ABSTRACT
One strategy for reducing the primary cesarean surgery rate and length of labor is using a peanut-shaped exercise ball for women laboring under epidural analgesia. A randomized, controlled study was conducted to determine whether use of a “peanut ball” decreased length of labor and increased the rate of vaginal birth. Women who used the peanut ball (n = 107) versus those who did not (n = 91) demonstrated shorter first stage labor by 29 min (p = .053) and second stage labor by 11 min (p < .001). The intervention was associated with a significantly lower incidence of cesarean surgery (OR = 0.41, p = .04). The peanut ball is potentially a successful nursing intervention to help progress labor and support vaginal birth for women laboring under epidural analgesia.
Keywords: peanut ball, epidural, first stage labor, second stage labor, cesarean birth
Cesarean surgery is often perceived as benign, but the surgery can place the woman at an increased risk of infection, hemorrhage, damage to abdominal and urinary tract organs, longer recovery, and complications from anesthesia. In 2010, the U.S. cesarean rate was at 32.8% (Martin, Hamilton, Ventura, Osterman, & Matthews, 2013), a drastic increase from the initial and ideal rate of 4.5% when it was first measured in 1965 (Taffel, Placek, & Liss, 1987). Organizations have begun assuming responsibility for limiting elective inductions, recognizing that the best outcomes overall for both the mother and the infant occur in facilities with cesarean surgery rates in the 5%–10% range (Althabe & Belizán, 2006). The Healthy People 2020 cesarean surgery rate target is 23.9% for low-risk full-term women with a singleton, vertex presentation (U.S. Department of Health and Human Services, 2013). As a result, efforts by the Association of Women’s Health, Obstetrics, and Neonatal Nursing Association (AWHONN), the American College of Obstetrics and Gynecology (ACOG), and March of Dimes discourage pregnant women from requesting an elective induction when not medically indicated.
Labor that fails to progress is the most common indication for primary cesarean surgery (Gifford et al., 2000). In low-risk nulliparous women, the use of epidural analgesia for labor pain was associated with higher risks of emergency cesarean surgery and vacuum-assisted birth (Eriksen, Nohr, & Kjærgaard, 2011). Epidural analgesia influences the course of labor and birth, and there is an increase in instrumental birth (forceps or vacuum), fetal malposition, a longer second stage labor, and fetal distress when compared with women who receive intravenous opiates (American College of Obstetricians and Gynecologists, 2002; Anim-Somuah, Smyth, & Jones, 2011; Lieberman & O’Donoghue, 2002).
Practitioners have reported in the literature that use of an exercise ball at the bedside of laboring women without an epidural can facilitate a more normal labor progression (Gau, Chang, Tian, & Lin, 2011; Johnston, 1997; Zwelling, 2010). The ball promotes spinal flexion, increasing the uterospinal angle, and increasing the pelvic diameters to facilitate occiput posterior rotation (Zwelling, 2010), which results in a widened pelvic outlet. In general, exercise/birthing balls widen the pelvic inlet and outlet dimensions passively stretching the adductor magnus muscles, resulting in the widening of the intertuberous diameter (Shermer & Raines, 1997). Using a peanut ball with women who have received an epidural is gaining popularity with labor and birth professionals, but there is limited evidence to support its use. Therefore, a research study was designed, based on pilot data, to explore the differences in labor time and spontaneous vaginal birth between women laboring with an epidural who use a peanut-shaped exercise ball compared to those who do not use a ball.
REVIEW OF LITERATURE
In 2008, a study in 27 states showed that 61% of singleton births were to women who received an epidural or spinal anesthesia during labor (Osterman & Martin, 2011). Although generally accepted as safe and a normal part of any birth, labor epidurals have a wide range of potential complications. In three systematic reviews and a prospective study, epidural analgesia was associated with an increased requirement of oxytocin augmentation, prolonged second stage, and instrumental births (Anim-Somuah et al., 2011; Caruselli et al., 2011; Leighton & Halpern, 2002; Lieberman & O’Donoghue, 2002). Other researchers found an increased cesarean surgery rate, prolonged time in labor, more instrumental births, and use of pharmacologic agents to augment labor (American College of Obstetricians and Gynecologists, 2002; Anim-Somuah et al., 2011; Eriksen et al., 2011). A meta-analysis concluded that epidural use is associated with prolonging labor 40–90 min and with an increased risk of second stage of labor that extended beyond 2 hr (American College of Obstetricians and Gynecologists, 2002; Sharma, McIntire, Wiley, & Leveno, 2004).
Association of Women’s Health, Obstetrics and Neonatal Nurses, the American College of Obstetricians and Gynecologists, and the March of Dimes discourage pregnant women from requesting an elective induction when not medically indicated.
