount of MCO performed in their operative note.
For the secondary analysis of the three groups based on talonavicular position, comparisons of FAOS subscale scores between the normal (n=29), mildly abducted (n=17), and mildly adducted (n=9) groups were evaluated using the Kruskal-Wallis test (K-W test). Post-hoc pairwise comparisons were performed for subscales identified by the K-W test as having differences between groups using analysis of variance (ANOVA) on the rank-transformed data with adjustment for multiple comparisons using Tukey’s method. This method enabled the identification of postoperative talonavicular groups that differed significantly from another group in average change in a FAOS subscale.
Additionally, a sub-analysis was performed in order to further investigate the effect of LCL on clinical outcomes. Patients were first divided into groups based on whether or not they had undergone a LCL as part of their flatfoot reconstruction. Wilcoxon rank-sum tests were used to compare abducted and adducted patients who had a LCL performed as well as to compare abducted and adducted patients who did not have a LCL.
In order to determine if the proportions of patients who underwent a concomitant procedure including LCL, 1TMT fusion, spring ligament reconstruction, or Cotton osteotomy in each midfoot group were different, Fisher’s exact tests were used. This statistical analysis was also utilized to determine if there were any differences between the proportion of patients who were preoperatively classified as adducted or abducted using the radiographic parameters discussed previously. Preoperative AP radiographs were available for all patients except for one patient postoperatively categorized as abducted.
RESULTS
Fifty-five feet (26 right, 29 left) in 55 patients met the inclusion and exclusion criteria. The cohort consisted of 20 men and 35 women with a mean age of 61.6 (range, 42 to 84) years and a mean BMI of 28.1 (range, 18.5 to 40.7). There were no statistically significant differences between BMI, gender, or age between the midfoot groups (Table 2). Postoperative AP radiographs were taken at an average of 1.9 (range, 0.9 to 3.8) years, and FAOS scores were obtained after an average of 3.1 (range, 1.8 to 4.4) years postoperatively.
For all patients with preoperative AP radiographs (n=54), the mean lateral incongruency angle was 19.5 (range, −92.6 to 147.6) degrees, the mean TUC angle was 28.6 (range, 1.6 to 69.6) degrees, and the mean 1TMT angle was 14.0 (range, −24 to 36.4) degrees (Table 3). Postoperatively, patients corrected to a position of abduction had a mean lateral incongruency angle of 18.2 (range, 7.1 to 159.3) degrees, TUC angle of 23.5 (range, 8.1 to 57.5) degrees, and 1TMT angle of 13.9 (range, −8.1 to 30.3) degrees. Patients with a postoperative adducted forefoot position had a mean lateral incongruency angle of −7.2 (range, −50.8 to 34.2) degrees, TUC angle of 5.8 (range, −11.9 to 22.5) degrees, and 1TMT angle of 0.7 (range, −10.4 to 21.2) degrees.
Table 3.
Preoperative and postoperative radiographic measurements.
| Midfoot Position Group | 1TMT Angle | Incongruency Angle | TUC Angle |
|---|---|---|---|
| Preoperative (n=54) | 14.0° ± 12.3° (range, −24° to 36.4°) | 19.5° ± 55.5° (range, −92.6° to 147.6°) | 28.6° ± 11.8° (range, 1.6° to 69.6°) |
| Postop Abduction (n=30) | 13.9° ± 9.7° (range, −8.1° to 30.3°) | 18.2° ± 40.1° (range, 7.1° to 159.3°) | 23.5° ± 10.3° (range, 8.1° to 57.5°) |
| Postop Adduction (n=25) | 0.7° ± 7.6° (range, −10.4° to 21.2°) | −7.2° ± 23.0° (range, −50.8° to 34.2°) | 5.8° ± 7.8° (range, −11.9° to 22.5°) |
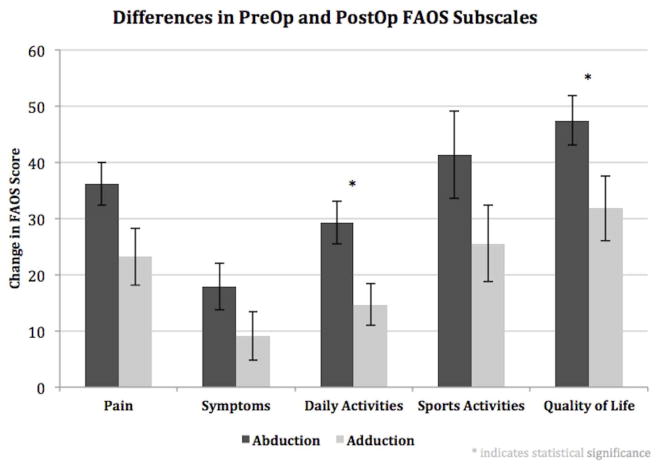
