Abstract
The goal of this study was to determine the incidence of avascular necrosis of the femoral head (AVNFH) after intramedullary nailing of femoral shaft fractures and to identify risk factors for developing AVNFH.
We retrospectively reviewed all patients with femoral shaft fractures treated with antegrade intramedullary nailing at 10 institutions. Among the 703 patients enrolled, 161 patients were excluded leaving 542 patients in the study. Average age was 42.1 years with average follow-up of 26.3 months. Patient characteristics and fracture patterns as well as entry point of femoral nails were identified and the incidence of AVNFH was investigated. Patients were divided into 2 groups according to open versus closed physis, open versus closed fractures, and age (<20 versus ≥20 years).
Overall incidence of AVNFH was 0.2% (1 of 542): the patient was 15-year-old boy. Of 25 patients with open physis, the incidence of AVNFH was 4%, whereas none of 517 patients with closed physis developed AVNFH (P < 0.001). The incidence of AVNFH in patients aged < 20 versus ≥20 years was 1.1% (1 of 93) and 0.0% (0 of 449), respectively (P = 0.172), which meant that the incidence of AVNFH was 0% in adult with femur shaft fracture. Of 61 patients with open fractures, the incidence of AVNFH was 0%. The number of cases with entry point at the trochanteric fossa or tip of the greater trochanter (GT) was 324 and 218, respectively, and the incidence of AVNFH was 0.3% and 0.0%, respectively (P = 0.412).
In patients aged ≥20 years with isolated femoral shaft fracture, there was no case of AVNFH following antegrade intramedullary nailing regardless of the entry point. Therefore, our findings suggest that the risk of AVNFH following antegrade femoral nailing is extremely low in adult patients.
INTRODUCTION
Intramedullary (IM) nailing has been widely used as the gold standard treatment of femur shaft fractures, and many studies have reported excellent results with this technique.1–3 Although the potential complications include angular or rotational malalignment, delayed union, nonunion, and infection, avascular necrosis of the femoral head (AVNFH) after antegrade IM nailing has been reported as a rare complication.4–6 AVNFH after IM nailing is more common in skeletally immature adolescents than in adults.7–13 In skeletally mature patients, we found only 3 cases of AVNFH after IM nailing for femoral shaft fractures.4–6 Few studies have evaluated the epidemiology of AVNFH after femoral IM nailing, especially in adults; therefore, we conducted this retrospective descriptive multicenter study. The goal of this study was to determine the incidence of AVNFH after antegrade IM nailing of femoral shaft fractures and to identify the risk factors for AVNFH.
PATIENTS AND METHODS
The medical records of patients who presented with a femoral shaft fracture from January 2010 to June 2014 were retrospectively obtained from an institutionally approved, multicenter (10 institutions) orthopedic database. The inclusion criterion was treatment of a femoral shaft fracture with an antegrade interlocking IM nail at 1 of the 10 institutions. The exclusion criteria were pathologic fractures, ipsilateral femoral neck fracture, femoral shaft fractures extending to the intertrochanteric or subtrochanteric area, patients taking immunosuppressive agents, divers, and patients with <1 year of follow-up. Reported AVNFH rates of femoral neck fracture combined with ipsilateral femoral shaft fracture vary from 0% to 22% with an average rate of ∼5%,14 so we excluded it. The incidence of AVNFH after trochanter fixation was reported as 1.37% within the first 2 years of injury,15 which could affect the development of AVNFH when femur shaft fracture extended to the intertrochanteric or subtrochanteric area, so we decided to exclude this kind of fractures. Patients were followed clinically and radiographically until fracture union, and then annually. At final follow-up, each patient was evaluated by the treating surgeon. Diagnosis of AVNFH was made a combination of clinical symptoms, plain radiographs, or magnetic resonance imaging (MRI). Radiographs of all patients were reviewed by 2 independent observers, who did not participate in clinical care. Data regarding age, sex, and fracture pattern including open fractures as well as the entry point of the femoral nails were recorded. The reviewed clinical course involved the incidence of AVNFH and the time interval from the surgery to AVNFH.
