Supplemental Digital Content is available in the text
Abstract
Comparable data on trends of hospitalization rates for ST-segment elevation myocardial infarction (STEMI) and non-STEMI (NSTEMI) remain unavailable in representative Asian populations.
To examine the temporal trends of hospitalization for acute myocardial infarction (AMI) and its subtypes in Beijing.
Patients hospitalized for AMI in Beijing from January 1, 2007 to December 31, 2012 were identified from the validated Hospital Discharge Information System. Trends in hospitalization rates, in-hospital mortality, length of stay (LOS), and hospitalization costs were analyzed by regression models for total AMI and for STEMI and NSTEMI separately. In total, 77,943 patients were admitted for AMI in Beijing during the 6 years, among whom 67.5% were males and 62.4% had STEMI. During the period, the rate of AMI hospitalization per 100,000 population increased by 31.2% (from 55.8 to 73.3 per 100,000 population) after age standardization, with a slight decrease in STEMI but a 3-fold increase in NSTEMI. The ratio of STEMI to NSTEMI decreased dramatically from 6.5:1.0 to 1.3:1.0. The age-standardized in-hospital mortality decreased from 11.2% to 8.6%, with a significant decreasing trend evident for STEMI in males and females (P < 0.001) and for NSTEMI in males (P = 0.02). The rate of percutaneous coronary intervention increased from 28.7% to 55.6% among STEMI patients. The total cost for AMI hospitalization increased by 56.8% after adjusting for inflation, although the LOS decreased by 1 day.
The hospitalization burden for AMI has been increasing in Beijing with a transition from STEMI to NSTEMI. Diverse temporal trends in AMI subtypes from the unselected “real-world” data in Beijing may help to guide the management of AMI in China and other developing countries.
INTRODUCTION
Coronary heart disease (CHD) is the leading cause of death worldwide.1 Acute myocardial infarction (AMI) represents a serious clinical manifestation of CHD and is associated with high mortality, especially during hospitalization in the acute phase.2 Therefore, information on trends of hospitalization for AMI is of considerable value to health-policy makers, hospital administrators, clinicians, and researchers.
Routinely collected data on hospital discharges in the United States and Europe have indicated declining trends of hospitalization rates for AMI, with a shift away from ST-segment elevation myocardial infarction (STEMI) toward rising rates of non-STEMI (NSTEMI).3–5 STEMI and NSTEMI are 2 major subtypes of AMI representing markedly different treatment options and outcomes. Unlike the dominance of NSTEMI in Western countries, STEMI accounts for 60% to 80% of AMI in Asians.6–8 A declining proportion of STEMI accompanied by an increasing proportion of NSTEMI was recently observed in a hospital-based registry study in Korea.8 However, to the best of our knowledge, comparable data on trends of hospitalization rates for STEMI and NSTEMI remain unavailable in representative Asian populations.
Beijing, the capital of China and home to more than 19.61 million people, is characterized by a Western lifestyle, and leads the increasing trends in the incidence and mortality rates of acute coronary events in China during the 1980s and 1990s according to the Sino-MONICA (multinational monitoring of trends and determinants in cardiovascular disease) project.9 Since the termination of the MONICA project, representative data on temporal trends of coronary events, particularly nonfatal events, are sparse in Beijing. The rapid development of the health information system in the past decade in Beijing provides an opportunity to monitor CHD morbidity and mortality based on routinely collected administrative data at the city level.10 Accordingly, based on the validated data from the Beijing Hospital Discharge Information System (HDIS) from 2007 to 2012, we examined the patient characteristics and temporal trends of hospitalization for AMI and its subtypes in terms of hospitalization rate, in-hospital mortality, length of stay (LOS), and hospitalization costs.
METHODS
Data Sources
Data on the age-specific annual population of permanent residents in Beijing for each year of interest were obtained from the Beijing Municipal Bureau of Statistics. Data were obtained from the Beijing HDIS, a system covering all secondary and tertiary nonmilitary hospitals in Beijing. A total of 162 hospitals, including both public and private hospitals, report hospital discharge abstracts to the HDIS. Hospital admissions for AMI from January 1, 2007 to December 31, 2012 among permanent residents of Beijing were identified according to the principal discharge diagnosis using the International Classification of Diseases 10th revision (ICD-10) codes I21 (AMI) or I22 (subsequent AMI), and subtypes of AMI were further classified (STEMI codes I21.0–I21.3, I22.0, I22.1, and I22.8; NSTEMI code I21.4; unspecified AMI I21.9 and I22.9) by referring to previous reports3,4 and our validation study (see Table 1, supplemental content, Concordance of ICD code-based diagnoses/procedures in hospital discharge information system with the clinical diagnoses/procedures in hospital charts). ICD-10 has been adopted in China since 2002 and the codes for AMI have not been changed during the study time period. Comorbidities were identified from secondary discharge diagnoses (up to 7 diagnoses). Revascularization treatments were identified using codes from International Classification of Diseases Clinical Modification of 9th Revision Operations and Procedures (ICD-9-CM-3), with codes 00.66, 36.01, 36.02, 36.05, 36.06, and 36.07 for percutaneous coronary intervention (PCI) and ×36.1 for coronary artery bypass grafting (CABG). ICD code-based diagnoses/procedures in the HDIS were validated based on chart reviews (see Table 1 and Table 2, supplemental content, which illustrate concordance of ICD code-based diagnoses/procedures in hospital discharge information system with the clinical diagnoses/procedures in hospital charts and predictive value of ICD codes for AMI in hospital discharge information system for clinical diagnosis of AMI defined by MONICA Criteria or Third Universal Definition of Myocardial Infarction respectively). Patients with a total LOS of ≤1 day and who were discharged alive were excluded (857 cases) because they were unlikely to have had an AMI.11 Patients who were discharged and then rehospitalized on the same day (including transferred patients) were linked according to personal identification information and considered a single continuous episode of care (2272 cases). In total, 77,943 hospital admissions for AMI were included in the final analysis. This project (contract No. 2011-1005-01) was funded by the Beijing Health Bureau and approved by the Ethics Committee of Beijing Anzhen Hospital.