Thirty patients were corrected to a midfoot position of abduction, and twenty-five patients were corrected to a midfoot position of adduction. Of the patients who had preoperative radiographs (n=54), twenty-seven patients in the postoperative abduction group (n=29) were preoperatively classified as abduction, and eighteen patients in the postoperative adduction group (n=25) were preoperatively classified as abduction. Means and ranges for changes in all FAOS subscales in both the abducted and adducted groups are shown in Table 4. Patients corrected to a position of adduction showed a significantly lower improvement in the FAOS daily activities (p=0.012) and quality of life subscales (p=0.046) (Figure 2). For patients in postoperative abduction, the mean change from preoperative to postoperative in the daily activities subscale was 29.2, whereas for patients in postoperative adduction, the mean change in the FAOS daily activities subscale was 14.7. The mean change in the quality of life subscale was 47.4 for patients in the abducted group versus 31.8 for patients in the adducted group. Mean change in subscale score for the adducted group was lower for pain (p=0.052) and sports activities (p=0.085) but did not reach statistical significance. No significant difference in the FAOS symptoms subscale (p=0.372) between groups was found. There was no difference in the mean postoperative FAOS scores between the two groups in any of the subscales. There was no significant difference in the mean postoperative hindfoot moment arm based on forefoot position (p=0.114).
Table 4.
Means and ranges for preoperative to postoperative changes in FAOS subscales between the abducted and adducted groups. Patients corrected to a position of adduction showed statistically significantly lower improvement in patient outcomes in the daily activities and quality of life subscales.
| Midfoot Position Group | Pain | Symptoms | Daily Activities | Sports Activities | Quality of Life |
|---|---|---|---|---|---|
| Abduction | 36.2 (range, −13.9 to 66.7) | 17.9 (range, −28.6 to 78.6) | 29.2 (range, −5.9 to 64.7) | 41.3 (range, −35.0 to 90.0) | 47.4 (range, 0.0 to 100.0) |
| Adduction | 23.2 (range, −58.3 to 63.9) | 9.1 (range, −40.7 to 46.4) | 14.7 (range, −47.1 to 44.1) | 25.6 (range, −25 to 70) | 31.8 (range, −18.8 to 87.5) |
Figure 2.
Differences in preoperative and postoperative FAOS subscales. Patients corrected to a position of adduction showed a significantly lower improvement in the FAOS daily activities and quality of life subscales than patients corrected to a position of abduction.
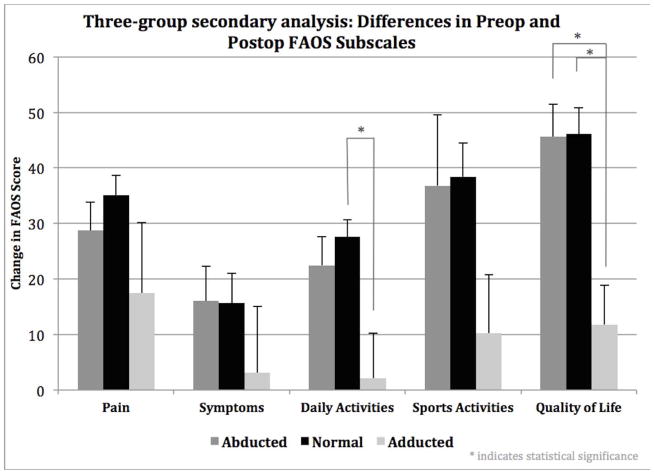
For the three-group secondary consisting of the normal, mildly abducted, and mildly adducted groups, statistically significant differences were found in the daily activities (K-W test p=0.025) and quality of life (K-W test p=0.004) FAOS subscales. The mild adduction group performed significantly worse in the daily activities FAOS subscale than the normal group (p=0.016) and significantly worse in the quality of life FAOS subscale than both the mildly abducted groups (p=0.005) and normal (p=0.003) groups (Figure 3). The average change in FAOS score for the daily activities subscale for the mildly adducted group was 2.1 compared with 22.5 and 27.6 for the mildly abducted and normal groups, respectively. Similarly, the average change in FAOS score for the quality of life subscale for the mildly adducted was 11.8 compared with 45.6 and 46.1 for the mildly abducted and normal groups, respectively. Although the mildly adducted group had a lower change in FAOS score compared to both the mildly abducted and normal groups in pain, symptoms, and sports activities, these were not statistically significant. There were no statistically significant differences between the normal and mildly abducted groups.
