Introduction
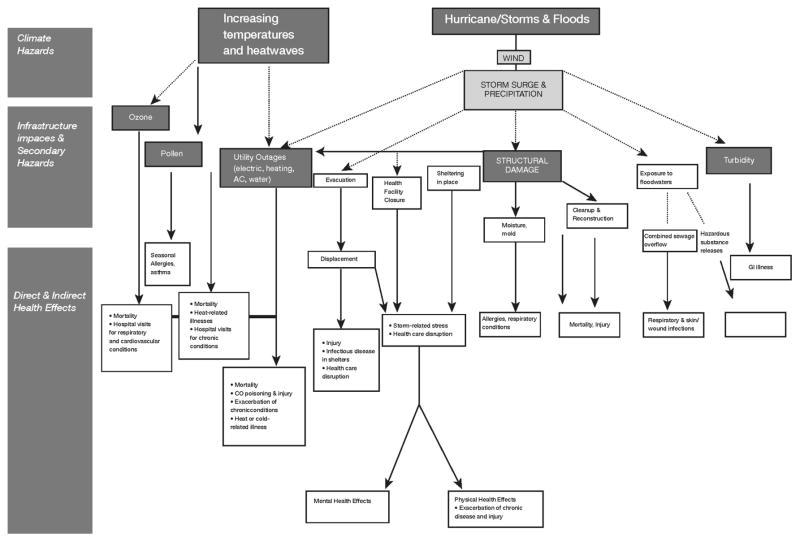
Recent experience from Hurricane Sandy and high-temperature episodes has clearly demonstrated that the health of New Yorkers can be compromised by extreme coastal storms and heat events. Health impacts that can result from exposure to extreme weather events include direct loss of life, increases in respiratory and cardiovascular diseases, and compromised mental health. Other related health stressors—such as air pollution, pollen, and vector-borne, water-borne, and food-borne diseases—can also be influenced by weather and climate. Figure 5.1 illustrates the complex pathways linking extreme weather events to adverse health outcomes in New York City. New York City and the surrounding metropolitan region face potential health risks related to two principal climate hazards: (1) increasing temperatures and heat waves, and (2) coastal storms and flooding. The health impacts of these hazards depend in turn on myriad pathways, the most important of which are illustrated in the figure.
Figure 5.1.
Pathways linking climate hazards to health impacts in New York City.
Although New York City is one of the best-prepared and most climate-resilient cities in the world, there remain significant potential vulnerabilities related to climate variability and change. As part of the NPCC2 process, a team of local climate and health specialists was mobilized to assess current vulnerabilities and to identify strategies that could enhance the resilience of New York City to adverse health impacts from climate events. The goal was to highlight some of the important climate-related health challenges that New York City is currently facing or may face in the future due to climate variability and change, based on emerging scientific understanding.
As indicated in Figure 5.1, health vulnerabilities can be magnified when critical infrastructure is compromised. Critical infrastructure is a highly complex, heterogeneous, and interdependent mix of facilities, systems, and functions that are vulnerable to a wide variety of threats, including extreme weather events. For example, delivery of electricity to households depends on a multi-faceted electrical grid system that is susceptible to blackouts that can occur during heat waves. These, in turn, can expose people to greater risk of contact with exposed wires or to greater heat stress due to failure of air conditioning. Understanding and predicting the impacts that extreme weather events may have on health in New York City require careful analysis of these interactions.
Two recent plans to enhance climate resiliency in New York City have been released. A Stronger, More Resilient New York (City of New York, 2013) was developed in the aftermath of Hurricane Sandy by a task force of representatives from City agencies and consultants. This plan was informed by a detailed analysis of the impacts of Hurricane Sandy on infrastructure and the built environment and by the NPCC’s updated 2013 climate projections for the New York metropolitan region. It includes more than 250 initiatives and actionable recommendations addressing 14 domains of the built environment and infrastructure including the healthcare system and several other domains relevant to protecting public health.
In addition, the 2014 New York City Hazard Mitigation Plan (HMP) (City of New York, 2014), developed by the NYC Office of Emergency Management in collaboration with the Department of City Planning, updated the 2009 HMP and assesses risks from multiple hazards that threaten New York City. These include but are not limited to several climate-related hazards such as coastal storms and heat waves, and it lays out comprehensive strategies and plans to address these hazards. Many of the measures recommended by A Stronger, More Resilient New York and the HMP have already been implemented, are in progress, or are planned (City of New York, 2013; 2014). This chapter does not include a detailed review of these plans, which would be beyond the expertise and charge of the contributors. Nonetheless, the recommendations in this chapter do broadly support the plans laid out in A Stronger, More Resilient New York and the 2014 HMP, and these are referenced at several points where they are especially relevant. Here we focus on summarizing and synthesizing the emerging scientific knowledge on climate-related health hazards, knowledge that can inform ongoing preparedness planning.
Key terms related to climate variability and change as they are applied in the health sector are defined in Box 5.1. This is followed by sections describing health risks, vulnerabilities, and resilience strategies for coastal storms and extreme heat events. We then briefly discuss the interactions of climate change with air pollution, pollen, vector-borne diseases, and water- and food-borne diseases. We conclude with recommendations for research and resiliency planning.
Box 5.1. Definitions of key cross-cutting terms in the health context.
Adaptation
Initiatives and measures to reduce the vulnerability of natural and human systems against actual or expected climate change effects. Various types of adaptation exist, such as anticipatory and reactive, private and public, and autonomous and planned. For health, physiological adaptation is also relevant.
Infrastructure
The man-made built environment and supporting systems and facilities, including buildings, land use (e.g., parks and green space), transportation systems, and utilities (e.g., electricity, running water).
Critical infrastructure
Systems and assets, whether physical or virtual, so vital to the United States that the incapacity or destruction of such systems and assets would have a debilitating impact on security, national economic security, national public health or safety, or any combination of those matters. In the health sector, examples include the electrical grid, water supply, and access to functioning health care facilities. Source: §1016(e) of the U.S. Patriot Act of 2001 (42 U.S.C. §5195c(e)).
Environmental public health indicators
Summary measures that provide information about a population’s health status in relation to environmental factors. Ongoing collection, integration, analysis, and dissemination of indicators can be used to:
Quantify the magnitude of a public health problem
Detect trends in health, exposures, and hazards
Identify populations at risk of environmentally related diseases or of exposure to hazards
Generate hypotheses about the relationship between health and the environment
Direct and evaluate control and prevention measures and individual actions
Facilitate policy development Source: U.S. CDC (2014).
Vulnerability
The propensity for the health of individuals or groups to be adversely affected as a result of exposure to a climate hazard. Vulnerability is an internal characteristic of the affected system and includes the characteristics of persons or groups and their situation that influence their capacity to anticipate, cope with, resist, and recover from an adverse climate event. Different levels of vulnerability will lead to different levels of health damage and loss under similar conditions of exposure to physical events of a given magnitude. Source: IPCC (2012).
Resilience
Resilience is the ability of a system and its component parts to anticipate, absorb, accommodate, or recover from the effects of a potentially hazardous event in a timely and efficient manner, including through ensuring the preservation, restoration, or improvement of its essential basic structures. Source: Lavell et al. (2012).
5.1. Coastal storms and flooding
Storm surge-related health risks will be compounded in the future as sea level continues to rise and with the potential for more intense storms in a changing climate (Lane et al., 2013a; Chapter 2). Large and growing numbers of people live near coasts and within areas likely to be impacted by coastal storms (Walsh et al., 2014).
The health risks related to coastal storms can vary widely and in ways that are hard to predict due to differences in the severity, timing, and location of landfall, the topographic and infrastructure characteristics of affected areas, and the capacity for preparedness and response.
Storm health impact pathways
There are at least seven pathways through which storm events can adversely affect health, including:
Direct exposure to storm hazards
Evacuation
Exposure to secondary hazards related to utility outages and sheltering in place in inadequate housing after the storm
Exposure to secondary hazards including contaminated drinking water, contact with contaminated floodwaters, and mold and moisture in housing
Population displacement and disruption of services
Mental health effects from traumatic or stressful experiences during and after the storm
Health and safety risks from cleanup and recovery activities
These pathways and their interactions are elaborated in Figure 5.1. Storms can impact health not only through direct exposure to climate hazards such as wind and flood waters but also via a range of secondary hazards, many of which operate through disruptions in critical infrastructure. These hazards, for which few data often exist, can result in a range of short-term and long-term health outcomes.