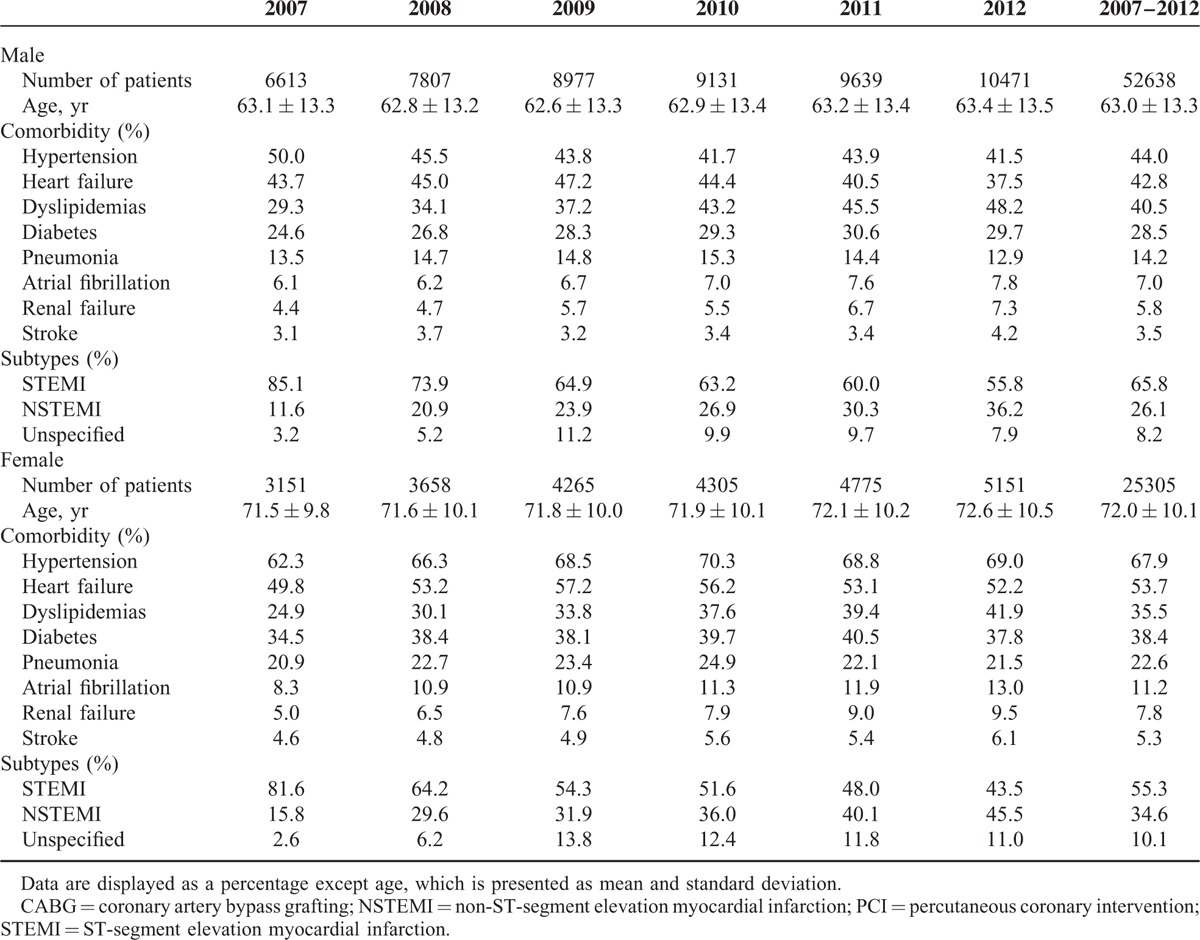
TABLE 1.
Characteristics of Patients Hospitalized for AMI in Beijing by Sex, 2007 to 2012
Statistical Analysis
The hospitalization rate of AMI was defined as the number of AMI hospitalizations for each age–sex category divided by the corresponding population estimate and standardized to the 2000 Census population of Beijing. The in-hospital mortality of AMI was calculated as the number of inpatients who died of AMI for each age–sex category divided by the corresponding number of AMI hospitalizations and was standardized according to the total of AMI admissions from 2007 to 2012. Trends in hospitalization rates and in-hospital mortality rates throughout the study period were tested using the Poisson regression and adjusted for age and sex or age alone as needed.11 The LOS is presented as the geometric means in days, given the skewed distribution, and the temporal trends of LOS were estimated by linear regression models after log-transformation.5 Similar methods were used for the analysis of the temporal trends of hospital cost per hospitalization. To facilitate direct comparisons between years for hospital costs, we converted all hospital costs to 2012 Chinese Yuan RMB using the consumer price index in China. All P values were 2-sided, with significance set at P < 0.05. Statistical analyses were performed using SAS version 9.2 (SAS Institute Inc, Cary, NC).
RESULTS
Patient Characteristics
There were 77,943 hospital admissions for AMI in Beijing from 2007 to 2012 (Figure 1). The mean age was 65.9 ± 13.1 years, and 67.5% of patients were men. Female patients were 9 years older and more multimorbid than males (Table 1). The proportion of STEMI was higher in males, while the opposite was true for NSTEMI. Collectively, 62.4% of the AMI cases were STEMI, 28.8% were NSTEMI, and 8.8% were unspecified. During the 6 years, the ratio of STEMI to NSTEMI decreased dramatically from 6.5:1.0 in 2007 to 1.3:1.0 in 2012 (Figure 2). Compared with patients with STEMI, those with NSTEMI were 4.9 years older (69.0 ± 12.2 vs 64.1 ± 13.2 yr) and more likely to have coexisting illnesses (Figure 3). The proportion of PCI use increased from 28.7% to 55.6% over the 6 years in patients with STEMI, and from 22.7% to 30.0% in those with NSTEMI (both P < 0.001). The rate of CABG dropped slightly from 2.7% to around 2% in patients with STEMI (P = 0.04) and remained stable at around 3% in those with NSTEMI throughout the study period (P = 0.65) (Figure 4).
FIGURE 1.