Figure 3.
Three-group secondary analysis. Change in FAOS subscales were compared between mildly abducted, normal and mildly adducted patients. Patients in the mildly adducted group performed significantly worse in the daily activites subscale than patients to corrected to a normal position (p=0.016) and in the quality of life subscale than both the normal (p=0.003) and mildly abducted group (p=0.005).
Comparison between abducted (n=19) and adducted (n=20) patients who had undergone both a LCL and MCO showed similar results to the combined MCO + LCL and MCO group described just above. A statistically significant smaller improvement was seen in the daily activities subscale for adducted patients who had a LCL performed compared to abducted patients who had a LCL performed (p=0.011). Additionally, for patients who had a LCL, the mean change in FAOS subscale scores for the adducted patients was lower in pain (p=0.059), symptoms (p=0.273), sports activities (p=0.145), and quality of life (p=0.180) compared to abducted patients but these did not reach statistical significance. No statistical significance was found between abducted (n=11) and adducted (n=5) patients who did not have a LCL in any of the FAOS subscales (all p-values > 0.25), but the sample size was small. Patients moved to a position of midfoot adduction postoperatively without a LCL as part of their flatfoot reconstruction, in general, had a lower average change (but not statistically significant) than abducted patients who did not undergo a LCL procedure in each of the FAOS subscales, with the exception of the symptoms subscale in which the difference between the two groups was 0.7 points.
The proportions of patients undergoing an LCL, 1TMT fusion, Cotton osteotomy, and spring ligament reconstruction did not differ significantly between the two groups. Similarly, there were no differences in the mean amount of LCL performed or postoperative hindfoot moment arm between the postoperative midfoot groups. The groups also did not significantly differ in the proportion of patients who were preoperatively classified as either abducted or adducted.
DISCUSSION
To the authors’ knowledge, this is the first study to examine the relationship between postoperative midfoot alignment and clinical outcomes. Our study indicates that correction of the talonavicular joint to a position of adduction (Figure 4a) following stage II AAFD surgery is associated with significantly reduced improvements of patient outcomes in daily activities and quality of life compared with correction to a forefoot abducted position (Figure 4b). This is supported by data from the three-group secondary analysis, which showed that patients corrected to a postoperative position of mild adduction performed significantly worse than the normal group in the daily activities subscale and significantly worse than both the normal and mildly abducted group in the quality of life subscale.
Figure 4.
- Postoperative radiograph of a patient in adduction
- Postoperative radiograph of a patient in abduction
The daily activities and quality of life FAOS subscales are particularly relevant for evaluating midfoot position as procedures such as LCL are used to achieve adequate correction without resorting to a subtalar or talonavicular fusion. Patients in the postoperative adducted group also had less improvement in the pain, symptoms, and quality of life subscales, although these were not statistically significant. These results suggest that overcorrecting the talonavicular joint into adduction reduces the amount of improvement in postoperative patient outcomes. There was no difference in the mean postoperative FAOS score between the adduction and abduction groups in any of the subscales. However, because the change in outcome score takes into account individual differences in preoperative function (assessing improvement for the individual), we believe that the difference in improvement in FAOS subscales between is noteworthy.
In 1975, Evans first described the use of an LCL to correct deformity in calcaneo-valgus feet, which included patients with tibialis posterior insufficiency7. Since then, the literature has supported the use of an LCL in order to reduce talonavicular uncoverage associated with stage II AAFD1,4,9,17,19. A recent biomechanical mechanical study by Zanoli et al. (2014) demonstrated that flatfoot reconstructions incorporating an LCL provided substantial sagittal and midfoot deformity correction20.
However, LCLs also cause a significant shift of plantar load to the lateral column2,15,17. Davitt et al. (2001) showed that LCLs led to decreased contact in the medial midfoot through increased talonavicular coverage in addition to higher maximum mean plantar pressures along the lateral midfoot in eleven pediatric patients2. Davitt and Morgan also reported two cases of stress fractures of the fifth metatarsal following Evans’ calcaneal lengthening procedure3. Oh et al. (2013) demonstrated the effects of different amounts of LCL on lateral plantar pressures of the foot15. They found significantly decreased talonavicular uncoverage and increased lateral column plantar pressures as they increased the amount of LCL performed from 6 mm to 10 mm15. These studies suggest that overcorrection of the abduction deformity in patients with stage II AAFD may lead to inferior clinical outcomes.
