Abstract
Purpose
We report a rare case of primary uveal lymphoma and characterize it using histopathology and multimodal imaging.
Patient and Methods
A 41-year-old male presented with a 2-year history of increasingly blurry vision in his right eye and no systemic symptoms. Examination revealed a retinal detachment and mass lesion in the right eye. Radiologic and histologic testing was performed.
Results
Multimodal imaging localized the lesion to the choroid, and fine needle aspiration biopsy diagnosed the lesion as a low-grade B-cell lymphoma. The patient was treated with external beam radiation, resulting in regression of the mass and resolution of the retinal detachment.
Conclusions
Primary uveal lymphoma is a rare, usually indolent tumor that carries a good prognosis. In this case, we show that primary uveal lymphoma has distinct findings via histopathology and multimodal imaging, and that imaging after radiation treatment documents disease regression.
Key Words: Primary uveal lymphoma, Histopathology, Fluorescein angiography, Optical coherence tomography
Introduction
Primary uveal lymphoma is a rare condition, with approximately 80 cases described in the literature [1]. Our understanding of this disease has undergone several major shifts. Although initial reports perpetuated the thinking that these lesions represented malignant lymphosarcoma, this changed in 1967 when Crookes and Mullaney [2] argued that they were actually a form of lymphoid hyperplasia. This characterization was subsequently challenged by Mauriello [3] in 1982, who reported that a majority of previously identified lymphoid hyperplasia cases were actually malignant lymphomas. Since then, newer diagnostic techniques have led to a gradual refinement of our understanding of these lesions, culminating in Coupland's 2002 report [1] that utilized immunohistochemistry and polymerase chain reaction to identify these lesions as extranodal marginal zone B-cell lymphomas.
Primary uveal lymphomas are extremely rare, and there are few reports showing multimodal imaging of the disease. Herein we present a case of primary uveal lymphoma with histopathologic correlation and multimodal imaging before and after treatment.
Case Report
A healthy 41-year-old male presented with a 2-year history of increasingly blurry vision in the right eye. His review of systems was otherwise negative. He had a family history of skin cancer in his father and leukemia in his cousin. Visual acuity was hand motions in the right eye and 20/20 in the left eye. Pressure was 16 OU. Slit-lamp biomicroscopy showed trace nuclear sclerotic cataracts in both eyes with no other abnormalities. Dilated examination of the right eye revealed a retinal detachment and an amelanotic subretinal mass extending from the posterior pole and tapering into the periphery (fig. 1).
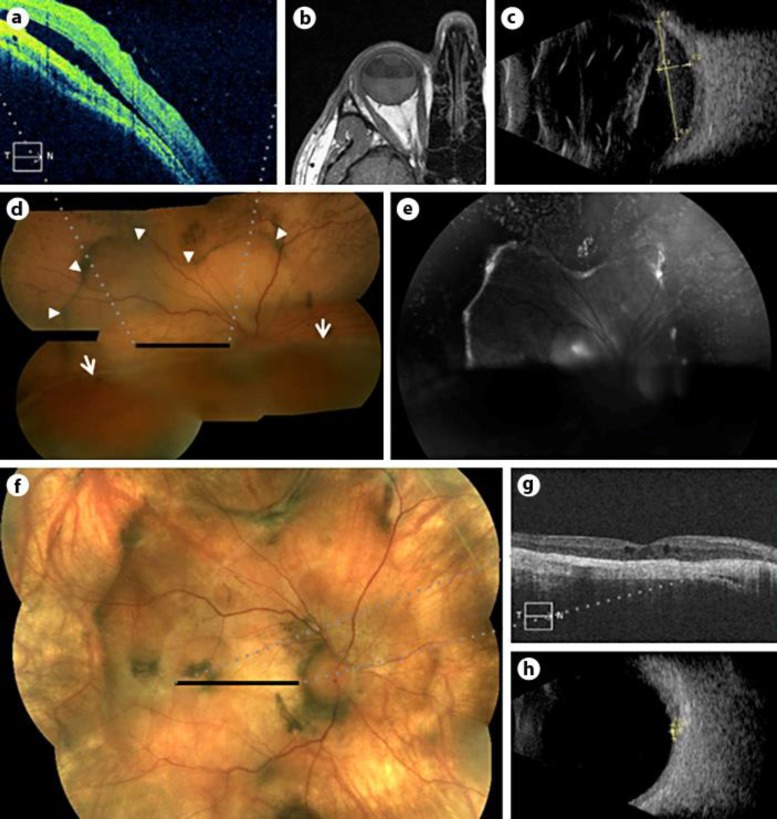
Fig. 1.
a–e Initial presentation. a OCT showing subretinal fluid, elevated choroid, and atrophic ONL (horizontal black bar in d shows corresponding area of fundus). b Axial T1 MRI showing hyperintense, thickened choroid and detachment. c Transverse B-scan showing bullous retinal detachment and irregular choroidal thickening. d Color fundus image showing choroidal mass lesion (arrowheads) and retinal detachment (arrows). e Sub-RPE and choroidal mass are highlighted with increased autofluorescence in the RPE. f–h 4.5 months after EBRT. f Color fundus showing mass regression, as well as prominent choroidal vasculature, RPE hyperplasia, and residual scarring. g OCT showing regression of mass and absence of subretinal fluid, along with some RPE atrophy and subretinal scar (horizontal black bar in f shows corresponding area of fundus). h Transverse B-scan showing mass regression and resolution of retinal detachment.