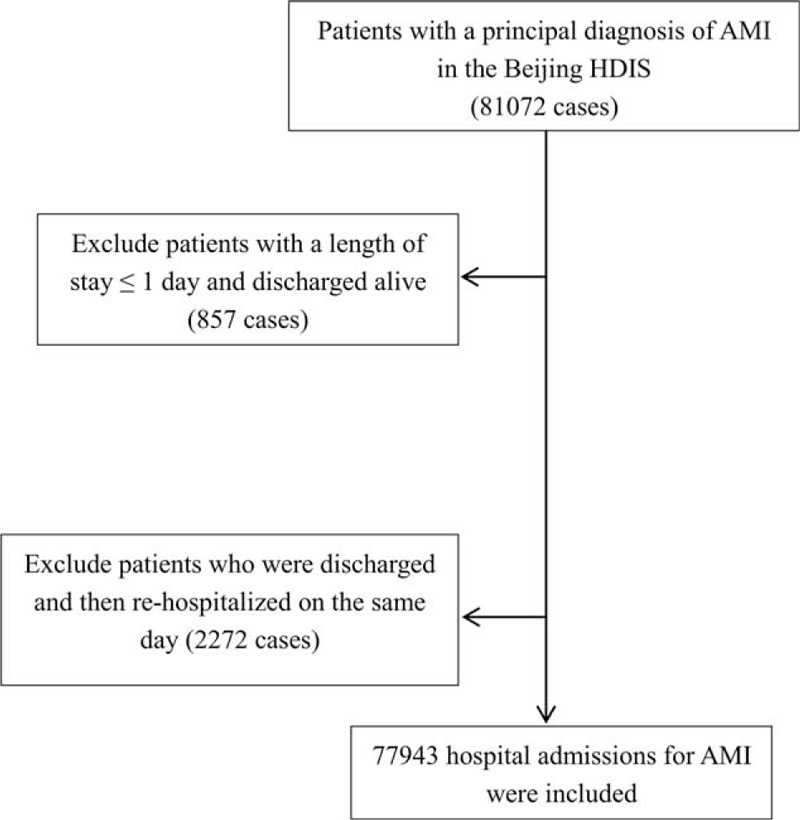
Flow diagram for the selection of patients hospitalized with AMI. AMI = acute myocardial infarction; HDIS = hospital discharge information system.
FIGURE 2.
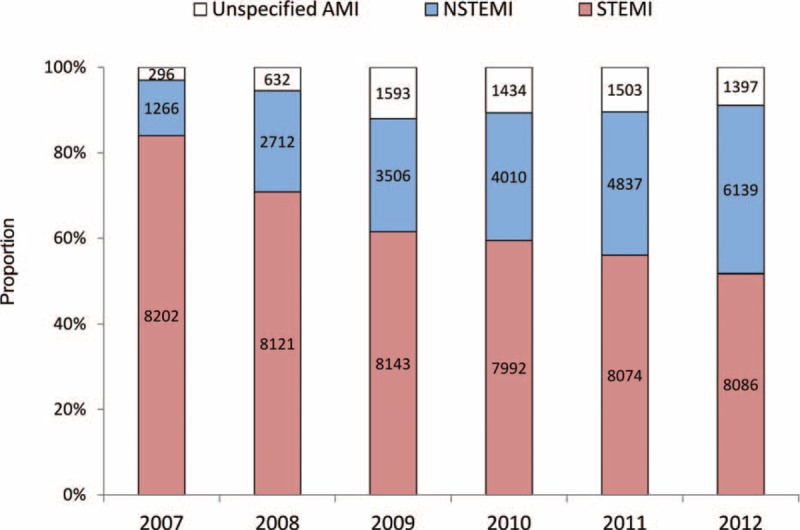
Proportion and the number of patients hospitalized for different subtypes of acute myocardial infarction in Beijing, 2007 to 2012. NSTEMI = non-ST-segment elevation myocardial infarction; STEMI = ST-segment elevation myocardial infarction.
FIGURE 3.
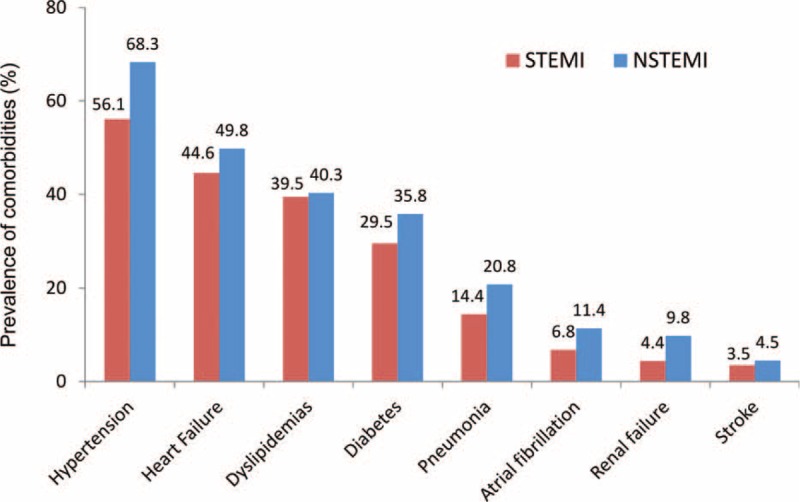
Prevalence of comorbidities in patients hospitalized for ST-segment elevation and non-ST-segment elevation myocardial infarction in Beijing, 2007 to 2012. NSTEMI = non-ST-segment elevation myocardial infarction; STEMI = ST-segment elevation myocardial infarction.
FIGURE 4.
