Abstract
Background
We aimed to characterize the clinical and electrophysiological features of patients with slow orthostatic tremor.
Case Report
The clinical and neurophysiological data of patients referred for lower limb tremor on standing were reviewed. Patients with symptomatic or primary orthostatic tremor were excluded. Eight patients were identified with idiopathic slow 4–8 Hz orthostatic tremor, which was associated with tremor and dystonia in cervical and upper limb musculature. Coherence analysis in two patients showed findings different to those seen in primary orthostatic tremor.
Discussion
Slow orthostatic tremor may be associated with dystonia and dystonic tremor.
Keywords: Slow orthostatic tremor, dystonia, clinical neurophysiology
Introduction
Primary orthostatic tremor (POT) typically presents with unsteadiness on standing, accompanied by a 13–18 Hz lower limb tremor.1 Otherwise typical orthostatic tremor (OT) has been described secondary to other conditions, including parkinsonism and restless legs syndrome.2–4 Slow OT may be symptomatic of midbrain lesions including demyelinating plaques,5 and has also been reported in Parkinson’s disease (PD).3 However, there are few reports of idiopathic slow OT in the literature,6 and its pathophysiology is unknown.7 We aimed to describe the neurophysiological characteristics of slow OT without underlying symptomatic lesions, and its associated neurological features, in a retrospective review of patients presenting to a large academic movement disorders service.
Case report
Patients
Records of patients with symptoms of lower limb tremor on standing, seen between 2004 and 2014 in the regional movement disorders clinic of the Greater Manchester Neurosciences Centre and referred for neurophysiological studies, were reviewed. We recorded the demographic and clinical characteristics of patients with slow OT that did not meet the criteria for POT. Patients with an underlying symptomatic lesion, including stroke and multiple sclerosis, were excluded. All patients had been initially reviewed by a specialist movement disorder neurologist (C.K., M.A.S., J.P.D., or M.W.K.), and information about their clinical syndrome and response to medications were recorded from the case notes.
Neurophysiological examination
All patients underwent surface electromyography (SEMG, bandpass filtered 30 Hz to 2 kHz; 5 kHz digitization) using self-adhesive 9-mm silver–silver chloride electrodes. Electrodes were placed over the right and left vastus lateralis (VL), biceps femoris, tibialis anterior (TA), and medial gastrocnemius (MG). The upper limb muscles studied included the deltoid, extensor carpi radialis, flexor carpi ulnaris, and abductor pollicis brevis. Lower limb tremor was assessed at rest, with the patient recumbent, and on standing. In two cases, spectral and coherence analysis were performed using commercial software (Natus Nicolet Viking Select).8,9 SEMG recordings (bandpass filtered 80–500 Hz) were taken from right and left TA and MG. All data were simultaneously sampled at 1000 Hz. The recording length was 30 seconds. For spectral analysis the periodogram was smoothed using a frequency-dependent smoothing window function (width 1.23 Hz, offset 3.20, slope 0.20); for coherence analysis, a smoothing window of 2.46 Hz was used to reduce the level of noise.10 All examinations were performed by the same clinical neurophysiologist with special training in movement disorders (A.G.M.).
Video 1. Patient 6, Video Clip A. The video shows a jerky asymmetrical postural tremor with dystonic posturing of the right upper limb, and jerky dystonic head tremor.
Patient characteristics
A total of eight patients were identified with idiopathic slow OT; their demographic and clinical characteristics are summarized in Table 1. A total of 12 patients with POT and three with symptomatic OT (one tardive, one secondary to stroke, one multiple sclerosis) were excluded. The mean age of patients at initial evaluation was 54.3±14.6 years and the mean symptom duration at the time of evaluation was 8.6±5.2 years. All patients had lower limb tremor on standing with a frequency of between 4 and 8 Hz, (Video 2, 4 and 6) as well as upper limb postural and action tremor, which was asymmetrical in all cases (Video 1, 3 and 5). In seven of the eight cases, unsteadiness or leg tremor when standing was the prominent presenting symptom. There was a family history of upper limb tremor in a first-degree relative in two patients. Six patients had evidence of dystonia in the cervical segment, upper limbs, or both. The remainder had asymmetrical, jerky rest and action tremor. None had signs of parkinsonism. Two patients had mild white matter changes on a magnetic resonance imaging brain scan without concomitant clinical signs; brain imaging was normal in all other cases. Two patients, initially suspected clinically to have PD, underwent [123I]-Ioflupane single photon emission computed tomography (FP-CIT SPECT) imaging, which was normal in both cases. The response to medication was heterogeneous, with benefit being reported for various anti-tremor drugs.