Prolonging Labor
Preventing the first cesarean surgery requires allowing adequate time for first and second stages of labor, as long as no maternal and fetal distress occurs. The likelihood of vaginal birth is lower after elective labor induction than after spontaneous labor, especially when the induction is attempted on a nulliparous woman with an unripened/unfavorable cervix or low bishop score (Maslow & Sweeny, 2000; van Gemund, Hardeman, Scherjon, & Kanhai, 2003). Induction of labor reportedly increased from 9.5% of births in 1990 to 23.2% of births in 2011 (Martin et al., 2013). The diagnosis of “failed induction” or “failure to progress” should be made only after an adequate attempt (Spong, Berghella, Wenstrom, Mercer, & Saade, 2012). Adequate time for first and second stage labor is longer than traditionally estimated (Zhang et al., 2010). Spong et al. (2012) defines second stage arrest as no progress (descent or rotation) for more than 4 hr in a nullipara with an epidural and more than 3 hr in multiparous women with an epidural. A major concern with unanticipated prolonged labor is the potential need for further medical intervention.
Additional Birth Interventions
In addition to prolonged labor, epidural use is associated with additional birth interventions, such as a higher rate of operative instrumental births (Anim-Somuah et al., 2011; Leighton & Halpern, 2002; Lieberman & O’Donoghue, 2002). An increased risk of instrumental births has been reported in nulliparous women using epidural analgesia in comparison to other forms of pain relief (Comparative Obstetric Mobile Epidural Trial Study Group, 2001). The risk of vacuum birth was more than doubled among the women who had epidural analgesia (Anim-Somuah et al., 2011). Instrumental vaginal births are associated with increased maternal risks, such as vaginal and perineal trauma and anal sphincter damage, resulting in urinary incontinence, bowel and sexual problems, and dyspareunia (Eason, Labrecque, Wells, & Feldman, 2000; Ekeus, Nilsson, & Gottvall, 2008; Groutz et al., 2011). In addition, instrument-assisted vaginal births can be associated with adverse events in infants, such as caput succedaneum or cephalhematoma, or skull fractures with vacuum-assisted births (Simonson et al., 2007).
Widening the Pelvic Outlet
Gifford et al. (2000) reported that lack of progress in labor was the reason for 68% of unplanned cesarean surgeries for cephalic-presenting fetuses. Widening the pelvic outlet is one method of supporting the natural progression of birth. When a woman is leaning forward while on her side, the contractions direct the fetus toward the larger posterior half of the pelvic inlet, where the fetus has more room to flex, rotate, and descend (Biancuzzo, 1993; Fenwick & Simkin, 1987). Although many factors can contribute to the protraction and arrest of labor, including weakened contractions, fetal alignment, or maternal pelvic size (Ehsanipoor & Satin, 2012), using position changes to widen the pelvic outlet can be beneficial.
NURSE-DRIVEN PEANUT BALL INTERVENTION
There are multiple benefits associated with maternal position changes, including decreased pain, increased maternal–fetal circulation, improved quality of uterine contractions, decreased length of labor, and facilitation of fetal descent (Zwelling, 2010). A laboring woman with an epidural is limited in the number of different positions she can try.
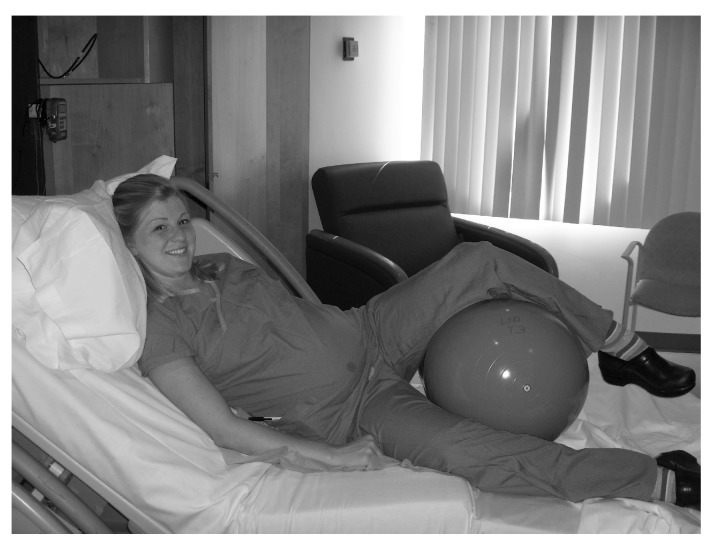
Midwives were the first to use a round exercise ball as a nonpharmacological means to facilitate progression of labor. The ball is believed to enhance labor by optimally positioning the fetus in relation to the pelvis (Johnston, 1997). A “peanut ball” is shaped like a peanut shell, where the middle circumference is smaller than the ends. To facilitate the desired upright position for successful labor progression, a peanut ball could be placed between a woman’s legs while she is limited to staying in bed (Figure 1). The ball is supported in place with a pillow behind the woman’s hips to support the woman’s legs.