Direct exposure to storm hazards
Adverse health effects due to direct exposure to storm hazards include deaths and injuries from drowning, electrocution, or physical trauma. All of these health effects were observed in the immediate aftermath of Hurricane Sandy (see Box 5.2). Flash flooding, due to excessive rainfall, although often a key risk factor for drowning during extreme storm events in many locations (French et al., 1983; Rosenzweig et al., 2011), is generally not a major threat to life safety in New York City and was not observed for Sandy.
Box 5.2. Hurricane Sandy and health in New York City.
Hurricane Sandy showed in stark terms the extent to which the health of New Yorkers can be rapidly put at risk by powerful coastal storms. In its initial landfall on October 29, 2012, Sandy caused 44 deaths in New York City, nearly four-fifths of which occurred by drowning due to the storm-driven tidal surge. The remaining deaths were caused by falling trees, falls, electrocution, and other trauma. Nearly half of fatalities occurred among adults aged 65 or older. Although these deaths represent the most obvious and tragic impact of Sandy, they do not account for the storm’s full impact on excess mortality from accidental and natural causes, as well as other nonfatal health impacts, in impacted communities.
Hurricane Sandy had substantial impacts due to its unusually large size and low pressure, a massive storm surge, and the fact that its landfall coincided with high tide (see Box 2.1). Further, impacts differed considerably across locations within the flood zone due to local variations in the storm and tidal surges, differing housing types, the extent to which energy, water, and/or transportation infrastructure was disrupted, and underlying population health and resilience.
Five acute-care hospitals in New York City shut down due to Sandy, three of which required evacuation of patients after the storm hit due to flooding and damage to energy infrastructure in lower floors (NYU Langone Medical Center, Bellevue Hospital, and Coney Island Hospital). Other health facilities affected by Sandy included a psychiatric hospital, nursing homes, long-term-care facilities, outpatient and ambulatory care facilities, community-based providers, and pharmacies.
After Hurricane Sandy made landfall, 2 million of New York City residents lost power at some point during the storm. However, even after the electric grid had been largely restored, many residential buildings in storm-inundated areas still lacked electric power, heat, or running water, often because of saltwater flood damage to electrical and heating systems. Many people who did not evacuate in advance of the storm sheltered in place in housing conditions that lacked one or more of these essential services.
Developing a fuller understanding of the health impacts of Sandy requires careful analysis of health data, only some of which have so far been available. For example, in the days following Sandy, health department surveillance data showed the impact of people living without power or heat and, in some cases, trying to provide power or heat in unsafe ways. From the storm impact until November 9 (10 days), carbon monoxide (CO)-related emergency department visits and Poison Control Center (PCC) calls related to CO exposure were elevated for the time of year; PCC data frequently identified storm-related sources of exposure including charcoal grills and household cooking appliances used for heating, as well as portable generators. Calls to the PCC about gasoline exposures, often due to siphoning, were also elevated, although no serious outcomes were reported (http://www.ncbi.nlm.nih.gov/pubmed/24237625). On the other hand, there was no observed increase in reportable infectious diseases (http://www.ncbi.nlm.nih.gov/pubmed/24274131).
A more complete accounting for immediate, delayed, and longer-term Sandy health impacts, including those related to health-care facilities, power outages, stress and mental health disorders, and flood damage to homes requires longer-term study and access to data that were not immediately available, such as all-cause mortality data, hospital discharge data, and follow-up surveys. Several ongoing studies aim to characterize these impacts with funding by the Centers for Disease Control and Prevention (http://www.cdc.gov/phpr/science/hurricane_sandy_recovery_research.html).
Evacuation
Evacuation before, during, or after a storm event can result in health impacts, including those due to traffic accidents. An inability to evacuate in advance of a storm due to age, disability, or lack of economic resources, or an unwillingness to evacuate in order to protect one’s home and/or property, increases vulnerability to direct storm hazards (Jonkman and Kelman, 2005; Zoraster, 2010). Evacuation from health care and nursing home facilities presents complex challenges because of the unique needs of patients and elderly individuals (Klein and Nagel, 2007).
Secondary hazards from utility outages and sheltering in place
Widespread power outages can occur from storm events due to flooding and wind damage to infrastructure. Lack of electricity can make it difficult or impossible to control interior climate, refrigerate food, pump water to upper floors of high-rise buildings, move within buildings, and operate medical support equipment (Beatty et al., 2006). These infrastructure disruptions can lead to a wide range of adverse health effects depending on the age, health, and economic resources of residents in the affected households. For example, exposure to ambient heat or cold in the absence of climate control may lead to heat- or cold-related illness or exacerbate underlying chronic conditions. Carbon monoxide poisoning from backup generators or cooking equipment used improperly is another potential risk. Increases in overall mortality rates have been observed after widespread power outages (Anderson and Bell, 2012).
Secondary hazards from contaminated drinking water, floodwaters, and mold and moisture
Intense rainfall and wind can compromise water quality via mobilization of pathogens and/or toxins. Untreated sewage in urban areas sometimes contaminates surface waters when heavy rainfall leads to combined sewer overflows. Toxic waste reservoirs can also disperse pollutants (Rotkin-Ellman et al., 2010; Ruckart et al., 2008). Flooding of structures is a strong risk factor for mold growth and may result in subsequent respiratory symptoms such as cough or wheeze and be a risk factor for childhood asthma exacerbation (Barbeau et al., 2010; Jaakkola et al., 2005).
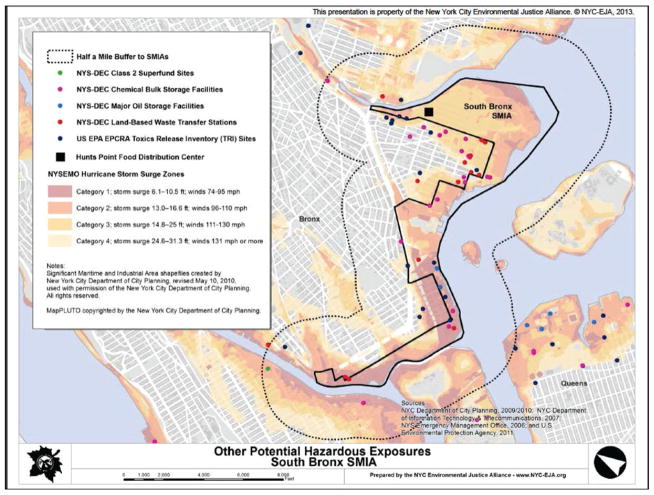
Research conducted by the New York City Environmental Justice Alliance’s (NYC-EJA)a Waterfront Justice Project has raised awareness about how hazardous substances handled, stored, or transferred in waterfront industrial neighborhoods may be accidentally released in the event of storm surge. For example, Figure 5.2 shows the close proximity of industrial facilities, residential neighborhoods, and food distribution facilities to storm surge zones in the Hunts Point neighborhood of the South Bronx (NYC-EJA, 2014).
Figure 5.2.
Storm surge zones and sources of potentially hazardous materials in the South Bronx. Source: Bautista et al., 2014
Damage to healthcare facilities, population displacement and disruption of services
As demonstrated by Hurricane Sandy, critical healthcare infrastructure can be damaged and made inoperable for extended periods by coastal flooding events (see A Stronger, More Resilient New York: City of New York, 2013). Institutions that provide care that can be impacted by coastal storms include hospitals, nursing homes, adult-care facilities, correctional facilities, primary and mental health–care facilities, and pharmacies.
In addition, for people who evacuate flood-prone neighborhoods, living for extended periods in shelters is associated with increased risk of communicable diseases and with interruption in medical care that could otherwise prevent complications from chronic health conditions (Arrieta et al., 2009). Loss of medical record information, medications (including information regarding names and dosages), and access to routine medical care can exacerbate health problems.