Table 1. Clinical and Neurophysiological Characteristics of Patients with Slow Orthostatic Tremor.
| Patient Number | Age/Sex | Duration (years) | Clinical Features | Treatment | Rest Tremor | EMG Burst Duration (ms) | Orthostatic Tremor | Investigations |
|---|---|---|---|---|---|---|---|---|
| 1 | 70/F | 6 | LL rest tremor LL tremor on standing Asymmetric R>L rest, postural, action UL tremor + jaw tremor No parkinsonism |
Levodopa – Gabapentin + Clonazepam + |
R UL 4.6 Hz R>L LL 5.2 Hz |
80–100 | R>L 5.8 Hz (increased amplitude) | [123I]-FP-CIT SPECT normal |
| 2 | 77/F | 15 | Retrocollis initially LL tremor on walking, no rest
tremor Intermittent R hand postural tremor |
BTX + (retrocollis) Clonazepam nt | None | 50–60 | 8 Hz | – |
| 3 | 43/M | 8 | LL/truncal tremor on standing, improved when
walking Slight LL rest tremor Dystonic posturing R>L UL, increased when writing Asymmetric jerky postural UL tremor Cervical dystonia and head tremor No parkinsonism |
Clonazepam – Propranolol – Levodopa – Topiramate – Primidone + Alcohol+THP– |
None | 80 | 5.3 Hz | Copper studies normal SCA genetics negative |
| 4 | 33/M | 16 | Jerky head tremor, cervical dystonia Moderate jerky L UL rest, postural, action tremor LL tremor on standing No parkinsonism | Propranolol + Topiramate – BTX + (head tremor) | L UL 6 Hz No LL tremor | 60–150 | 7.5 Hz | Copper studies normal |
| 5 | 62/M | 12 | LL tremor and unsteady when standing still No LL rest tremor Jerky UL R>L postural, action>rest tremor No parkinsonism |
THP – Levodopa +/– Topiramate – |
UL 6.5 Hz LL 6.5 Hz |
60–80 | 6.25 Hz | [123I]-FP-CIT SPECT normal |
| 6 | 53/F | 4 | UL jerky postural tremor R>L, increased with action Dystonic posturing R>L UL Unsteady on standing, slow OT improved on walking Head tremor, left torticollis No parkinsonism | Alcohol + SSRI + Metoprolol + Primidone nt THP + |
– | 150 | 4-5 Hz | Copper studies normal |
| 7 | 50/F | 6 | LL tremor, unsteady when standing still Jerky head tremor, cervical dystonia R>L rest tremor UL/LL R>L jerky postural tremor UL Writer’s cramp No parkinsonism |
Propranolol + Levodopa + |
R LL 4 Hz L LL 5 Hz |
100–120 | R LL 6 Hz L LL 5 Hz | Copper studies normal |
| 8 | 46/F | 2 | LL tremor, unsteady on standing Head tremor, UL action tremor R torticollis, jerky head tremor No rest tremor Jerky UL action tremor Slow OT on standing |
Primidone nt Clonazepam nt THP + | LL 5 Hz | R LL 7 Hz L LL 7.5 Hz | Copper studies normal |
Abbreviations: +, Benefit from Treatment; −, No Effect or Worsening; BTX, Botulinum Toxin; EMG; FP-CIT SPECT; L, Left; LL; nt, Not Tolerated; OT, Orthostatic Tremor; R, Right; SCA; SSRI, Selective Serotonin Reuptake Inhibitor; THP, Trihexiphenidyl; UL.