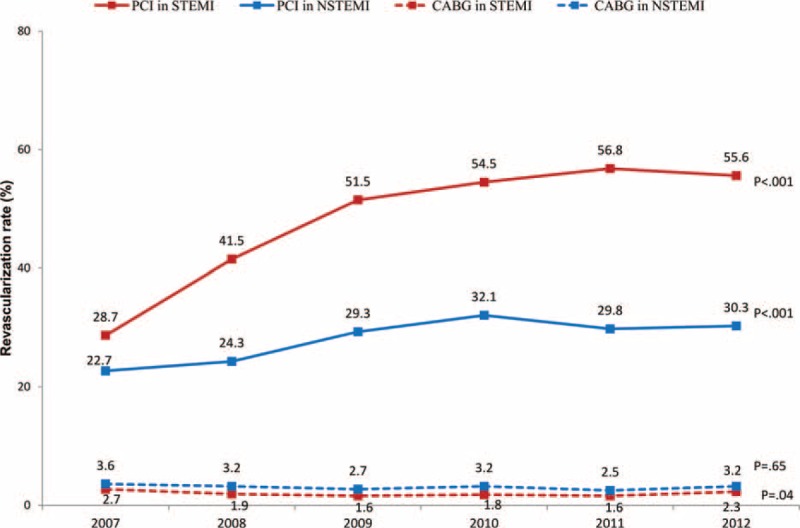
Use of revascularization in patients hospitalized for ST-segment elevation and non-ST-segment elevation myocardial infarction in Beijing, 2007 to 2012. CABG = coronary artery bypass grafting; NSTEMI = non-ST-segment elevation myocardial infarction; PCI = percutaneous coronary intervention; STEMI = ST-segment elevation myocardial infarction.
Hospitalization Rates
During the 6 years, the AMI hospitalization rate per 100,000 population increased by 49.5% (from 80.5 to 120.4) before and by 31.2% (from 55.8 to 73.3) after age standardization with the greatest increase noted in the youngest age group (<55 years) in both sexes (Table 2). Diverse trends were found for subtypes of AMI, with a slight decrease in the rate of STEMI but a three-fold increase in the rate of NSTEMI (Figure 5).
TABLE 2.
Hospitalization Rate (per 100,000 Population) for Patients With Acute Myocardial Infarction (AMI) in Beijing by Sex, Age, and AMI Subtype, 2007 to 2012
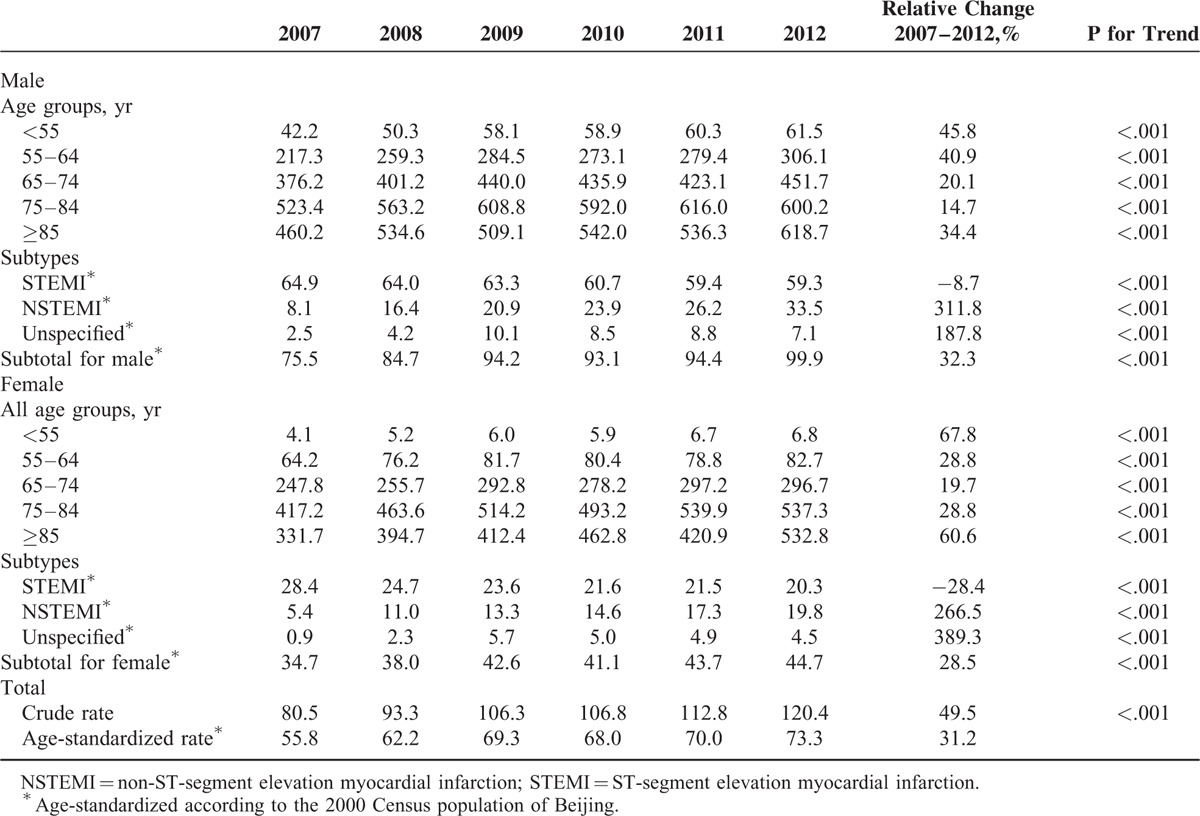
FIGURE 5.
Hospitalization rate of acute myocardial infarction in Beijing, 2007 to 2012. NSTEMI = non-ST-segment elevation myocardial infarction; STEMI = ST-segment elevation myocardial infarction.