Mental health
Exposure to direct and secondary storm hazards and their aftermath, including displacement, can have adverse consequences for mental health, exacerbating existing disease or contributing to new cases (Pietrzak et al., 2012; Galea et al., 2007). Post-traumatic stress disorder (PTSD) is a common observation following natural disasters. Some important predictors of mental-health impacts include storm-related physical illness or injury, physical adversity, and property loss. Mental health impacts can linger or intensify long after storm events as emergency support services wind down; however, this is an area for which more study is needed.
Clean-up and recovery work
Recovery efforts can include risks related to demolition and renovation work, including traumatic injuries and exposure to dust and to fumes from temporary generators. Mold remediation can potentially expose workers as well as residents to unhealthy levels of mold if precautions are not taken.
Health vulnerability factors for storms
Although the pathways linking coastal storm events to adverse health outcomes are numerous and complex, increased vulnerability tends to be associated with a number of factors:
Both the old and very young tend to be more vulnerable due to lack of mobility
Women tend to be more vulnerable with respect to economic resources available for recovery
Preexisting physical, mental, or substance-abuse disorders can impede safety-seeking behaviors
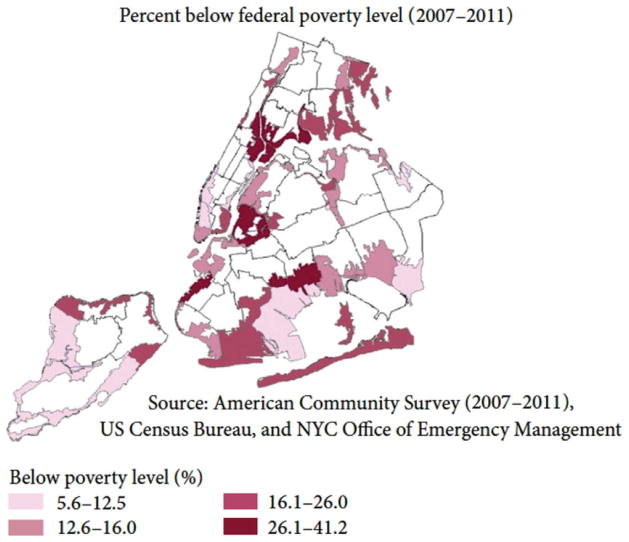
Residents of low-income households have fewer resources for relocation and/or sheltering in place. Figure 5.3 maps the percentage of people living below poverty within New York City flood evacuation zones
Workers engaged in recovery efforts, owing to their exposure to toxic contaminants and injury risks
Those with weak social networks, hindering safety-seeking behaviors
Those especially dependent on critical infrastructure such as electric power, putting them at risk of disruption of those services
Figure 5.3.
Poverty rate within 2012 NYC hurricane evacuation zones. Note that the prevalence estimates represent the entire United Hospital Fund neighborhood but are displayed only within the evacuation zone. Source: Lane et al. (2013a).
Vulnerability tends to be greater where multiple individual factors are present.
Improving health resilience to coastal stormsb
On the basis of our experience with Hurricane Sandy as well as lessons learned from other coastal storm events, we can highlight several ways in which health resiliency can be enhanced in the face of coastal storm events.
Enhancing community engagement is critical
Health resilience can be enhanced if communities in flood zones and evacuation zones are actively engaged to develop neighborhood-level climate-health vulnerability maps, deliver messages about ways to prepare for storms and other climate emergencies, create systems to locate vulnerable people, and disseminate information on locations of shelters and other types of care centers. Health impacts can be reduced by enhancing capacity for immediate post-storm door-to-door outreach, assessment of medical and other urgent needs, and assistance to populations stranded or sheltering in place, with a focus on the most vulnerable. To ensure effective responses, it is important to enhance communication among community-based volunteer organizations and government agencies involved in outreach and response.
Planning and preparation are needed for both short-term and long-term sheltering of evacuees
For those who take shelter, special effort is required to minimize the disruption of physical and mental health care and medication access. New York City’s Hazard Mitigation Plan (City of New York, 2014) includes the City’s Shelter Plan within the overall Coastal Storm Plan and describes efforts to develop more and improved post-disaster interim housing options.
Speedy restoration of electrical power and natural gas distribution and local delivery systems is key to public health protection in the aftermath of extreme weather events
People living in housing that lacks essential utilities (power, heat, and running water) face numerous health risks. Thus, measures to harden critical infrastructure against projected flooding and high wind risks will protect health as well as critical infrastructure. Transportation and communications infrastructure systems are also critical for public health.
Continuity of healthcare services is essential to protecting public health
Measures that can reduce disruptions of service delivery and/or speed recovery of services for the health system include building patient-care areas above flood elevation, elevating or flood-proofing back-up generators and fuel and other essential building systems from storm damage, preparedness for hospital evacuation decision-making and safety, systems to track displaced clients/residents, backup communications systems, and plans to ensure continuity of care and safe sheltering in place at storm-hardened facilities. Many health-system resiliency measures are addressed in the City’s Hazard Mitigation Plan (City of New York, 2014) and A Stronger, More Resilient New York (City of New York, 2013); some, including new design standards for facilities, are already being addressed in pending and enacted lawsc and initiatives.d
5.2. Extreme heat
More frequent and more severe coastal flooding events are not the only climate-related health hazards faced by New York City due to climate change in the coming decades. Warming temperatures will result in longer and more intense summer heat waves.
Heat was the largest of weather-relatede causes of death in the United States in 2012, as it has been on average since NOAA began reporting data for heat in 1988 (NOAA, 2014). Furthermore, heat-related morbidity (disease events such as emergency room visits or hospital admissions) and mortality (deaths) are the most well understood, measurable, and yet preventable impacts of climate change on human health (Confalonieri et al., 2007).
In recognition of the significance of these impacts, New York City is making substantial progress in building long-term resiliency to heat via enhanced messaging to the public and healthcare providers, advance warning of heat events, improved access to cooling centers, and other measures.
As are other large cities in the Northeast and upper Midwest of the United States and cities just over the border in Canada, New York City is particularly susceptible to the impacts of heat and will face challenges in the years to come. Factors that contribute to vulnerability in such cities include the urban heat island effect that can amplify the impacts of rising temperatures (Rosenzweig et al., 2009) and a relatively high proportion of older housing stock that may be poorly adapted to hot weather and lack air conditioning compared to many southern U.S. cities. In addition to hotter summers expected in the years to come, New York City’s population is aging, and the prevalence of obesity in adults has been increasing. Being elderly, obese, and/or diabetic are risk factors for heat-related morbidity and mortality (Basu and Samet, 2002).
Evidence for heat and health responses
A large number of studies have characterized health responses during and following severe heat waves such as the European heat wave of 2003 (Le Tertre et al., 2006) and the 1995 heat wave in Chicago (Whitman et al., 1997; Klinenberg, 2002) (Box 5.3). Early studies in New York City focused on specific heat-wave episodes (Marmor, 1975; Ellis and Nelson, 1978). More recent studies have assessed health responses in relation to less severe but more frequent temperature extremes. These more recent studies usually fit an exposure–response function that can be used to quantify the excess mortality that occurs when temperatures rise above certain levels (Fig. 5.4).
Box 5.3. Heat: Key concepts.
Heat exposure metrics
Various exposure metrics such as minimum, mean, or maximum temperature or composite indices of temperature, humidity, and/or other meteorological variables have been utilized to quantify the effects of heat on morbidity and mortality. In a recent analysis, various exposure metrics performed similarly as predictors of heat-related mortality in New York City (Metzger et al., 2010).
Health and heat waves
Heat waves are broadly defined as periods of unusually hot weather over an extended period of time, relative to local conditions. In New York, a heat wave is defined as a period of at least three consecutive days with temperatures ≥90°F (32°C) (See Chapter 1). However, it is worth noting that health impacts can occur when only one or two days of elevated temperatures are experienced.
NYC heat health warning system
In New York City, a citywide heat emergency response is triggered when an extreme heat event is forecast, defined as any one day reaching a heat index (HI)f of 100°F or any two or more consecutive days reaching 95°F HI. These thresholds are based on studies of the relationship between temperature and excess mortality in NYC (Metzger et al., 2010).