Neurophysiological examination
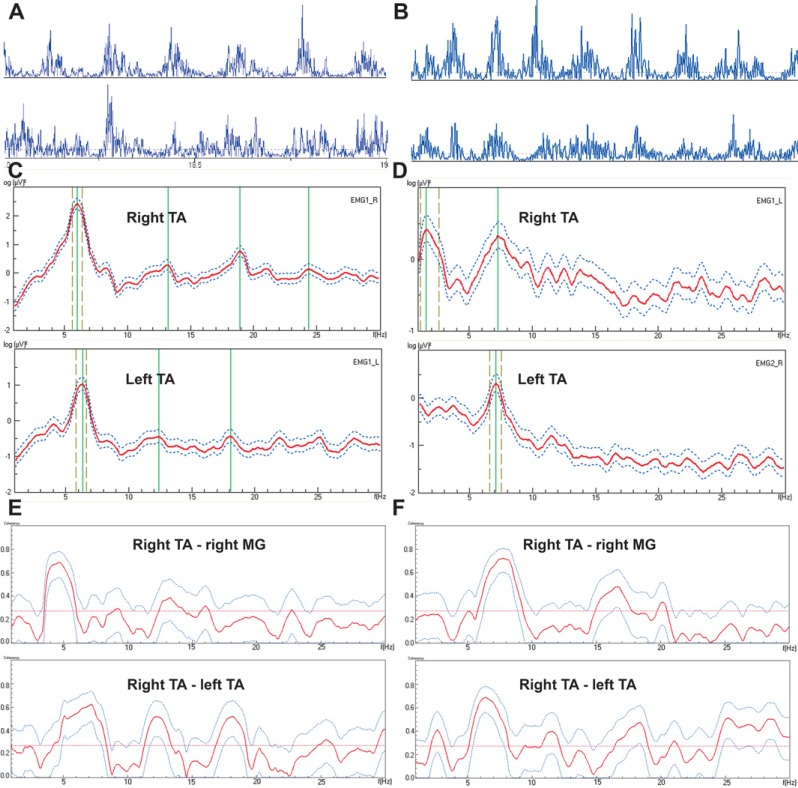
The neurophysiological characteristics of the patients are summarized in Table 1. All patients had slow 4–8 Hz lower limb tremor on standing, with variable degrees of upper and lower limb rest tremor (4.6–6.5 Hz), and postural tremor that was not altered by loading. There was evidence of co-contraction or an irregular relationship between ipsilateral agonist and antagonist muscles in three patients. Tremor increased in amplitude during standing on one leg in two patients. There was no evidence of distractibility or entrainment in any of the examinations performed. In patient 7 there is a notable variation in SEMG burst duration and asymmetry with more distinct bursts being seen on the right (Figure 1A).
Figure 1. Neurophysiological Analysis in Patients 7 (Left Column) and 8 (Right Column). (A,B) Raw electromyography recordings from right (top) and left (bottom) tibialis anterior (TA) over a 1-second epoch. (C,D) Power spectra from right and left TA demonstrating dominant peaks at 6–7 Hz for both patients. (E,F) Intralimb (right TA – right medial gastrocnemius) and interlimb (right TA – left TA) coherence analysis. The horizontal line represents the 5% significance level for the null hypothesis of zero coherence, and values above this line therefore show significant coherence.
Frequency domain analysis (Figure 1C,D) confirmed that the dominant frequency was ∼6 Hz for patient 7 and ∼7 Hz for patient 8. Smaller additional (12–13 and 18–19 Hz) sub-peaks were also seen in patient 7. Coherence analysis showed significant unilateral coherence around the dominant tremor frequency, with additional smaller peaks in the 12–20 Hz range (Figure 1E,F). Broader peaks, spanning an approximate 3 Hz range, of significant bilateral EMG–EMG coherence encompassing the dominant tremor frequency were seen. Significant bilateral EMG–EMG coherence peaks were also seen at 12–14 Hz and 17–18 Hz in case 7 and 15–17 Hz and 20 Hz in case 8.
Discussion
We report a series of patients who displayed idiopathic slow OT with a frequency of 4–8 Hz, significantly lower than that normally described in POT.11 Dystonic features were present in six of our series, leading us to examine the possible relationship between slow OT and dystonia.