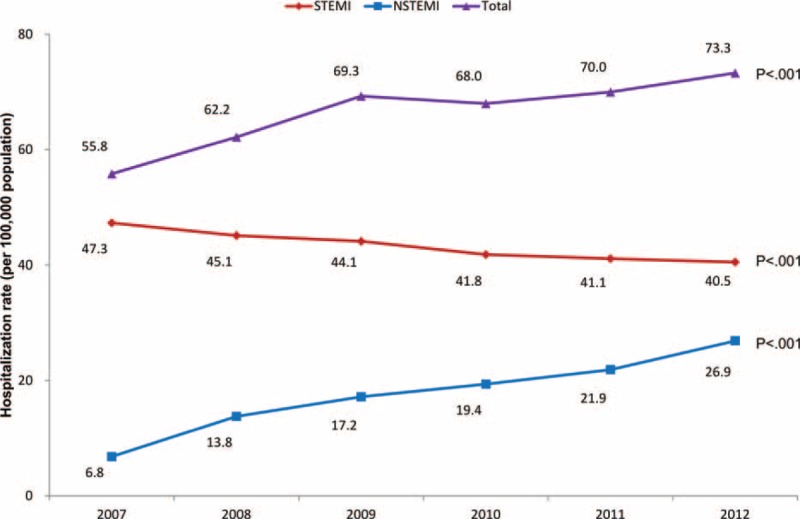
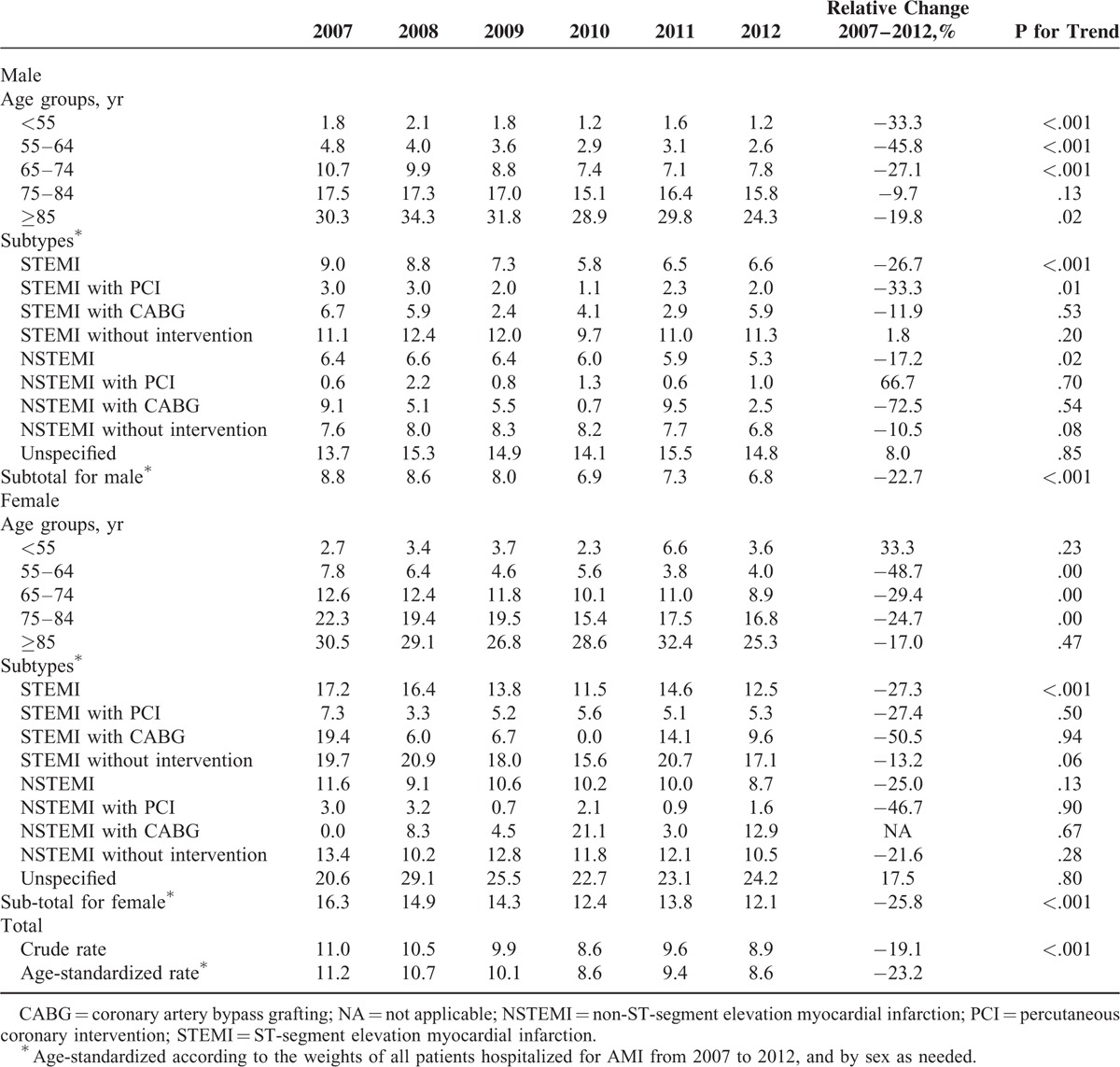
In-Hospital Mortality
In-hospital mortality was higher in women than men and higher in STEMI than NSTEMI (Table 3). From 2007 to 2012, the age-standardized in-hospital mortality decreased from 11.2% to 8.6%, with a significant decreasing trend evident for STEMI in both males and females and for NSTEMI in males. Regarding treatment, in-hospital mortality was lower for patients receiving revascularization therapies, particularly those undergoing PCI. During the 6 years, a significant decline in in-hospital mortality was observed for male patients with STEMI who underwent PCI (P = 0.01).
TABLE 3.
In-Hospital Mortality (%) for Patients With Acute Myocardial Infarction (AMI) in Beijing, by Sex, Age, AMI Subtype, and Type of Intervention, 2007 to 2012
Length of Hospital Stay and In-Hospital Costs
The LOS was longer in women than in men and longer in patients with NSTEMI than STEMI (see Table 3, supplemental content, which illustrates the geometric means of hospital LOS for patients with AMI). Over the period, the overall LOS was shortened by 0.9 day (from 10.6 to 9.7 days). Meanwhile, the in-hospital cost per hospitalization for AMI increased by 3.2% after adjusting for inflation (P < 0.001), with a significant decrease achieved in PCI for both STEMI and NSTEMI but an increase for CABG (see Table 4, supplemental content, which illustrate geometric means of hospital costs per hospitalization for patients with AMI in Beijing by sex, AMI subtype, and type of intervention from 2007 to 2012). The cost of all AMI hospitalizations increased by 81.6% before (from 0.38 billion RMB in 2007–0.69 billion RMB in 2012) and 56.8% after adjusting for inflation throughout the study period.