Urban heat island effect
“Urban heat island effect” refers to the occurrence of substantially higher temperatures (especially at night) within an urban area than in surrounding less-built-up areas. A recent study in New York City found that the city’s heat island effect can reach 8°F (Rosenzweig et al., 2009). The urban heat island may enhance the health risks of climate-related warming.
Figure 5.4.
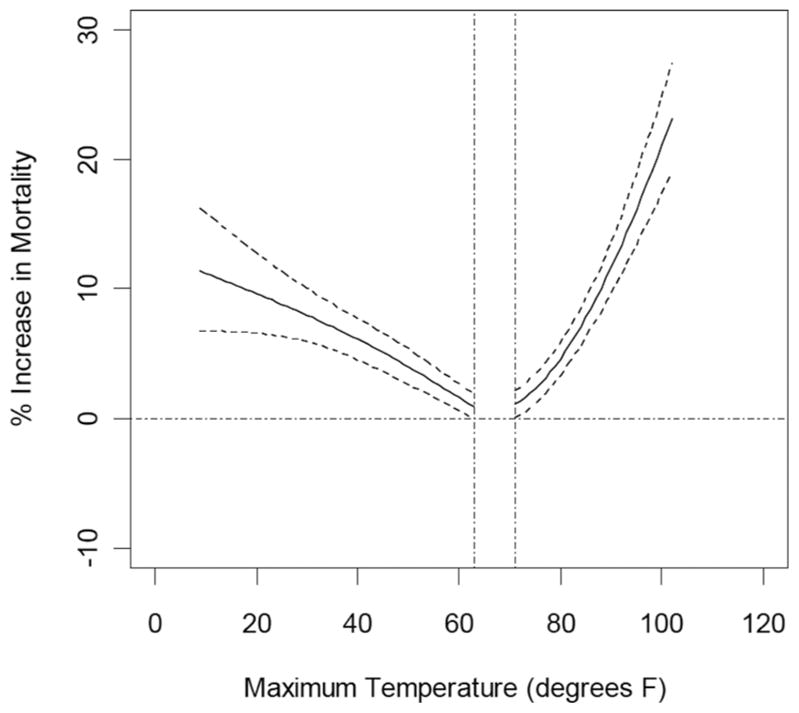
Exposure–response function for temperature-related mortality in Manhattan, NY, based on daily data from 1982 to 1999 (Li et al., 2013). Both cold and warm temperatures are associated with increased risk of premature death. The dashed lines indicate the 95% confidence bounds.
An example of a temperature exposure–health response function for Manhattan from Li et al. (2013) is reproduced in Figure 5.4. This shows that both cold and warm temperatures can increase risk of premature death. The gap in the curve at the bottom indicates the range of temperatures in Manhattan in which there is no observable mortality risk.
Most studies investigating the impacts of heat have focused on premature deaths (i.e., mortality) (Barnett, 2007; Basu et al., 2008; Curriero et al., 2002; Medina-Ramón and Schwartz, 2007). Heat has a direct impact on total daily deaths, with most deaths occurring on the same day or shortly after exposure to heat. Deaths due to specific causes also have been associated with high temperatures. For example, in New York City, daily deaths from cardiovascular disease were associated with higher warm-season temperatures in a recent study (Ito et al., 2010). Most deaths occur at home, but studies have also reported an increase in emergency room visits and hospital admissions for heat-sensitive diseases during heat episodes (Knowlton et al., 2006; Lin et al., 2009). According to a recent report based on data between 2000 and 2011, approximately 447 heat-related emergency department visits, 152 hospital admissions, and 13 deaths occurred annually in New York City (U.S. CDC, 2013c). Exposure to elevated temperatures may also have an impact on birth outcomes. For example, a recent study reported an association between high ambient temperature and pre-term births (Basu et al., 2010).
Heat-related deaths determined on death certificates often underestimate the full burden because of difficulties in establishing a conclusive diagnosis, especially for the large number of deaths that occur at home during extreme heat events (Nixdorf-Miller et al., 2006) (see Box 5.4). After a severe 10-day heat wave in New York City in 2006, for example, there were only approximately 40 deaths coded as heat stroke on death certificates, whereas there were 100 excess deaths that occurred in association with the heat wave as determined by NYC DOHMH (2006).
Box 5.4. Definitions of heat-related deaths.
Two different approaches are commonly employed to quantify the impacts of high ambient temperatures on deaths:
The first identifies individual deaths that have been listed as heat-related on death certificates.
The second estimates “statistical heat-related deaths” based on a statistical analysis of deaths from total daily death counts in relation to daily temperatures.
The advantage of the first method—based on death certificates—is that this information is available quickly, and these deaths can be individually counted and investigated to better understand risk factors, including housing conditions, the presence of air conditioning, levels of social isolation, and other factors that are key to informing prevention. However, this method substantially underestimates the total burden of heat-related deaths.
The advantage of the second method—based on statistical analysis—is that it potentially provides a fuller accounting for the total burden of heat-related deaths. However, the statistical analyses require multiple years of data as inputs, averaged over time and the population. In addition, there is no standardized method for the statistical estimation of heat deaths, leading to inconsistencies across assessments.
Morbidity and mortality effects of heat may be especially severe if a blackout occurs during an extreme heat event. Blackouts are more likely during heat waves due to the increased demand for electric power for air conditioning, an effect that places stress on the systems that supply and deliver electricity. On the other hand, air conditioning provides important protection from exposure to heat, limiting health impacts. When blackouts occur, exposure to heat increases, with a corresponding increase in health risks. Blackouts can also increase risk of carbon monoxide poisoning from improper use of generators and cooking equipment.
During August 2003, the largest blackout in U.S. history occurred in the Northeast. Although this particular blackout did not coincide with a heat wave, it occurred during warm weather and resulted in approximately 90 excess deaths and an increase in respiratory hospitalizations (Lin et al., 2012; Anderson and Bell, 2012). As a result of higher summertime temperatures (with a corresponding increase in electricity usage) and an already-stressed electricity grid, climate change may bring frequent blackouts. Other indirect health impacts of heat may be associated with increased violence and crime (Hsiang et al., 2013).
Projecting future heat-related health risks in a changing climate
Projecting potential future health impacts from warming temperatures involves linking together projections about future climate, the underlying health status of the population, the size and age distribution of the population, and the exposure–response function.
A recent study by Li and colleagues used down-scaled temperature projections from an ensemble of 16 global climate models and two greenhouse gas emission scenarios (high and low) to project heat-related mortality in Manhattan over the current century in the face of climate change (Li et al., 2013). Results are summarized in Figure 5.5, which plots statistically estimated heat-related deaths in an 18-year baseline period centered on the 1980s, and projected heat-related deaths in three future decades.
Figure 5.5.
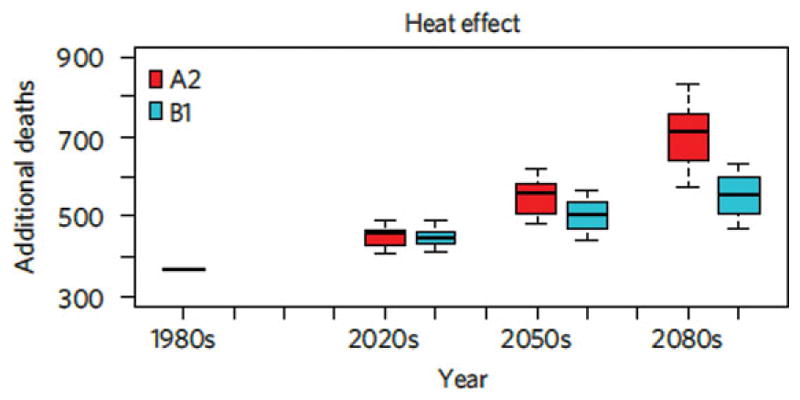
Distribution of heat-related deaths in the 1980s (observed), 2020s, 2050s, and 2080s for 16 global climate models and two greenhouse gas emission scenarios. The A2 scenario assumes relatively high, and the B1 assumes relatively low, greenhouse gas emissions over the 21st century. Source: Li et al. (2013).