Upper limb postural tremor is well described in POT, with 6–8 Hz tremor increasing to 16 Hz on standing,11 but in our cases the frequency of upper limb tremor remained low on posture holding and standing. While a degree of asymmetry may occur in essential tremor, the extent of asymmetry and presence of other neurological features such as dystonia excludes this diagnosis according to published diagnostic criteria.1 Another study reported slow 6–7 Hz OT in five patients: this was symptomatic in two cases, and only one other patient had postural upper limb tremor.12 It has been proposed that the term “pseudo-OT” be used instead of “slow OT” because of the differing features and probable underlying causes compared with POT.7 Consistent with this concept, electrophysiological studies in two of our patients confirm a dominant frequency peak at 6–7 Hz. Coherence analysis results are very different from typical findings in POT, in which very tight inter- and intra-limb coherence is seen around 13–18 Hz.13,14 A recent retrospective study of patients with OT suggested that around 50% with slow OT displayed lower levels of coherence and differing clinical features.15 The authors acknowledged the difficulties in nomenclature in this field, and their and our findings support that “slow” or “pseudo” OT is a different condition from POT.
Video 2. Patient 6, Video Clip B. Slow pseudo-orthostatic tremor is evident on standing.
Whereas many previous reports of slow OT in the literature have examined symptomatic cases,12,16 we specifically focused on those with idiopathic slow OT, which has been less reported. A recent report described a 10–11 Hz OT in a patient without underlying brain lesions, and suggested “primary slow OT” as a diagnostic entity,6 although the authors did not perform coherence analysis. Pseudo-OT has been previously linked to cases of genetic parkinsonism, particularly related to parkin mutations.17,18 However, there were no clinical features of parkinsonism in our cases. The presence of additional neurological features consistent with dystonia in the majority of our patients led us to consider the relationship between slow OT and dystonic tremor syndromes.
Video 3. Patient 7, Video Clip A. At rest this patient displays mild right sided rest tremor of upper and lower limbs. There is a jerky mixed head tremor. On posture holding she shows jerky right more than left upper limb tremor with dystonic right upper limb posturing and position specificity.
Dystonic tremor is defined as a mainly postural tremor with variable frequency (usually <7 Hz) occurring in a body part affected by dystonia.1,19 Tremor associated with dystonia is diagnosed where tremor is remote from the dystonic body part.1 All of our patients had asymmetrical jerky rest and/or postural tremor, often exacerbated by action, with additional features suggestive of dystonia in the majority, including head tremor, cervical and limb dystonia, and writer’s cramp, similar to those previously described.20,21 In a recent series of patients with primary OT the development of focal arm dystonia in one patient was reported, although the authors conceded this could be a chance association.4 In large recent studies of tremor in patients with adult-onset primary dystonia, orthostatic tremor was not observed.22,23 Although several of our patients had a family history of tremor, this is also reported in cases of suspected dystonic tremor.20
Video 4. Patient 7, Video Clip B. Gait is normal with no evidence of tremor until she stands still, at which point slow pseudo-orthostatic tremor is again seen.
While there are no agreed electrophysiological criteria for dystonic tremor, Schneider et al.20 described typical findings of a 3–7 Hz tremor that was not affected by loading and showed short latency to re-emergence on posture holding. The variable frequencies recorded in limbs and between different activities are also consistent with previous findings in dystonic tremor.1,19 One of the main limitations of this study is that it is a retrospective review of clinical data, and therefore systematic coherence analysis was only performed in two patients. These show a peak of coherence around the dominant frequency, as previously reported in cases of dystonic tremor and limb dystonia,20,24 while smaller peaks at higher frequencies suggest other driving frequencies. The response to medication and alcohol was heterogeneous, as expected in a small series, and consistent with other reports on dystonic tremor.20,21
Video 5. Patient 8, Video Clip A. At rest the patient has right torticollis with a jerky head tremor. There is action tremor of the upper limbs with no bradykinesia.
Video 6. Patient 8, Video Clip B. On standing a slow pseudo-orthostatic tremor is evident, which improves with walking.
We propose that slow OT can occur as a manifestation of, or in association with, dystonia and dystonic tremor; clinical and neurophysiological findings are different from those classically seen in primary 13–18 Hz OT. Limitations of our study include its retrospective nature and the consequent lack of a prespecified neurophysiological protocol. Prospective studies of such patients including neurophysiological protocols allowing assessment of brain plasticity would allow further elucidation of the link between slow orthostatic tremor and dystonia.