DISCUSSION
Using a large database of an unselected hospitalized patient population of AMI, we demonstrated a significant increase in AMI hospitalization rates in Beijing with a rapid change in the pattern of AMI subtypes: a marked rise in the rate of NSTEMI accompanied by an underlying reduction in the rate of STEMI. In-hospital mortality and LOS decreased, whereas per-hospitalization and total in-hospital costs increased steadily. This is, to our knowledge, the first study using validated “real-world” data at the city level in China.
Unlike the decrease in the AMI hospitalization rate in Western populations,4,11,12 our study found an overall increasing trend of AMI hospitalization in Beijing, whereas the trend varies greatly by subtypes of AMI. One notable finding was the transition of the AMI subtypes from STEMI to NSTEMI in Beijing, following earlier trends in Western populations.4,11,12 The hospitalization rate for NSTEMI exceeded that for STEMI around the year 2005 in Germany3 and Ireland4 and in the 1990s in the United States.2,13 Our findings indicate that this transition is happening in Asian populations, among which STEMI has been dominant.6,7 We found that the ratio of STEMI to NSTEMI decreased dramatically from 6.5:1.0 in 2007 to 1.3:1.0 in 2012 and that the proportion of NSTEMI outpaced STEMI in 2012 among females. Similarly, a proportional outweighing of NSTEMI to STEMI occurred in 2012 in the Korea Acute Myocardial Infarction Registry.8 Another interesting finding was the greatest increase in AMI hospitalization was noted in the youngest age group (<55 years) in both sexes, which was consistent with the high prevalence of cardiovascular risk factors in young and middle-aged adults and in elder age groups of Beijing.14–16
Both a decrease in STEMI and increase in NSTEMI may contribute to the transition in the pattern of AMI subtypes in a population. The decrease in the STEMI hospitalization rate in our population was consistent with the declining trend in most Western populations.2–5,17 In contrast, based on data from 162 hospitals across China, the estimated national hospitalization rate for STEMI increased from 3.5 in 2001 to 15.4 in 2011 per 100,000 people in the China PEACE study.18 More advanced primary and secondary prevention of cardiovascular disease in Beijing than in the rest of China may partly explain the decreasing trend in STEMI in Beijing, which is similar to the pattern in Western populations but differs from the national status as found in the China PEACE study. The use of certain cardioprotective medications (eg, statins, ACE inhibitors, beta-blockers, and aspirin) reportedly may contribute to a lower risk of presenting with STEMI.19 As a leading developed metropolis in China, Beijing has made substantial improvement in the treatment of AMI.20,21 Additionally, the awareness and treatment of cardiovascular risk factors, such as dyslipidemia, are more advanced in Beijing than in overall China,22,23 which may contribute to the decreased STEMI in Beijing. On the other hand, the hospitalization rates for NSTEMI increased remarkably by three-fold in Beijing during the 6 years, unlike the mild increases in Western populations.2,4,13,24 As a result, the overall rate of AMI increased significantly despite the decline in STEMI. The increase in hospitalization rates for NSTEMI is attributable to multiple causes. First, the use of highly sensitive cardiac biomarkers, particularly troponin, may have contributed to the increase in hospitalization for NSTEMI, as observed in Western countries in the early 2000s.2,4,13 Cardiac troponins have been introduced for the diagnosis of AMI in China since 2001 and widely available in urban cities in 2006.25 Moreover, previous studies reported that implementation of troponin classified an additional 26% to 58% of patients as having AMI compared with traditional enzymatic markers.26,27 Therefore, the use of troponins may not solely explain the three-fold increase in NSTEMI. Another possible reason for the increase in NSTEMI could be the changing characteristics of patients. Previous studies have observed that advanced age and the presence of comorbidities are associated with a higher probability of presenting with NSTEMI.3,28 Similar results were found in our study. Given the population aging and increasing prevalence of cardiovascular risk factors in both the general population and patients with CHD,18,29,30 the hospitalization rates for NSTEMI are expected to continue increasing in Beijing and the rest of China.
We observed a declined trend in the AMI in-hospital mortality in Beijing. The trends toward improved outcome of AMI were also observed in some Western countries.31–33 Previous studies indicated that the outcomes of STEMI and NSTEMI are distinct and vary by the type of intervention received.3–5 Our study supports previous findings in that the in-hospital mortality was significantly higher in patients with STEMI than in those with NSTEMI. However, during the study period, in-hospital mortality declined significantly for patients with STEMI, particularly for those who underwent PCI, but the outcome for patients with NSTEMI was not improved by the type of treatment received. Similarly, among patients with STEMI in the United States, the improvement in in-hospital mortality was statistically significant only for those who underwent PCI; no improvement was observed for those who received CABG or no intervention.5 Compared with STEMI, patients with NSTEMI were less likely to undergo cardiac catheterization or PCI during their hospitalization, and no significant improvement in in-hospital mortality by type of therapy was observed in our analysis. Evidence has demonstrated that improvement in medical or intervention therapies consistent with guidelines was associated with improvement in in-hospital mortality for patients with NSTEMI.5,24,34 However, a substantial gap in the in-hospital treatment for patients with NSTEMI was also found in studies in Europe and the United States.2,35,36 Moreover, the long-term mortality for patients with NSTEMI is reportedly worse than that for patients with STEMI because the former are considerably older and have a higher prevalence of cardiovascular comorbidities.2,35,36 These findings, in line with ours, indicate that there is an urgent need to improve the quality of care for patients with NSTEMI, a condition that is on the rise.
The LOS and hospitalization costs are valuable indicators of health burden and allocation of resources. We observed that the LOS for AMI declined by an average of 1 day over 6 years in Beijing, but it remained longer than that in the United States and Europe.37 Despite the decline in LOS, the in-hospital cost per hospitalization for AMI increased by 3.2% in Beijing during the 6 years. Although there was a marked decline in the hospitalization cost for patients undergoing PCI and no intervention, the decline was offset by the increased hospitalization costs in patients undergoing CABG. Due to the increase in hospital cost per hospitalization and the number of hospitalizations, the aggregate hospital cost for AMI hospitalization reached 0.69 billion RMB (0.11 billion USD) at the city level in 2012, representing a 56.8% increase after adjusting for inflation compared with 2007. The current governmental health insurance system will face a substantial challenge if no effective measure is taken to control the increase in total health expenditure associated with AMI hospitalization in Beijing.