FIGURE 1.
A nurse demonstrates a side-lying position with the peanut ball placed between her legs.
A “peanut ball” is shaped like a peanut shell, where the middle circumference is smaller than the ends.
Based on previous knowledge of maternal position changes, it was hypothesized that the simple placement of the peanut ball between a laboring woman’s legs could increase pelvic diameter and allow more room for fetal descent. Although the peanut ball is currently used in labor and birth units, little research exists to support its effectiveness in improving labor outcomes. In an effort to explore the effectiveness of using a peanut ball for laboring women with an epidural, a nurse-led study was designed to compare the length of labor and mode of birth in a controlled, randomized study with two groups: women who used a peanut ball compared to those who did not use a peanut ball.
METHODS
Design and Setting
A two-group controlled, randomized study was conducted to test the effectiveness of the peanut ball intervention related to shorter labor time and improved rates of spontaneous vaginal birth. The study was given full review and approved by the hospital’s institutional review board.
The study was conducted at a large, nonprofit, inner-city teaching hospital in the Southwestern United States from January 2009 to January 2010. The labor and birth unit consisted of 20 labor and birth rooms staffed by registered nurses that maintained a 2:1 or less patient ratio. The unit’s standard of care for continuous electronic fetal monitoring laboring patients with an epidural followed American College of Obstetricians and Gynecologists and AWHONN guidelines, including an assessment of maternal uterine and fetal status every 15-30 min and every time the oxytocin was adjusted. The patient was assisted with turning or changing their position and adjusting the peanut ball every 1–2 hours after receiving the epidural. All anesthesiologists in the study hospital belong to the same physician practice group and use a standard protocol for epidural dosing. Prior to the study, the facility was experiencing a 67.9% epidural rate and 32.5% cesarean surgery rate.
Participants
Laboring women were recruited if they met the inclusion criteria, which included being in active labor, using an epidural for pain control, and with the fetus in the cephalic presentation. Women who had an indication for either elective induction or augmentation of labor, such as mild preeclampsia, possible macrosomia, or patient request, were eligible for inclusion. Women younger than the age of 18 years were included with parental consent. Women were excluded if they required magnesium sulfate for preeclampsia, had signs of an intrauterine infection, or had a Category 3 fetal heart rate tracing, indicating the fetus may be hypoxia or acidotic.
Power Analysis
To determine the number of participants needed in each group, data from an internal pilot study were used to calculate power. A small group of nonrandomized laboring women with an epidural who used a peanut ball (n = 30) were compared to those who did not (n = 22). Lengths of first and second stage labor were recorded. Results demonstrated a 46-min reduction in first stage labor and an 11-min reduction in second stage labor with women who used the peanut ball. It was determined that 90 subjects in each group would provide a power of .80 at an alpha of .05. To account for dropouts, a sample size of 100 subjects per group was planned.
Subject Recruitment
Potential study participants were identified and approached after they received an epidural. The principal researcher or research assistant recruited and obtained written informed consent using the participant’s primary language (English or Spanish). Participants were randomly assigned to either the intervention or control group in a 1:1 ratio using randomized blocks of varying sizes from an online randomization plan generator. Participant assignments were placed in sealed, sequentially numbered opaque envelopes by a person not involved with the study. Each allocation was revealed once an eligible participant completed the informed consent process.
Intervention
There were peanut balls on the unit and available to be used for the study in each labor and birth room. Each peanut ball was made of durable, nonlatex material and was covered with a large plastic bag. A patient gown was tied around the ball to prevent discomfort from the plastic resting against the woman’s legs. The balls were thoroughly cleaned using antiseptic techniques between each patient use.
Registered nurses were educated by the investigators on the study protocol, and standard care was given to both the intervention and control groups. Standard care involved turning patients from side to side or placing the woman in semi- or high-Fowler position every 1–2 hr. No other restrictions were placed on the patient as part of the study protocol.