Footnotes
Funding: None.
Financial Disclosures: None.
Conflict of Interest: The authors report no conflict of interest.
Ethics Statement: All patients that appear on video have provided written informed consent; authorization for the videotaping and for publication of the videotape was provided.
References
- 1.Deuschl G, Bain P, Brin M. Consensus statement of the Movement Disorder Society on Tremor. Ad Hoc Scientific Committee. Mov Disord. 1998;13(Suppl.3):2–23. doi: 10.1002/mds.870131303. [DOI] [PubMed] [Google Scholar]
- 2.Gerschlager W, Munchau A, Katzenschlager R, et al. Natural history and syndromic associations of orthostatic tremor: A review of 41 patients. Mov Disord. 2004;19:788–795. doi: 10.1002/mds.20132. [DOI] [PubMed] [Google Scholar]
- 3.Leu-Semenescu S, Roze E, Vidailhet M, Legrand A, Trocello JM, Cochen V. Myoclonus or tremor in orthostatism: An under-recognized cause of unsteadiness in Parkinson’s disease. Mov Disord. 2007;22:2063–2069. doi: 10.1002/mds.21651. doi: http://dx.doi.org/10.1002/mds.21651. [DOI] [PubMed] [Google Scholar]
- 4.Mestre TA, Lang AE, Ferreira JJ, et al. Associated movement disorders in orthostatic tremor. J Neurol Neurosurg Psychiatry. 2012;83:725–729. doi: 10.1136/jnnp-2012-302436. doi: http://dx.doi.org/10.1136/jnnp-2012-30243. [DOI] [PubMed] [Google Scholar]
- 5.Baker M, Fisher K, Lai M, Duddy M, Baker S. Slow orthostatic tremor in multiple sclerosis. Mov Disord. 2009;24:1550–1553. doi: 10.1002/mds.22630. doi: http://dx.doi.org/10.1002/mds.22630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coffeng SM, Hoff JI, Tromp SC. A slow orthostatic tremor of primary origin. Tremor Other Hyperkinet Mov (NY) 2013;3:147. doi: 10.7916/D8057DNW. doi: http://dx.doi.org/10.7916/D8057DNW. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Erro R, Bhatia K, Cordivari C. Shaking on standing: A critical review. Mov Disord Clin Pract. 2014;1:173–179. doi: 10.1002/mdc3.12053. doi: http://dx.doi.org/10.1002/mdc3.12053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lauk M, Timmer J, Lucking CH, Honerkamp J, Deuschl G. A software for recording and analysis of human tremor. Comput Methods Programs Biomed. 1999;60:65–77. doi: 10.1016/s0169-2607(99)00012-7. doi: http://dx.doi.org/10.1016/S0169-2607(99)00012-7. [DOI] [PubMed] [Google Scholar]
- 9.Timmer J, Lauk M, Haussler S, et al. Cross-spectral analysis of tremor time series. IJBC. 2000;10:2595–2610. doi: http://dx.doi.org/10.1142/S0218127400001663. [Google Scholar]
- 10.Timmer J, Lauk M, Vacha W, Lucking CH. A test for a difference between spectral peak frequencies. Comput Stat Data Anal. 1999;30:45–55. doi: http://dx.doi.org/10.1016/S0167-9473(98)00106-6. [Google Scholar]
- 11.Piboolnurak P, Yu QP, Pullman SL. Clinical and neurophysiologic spectrum of orthostatic tremor: Case series of 26 subjects. Mov Disord. 2005;20:1455–1461. doi: 10.1002/mds.20588. doi: http://dx.doi.org/10.1002/mds.20588. [DOI] [PubMed] [Google Scholar]
- 12.Gabellini AS, Martinelli P, Gulli MR, Ambrosetto G, Ciucci G, Lugaresi E. Orthostatic tremor: Essential and symptomatic cases. Acta Neurol Scand. 1990;81:113–117. doi: 10.1111/j.1600-0404.1990.tb00944.x. doi: http://dx.doi.org/10.1111/j.1600-0404.1990.tb00944.x. [DOI] [PubMed] [Google Scholar]