In total, 703 patients were enrolled. Of these, 161 patients were excluded from the study (Figure 1). Thus, 542 patients (355 men and 187 women) were included in the study. The average patient age was 42.1 years (range, 13–85 years). The average follow-up period was 26.3 months (range, 12–64 months). The patients were divided into 2 groups according to open versus closed physis, age (<20 versus ≥20 years), and open versus closed fractures. We determined physis state assessing proximal and distal femur physis, and closed physis defined as all close of physis of both proximal and distal femur physis. The oldest patient with open physis was 19 years old, so we decided the cutoff point of age at 20 years. The types of nails used in each group of cases were following: 35 cases of Unreamed femoral nail (UFN; Synthes, Oberdorf, Switzerland); 213 cases of Cannulated femoral nail (CFN; Synthes); 17 cases of 4CIS femoral nail (Solco Biomedical, Pyeontaek, Korea), 35 cases of ACE femoral nail (DePuy ACE, Warsaw, IN), 6 cases of DLI femoral nail (U & I, Koyang, Korea), T2 femoral nail (Stryker, Mahwah, NJ), 4 cases of Osteo IC femoral nail (Osteonics, Allendale, NJ), 2 cases of Russel–Taylor femoral nail (Smith & Nephew, Memphis, TN), 37 cases of Sirus femoral nail (Zimmer, Winterthur, Switzerland), 153 cases of Expert Asian femoral nail (A2FN; Synthes), 4 cases of ITST nail (Zimmer), 9 cases of Gamma nail (Stryker), 12 cases of proximal femoral nail anti-rotation (PFNA; Synthes), 3 cases of Cephalomedullary Nail (Zimmer), and 1 case of Miss-A nail (Synthes).
FIGURE 1.
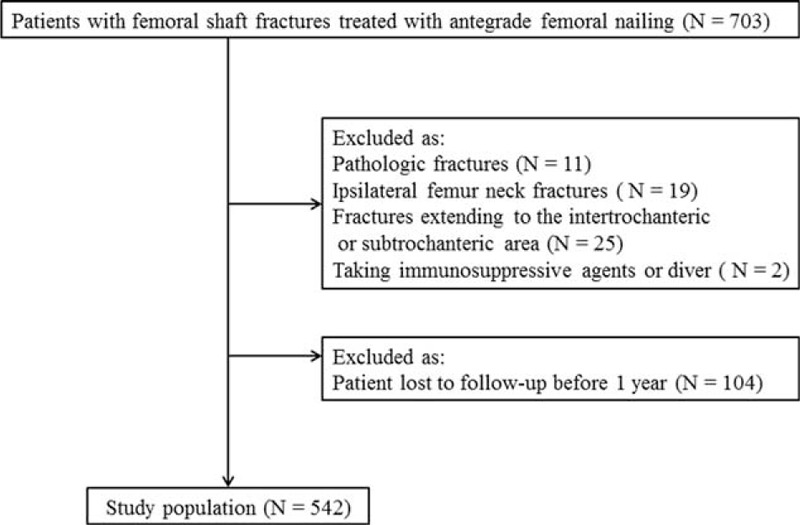
Flowchart demonstrating patient selection, exclusions, and those lost to follow-up.
Statistical Analysis
All statistical analyses were performed using PASW Statistics version 23.0 (IBM Corp., Armonk, NY). Statistical significance was set at P < 0.05. The incidence of AVNFH between the groups was compared using the chi-square test or Fisher's exact test when 1 or more cell of the cells has an expected frequency of 5 or less. Multiple logistic regression (stepwise) models were used to evaluate risk factors associated with AVNFH.
RESULTS
The overall incidence of AVNFH after antegrade IM nailing of femoral shaft fractures was 0.2% (1 of 542 patients): the patient was a 15-year-old boy (Figure 2). However, the incidence of AVNFH after antegrade interlocking IM nailing for in adults was 0%. There were no recorded intraoperative complications. There were 15 cases (2.8%) of nonunion, 2 cases (0.4%) of delayed union, 1 case (0.2%) of infection, and 1 case (0.2%) of peri-implant fracture.