This study has important implications. The rising hospitalization rates and expenditures should encourage policy makers to develop more cost-effective approaches for the prevention and management of AMI. From the clinical perspective, the transition from STEMI to NSTEMI emphasized the necessity of improving the treatment of patients with NSTEMI and the management of cardiovascular comorbidities. This study involved a large, unselected population from a megacity characterized by rapid socioeconomic development and transition in the pattern of disease, which may indicate coming trends in other cities in China and other developing countries.
Our findings should be interpreted with caution because of several limitations. First, the current analysis was based on the routinely collected data in the HDIS. The quality of hospital discharge data regarding the diagnosis of AMI has not been validated in China before. Our validation study is the first to show that hospital discharge data are reliable regarding the diagnosis of AMI and the differentiation of AMI subtypes. However, given the large sample size, the validation was conducted only for a sample of 1736 patients selected by using stratified sampling method. Second, military hospitals are not covered by the Beijing HDIS. However, the number of local patients with AMI admitted to military hospitals is likely to be small and stable; thus, their exclusion was unlikely to alter the current trends, although the hospitalization rates would be somewhat underestimated. Besides, information on medications provided during hospitalization are not available in Beijing HDIS, thus precluding the assessment of thrombolysis, as reported by previous studies using hospital discharge data.38
In conclusion, the hospitalization rates of AMI increased significantly in Beijing from 2007 to 2012 with a transition from STEMI to NSTEMI. In-hospital mortality and LOS decreased, whereas per-hospitalization and total in-hospital costs increased steadily. Findings from these unselected “real-world” data in Beijing may help to guide the management of AMI in China and other developing countries.
Supplementary Material
Footnotes
Abbreviations: AMI = acute myocardial infarction, CABG = coronary artery bypass graft, CHD = coronary heart disease, HDIS = Hospital Discharge Information System, ICD-10 = the International Classification of Diseases 10th Revision, ICD-9-CM-3 = International Classification of Diseases Clinical Modification of 9th Revision Operations and Procedures, LOS = length of stay, NSTEMI = non-ST-segment elevation myocardial infarction, PCI = percutaneous coronary intervention, STEMI = ST-segment elevation myocardial infarction.
This work was supported by the Capital Health Research and Development of Special [contract No. 2011-1005-01]. The fund provider had no role in study design, data collection and analysis, decision to publish, and preparation of the manuscript. No additional external funding was received for this study.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015; 385:117–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McManus DD, Gore J, Yarzebski J, et al. Recent trends in the incidence, treatment, and outcomes of patients with STEMI and NSTEMI. Am J Med 2011; 124:40–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Freisinger E, Fuerstenberg T, Malyar NM, et al. German nationwide data on current trends and management of acute myocardial infarction: discrepancies between trials and real-life. Eur Heart J 2014; 35:979–988. [DOI] [PubMed] [Google Scholar]
- 4.Jennings SM, Bennett K, Lonergan M, et al. Trends in hospitalisation for acute myocardial infarction in Ireland, 1997–2008. Heart 2012; 98:1285–1289. [DOI] [PubMed] [Google Scholar]
- 5.Sugiyama T, Hasegawa K, Kobayashi Y, et al. Differential time trends of outcomes and costs of care for acute myocardial infarction hospitalizations by ST elevation and type of intervention in the United States, 2001-2011. J Am Heart Assoc 2015; 4:e001445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gao R, Patel A, Gao W, et al. Prospective observational study of acute coronary syndromes in China: practice patterns and outcomes. Heart 2008; 94:554–560. [DOI] [PubMed] [Google Scholar]
- 7.Ishihara M, Fujino M, Ogawa H, et al. Clinical presentation, management and outcome of Japanese patients with acute myocardial infarction in the troponin era: Japanese Registry of Acute Myocardial Infarction diagnosed by universal definition (J-MINUET). Circ J 2015; 79:1255–1262. [DOI] [PubMed] [Google Scholar]
- 8.Kook HY, Jeong MH, Oh S, et al. Current trend of acute myocardial infarction in Korea (from the Korea Acute Myocardial Infarction Registry from 2006 to 2013). Am J Cardiol 2014; 114:1817–1822. [DOI] [PubMed] [Google Scholar]
- 9.Wu Z, Yao C, Zhao D, et al. Sino-MONICA project: a collaborative study on trends and determinants in cardiovascular diseases in China, Part i: morbidity and mortality monitoring. Circulation 2001; 103:462–468. [DOI] [PubMed] [Google Scholar]
- 10.Xie W, Li G, Zhao D, et al. Relationship between fine particulate air pollution and ischaemic heart disease morbidity and mortality. Heart 2015; 101:257–263. [DOI] [PubMed] [Google Scholar]
- 11.Chen J, Normand SL, Wang Y, et al. Recent declines in hospitalizations for acute myocardial infarction for Medicare fee-for-service beneficiaries: progress and continuing challenges. Circulation 2010; 121:1322–1328. [DOI] [PubMed] [Google Scholar]
- 12.Koopman C, Bots ML, van Oeffelen AA, et al. Population trends and inequalities in incidence and short-term outcome of acute myocardial infarction between 1998 and 2007. Int J Cardiol 2013; 168:993–998. [DOI] [PubMed] [Google Scholar]
- 13.Yeh RW, Sidney S, Chandra M, et al. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med 2010; 362:2155–2165. [DOI] [PubMed] [Google Scholar]
- 14.Wang JH, Hu DY, Fu YY, et al. Epidemiologic characteristics of major risk factors of coronary heart disease in residents from Beijing communities in different age groups. Zhonghua Yi Xue Za Zhi 2010; 90:529–534. [PubMed] [Google Scholar]