The peanut ball was placed between the legs of a woman in the intervention group immediately after she received her epidural and consented to participate in the study. The ball was removed when the cervix of the woman became completely effaced and dilated, passive descent had occurred, and she was ready to actively push. Demographic data were collected orally from all participants by the investigators in their preferred language of English or Spanish. Women were asked their age, gravidity, parity, ethnicity, estimated date of birth, and whether or not they had been diagnosed with diabetes. The cervical dilation, effacement, and station were recorded from their vaginal exam (usually 30–60 min prior) before epidural placement. After birth, nuchal cord occurrence, Apgar scores, and fetal weight were recorded. In addition, data on whether the participant was induced, received oxytocin augmentation, had forceps or vacuum intervention, gave birth vaginally or via cesarean, and the length of first and second stages of labor was collected.
The main outcome measures of the study were length of labor and mode of birth (spontaneous vaginal or cesarean surgery). The length of first stage labor time was recorded from placement of the peanut ball to full effacement, station, dilation, and birth (length of first stage of labor is from placement of the peanut ball to 100% effacement and 10 cm dilation). The length of second stage labor time was recorded from complete cervical dilation to expulsion of the fetus (Cunningham et al., 2010). The mode of birth was recorded as spontaneous vaginal or cesarean surgery. The use of any interventional devices, such as vacuum or forceps, or pharmacological interventions, such as oxytocin, was documented.
Data Analysis
Data were analyzed using SPSS Version 17.0. Descriptive statistics of the two groups were analyzed and compared. Outcome measures were compared between the groups using independent t tests and Fisher exact tests, as appropriate. Linear and logistic regression modeling was conducted to determine the effect of the peanut ball on first and second stage labor time and spontaneous birth, controlling for independent significant predictors.
RESULTS
Between January 2009 and January 2010, 200 women were randomly assigned to either the peanut ball (n = 107) or control group (n = 94). Most participant demographics were statistically similar between the groups (Table 1); however, it was noted that the women’s parity and cervical dilation were significantly different between the two groups, and further post hoc analysis was completed to statistically control for the difference. No complications were reported from the use of the peanut ball intervention and no differences in Apgar scores occurred in either group during the study. In addition, no neonatal or maternal deaths occurred in either group.
TABLE 1. Maternal Demographic Characteristics in Control and Intervention Groups.
| Characteristic | Peanut Ball Group (n = 107) | Control Group (n = 94) |
| Age, M (SD) | 27.5 (6.7) | 27.3 (6.2) |
| Average gravidity, median | 2.0 | 2.0 |
| Parity,a median | 1.0 | 0.0 |
| Nulliparity,a % | 47.7 | 59.6 |
| White ethnicity, % | 43.9 | 35.5 |
| Hispanic ethnicity,% | 43.0 | 46.2 |
| Estimated date of birth in weeks, M (SD) | 38.9 (2.4) | 39.1 (2.5) |
| Diabetic, % | 4.8 | 4.4 |
| Cervical dilationa (in centimeters) at enrollment, median | 4.5 | 4.0 |
| Effacement at enrollment, % | 84.2 | 77.7 |
| Station at enrollment, median | −1.0 | −1.0 |
Note. Gravidity defined as number of pregnancies; parity defined as number of births; nulliparity defined as never given birth.
aSignificant p < .05.
Significant unadjusted differences were found in comparing length of labor and mode of birth between the two groups (Table 2). Women in the peanut ball group had a significantly shorter first stage labor time than those in the control group (p < .01). Second stage labor was also significantly shorter in the peanut ball group than in the control group (p < .001). The percentage of labors that resulted in cesarean surgery was statistically higher in the control group. Twenty-one percent (n = 19) of women assigned to the control group had cesarean surgery compared to 10% (n = 11) of the intervention group (p < .05). No significant differences were found between the groups in the use of pharmacological intervention (induction or augmentation by oxytocin use) and instrumental intervention (forceps or vacuum use).
TABLE 2. Labor and Birth Outcomes.
| Outcome | Peanut Ball Group (n = 107) | Control Group (n = 94) | Statistic | p Value |
| Length of first stage labora (min) | 268.8 (228.1–309.6) | 356.2 (308.8–403.6) | t test | .006 |
| Length of second stage labora (min) | 21.3 (16.3–26.3) | 43.5 (32.3–54.8) | t test | <.001 |
| Cesarean surgeryb | 11 (10.3) | 19 (21.1) | χ2 | .011 |
| Inductionb | 30 (28.0) | 29 (31.5) | χ2 | .592 |
| Oxytocin usedb | 85 (79.3) | 74 (79.8) | χ2 | .925 |
| Forceps usedb | 2 (1.9) | 2 (2.2) | χ2 | .895 |
| Vacuum usedb | 7 (6.7) | 9 (9.7) | χ2 | .438 |
| Nuchal cord presentb | 18 (17.5) | 19 (21.1) | χ2 | .522 |
| Apgar score at 1 minc | 9 (8–9) | 9 (8–9) | Wilcoxon test | .926 |
| Apgar score at 10 minc | 9 (9–9) | 9 (9–9) | Wilcoxon test | .529 |
| Fetal weight in gramsa | 3,456 (3,369–3,544) | 3,393 (3,264–3,521) | Wilcoxon test | .337 |
aReported as M, (95% CI).
bReported as n, (%).
cReported as median, (25th–75th interquartile range).