Comparisons of recent heat impacts with mortality reported during severe heat waves in the 1970s suggest that in New York City vulnerability to heat waves may be decreasing over time, as has been reported in other locations (Carson et al., 2006). A recent study by Columbia University documents a decreasing trend in heat impacts over the 20th century (Petkova et al., 2014). Increasing use of home air conditioning and better air quality during heat waves may have played a role in reducing vulnerability. Vulnerability aside, continuing climate warming and urbanization mean more people will migrate to cities, and more people will be exposed to extreme heat. Whether future trends in these parameters or the growing populations of elderly and obese individuals in New York City will produce a net increase or decrease in heat-related health outcomes is uncertain.
Vulnerability mapping
Several studies have found that certain subpopulations—the elderly, African-Americans, and those with less education—are more susceptible to the health impacts of temperature (Anderson and Bell, 2009; Medina-Ramón et al., 2006). A recent investigation in New York City (J. Madrigano, personal communication, 2014) found that during heat waves (compared to other warm-season days), deaths were more likely to occur in African-American individuals than other groups, more likely to occur at home than in institutions and hospital settings, and more likely among those living in census tracts where more households received public assistance. Finally, deaths during heat waves were more likely among residents in areas of the city with higher relative daytime summer surface temperature and less likely among residents living in areas with more green space. Air conditioning prevalence also varies among New York City neighborhoods (NYC DOHMH, 2007).
Understanding within-city vulnerability can help guide efforts to prevent heat-related deaths, including urban planning measures that apply susceptibility and exposure information to prioritize urban heat island reduction efforts, public messaging during heat waves, and provision of air conditioners and electric power subsidies (Lane et al., 2013b).
At-home deaths could be a marker of social isolation, lack of mobility, or both. In previous major heat waves in Chicago (1995) and Paris (2003), social isolation and lack of mobility were determined to be major risk factors for death (Semenza et al., 1996; Vandentorren et al., 2006). Public-awareness campaigns on the dangers posed by extreme heat events could help encourage New Yorkers to check in on neighbors and relatives who may be particularly vulnerable.
The burden of heat-related mortality experienced by socioeconomically disadvantaged populations is likely the result of a complex interplay of factors, but one explanatory factor is the lack of access to air conditioning. A recent telephone survey indicated that approximately 11% of New Yorkers do not have a functioning air conditioner, and an additional 14% do not use their air conditioner regularly (Lane et al., 2013b). The most frequently cited reason for lack of air conditioning ownership was cost, followed by the perception that it was not needed and a dislike of air conditioning. In addition to making air conditioning and cooling centers accessible, emphasis also needs to be placed on educating New York City residents on heat health risks and how they can be alleviated.
Climate health indicators are measurable characteristics that potentially offer tools to track or give early warning of more complex health-relevant climate conditions. Some of the top-priority proposed health indicators for New York City and the New York metropolitan region that emerged from NPCC2 discussions are shown in Table 5.1 with a complete listing in Appendix IIE (NPCC, 2015).
Table 5.1.
Proposed priority Climate–Health Indicators for New York City (see Appendix IIE (NPCC, 2015) for detailed, complete set of suggested indicators).
| Climate hazard | Type of indicator | Indicator |
|---|---|---|
| Heat | Health outcome |
|
| Heat | Vulnerability |
|
| Power outages | Health outcome |
|
| Extreme weather | Health outcome |
|
| Coastal storms/floods | Vulnerability |
|
| Heat, power outages | Vulnerability |
|
| All | Vulnerability |
|
Improving health resilience to heat extremes
A range of measures is available to reduce heat-health risks before and during extreme heat events.g
Programs are needed to enhance availability of air conditioning for people who are most vulnerable to heat
They should also aim to improve energy efficiency, curtail wasteful use of air conditioning in overcooled spaces, implement urban heat island mitigation measures, and reduce overall citywide power demand during heat waves. A lack of air conditioning at home increases the risk of heat-related death (O’Neill et al., 2005). However, air conditioning also contributes to higher electrical demand during heat waves, which increases the risk of power disruptions or blackouts and increases emissions of greenhouse gases.
The city operates large numbers of cooling shelters during heat emergencies, although a relatively small proportion of vulnerable New Yorkers use them (Lane et al., 2013b). It is therefore especially important to identify and enhance outreach to assist vulnerable individuals—those who are old, sick, and poor—with getting to a cool place or staying cool at home. This can operate through caregivers, community organizations, neighbors, and so on. Improved health education around heat extremes will assist in this regard.
Urban-scale cooling strategies are needed
Because green spaces reduce local temperatures (Harlan et al., 2006), tree planting can be an important strategy for urban cooling, especially when targeted to vulnerable neighborhoods. Green and light-colored roofs are additional strategies with potential for local cooling. Several ongoing New York City programs are contributing to reducing impacts of the urban heat islandh (see Chapter 6, NPCC, 2015).
The development and application of a heat-health vulnerability index, mapped to the block level, can help to target urban heat interventions
In the longer term, building design standards can be revised to reduce heat load related to facades and other building treatments and improve passive ventilation and thermal performance, especially during power outages.
Health resiliency during extreme heat events depends on a well-functioning electrical grid. Robust electrical infrastructure, especially in vulnerable neighborhoods and public housing, is thus essential.
5.3. Air pollution, aeroallergens, and vector-borne, water-borne, and food-borne diseases
New York City residents face a variety of climate-related health impacts in addition to the direct effects of storms and extreme heat. Four important additional risks are air pollution, aeroallergens, vector-borne diseases, and water and food-borne diarrheal illnesses.
Air pollution
Climate change has the potential to increase morbidity and mortality from respiratory and cardiovascular causes through its effects on air pollution. Respiratory diseases such as childhood asthma are a major public health challenge in New York City, and cardiovascular disease is the most common cause of death in New York State (NYC DOHMH, 2003; U.S. CDC, 2008). In 2008, asthma prevalence among children in New York State was 10.8% compared to 9.4% in the United States as a whole (U.S. CDC, 2010, 2011). Within New York City, asthma prevalence varies dramatically among neighborhoods, with the prevalence of asthma among children under the age of 5 in New York City neighborhoods varying from 3% to 19% (NYC DOHMH, 2003).
An important air pollutant in the context of climate change is ground-level ozone, which is produced on hot, sunny days from a combination of nitrogen oxides, carbon monoxide, and volatile organic compounds. Ozone production is dependent on temperature and the presence of sunlight, with higher temperatures and still, cloudless days leading to increased production. Thus, ground-level ozone concentrations have the potential to increase in some regions in response to climate change (Ebi and McGregor, 2008; Tsai et al., 2008; Cheng et al., 2011; Polvani et al., 2011; Hogrefe et al., 2004).
Exposure to ozone is associated with decreased lung function, increased premature mortality, increased cardiopulmonary mortality, increased hospital admissions, and increased emergency room visits (Dennekamp and Carey, 2010; Kampa and Castanas, 2008; Kinney, 2008; Smith et al., 2009). In New York City, ozone-related emergency room visits for asthma among children under the age of 18 have been projected to rise by 7.3% by the 2020s versus the 1980s as the result of climate change-induced increases in ozone concentrations (Sheffield et al., 2011a). The New York Climate and Health Project, a multidisciplinary study of climate change and human health in the New York metropolitan area, reported potential increases in ozone-related deaths in New York City ranging from 4% to 6% across the five boroughs by 2050 (Fig. 5.6) (Knowlton et al., 2008).
Figure 5.6.