- 15.Cai L, Liu A, Zhang L, et al. Prevalence, awareness, treatment, and control of hypertension among adults in Beijing, China. Clin Exp Hypertens 2012; 34:45–52. [DOI] [PubMed] [Google Scholar]
- 16.Zhang J, Dong Z, Li G, et al. A cross-sectional study on risk factors of associated type 2 diabetes mellitus among adults in Beijing. Zhonghua Liu Xing Bing Xue Za Zhi 2011; 32:357–360. [PubMed] [Google Scholar]
- 17.Movahed MR, Khan MF, Hashemzadeh M, et al. Age adjusted nationwide trends in the incidence of all cause and ST elevation myocardial infarction associated cardiogenic shock based on gender and race in the United States. Cardiovasc Revasc Med 2015; 16:2–5. [DOI] [PubMed] [Google Scholar]
- 18.Li J, Li X, Wang Q, et al. ST-segment elevation myocardial infarction in China from 2001 to 2011 (the China PEACE-Retrospective Acute Myocardial Infarction Study): a retrospective analysis of hospital data. Lancet 2015; 385:441–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bjorck L, Wallentin L, Stenestrand U, et al. Medication in relation to ST-segment elevation myocardial infarction in patients with a first myocardial infarction: Swedish Register of Information and Knowledge About Swedish Heart Intensive Care Admissions (RIKS-HIA). Arch Intern Med 2010; 170:1375–1381. [DOI] [PubMed] [Google Scholar]
- 20.Liu HX, Gao W, Zhao D, et al. Survey on the hospitalization treatment status of acute myocardial infarction patients in 13 hospitals of western medicine and traditional Chinese medicine in Beijing. Zhonghua Xin Xue Guan Bing Za Zhi 2010; 38:306–310. [PubMed] [Google Scholar]
- 21.Wang SR, Liu HX, Zhao D, et al. Study on the therapeutic status of 1242 hospitalized acute myocardial infarction patients in Beijing. Zhonghua Liu Xing Bing Xue Za Zhi 2006; 27:991–995. [PubMed] [Google Scholar]
- 22.Qian F, Ling FS, Deedwania P, et al. Care and outcomes of Asian-American acute myocardial infarction patients: findings from the American Heart Association Get With The Guidelines-Coronary Artery Disease program. Circ Cardiovasc Qual Outcomes 2012; 5:126–133. [DOI] [PubMed] [Google Scholar]
- 23.Cai L, Zhang L, Liu A, et al. Prevalence, awareness, treatment, and control of dyslipidemia among adults in Beijing, China. J Atheroscler Thromb 2012; 19:159–168. [DOI] [PubMed] [Google Scholar]
- 24.Khera S, Kolte D, Aronow WS, et al. Non-ST-elevation myocardial infarction in the United States: contemporary trends in incidence, utilization of the early invasive strategy, and in-hospital outcomes. J Am Heart Assoc 2014; 3:e000995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhan L, Masoudi FA, Li X, et al. Trends in cardiac biomarker testing in China for patients with acute myocardial infarction, 2001 to 2011: China PEACE-retrospective AMI study. PLoS One 2015; 10:e0122237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Trevelyan J, Needham EW, Smith SC, et al. Impact of the recommendations for the redefinition of myocardial infarction on diagnosis and prognosis in an unselected United Kingdom cohort with suspected cardiac chest pain. Am J Cardiol 2004; 93:817–821. [DOI] [PubMed] [Google Scholar]
- 27.Pell JP, Simpson E, Rodger JC, et al. Impact of changing diagnostic criteria on incidence, management, and outcome of acute myocardial infarction: retrospective cohort study. BMJ 2003; 326:134–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rosengren A, Wallentin L, Simoons M, et al. Age, clinical presentation, and outcome of acute coronary syndromes in the Euroheart acute coronary syndrome survey. Eur Heart J 2006; 27:789–795. [DOI] [PubMed] [Google Scholar]
- 29.Cao CF, Ren JY, Zhou XH, et al. Twenty-year trends in major cardiovascular risk factors in hospitalized patients with acute myocardial infarction in Beijing. Chin Med J (Engl) 2013; 126:4210–4215. [PubMed] [Google Scholar]
- 30.Yang W, Xiao J, Yang Z, et al. Serum lipids and lipoproteins in Chinese men and women. Circulation 2012; 125:2212–2221. [DOI] [PubMed] [Google Scholar]
- 31.Smolina K, Wright FL, Rayner M, et al. Determinants of the decline in mortality from acute myocardial infarction in England between 2002 and 2010: linked national database study. Bmj 2012; 344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hanssen M, Cottin Y, Khalife K, et al. French Registry on Acute ST-elevation and non ST-elevation Myocardial Infarction 2010 FAST-M. Heart 2012; 98:699–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hanania G, Cambou JP, Gueret P, et al. Management and in-hospital outcome of patients with acute myocardial infarction admitted to intensive care units at the turn of the century: results from the French nationwide USIC 2000 registry. Heart 2004; 90:1404–1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rogers WJ, Frederick PD, Stoehr E, et al. Trends in presenting characteristics and hospital mortality among patients with ST elevation and non-ST elevation myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J 2008; 156:1026–1034. [DOI] [PubMed] [Google Scholar]
- 35.Chan MY, Sun JL, Newby LK, et al. Long-term mortality of patients undergoing cardiac catheterization for ST-elevation and non-ST-elevation myocardial infarction. Circulation 2009; 119:3110–3117. [DOI] [PubMed] [Google Scholar]
- 36.Darling CE, Fisher KA, McManus DD, et al. Survival after hospital discharge for ST-segment elevation and non-ST-segment elevation acute myocardial infarction: a population-based study. Clin Epidemiol 2013; 5:229–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gupta A, Wang Y, Spertus JA, et al. Trends in acute myocardial infarction in young patients and differences by sex and race, 2001 to 2010. J Am Coll Cardiol 2014; 64:337–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Insam C, Paccaud F, Marques-Vidal P. Trends in hospital discharges, management and in-hospital mortality from acute myocardial infarction in Switzerland between 1998 and 2008. BMC Public Health 2013; 13:270. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