Multiple regression analysis was used to determine independent predictors of first stage length of labor, second stage length of labor, and spontaneous vaginal birth. Univariate analysis was conducted on each outcome with all predictors. Predictors with a p < .10 were selected to be entered into regression models (Table 3). Because significant differences were found in nulliparity and cervical dilation between the groups, both predictors were entered into each regression model and a stepwise method was used to determine the final models. The final models contained only those predictors that remained in the model with a p < .05.
TABLE 3. Univariate Analysis of Predictors of Outcomes.
| Variable | p |
| First stage labor | |
| Age | .027 |
| Gravidity | .047 |
| Parity | .001 |
| Oxytocin | .062 |
| Nulliparity | <.001 |
| Cervical dilation | <.001 |
| Effacement | <.001 |
| Peanut ball | .001 |
| Second stage labor | |
| Gravidity | <.001 |
| Parity | <.001 |
| Nulliparity | <.001 |
| Peanut ball | <.001 |
| Cesarean surgery | |
| Gravidity | .009 |
| Parity | <.001 |
| Nulliparity | <.001 |
| Dilation | <.001 |
| Peanut ball | .011 |
Note. Gravidity = defined as number of pregnancies; parity = defined as number of births; nulliparity = defined as never given birth.
Linear regression models were used to determine significant predictors, including use of the peanut ball, on the length of first and second stage labor, and logistic regression modeling was conducted for the cesarean surgery outcome (Table 4). Linear regression models revealed that time of the first stage of labor was significantly independently predicted by maternal age, nulliparity, and cervical dilation. In this model, when controlling for these significant predictors of length of first stage labor, the peanut ball approached significance (p = .053). Use of the peanut ball would decrease the first stage of labor by 29 min, which could be considered a clinically significant result. In a model assessing second stage labor, use of the peanut ball was the only significant predictor, decreasing labor time by 11 min (p < .001). In a model assessing mode of birth, adjusting for nulliparity, women in the peanut ball group were less than half as likely (OR = 0.41, p = .04) to undergo cesarean surgery.
TABLE 4. Regression Models for Length of First and Second Stage Labor and Cesarean Surgery.
| First Stage Labor | Coefficient | p |
| Maternal age (for each year increase) | 5.83 | .011 |
| Cervical dilation (for each cm increase) | −30.80 | <.001 |
| Nulliparous (yes vs. no) | 58.20 | <.001 |
| Use of peanut ball (yes vs. no) | −28.60 | .053 |
| Second Stage Labor (min) | Coefficient | p |
| Use of peanut ball (yes vs. no) | −11.10 | <.001 |
| Cesarean Surgery | Odds Ratio | p |
| Nulliparous (yes vs. no) | 8.00 | <.001 |
| Use of peanut ball (yes vs. no) | 0.41 | .035 |
DISCUSSION
The purpose of this study was to compare labor times and mode of birth between laboring women with an epidural who used a peanut ball and those who did not. Results showed that women using the peanut ball during labor had a significantly shorter length of second stage labor. In addition, the cesarean rate for those that used the peanut ball was statistically lower than those women who did not use the peanut ball. Pharmacologic (induction and augmentation) and instrument (forceps and vacuum) intervention were lower in the peanut ball intervention group, but the difference was not statistically significant. Although randomization resulted in differences in the parity and cervical dilation between the two groups, additional analyses showed that the peanut ball is still a significant predictor for nulliparous women for length of second stage of labor and vaginal birth and approached significance for first stage labor length.
Because limited research is available on the use of exercise or peanut balls with women with an epidural, the research question was generated from a growing trend in hospital labor and birth units to use such balls. Epidural analgesia relaxes the pelvic floor muscles, which may delay the rotation of the fetal head, engender a weakened desire to push because of diminution of the bearing down reflex, and reduce uterine activity (Mayberry et al., 1999). Lieberman & O’Donoghue (2002) found that epidural analgesia was associated with persistent occiput posterior position at birth, which plays a role with increasing risk of operative birth. The duration of the active phase of labor before 6 cm dilation is longer in women undergoing induction (Zhang, Troendle, & Yancey, 2002). Most inductions are performed on patients before 6 cm, and in this study, 4 cm was the median exam at the time the epidural was received. In addition, upright positioning in combination with the peanut ball can potentially optimize gravity and pelvic widening; when the woman leans forward in a “C-curve” position, the sacrum and coccyx are free to move back, thus increasing the anterior-posterior diameter of the pelvis (Zwelling, 2010).