- 13.Lauk M, Koster B, Timmer J, Guschlbauer B, Deuschl G, Lucking CH. Side-to-side correlation of muscle activity in physiological and pathological human tremors. Clinical Neurophysiol. 1999;110:1774–1783. doi: 10.1016/s1388-2457(99)00130-3. [DOI] [PubMed] [Google Scholar]
- 14.Koster B, Lauk M, Timmer J, Poersch M, Guschlbauer B, Deuschl G. Involvement of cranial muscles and high intermuscular coherence in orthostatic tremor. Ann Neurol. 1999;45:384–388. doi: 10.1002/1531-8249(199903)45:3<384::aid-ana15>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 15.Rigby HB, Rigby MH, Caviness JN. Orthostatic tremor: A spectrum of fast and slow frequencies or distinct entities? Tremor Other Hyperkinet Mov (NY) 2015;5:324. doi: 10.7916/D8S75FHK. doi: http://dx.doi.org/10.7916/D8S75FHK. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Benito-Leon J, Rodriguez J, Orti-Pareja M, Ayuso-Peralta L, Jimenez-Jimenez FJ, Molina JA. Symptomatic orthostatic tremor in pontine lesions. Neurology. 1997;49:1439–1441. doi: 10.1212/wnl.49.5.1439. doi: http://dx.doi.org/10.1212/WNL.49.5.1439. [DOI] [PubMed] [Google Scholar]
- 17.Thomas A, Bonanni L, Antonini A, Barone P, Onofrj M. Dopa-responsive pseudo-orthostatic tremor in parkinsonism. Mov Disord. 2007;22:1652–1656. doi: 10.1002/mds.21621. doi: http://dx.doi.org/10.1002/mds.21621. [DOI] [PubMed] [Google Scholar]
- 18.Infante J, Berciano J, Sanchez-Juan P, et al. Pseudo-orthostatic and resting leg tremor in a large Spanish family with homozygous truncating parkin mutation. Mov Disord. 2009;24:144–147. doi: 10.1002/mds.22349. doi: http://dx.doi.org/10.1002/mds.22349. [DOI] [PubMed] [Google Scholar]
- 19.Jedynak CP, Bonnet AM, Agid Y. Tremor and idiopathic dystonia. Mov Disord. 1991;6:230–236. doi: 10.1002/mds.870060307. doi: http://dx.doi.org/10.1002/mds.870060307. [DOI] [PubMed] [Google Scholar]
- 20.Schneider SA, Edwards MJ, Mir P, et al. Patients with adult-onset dystonic tremor resembling parkinsonian tremor have scans without evidence of dopaminergic deficit (SWEDDs) Mov Disord. 2007;22:2210–2215. doi: 10.1002/mds.21685. [DOI] [PubMed] [Google Scholar]
- 21.Schwingenschuh P, Ruge D, Edwards MJ, et al. Distinguishing SWEDDs patients with asymmetric resting tremor from Parkinson’s disease: A clinical and electrophysiological study. Mov Disord. 2010;25:560–569. doi: 10.1002/mds.23019. doi: http://dx.doi.org/10.1002/mds.23019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Defazio G, Gigante AF, Abbruzzese G, et al. Tremor in primary adult-onset dystonia: Prevalence and associated clinical features. J Neurol Neurosurg Psychiatry. 2013;84:404–408. doi: 10.1136/jnnp-2012-303782. doi: http://dx.doi.org/10.1136/jnnp-2012-303782. [DOI] [PubMed] [Google Scholar]
- 23.Erro R, Rubio-Agusti I, Saifee TA, et al. Rest and other types of tremor in adult-onset primary dystonia. J Neurol Neurosurg Psychiatry. 2014;85:965–968. doi: 10.1136/jnnp-2013-305876. doi: http://dx.doi.org/10.1136/jnnp-2013-305876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grosse P, Edwards M, Tijssen MA, et al. Patterns of EMG–EMG coherence in limb dystonia. Mov Disord. 2004;19:758–769. doi: 10.1002/mds.20075. doi: http://dx.doi.org/10.1002/mds.20075. [DOI] [PubMed] [Google Scholar]