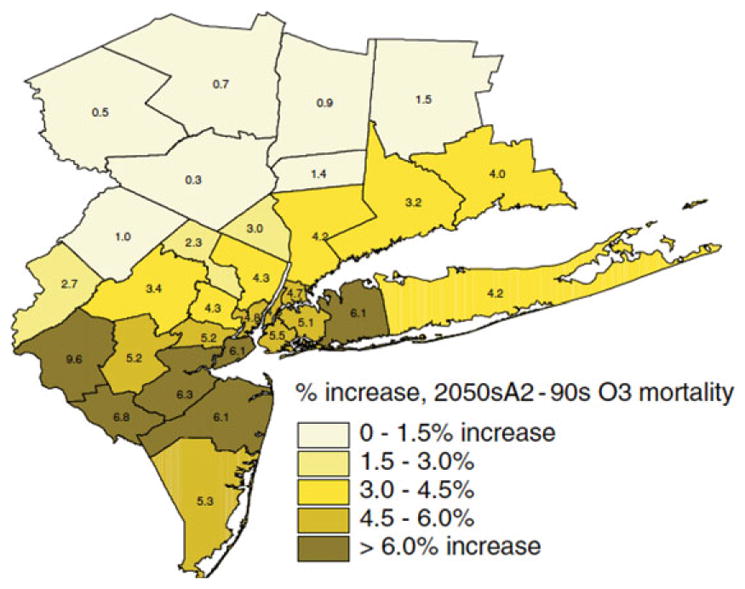
Percentage change in ozone-related deaths projected for the decade of the 2050s under a rapid climate change scenario. Increases of between 4% and 6% were projected for the New York metropolitan region. Source: Knowlton et al. (2008).
Particulate matter (PM) is another important air pollutant in New York City from a human health perspective. The most health-relevant PM is emitted by the combustion of fuels—by cars, diesel vehicles, power plants, and heating systems. Combustion particles are small enough to penetrate deep into lungs and contain toxic components. Some kinds of PM, such as black carbon or soot particles, also affect the climate further by darkening ice and snow, thereby increasing temperatures through greater absorption of solar radiation. Power plant emissions may rise with increased power demands in response to warming temperatures. Thus, controlling PM sources can provide a double benefit in terms of both health and climate.
Both climate adaptation measures to improve resilience, such as increased air conditioner use, and mitigation measures (i.e., efforts to reduce atmospheric greenhouse gas concentrations), such as building weatherization and energy efficiency measures, can have impacts on indoor air quality and human health. On the positive side, air conditioning tends to diminish indoor penetration of outdoor ozone and pollens. However, tighter buildings reduce air exchange between indoors and outdoors, and tighter buildings can increase exposures to pollutants generated indoors, such as second-hand cigarette smoke, NO2 from gas stoves, and indoor allergens.
Aeroallergens
Exposure to certain types of airborne pollen is associated with multiple allergic outcomes, including allergic sensitization to pollen (Bjorksten et al., 1980; Porsbjerg et al., 2002; Kilhström et al., 2003), exacerbation of hay fever (Cakmak et al., 2002; Villeneuve et al., 2006; Sheffield et al., 2011a), and exacerbation of allergic asthma (Delfino et al., 2010; Darrow et al., 2012). Recent work has shown that several tree-pollen genera that are present in midspring—particularly birch, sycamore, and ash—are important drivers of allergic disease in the New York City population (Dr. Kazuhiko Ito, personal communication).
Pollen timing and amount are sensitive to climate change because both pollen production and release are linked to temperature and precipitation in the months prior to the pollen season (Reiss and Kostic, 1976; U.S. EPA, 2008; Sheffield et al., 2011c). The duration of the pollen season has already been demonstrated to be lengthening for certain species (Emberlin et al., 2002; Ziska et al., 2011). Pollen is also directly increased by rising CO2 concentrations due to CO2 fertilization (Ziska and Caulfield, 2000; Ziska et al., 2003; Singer et al., 2005). Studies in Europe have shown advances in the start date of the tree pollen season by as much as 23 days over the last two to three decades of recent warming (Emberlin et al., 2002). In central North America, the length of the ragweed season has increased by as much as 27 days between 1995 and 2009 (especially in more northern latitudes) in association with rising temperatures and later first-frost dates (Ziska et al., 2011). Urban areas such as New York City may experience further influences on the length and severity of the pollen season from the urban heat island effect and locally higher CO2 concentrations (Ziska et al., 2003). In addition, exposure to air pollutants common in urban areas such as diesel exhaust particles can enhance allergic response to pollens (Diaz-Sanchez et al., 1997, 1999; D’Amato and Cecchi, 2008; D’Amato et al., 2010). As a result, future changes in temperature and CO2 could lead to changes in the dynamics of the pollen season and potentially increase the morbidity of allergic diseases such as asthma.
Urban forests provide important environmental and social goods and can support both climate change mitigation and adaptation goals. Research is ongoing concerning relations among urban tree density and species distribution, ambient pollen concentrations, and human health. Trees can also be an important source of volatile organic compounds (VOCs), which are precursors to ozone. Evolving knowledge from this work should inform future policy and practice, including urban tree-planting programs such as MillionTreesNYC, while taking into consideration that tree species are also sensitive to changing climate conditions.
Other aeroallergens such as mold also contribute to the burden of respiratory and allergic disease and have been linked to indoor air quality (IAQ) and climate change (IOM, 2011). Increased temperatures, coastal flooding, and heavy precipitation events can present ideal conditions for the growth of mold and other fungi in the indoor environment (Fisk et al., 2007; Mudarri and Fisk, 2007; Wolf et al., 2010; Spengler, 2012) (see Section 5.1, above).
Vector-borne diseases
Vector-borne diseases are spread by organisms such as ticks and mosquitoes. Cases of several types of vector-borne diseases have been reported in New York State, including Lyme disease, West Nile virus, and dengue fever (Knowlton et al., 2009; Centers for Disease Control and Prevention, 2013a). Vector-borne disease incidence is influenced by climate factors such as temperature and precipitation, on multiple timescales. For example, there is evidence that the Lyme disease vector, the tick species Ixodes scapularis, has expanded its range northward into Canada over the last several decades in part due to warming temperatures (Ogden et al., 2009, 2010). Thus, climate change may lead to changes in the seasonal cycle and spatial distribution of some vector-borne diseases or even expand their ranges, although it is important to note that climate is only one of many drivers of vector-borne disease distribution (Lafferty, 2009; McGregor, 2012; Wilson, 2009).
Water- and food-borne illnesses
Humans can be exposed to water- and food-borne pathogens through a variety of routes, including through the consumption of polluted drinking water and ingestion of contaminated food (Rose et al., 2001). A number of pathogens that cause water and food-borne illnesses in humans are sensitive to projected climate parameters, including increased temperature, changing precipitation patterns, more frequent extreme precipitation events, and associated changes in seasonal patterns in the hydrological cycle. Although specific relationships vary by pathogen, increased temperatures appear to increase the incidence of common North American diarrheal diseases such as campylobacteriosis and salmonellosis (Curriero et al., 2001; European Centre for Disease Prevention and Control, 2012; Semenza et al., 2012). Water-borne illnesses from exposures to pathogens in recreational waters increase in the hours after extreme rainfall events and are projected to increase in the Great Lakes region as climate change continues (Patz et al., 2008).
Improving resilience to public health threats
Air pollution
Because ozone production is especially sensitive to warming temperatures, strategies to control anthropogenic emissions of ozone precursors, including nitrogen oxides from vehicles and other fuel-combustion sources, and volatile organic compounds from fuel storage and refueling operations, will be more important than ever in a changing climate. New York City and surrounding regions are frequently exposed to unhealthy levels of ozone concentrations and other air pollutants.i Because of the regional nature of ozone, success in reducing episodic ozone concentrations necessitates a regional approach via cooperation with upwind states and cities. New York City should also consider enhancing early-warning systems for forecasted air pollution episodes, keeping in mind the potential compounding influences of heat waves and ozone precursors.
Aeroallergens
In the short term, health impacts from earlier or more severe pollen seasons can be potentially reduced by early-warning systems that inform patients and health-care providers at the start of the pollen season so they have adequate supplies of allergy and asthma medications. Populations who lack access to primary care need to be reached through other means. New York City should include allergenicity as a criterion for species selection in future tree-planting programs.
Vector-borne diseases
eillance of infected disease vectors is an integral part of health systems to enhance resilience to risks, including networks to routinely trap and analyze vector organisms such as mosquitos and ticks. Long-term surveillance of vectors should take place not only in areas where they are known to exist but also in areas where they may expand to in a warming climate in order to assess range expansion as well as the introduction of invasive species. Health professionals and the general public need to be educated about the signs and symptoms of now-rare diseases that may occur more often with projected climate change, such as dengue fever. Mosquito vector control can be enhanced via the reduction of standing water and community education about the importance of reducing it.