Although the sample size was small and not all potential confounders were measured, findings suggest that the peanut ball can be an effective clinical intervention in saving time pushing and reducing the cesarean surgery rate, particularly in women who have not previously had children. In both the peanut ball and control group, the primary reason for cesarean surgery in the study included diagnosis of failure to progress or fetal intolerance to labor. Because 90% of cesarean surgeries result in subsequent repeat cesareans for future births (Spong et al., 2012), the peanut ball can be particularly useful in helping nulliparous women avoid a primary cesarean.
Despite randomization, some demographic characteristics were unequally distributed and influential in the length of labor or outcome, and additional analysis was needed to assess the peanut ball intervention controlling for their effects. As an exploratory study into the effectiveness of the peanut ball, it is evident that future research should assess the many more potential confounders for failure of labor to progress. For example, recent research on obesity and birth outcomes has demonstrated that obese nulliparous women undergoing labor induction were at increased risk for increased labor time and cesarean surgery (Green & Shaker, 2011; Nuthalapaty, Rouse, & Owen, 2004). Studies assessing the use of the peanut ball in a high-risk group would be useful in determining its effectiveness.
The peanut ball was well received by patients, who expressed satisfaction with a noninvasive, nonpharmacologic intervention that did not cause discomfort and could potentially prevent complications. After completion of the study, a practice change was implemented to offer all laboring women with an epidural the use of a peanut ball, and providers and staff readily adopted the change.
The peanut ball was well received by patients, who expressed satisfaction with a noninvasive, nonpharmacologic intervention that did not cause discomfort and could potentially prevent complications.
Limitations
The study was limited to a single facility in the Southwest. Although the study measured specific labor outcomes, it did not control for all factors that could potentially influence these outcomes. Practice variation with physicians and nurses was not tightly controlled; that is, patients and practitioners were still given the option of when to actively push based on patient’s desire, fetal heart rate tracing, and physician’s order. Additional analysis was needed to control for differences between the groups. The study did not monitor the total length of time a woman sat in an upright position (head of bed up greater than 45°) versus women in a recumbent position; however, there is insufficient data on which position for practitioners to recommend for second stage labor for women with an epidural (Kemp, Kingswood, Kibuka, & Thornton, 2013). In future studies, cervical dilation at time of placement of the epidural and multiparity should be controlled/randomly assigned to the intervention and control groups.
A potential benefit was found in using this nonpharmacologic intervention to improve the likelihood of a woman having progression of labor, a vaginal birth, and reducing complications during childbirth. However, any intervention to progress labor should be used with caution for women who require Group B streptococcal prophylaxis because antibiotic infusion is recommended to be administered at least 4 hr prior to birth (Centers for Disease Control and Prevention, 2013).
Implications for Practice and Recommendations for Future Research
The findings from this study demonstrate the potential of the peanut ball to reduce length of labor and promote spontaneous vaginal birth. Future research should address the effectiveness of the peanut ball with a larger sample controlling for more potential confounders. However, as a low-risk, low-cost nursing intervention, the peanut ball can be introduced to women to promote positive labor outcomes. Integration of the use of a peanut ball can begin with childbirth educators demonstrating the peanut ball to participants of childbirth classes; nurses in labor and birth units can include the peanut ball use in basic labor management classes in nursing orientation. The peanut ball has the potential to help decrease the length of second stage labor and provide a successful vaginal birth. Of U.S. women who require a primary cesarean surgery, more than 90% will have a subsequent repeat cesarean. The peanut ball provides an option for reducing the risks associated the primary cesarean surgery and implications for subsequent pregnancies.
CONCLUSION
This study provides evidence that laboring women with an epidural who use a peanut-shaped exercise ball, compared to women who did not, had significantly shorter length of labor and a higher likelihood of spontaneous vaginal birth. In addition, no harmful effects were identified to the mother or the fetus/newborn. The researchers think that these changes are likely attributed to the potential opening of the pelvic outlet; however, more research is needed on the peanut ball as a nonpharmacologic intervention.
The study hospital, which is part of a larger health system, implemented the use of the peanut ball to all laboring women with an epidural after the study was completed. In conjunction with other efforts, the hospital’s outcomes resulted in system-wide implementation of the peanut ball in all labor and birth units.
Biographies
CHRISTINA MARIE TUSSEY is a women and infant service clinical nurse specialist. She leads patient care initiatives, research, evidence-based practice changes, and program development.