FIGURE 2.
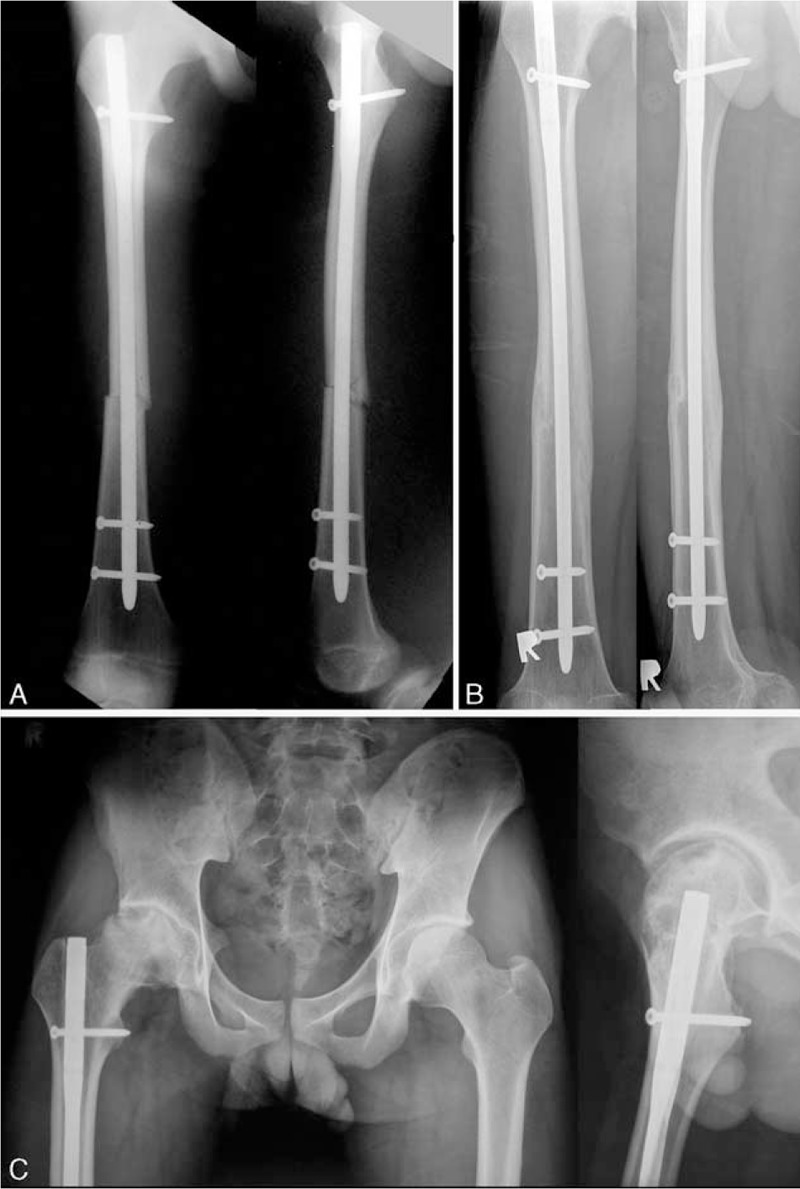
(A) A 15-year-old boy with an isolated closed fracture of the right femoral shaft was treated by antegrade intramedullary nailing with trochanteric fossa insertion. (B) The 14-month postoperative radiographs showed fracture-healing, and the patient was pain-free. (C) Twenty-one months after the injury, radiographs of the right hip showed early collapse of the femoral head that was consistent with avascular necrosis.