Color fundus photography revealed an exudative retinal detachment and an elevated whitish subretinal/choroidal mass lesion in the posterior pole. Fluorescein angiography revealed early hypofluorescence with minimal late hyperfluorescence. An MRI of the brain and orbit showed a 5-mm right choroidal mass in the posterior globe with no other intracranial findings, and OCT also revealed choroidal thickening. All of these findings were highly suggestive of uveal lymphoma [4] and help to differentiate this lesion from primary vitreoretinal lymphoma, which typically shows hyperreflective nodules at the RPE level and sub-RPE space on OCT, and clusters of round, hyper- or hypofluorescent lesions on fluorescein angiography [5]. The remainder of the workup was negative, including CT of the chest/abdomen/pelvis, CMP, LDH, CBC with differential, ACE, RPR, and quantiferon TB-gold.
Transcleral fine needle aspiration biopsy of the choroidal lesion was performed. Immunohistochemical staining of the cell block revealed a population of predominantly CD20-positive B lymphocytes with comparatively fewer CD3- and CD5-positive T cells. No co-expression of CD5 and BCL-1 was appreciated. IgH gene rearrangement for IgH V-D-J revealed a monoclonal population of B lymphocytes, consistent with lymphoma (fig. 2).
Fig. 2.
a Fine needle aspirate showing small lymphocytes, scattered pigmented and nonpigmented cells, and proteinaceous material (cell block HE; magnification ×1,000). b Immunohistochemical stain showing CD20 B lymphocytes (magnification ×1,000). c Immunohistochemical stain showing few CD3 T lymphocytes (magnification ×1,000).
The patient was treated with external beam radiation therapy (EBRT). Imaging obtained 4.5 months after ERBT showed excellent regression of the uveal mass, significantly reduced thickness of the choroidal lesion, resolution of the retinal detachment, and no signs of subretinal fluid. OCT demonstrated residual subretinal scarring (fig. 1). The patient's visual acuity remained hand motions.
Discussion
Primary uveal lymphomas arise in the uveal tract and are characterized by the absence of any systemic lymphoma. Patients are most often males in the fifth to seventh decade of life who present with unilateral painless blurring or vision loss [6]. Patients may respond to steroid therapy and chlorambucil has been effectively used in one reported case [7]. EBRT has frequently been reported to induce full remission [8].
Although our patient's vision did not improve following treatment, improvement in visual acuity has been reported in other cases. A retrospective review of nine cases showed high variability in visual outcomes, with no average improvement; however, in the case of a patient who was diagnosed and treated within 2 months of onset of symptoms, visual acuity went from 20/100 to 20/32 following treatment [4]. With smaller disease extent and timely diagnosis, good visual outcomes are still possible.
Conclusion
Approximately 80 cases of primary uveal lymphoma have been reported [1]. The tumor is usually indolent and carries a good prognosis. It tends to respond well to radiation treatment, as was the case with our patient. This report has shown that primary uveal lymphoma demonstrates distinct findings via histopathology and multimodal imaging, and that post-ERBT follow-up imaging clearly documents regression of the lesion.
Statement of Ethics
This is a case report that complied with the guidelines for human studies. The patient has given informed consent for publication.
Disclosure Statement
The authors declare no conflicts of interest.
Acknowledgments
Supported by the National Eye Institute of the National Institutes of Health under Award Number K08EY022672. The content is solely the responsibility of the authors and does not necessarily represent the official views of these institutions. Additional funds were provided by the Ohio Lions Eye Research Foundation and the Patti Blow Fund.
References
- 1.Coupland SE, Foss H-D, Hidayat AA, Cockerham GC, Hummel M, Stein H. Extranodal marginal zone B cell lymphomas of the uvea: an analysis of 13 cases. J Pathol. 2002;197:333–340. doi: 10.1002/path.1130. [DOI] [PubMed] [Google Scholar]
- 2.Crookes GP, Mullaney J. Lymphoid hyperplasia of the uveal tract simulating malignant lymphoma. Am J Ophthalmol. 1967;63:962–967. doi: 10.1016/0002-9394(67)90040-2. [DOI] [PubMed] [Google Scholar]
- 3.Mauriello JA. A clinicopathologic and immunohistologic study of lymphoproliferative lesions of the uveal tract. ARVO Abstracts. Invest Ophthalmol Vis Sci. 1982;22:171. [Google Scholar]
- 4.Loriaut P, Charlotte F, Bodaghi B, Decaudin D, Leblond V, Fardeau C, et al. Choroidal and adnexal extranodal marginal zone B-cell lymphoma: presentation, imaging findings, and therapeutic management in a series of nine cases. Eye Lond Engl. 2013;27:828–835. doi: 10.1038/eye.2013.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chan C-C, Rubenstein JL, Coupland SE, Davis JL, Harbour JW, Johnston PB, et al. Primary vitreoretinal lymphoma: a report from an International Primary Central Nervous System Lymphoma Collaborative Group symposium. Oncologist. 2011;16:1589–1599. doi: 10.1634/theoncologist.2011-0210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coupland SE, Damato B. Understanding intraocular lymphomas. Clin Experiment Ophthalmol. 2008;36:564–578. doi: 10.1111/j.1442-9071.2008.01843.x. [DOI] [PubMed] [Google Scholar]
- 7.Rospond-Kubiak I, Kocięcki J, Stopa M. Primary uveal lymphoma effectively managed with oral chlorambucil: a case report. J Med Case Reports. 2013;7:173. doi: 10.1186/1752-1947-7-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aronow ME, Portell CA, Sweetenham JW, Singh AD. Uveal lymphoma: clinical features, diagnostic studies, treatment selection, and outcomes. Ophthalmology. 2014;121:334–341. doi: 10.1016/j.ophtha.2013.09.004. [DOI] [PubMed] [Google Scholar]