Water- and food-borne illnesses
Continued and enhanced protection of New York City’s watershed in the face of changing development, temperature, and precipitation patterns will be essential to ensuring an adequate supply of fresh water over the coming decades. Stormwater drainage is another critical infrastructure system in New York City. Extreme rain events can overwhelm the capacity of the combined sewer system, leading to direct contamination of surrounding waters by untreated sewage. Efforts to retain and slow the drainage of storm water via green infrastructure can address this problem to some extent (Rosenzweig et al., 2011). Assessments of the water quality and heat island benefits of these initiatives are needed.
5.4. Research recommendations
Further knowledge generation will be essential for New York City to anticipate and avoid future health impacts from extreme weather events in a changing climate. To promote research that has the greatest potential value for resiliency planning, it is recommended that a climate-health partnership involving local university researchers and city practitioners be established and supported. Recognizing that information needs will evolve over time, the NPCC2 Health Work Group identified a set of immediate areas in which research knowledge is needed.
Specific near-term research recommendations include
Evaluate and quantify the efficacy of cool roofs and other urban heat island mitigation measures for public health protection.
Understand the factors (structural, behavioral, etc.) that lead to unhealthy levels of exposure to heat inside New York City apartment buildings, where most deaths occur during heat events.
Develop vulnerability indicators of health risks from both coastal storms and extreme heat events that can be applied at fine spatial (e.g., block or neighborhood) scales to target resiliency initiatives.
Examine risks of coupled extreme events. Worst-case health impacts could occur when multiple climate-related extreme events happen simultaneously or in rapid succession, for example, a heat event followed by a coastal storm and/or an air pollution episode. Research is needed to examine these scenarios, quantify their probabilities and health impacts, and devise response strategies.
Conduct studies that couple infrastructure system failures with human health impacts. Analysis and quantification of linkages between critical infrastructure systems and human health would provide essential information for risk planning in New York City.
Evaluate expansion of the current syndromic heat-illness surveillance program, a NYC DOH initiative that tracks emergent cases of heat-related illnesses at hospitals, to more locations in the New York metropolitan region to aid in early warning for communities with disproportionate heat-health burdens.
Analyze and quantify potential health co-benefits and possible negative consequences of climate adaptation and mitigation measures at the local level in New York City, including effects on indoor air quality. Take actions to mitigate greenhouse gas emissions and adapt to warming temperatures that result in reductions in air pollution or changes in other health-relevant factors such as increased green space or physical activity.
5.5. Resiliency recommendations
In reviewing the current knowledge base on climate impacts and vulnerability in New York City, we identify several opportunities for further resiliency planning. These generally fall within the broad categories of engagement with preparedness planning; enhancement of social networks and linkages; and evaluation of existing resilience efforts with a health lens.
Coastal storms
New York City has a number of programs and initiatives under way to build resilience to more intense coastal flooding in response to projected climate change effects on sea level rise and storm surge. Strategies addressing community preparedness and infrastructure measures are described in the City’s Hurricane Sandy After Action Report, the NYC Hazard Mitigation Plan, and A Stronger, More Resilient New York.j
The NPCC2 Health Workgroup highlighted short-term and long-term recommendations to build health-related coastal storm resilience in New York City.
Short-term resilience strategies include:
Enhance communications to vulnerable sites, neighborhoods, and populations. This should draw on baseline surveys of locational risks including industrial waste sites, concentrations of at-risk or isolated populations, neighborhoods with infrastructure problems and locations (e.g., schools and daycare centers that often become shelters). Working with leaders in the most vulnerable communities and at-risk populations, the City should conduct flood emergency drills and practices, prioritizing public housing.
Leverage local community-based organizations, social networks, and business leaders in designing effective targeted responses. Businesses and community-based organizations that assess baseline vulnerability should evaluate potential hazardous exposures and disproportionate health impacts immediately postflooding. Rapid-response teams that assess pre- and post-storm impacts and infrastructure breakdowns in highly vulnerable neighborhoods should include community groups, social networks, and health and safety professionals.
Infrastructure improvements for longer-term flood resiliency include:
Assess public health aspects of New York City’s resiliency plan. The city’s resiliency investments in critical infrastructure are crucial—not only to prevent future damage and promote faster recovery but also for protecting against adverse health impacts from these events. It is important to understand the complex linkages between infrastructure and health in New York City and to use this knowledge to anticipate and account for the health improvements that can be achieved via infrastructure investments.
Heat events
Although some programs are already in place to adapt to more frequent, intense, and longer-lasting heat waves in New York City, several preparedness gaps have been identified.
Recommendations for short-term resilience strategies to enhance heat-wave preparedness in New York City include:
Enhance communication before heat waves, targeting those most at risk. Heat-risk awareness should be targeted to vulnerable populations and their caregivers (e.g., doctors, teachers, meals-on-wheels programs) and include pharmacists who should provide information about heat-health risks when they disperse medications that increase susceptibility to heat illness.
During heat waves, ensure access to cool indoor spaces while avoiding power outages. Approaches to increasing use of cooling centers in high-risk areas should be considered. Consideration should also be given to the needs of people who are unable to travel to cooling centers. Neighbor look-in programs to check on people at risk from heat stress should be activated.
Develop robust public messaging that promotes use of air conditioning by those who are vulnerable while discouraging excessive cooling of residential and commercial spaces. Ample evidence exists of the benefits of air conditioning for people most vulnerable to heat-related health risks.
Expand use of multimedia to reduce vulnerabilities. Wider use of mobile devices, social media, and mainstream media to disseminate heat warnings can help reduce health risks, especially for prolonged heat waves and complex disasters.
Recommendations for longer-term resilience strategies that could enhance New York City’s heat-wave preparedness include:
Conduct urban heat island vulnerability assessments. Develop a combined heat vulnerability index that includes local exposures and susceptibilities to target and prioritize urban heat island interventions in the hottest city neighborhoods and perform before/after health outcome evaluations.
Develop programs for built environment upgrades to increase green spaces, making sure all buildings have windows that can open and provide air conditioners to those who need relief from heat but cannot afford the cost of purchase or operation.
Improve energy resilience of the power grid by increasing energy efficiency and using alternative energy sources for cooling, especially in vulnerable neighborhoods and public housing. To reduce electrical load, the City should combine heat island mitigation (white roofs, greening, etc.), efficiency improvements, expanded marketing of voluntary conservation measures (such as setting thermostats to avoid excessive cooling), and promoting—in collaboration with electric utilities—expanded participation in load-shaving programs.
5.6. Looking ahead
New York City is in the fortunate position of having a wealth of research capacity for projecting how climate change will affect flooding and extreme heat conditions locally. These NPCC2 projections afford the city a certain independence from relying on federal agency sources for these data. However, it is increasingly important for federal agencies to provide a national source of locally relevant information on the effects of climate change (Parris, 2014). The inclusion of sea level rise in FEMA’s flood risk maps is one example.k One pathway for provision of regionally focused climate information is NOAA’s Regional Integrated Science and Assessment (RISA) network. In particular, the NOAA-funded Consortium for Climate Risks in the Urban Northeast (CCRUN) is a source of climate information for urban decision-makers in the northeastern states.l
To advance the recommendations in this chapter, New York City should improve its ability to monitor and evaluate the ongoing local effects of climate change on the public’s health (see Chapter 6 of NPCC, 2015). This means establishing networks to monitor climate-health indicators, such as emergency room visits and hospital admissions for heat illness, or injuries and deaths due to extreme weather events, and actively supporting their operation and long-term maintenance in New York City and the surrounding metropolitan region. Other important data needs relate to expanded monitoring of pollen levels and disease vectors over time and space in New York City. Gathering information on these health indicators should become part of the City’s standard operating procedure. This will establish baselines and build a suite of city- and neighborhood-specific climate-health indicators for analysis of trends over time.