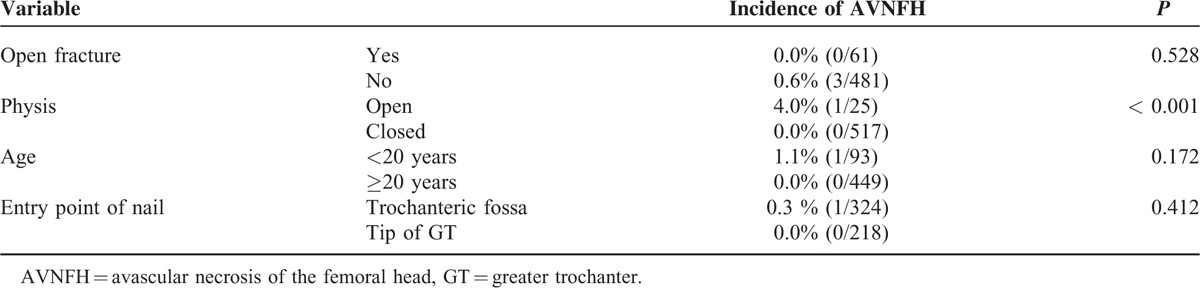
The incidence of AVNFH according to open fracture, open physis, and age is summarized in Table 1. In 25 patients with open physis, the incidence of AVNFH was 4.0%, whereas in 517 patients with closed physis, the incidence of AVNFH was 0.0%; this difference was significant (P < 0.001). The incidence of AVNFH in patients aged <20 versus ≥20 years was 1.1% (1 of 93 patients) and 0.0% (0 of 449 patients), respectively, and this difference was not significant (P = 0.172). In 61 patients with open fractures, the incidence of AVNFH was 0%. The number of cases with an entry point at the trochanteric fossa or the tip of the GT was 324 and 218, respectively, and the incidence of AVNFH was 0.3% and 0%, respectively; this difference was not significant (P = 0.412). The variables including sex, age, open physis, open fracture, and entry point were inappropriate to perform multivariate analysis because the number of outcome events was too small.
TABLE 1.
Incidence of Avascular Necrosis of the Femoral Head According to Open Fracture, Open Physis, Age, and Entry Point of the Nail
DISCUSSION
The present study showed that the overall incidence of AVNFH after femoral IM nailing was 0.2% and that the incidence was 0.0% in adults. In addition, the incidence of AVNFH in the patients with open femoral physis was higher than that with closed physis. Previous reports on AVNFH in adolescents have highlighted the risk of AVNFH after femoral IM nailing, but our results indicate that the risk is very low in adults. Contrary to adults, the incidence of AVNFH after femoral IM nailing in adolescents reportedly ranges from 1.4 to 2.0%;16 our results also showed an incidence of 1.1% in adolescents aged <20 years and 1.5% in patients aged <18 years. A systemic review article including 19 studies of 458 skeletally immature patients showed that the incidence of AVNFH was 2.0% with a trochanteric fossa entry point, 1.4% for an entry point at the tip of the GT, and 0.0% for an entry point lateral to the GT.16 However, our study also demonstrated that AVNFH never occurred in adults, regardless of the entry point. One theory of the etiology of AVNFH after femur IM nailing is vascular injury of the medial femoral circumflex artery (MFCA) and/or the superior retinacular artery during entry to the trochanteric fossa. Dora et al17 found that a trochanteric fossa entry point damaged either the deep branch of the MFCA or its distal superior retinacular artery in 100% of cases (7/7 cadavers) and warned about the risk of AVNFH after femur IM nailing at the trochanteric fossa. The number of reported cases of AVNFH in adults is very limited despite general use of the trochanteric fossa entry point, and none of these studies provide a satisfactory explanation for this discrepancy. A recent cadaver study showed a different result. Schottel et al18 studied the effect of an antegrade femoral IM nail on femoral perfusion and found no obvious damage to the deep MFCA with entry at either the trochanteric fossa or the tip of the GT; additionally, quantitative MRI revealed nearly full femoral head perfusion (95% and 97%, respectively). Therefore, this cadaver study supports our finding that the risk of AVNFH development following antegrade femoral nailing is extremely low in adult patients. In addition, surgeons should pay attention of risk of AVNFH after IM nailing in skeletally immature patients with open femoral physis.