EMILY BOTSIOS is a labor and delivery nurse, a nursery nurse, and an adjunct instructor for nursing. She uses complementary therapies in her practice and supports multiple modalities for progression of labor.
RICHARD D. GERKIN is a physician and biostatistician with an extensive background in supporting clinical research for residents and nurses.
LESLY A. KELLY is a hospital-based nurse researcher and university assistant professor. She is skilled in health services research.
JUANA GAMEZ is a bilingual labor and delivery nurse who supports the translation of research for the Spanish-speaking population.
JENNIFER MENSIK is the past system director of clinical practice and has an extensive background in nursing administration.
REFERENCES
- Althabe F., Belizán J. M. (2006). Caesarean section: The paradox. Lancet, 368(9546), 1472–1473. [DOI] [PubMed] [Google Scholar]
- American College of Obstetricians and Gynecologists (2002). ACOG practice bulletin. Obstetric analgesia and anesthesia. Number 36, July 2002. International Journal of Gynaecology & Obstetrics, 78(3), 321–335. [DOI] [PubMed] [Google Scholar]
- Anim-Somuah M., Smyth R. M., Jones L. (2011). Epidural versus non-epidural or no analgesia in labour. Cochrane Database of Systematic Reviews, (12), CD000331. [DOI] [PubMed] [Google Scholar]
- Biancuzzo M. (1993). Six myths of maternal posture during labor. MCN, the American Journal of Maternal Child Nursing, 18(5), 264–269. [PubMed] [Google Scholar]
- Caruselli M., Camilletti G., Torino G., Pizzi S., Amici M., Piattellini G., Pagni R. (2011). Epidural analgesia during labor and incidence of cesarean section: Prospective study. The Journal of Maternal-Fetal & Neonatal Medicine, 24(2), 250–252. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2013). 2010 guidelines for the prevention of perinatal group B streptococcal disease. Retrieved from http://www.cdc.gov/groupbstrep/guidelines/guidelines.html
- Comparative Obstetric Mobile Epidural Trial Study Group (2001). Effect of low-dose mobile versus traditional epidural techniques on mode of delivery: A randomised controlled trial. Lancet, 358(9275), 19–23. [DOI] [PubMed] [Google Scholar]
- Cunningham G. F., Leveno K. J., Bloom S. L., Hauth J. C., Rouse D. J., Spong C. Y. (2010). Williams obstetrics (23rd ed.). New York, NY: McGraw-Hill. [Google Scholar]
- Eason E., Labrecque M., Wells G., Feldman P. (2000). Preventing perineal trauma during childbirth: A systematic review. Obstetrics and Gynecology, 95(3), 464–471. [DOI] [PubMed] [Google Scholar]
- Ehsanipoor R. M., Satin A. (2012). Abnormal labor: Protraction and arrest disorders. Retrieved from http://www.uptodate.com/contents/overview-of-normal-labor-and-protraction-and-arrest-disorders
- Ekeus C., Nilsson E., Gottvall K. (2008). Increasing incidence of anal sphincter tears among primiparas in Sweden: A population-based register study. Acta Obstetrics Gynecology Scandinavia, 87, 564–573. [DOI] [PubMed] [Google Scholar]
- Eriksen L., Nohr E. A., Kjærgaard H. (2011). Mode of delivery after epidural analgesia in a cohort of low-risk nulliparas. Birth, 38(4), 317–326. [DOI] [PubMed] [Google Scholar]
- Fenwick L., Simkin P. (1987). Maternal positioning to prevent or alleviate dystocia in labor. Clinical Obstetrics and Gynecology, 30(1), 83–89. [DOI] [PubMed] [Google Scholar]
- Gau M., Chang C., Tian S., Lin K. (2011). Effects of birth ball exercise on pain and self-efficacy during childbirth: A randomised controlled trial in Taiwan. Midwifery, 27(6), e293–e300. [DOI] [PubMed] [Google Scholar]
- Gifford D. S., Morton S. C., Fiske M., Keesey J., Keeler E., Kahn K. L. (2000). Lack of progress in labor as a reason for cesarean. Obstetrics and Gynecology, 95(4), 589–595. [DOI] [PubMed] [Google Scholar]
- Green C., Shaker D. (2011). Impact of morbid obesity on the mode of delivery and obstetric outcome in nulliparous singleton pregnancy and the implications for rural maternity services. The Australian & New Zealand Journal of Obstetrics & Gynaecology, 51(2), 172–174. [DOI] [PubMed] [Google Scholar]
- Groutz A., Cohen A., Gold R., Hasson J., Wengier A., Lessing J. B., Gordon D. (2011). Risk factors for severe perineal injury during childbirth: A case-control study of 60 consecutive cases. Colorectal Disease, 13(8), e216–219. [DOI] [PubMed] [Google Scholar]