Neither additional procedures nor the amount of LCL performed were found to significantly affect patient outcomes. All patients had an MCO and similar proportions of patients in each group had a 1TMT fusion, Cotton osteotomy, and spring ligament reconstruction. Thus, differences in the procedures performed did not account for the differences in patient outcomes between the two midfoot position groups. The amount of LCL performed in the abducted and adducted groups was not significantly different, which indicates that the results of this study do not depend on how much the midfoot position was changed but rather on the final postoperative radiographic alignment. The hindfoot moment arm was not statistically different between the adducted and abducted groups. We were therefore able to isolate the postoperative midfoot radiographic alignment and correlate that with clinical outcomes.
A recent study described the differences in radiographic alignment between 75 patients with flatfoot deformity (85 feet) and 57 patients with no deformity (70 feet) 10. On preoperative AP radiographs, Kang et al. (2013) reported that patients with AAFD had a mean TUC angle of 26.2 degrees and a mean 1TMT angle of 20.0 degrees 10. Patients with no deformity had a mean TUC angle of 8.2 degrees and a mean 1TMT angle of 7.7 degrees 10. Ellis et al. (2009) found that patients with stage IIb AAFD (n=30) had a mean preoperative lateral incongruency angle of 70.4 degrees while patients with no deformity had a mean lateral incongruency angle of 6.4 degrees 6.
The mean postoperative AP radiograph angles in both groups were more adducted those reported in preoperative patients with AAFD by Ellis et al. (2009) and Kang et al. (2012). Patients in the adducted group in our study had mean postoperative AP radiographic angles that were more adducted than the values reported in a normal foot with no deformity6,10. In contrast, patients in the abducted group had mean postoperative AP radiographic parameters that were more abducted than the normal foot. Thus, overcorrection of the abduction deformity in stage II AAFD leads to statistically significantly worse outcomes, and the surgeon should aim to move the midfoot to a position in slight abduction compared to the normal foot with no deformity.
There are several limitations to this study. First, we used a retrospective study design with limited sample sizes for the two midfoot position groups. Radiographic and clinical outcomes follow-up time restricted the number of patients eligible for this study, and one patient did not have a preoperative AP radiograph. Additional power may have changed the significance of the pain and symptoms subscales, which had p-values just greater than our limit of 0.05. Second, the radiographic measurements have inherent limitations. Patients need to be carefully instructed to let their arch collapse fully while the x-ray is taken. If they do not, the x-ray measurements will underestimate the deformity. In this study, we did not measure eversion of the foot because it is difficult to quantify; however, the authors believe is important to outcomes to maintain near normal eversion, and the abduction and adduction categories are likely to have differences in the amount of eversion remaining after surgery with the adduction group having less eversion motion.
If the patient has adducted position at the talonavicular joint, the risk of lateral overload and lateral discomfort or pain increases2,5,8. Clearly, leaving the patient in more than mild abduction risks undercorrection and failure of the operation. Therefore we recommend leaving the patient in minimal abduction. In addition to an AP fluoroscopic simulated weight bearing view, we assess the eversion in the hindfoot, which is often excessive in patients with midfoot abduction deformity. Ideally the patient needs to have not a stiff hindfoot but near normal eversion motion remaining and no adduction but slight abduction on the AP view.
In this paper, we correlated midfoot position on postoperative AP radiographs to patient outcomes as measured by the FAOS, which has been previously validated in flatfoot patients. Correction of the talonavicular joint to a position of adduction following stage II AAFD was associated with a decreased amount of improvement in patient outcomes compared with correction to a midfoot abducted position. These results suggest that overcorrection to a position of midfoot adduction leads to a lesser amount of individual patient improvement in the reconstruction of stage II AAFD.