We attempted to explain AVNFH development following antegrade femoral nailing in adults, which were reported in 3 literatures.4–6 The first cadaver study did not use an image intensifier because it was not possible in the dissection room.17 It is not a standard technique, and the surgeons inserted an awl at the entry point by palpation of anatomic landmarks such as the piriformis tendon, which would possibly lead to incorrect positioning. A recent cadaver study found that 40% of trochanteric fossa entry points were within 1 mm of the deep branch of the MFCA, meaning that 1 mm of posteromedial malpositioning can damage the deep branch of the MFCA. In cases of AVNFH in adults, the authors thought the entry point to the trochanteric fossa was more medial and that the large diameter (10 mm) of the proximal nail tip impinged the blood supply of the femoral head; these factors may have jeopardized the vascular supply to the femoral head, leading to AVNFH.4 Therefore, we hypothesize that these vessel injuries could cause AVNFH. Another possible cause of AVNFH seems to be the forceful use of an awl in the wrong direction or multiple entry points, which can injure the blood supply of the femoral head.17
Why AVNFH after femoral IM nailing is relatively more common in adolescents than adults remains unclear. However, we hypothesize that the MFCA injury is more common in adolescents than adults because this injury is seemingly more likely to occur in relatively smaller-sized patients,19,20 and epiphyseal viability is more dependent on the blood supply from the MFCA through the lateral epiphyseal vessels due to the adjacent open physis in the proximal femur.19 In their systematic review of adolescent patients, MacNeil et al16 reported that AVNFH after IM nailing with trochanteric fossa insertion was more frequent than at any other entry point of the tip of the GT or the lateral aspect of the GT (2.0%, 1.4%, and 0.0%, respectively). However, our results showed that the entry point did not matter in terms of development of AVNFH in adults.
This study has several limitations. First, because this study was performed at 10 centers, there may have been multicenter study bias. Although all surgeons were experts, a potential for bias was present because the surgeries were performed in different centers. However, because we performed a standard surgical procedure based on basic fracture repair principles, the potential for bias is expected to be minimal. Another source of bias may have arisen in patient selection. Because this study was performed at Level I trauma centers or tertiary referral hospitals with a significant number of patients with high-energy injuries, this may have subjected the data to selection bias. Finally, the minimal follow-up period of the present study was 12 months, which is not sufficient to determine the occurrence of AVNFH, leading to possible underestimation of the incidence of AVNFH. However, it should be considered that enrolling a large number of patients with a minimum of 24 to 36 months is difficult in clinical situation, and most patients with discomfort tend to revisit their hospital.
Despite these limitations, this study made significant findings that there was no case of AVNFH following antegrade IM nailing regardless of the entry point in our patients aged ≥20 years with an isolated femoral shaft fracture. Therefore, our findings indicate that the risk of AVNFH development following antegrade femoral nailing is extremely low in adult patients, and we believe that antegrade IM nailing is a safe procedure for the femoral shaft fractures.