- Johnston J. (1997). Birth balls. Midwifery Today With International Midwife, (43), 59–67. [PubMed] [Google Scholar]
- Kemp E., Kingswood C. J., Kibuka M., Thornton J. G. (2013). Position in the second stage of labour for women with epidural anaesthesia. The Cochrane Database of Systematic Reviews, (1), CD008070. [DOI] [PubMed] [Google Scholar]
- Leighton B. L., Halpern S. H. (2002). The effects of epidural analgesia on labor, maternal, and neonatal outcomes: A systematic review. American Journal of Obstetrics and Gynecology, 186(5, Suppl), S69–S77. 10.1016/S0002-9378(02)70182-8 [DOI] [PubMed] [Google Scholar]
- Lieberman E., O’Donoghue C. (2002). Unintended effects of epidural analgesia during labor: A systematic review. American Journal of Obstetrics and Gynecology, 186(5, Suppl. Nature), S31–S68. [DOI] [PubMed] [Google Scholar]
- Martin J. A., Hamilton B. E., Ventura S., Osterman M. J., Mathews T. J. (2013). Births: Final data for 2011. National Vital Statistics Reports, 62(1). Retrieved from http://www.cdc.gov/nchs/data/nvsr/nvsr62/nvsr62_01.pdf [PubMed] [Google Scholar]
- Maslow A. S., Sweeny A. L. (2000). Elective induction of labor as a risk factor for cesarean delivery among low-risk women at term. Obstetrics and Gynecology, 95(6, Pt. 1), 917–922. [DOI] [PubMed] [Google Scholar]
- Mayberry L. J., Wood S. H., Strange L. B., Flee L., Heisler D. R., Neilsen-Smith K. (1999). Managing second-stage labor. AWHONN Lifelines, 3(6), 28–34. [DOI] [PubMed] [Google Scholar]
- Nuthalapaty F., Rouse D., Owen J. (2004). The association of maternal weight with cesarean risk, labor duration, and cervical dilatation rate during labor induction. American College of Obstetricians and Gynecologists, 103, 452–456. [DOI] [PubMed] [Google Scholar]
- Osterman M. J., Martin J. A. (2011). Epidural and spinal anesthesia use during labor: 27-state reporting area, 2008. National Vital Statistics Reports, 59(5), 1–13, 16. [PubMed] [Google Scholar]
- Sharma S., McIntire D., Wiley J., Leveno K. (2004). Labor analgesia and cesarean delivery: An individual patient meta-analysis of nulliparous women. Anesthesiology, 100(1), 142–148. [DOI] [PubMed] [Google Scholar]
- Shermer R. H., Raines D. A. (1997). Positioning during the second stage of labor: Moving back to basics. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 26(6), 727–734. [DOI] [PubMed] [Google Scholar]
- Simonson C., Barlow P., Dehennin N., Sphel M., Toppet V., Murillo D., Rozenberg S. (2007). Neonatal complications of vacuum-assisted delivery. Obstetrics and Gynecology, 109(3), 626–633. [DOI] [PubMed] [Google Scholar]
- Spong C. Y., Berghella V., Wenstrom K. D., Mercer B. M., Saade G. R. (2012). Preventing the first cesarean delivery: Summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, and American College of Obstetricians and Gynecologists workshop. Obstetrics and Gynecology, 120(5), 1181–1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taffel S. M., Placek P. J., Liss T. (1987). Trends in the United States cesarean section rate and reasons for the 1980–85 rise. American Journal of Public Health, 77(8), 955–959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (2013). Maternal, infant, and child health. Retrieved from http://healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=26
- Van Gemund N., Hardeman A., Scherjon S. A., Kanhai H. H. (2003). Intervention rates after elective induction of labor compared to labor with a spontaneous onset. A matched cohort study. Gynecologic & Obstetric Investigation, 56, 133–138. [DOI] [PubMed] [Google Scholar]
- Zhang J., Landy H., Branch D. W., Burkman R., Haberman S., Gregory K., Reddy U. M. (2010). Contemporary patterns of spontaneous labor with normal neonatal outcomes. Obstetrics and Gynecology, 116(6), 1281–1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Troendle J., Yancey M. (2002). Reassessing the labor curve in nulliparous women. American Journal of Obstetrics and Gynecology, 187(4), 824–828. [DOI] [PubMed] [Google Scholar]
- Zwelling E. (2010). Overcoming the challenges: Maternal movement and positioning to facilitate labor progress. American Journal of Maternal/Child Nursing, 35(2), 72–78. [DOI] [PubMed] [Google Scholar]