References
- 1.Chi TD, Toolan BC, Sangeorzan BJ, Hansen ST., Jr The lateral column lengthening and medial column stabilization procedures. Clin Orthop Relat Res. 1999;(365):81–90. doi: 10.1097/00003086-199908000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Davitt JS, MacWilliams BA, Armstrong PF. Plantar pressure and radiographic changes after distal calcaneal lengthening in children and adolescents. J Pediatr Orthop. 2001;21(1):70–75. doi: 10.1097/00004694-200101000-00015. [DOI] [PubMed] [Google Scholar]
- 3.Davitt JS, Morgan JM. Stress fracture of the fifth metatarsal after evans’ calcaneal osteotomy: A report of two cases. Foot Ankle Int. 1998;19(10):710–712. doi: 10.1177/107110079801901011. [DOI] [PubMed] [Google Scholar]
- 4.Deland JT. Adult-acquired flatfoot deformity. J Am Acad Orthop Surg. 2008;16(7):399–406. doi: 10.5435/00124635-200807000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Ellis SJ, Yu JC, Johnson AH, Elliott A, O’Malley M, Deland J. Plantar pressures in patients with and without lateral foot pain after lateral column lengthening. J Bone Joint Surg Am. 2010;92(1):81–91. doi: 10.2106/JBJS.H.01057. [DOI] [PubMed] [Google Scholar]
- 6.Ellis SJ, Yu JC, Williams BR, Lee C, Chiu YL, Deland JT. New radiographic parameters assessing forefoot abduction in the adult acquired flatfoot deformity. Foot Ankle Int. 2009;30(12):1168–1176. doi: 10.3113/FAI.2009.1168. [DOI] [PubMed] [Google Scholar]
- 7.Evans D. Calcaneo-valgus deformity. J Bone Joint Surg Br. 1975;57(3):270–278. [PubMed] [Google Scholar]
- 8.Griend R. Lateral column lengthening using a “Z” osteotomy of the calcaneus. Techniques in Foot & Ankle Surgery. 2008;7(4):257–263. [Google Scholar]
- 9.Hill K, Saar WE, Lee TH, Berlet GC. Stage II flatfoot: What fails and why. Foot Ankle Clin. 2003;8(1):91–104. doi: 10.1016/s1083-7515(03)00008-1. [DOI] [PubMed] [Google Scholar]
- 10.Kang S, Charlton TP, Thordarson DB. Lateral column length in adult flatfoot deformity. Foot Ankle Int. 2013;34(3):392–397. doi: 10.1177/1071100712465738. [DOI] [PubMed] [Google Scholar]
- 11.Mani SB, Brown HC, Nair P, et al. Validation of the foot and ankle outcome score in adult acquired flatfoot deformity. Foot Ankle Int. 2013 doi: 10.1177/1071100713483117. [DOI] [PubMed] [Google Scholar]
- 12.Mann RA, Thompson FM. Rupture of the posterior tibial tendon causing flat foot. surgical treatment. J Bone Joint Surg Am. 1985;67(4):556–561. [PubMed] [Google Scholar]
- 13.Mosca VS. Calcaneal lengthening for valgus deformity of the hindfoot. results in children who had severe, symptomatic flatfoot and skewfoot. J Bone Joint Surg Am. 1995;77(4):500–512. doi: 10.2106/00004623-199504000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Niki H, Hirano T, Okada H, Beppu M. Outcome of medial displacement calcaneal osteotomy for correction of adult-acquired flatfoot. Foot Ankle Int. 2012;33(11):940–946. doi: 10.3113/FAI.2012.0940. [DOI] [PubMed] [Google Scholar]
- 15.Oh I, Imhauser C, Choi D, Williams B, Ellis S, Deland J. Sensitivity of plantar pressure and talonavicular alignment to lateral column lengthening in flatfoot reconstruction. J Bone Joint Surg Am. 2013;95(12):1094–1100. doi: 10.2106/JBJS.K.01032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sangeorzan BJ, Mosca V, Hansen ST., Jr Effect of calcaneal lengthening on relationships among the hindfoot, midfoot, and forefoot. Foot Ankle. 1993;14(3):136–141. doi: 10.1177/107110079301400305. [DOI] [PubMed] [Google Scholar]
- 17.Scott AT, Hendry TM, Iaquinto JM, Owen JR, Wayne JS, Adelaar RS. Plantar pressure analysis in cadaver feet after bony procedures commonly used in the treatment of stage II posterior tibial tendon insufficiency. Foot Ankle Int. 2007;28(11):1143–1153. doi: 10.3113/FAI.2007.1143. [DOI] [PubMed] [Google Scholar]
- 18.Thomas RL, Wells BC, Garrison RL, Prada SA. Preliminary results comparing two methods of lateral column lengthening. Foot Ankle Int. 2001;22(2):107–119. doi: 10.1177/107110070102200205. [DOI] [PubMed] [Google Scholar]
- 19.Trnka HJ, Easley ME, Myerson MS. The role of calcaneal osteotomies for correction of adult flatfoot. Clin Orthop Relat Res. 1999;(365):50–64. doi: 10.1097/00003086-199908000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Zanolli DH, Glisson RR, Nunley JA, 2nd, Easley ME. Biomechanical assessment of flexible flatfoot correction: Comparison of techniques in a cadaver model. J Bone Joint Surg Am. 2014;96(6):e45. doi: 10.2106/JBJS.L.00258. [DOI] [PubMed] [Google Scholar]