Footnotes
Abbreviations: AVNFH = avascular necrosis of the femoral head, GT = greater trochanter, IM = intramedullary, MFCA = medial femoral circumflex artery.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Brumback RJ, Uwagie-Ero S, Lakatos RP, et al. Intramedullary nailing of femoral shaft fractures. Part II: fracture-healing with static interlocking fixation. J Bone Joint Surgery Am 1988; 70:1453–1462. [PubMed] [Google Scholar]
- 2.Clawson DK, Smith RF, Hansen ST. Closed intramedullary nailing of the femur. J Bone Joint Surgery Am 1971; 53:681–692. [PubMed] [Google Scholar]
- 3.Winquist RA, Hansen ST, Jr, Clawson DK. Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. J Bone Joint Surgery Am 1984; 66:529–539. [PubMed] [Google Scholar]
- 4.Graves RM, Sands KC. Avascular necrosis of the femoral head following intramedullary nailing of the femur in a skeletally mature young adult: a case report. Am J Orthop 2008; 37:319–322. [PubMed] [Google Scholar]
- 5.Shahane SA, Farhan MJ. Avascular necrosis of the head of femur after intramedullary nailing for fracture of the shaft of the femur. Injury 1996; 27:663–665. [DOI] [PubMed] [Google Scholar]
- 6.Wu CC, Yu CT, Hsieh CP, et al. Femoral head avascular necrosis after interlocking nail of a femoral shaft fracture in a male adult: a case report. Arch Orthop Trauma Surg 2008; 128:399–402. [DOI] [PubMed] [Google Scholar]
- 7.Astion DJ, Wilber JH, Scoles PV. Avascular necrosis of the capital femoral epiphysis after intramedullary nailing for a fracture of the femoral shaft. A case report. J Bone Joint Surgery Am 1995; 77:1092–1094. [DOI] [PubMed] [Google Scholar]
- 8.Beebe KS, Sabharwal S, Behrens F. Femoral shaft fractures: is rigid intramedullary nailing safe for adolescents? Am J Orthop 2006; 35:172–174. [PubMed] [Google Scholar]
- 9.Buckaloo JM, Iwinski HJ, Bertrand SL. Avascular necrosis of the femoral head after intramedullary nailing of a femoral shaft fracture in a male adolescent. J South Orthop Assoc 1997; 6:97–100. [PubMed] [Google Scholar]
- 10.Krikler SJ. Avascular necrosis of the capital femoral epiphysis after intramedullary nailing for a fracture of the femoral shaft. A case report. J Bone Joint Surgery Am 1996; 78:793–794. [PubMed] [Google Scholar]
- 11.Mileski RA, Garvin KL, Crosby LA. Avascular necrosis of the femoral head in an adolescent following intramedullary nailing of the femur. A case report. J Bone Joint Surgery Am 1994; 76:1706–1708. [DOI] [PubMed] [Google Scholar]
- 12.O’Malley DE, Mazur JM, Cummings RJ. Femoral head avascular necrosis associated with intramedullary nailing in an adolescent. J Pediatr Orthop 1995; 15:21–23. [DOI] [PubMed] [Google Scholar]
- 13.Thometz JG, Lamdan R. Osteonecrosis of the femoral head after intramedullary nailing of a fracture of the femoral shaft in an adolescent. A case report. J Bone Joint Surgery Am 1995; 77:1423–1426. [DOI] [PubMed] [Google Scholar]
- 14.Boulton CL, Pollak AN. Special topic: ipsilateral femoral neck and shaft fractures—does evidence give us the answer? Injury 2015; 46:478–483. [DOI] [PubMed] [Google Scholar]
- 15.Barquet A, Mayora G, Guimaraes JM, et al. Avascular necrosis of the femoral head following trochanteric fractures in adults: a systematic review. Injury 2014; 45:1848–1858. [DOI] [PubMed] [Google Scholar]
- 16.MacNeil JA, Francis A, El-Hawary R. A systematic review of rigid, locked, intramedullary nail insertion sites and avascular necrosis of the femoral head in the skeletally immature. J Pediatr Orthop 2011; 31:377–380. [DOI] [PubMed] [Google Scholar]
- 17.Dora C, Leunig M, Beck M, et al. Entry point soft tissue damage in antegrade femoral nailing: a cadaver study. J Orthop Trauma 2001; 15:488–493. [DOI] [PubMed] [Google Scholar]
- 18.Schottel PC, Hinds RM, Lazaro LE, et al. The effect of antegrade femoral nailing on femoral head perfusion: a comparison of piriformis fossa and trochanteric entry points. Arch Orthop Trauma Surg 2015; 135:473–480. [DOI] [PubMed] [Google Scholar]
- 19.Gautier E, Ganz K, Krugel N, et al. Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surgery Am 2000; 82:679–683. [DOI] [PubMed] [Google Scholar]
- 20.Gordon JE, Khanna N, Luhmann SJ, et al. Intramedullary nailing of femoral fractures in children through the lateral aspect of the greater trochanter using a modified rigid humeral intramedullary nail: preliminary results of a new technique in 15 children. J Orthop Trauma 2004; 18:416–422. [DOI] [PubMed] [Google Scholar]