Footnotes
The NYC-EJA is a nonprofit New York City–wide membership network linking grassroots organizations from low-income communities of color in their struggle for environmental justice. NYC-EJA coalesces its member organizations around common issues to advocate for improved environmental conditions and against inequitable burdens by coordinating campaigns designed to affect City and State policies. The Waterfront Justice Project is an advocacy campaign created by NYC-EJA to (1) research potential threats affecting industrial waterfront communities based on local vulnerabilities; (2) identify proactive policies and programs to promote climate resiliency that reflect local priorities; and (3) convene local communities, government agencies, and private-sector representatives to share priorities and resources. Current members include UPROSE (Southwest Brooklyn), El Puente (North Brooklyn); Morningside Heights-West Harlem Sanitation Coalition (Upper Manhattan); Nos Quedamos (South Bronx); The Point CDC (South Bronx); Youth Ministries for Peace & Justice (South Bronx); and Sustainable South Bronx (South Bronx). For more information see: http://www.nyc-eja.org.
Recommendations regarding improving health resiliency to coastal storms were distilled from discussions that occurred during the December 13, 2013 NPCC2 Health Workshop held at Columbia University’s Mailman School of Public Health.
Includes lightning, tornados, floods, hurricanes, and cold snaps.
The heat index (HI) or “apparent temperature” is an approximation of how hot it “feels” for a given combination of air temperature and relative humidity (American Meteorological Society, 2013).
Here we summarize suggestions discussed at the December 13, 2013, NPCC2 Health Workshop held at Columbia University’s Mailman School of Public Health.
NYC Cool Roofs (http://www.nyc.gov/html/coolroofs/html/home/home.shtml); MillionTreesNYC (http://www.milliontreesnyc.org/html/home/home.shtml); Green Infrastructure Plan (http://www.nyc.gov/html/dep/html/stormwater/nyc_green_infrastructure_plan.shtml).
Hurricane Sandy After Action Report (City of New York, 2013), Hazard Mitigation Plan (City of New York, 2014), and A Stronger, More Resilient New York (City of New York, 2013).
References
- Anderson BG, Bell ML. Weather-related mortality: how heat, cold, and heat waves affect mortality in the United States. Epidemiology. 2009;20:205–213. doi: 10.1097/EDE.0b013e318190ee08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson GB, Bell ML. Lights out: impact of the August 2003 power outage on mortality in New York, NY. Epidemiology. 2012;23:189–193. doi: 10.1097/EDE.0b013e318245c61c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arrieta MI, Foreman RD, Crook ED, Icenogle ML. Providing continuity of care for chronic diseases in the aftermath of Katrina: from field experience to policy recommendations. Disaster Med Publ Health Prep. 2009;3:174–182. doi: 10.1097/DMP.0b013e3181b66ae4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbeau DN, Grimsley LF, White LE, et al. Mold exposure and health effects following Hurricanes Katrina and Rita. Annu Rev Publ Health. 2010;31:165–178. doi: 10.1146/annurev.publhealth.012809.103643. [DOI] [PubMed] [Google Scholar]
- Barnett AG. Temperature and cardiovascular deaths in the US elderly: changes over time. Epidemiology. 2007;18:369–372. doi: 10.1097/01.ede.0000257515.34445.a0. [DOI] [PubMed] [Google Scholar]
- Basu R, Samet JM. Relation between elevated ambient temperature and mortality: a review of the epidemiologic evidence. Epidemiol Rev. 2002;24:190–202. doi: 10.1093/epirev/mxf007. [DOI] [PubMed] [Google Scholar]
- Basu R, Feng WY, Ostro BD. Characterizing temperature and mortality in nine California counties. Epidemiology. 2008;19:138–145. doi: 10.1097/EDE.0b013e31815c1da7. [DOI] [PubMed] [Google Scholar]
- Basu R, Malig B, Ostro B. High ambient temperature and the risk of preterm delivery. Am J Epidemiol. 2010;172:1108–1117. doi: 10.1093/aje/kwq170. [DOI] [PubMed] [Google Scholar]
- Bautista E, Hanhardt E, Osorio JC, Dwyer N. New York City Environmental Justice Alliance Waterfront Justice Project. Local Environment. 2014:1–19. [Google Scholar]
- Beatty ME, Phelps S, Rohner C, Weisfuse I. Blackout of 2003: public health effects and emergency response. Public Health Reports. 2006;121:36–44. doi: 10.1177/003335490612100109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjorksten F, Suoniemi I, Koski V. Neonatal birch-pollen contact and subsequent allergy to birch pollen. Clin Exp Allergy. 1980;10:585–591. doi: 10.1111/j.1365-2222.1980.tb02140.x. [DOI] [PubMed] [Google Scholar]
- Cakmak S, Dales RE, Burnett RT, et al. Effect of airborne allergens on emergency visits by children for conjunctivitis and rhinitis. Lancet. 2002;359:947–948. doi: 10.1016/S0140-6736(02)08045-5. [DOI] [PubMed] [Google Scholar]
- Carson C, Hajat S, Armstrong B, Wilkinson P. Declining vulnerability to temperature-related mortality in London over the 20th century. Am J Epidemiol. 2006;164:77–84. doi: 10.1093/aje/kwj147. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (U.S. CDC) Current asthma prevalence percents by age, United States: National Health Interview Survey, 2008. 2010 Available online at http://www.cdc.gov/asthma/nhis/08/table4-1.htm.
- Centers for Disease Control and Prevention (U.S. CDC) Asthma in New York state. 2011 Available online at http://www.cdc.gov/asthma/stateprofiles/Asthma_in_NYS.pdf.
- Centers for Disease Control and Prevention (U.S. CDC) New York: Burden of Chronic Diseases; 2013a. Available online at http://www.cdc.gov/chronicdisease/states/pdf/new_york.pdf. [Google Scholar]
- Centers for Disease Control and Prevention (U.S. CDC) Current asthma prevalence percents by age, United States: National Health Interview Survey 2008. 2013b Available online at http://www.cdc.gov/asthma/nhis/08/table4-1.htm.
- Centers for Disease Control and Prevention (U.S. CDC) Heat Illness and Deaths – New York City, 2000–2011. 2013c Available online at http://www.cdc.gov/mmwr/pdf/wk/mm6231.pdf.
- Centers for Disease Control and Prevention (U.S. CDC) Asthma in New York State. 2014a Available online at http://www.cdc.gov/asthma/stateprofiles/Asthma_in_NYS.pdf.
- Centers for Disease Control and Preventation (U.S. CDC) Environmental Public Health Tracking. 2014b Available online at http://ephtracking.cdc.gov/showIndicatorsData.action.
- Cheng CH, Huang SF, Teoh HJ. Predicting daily ozone concentration maxima using fuzzy time series based on a two-stage linguistic partition method. Comput Math Appl. 2011;62:2016–2028. [Google Scholar]
- City of New York. A Stronger, More Resilient. New York: 2013. Healthcare. [Google Scholar]
- City of New York. Hurricane Sandy After Action Report: Report and recommendations to Mayor Michael R. Bloomberg. 2013. [Google Scholar]
- City of New York. City of New York, Hazard Mitigation Plan. 2014. [Google Scholar]
- Confalonieri U, et al. Human health. In: Parry ML, Canziani OF, Palutikof JP, et al., editors. Climate Change 2007: Impacts, Adaptation, and Vulnerability. Contribution of Working Group II to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge: Cambridge University Press; 2007. pp. 391–431. [Google Scholar]
- Curriero FC, Patz JA, Rose JB, Lele S. The association between extreme precipitation and waterborne disease outbreaks in the United States, 1948–1994. Am J Epidemiol. 2001;91:1194–1199. doi: 10.2105/ajph.91.8.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curriero FC, Heiner KS, Samat JM, et al. Temperature and mortality in 11 cities of the eastern United States. Am J Epidemiol. 2002;155:80–87. doi: 10.1093/aje/155.1.80. [DOI] [PubMed] [Google Scholar]
- D’Amato G, Cecchi L. Effects of climate change on environmental factors in respiratory allergic diseases. Clin Exp Allergy. 2008;38:1264–1274. doi: 10.1111/j.1365-2222.2008.03033.x. [DOI] [PubMed] [Google Scholar]
- D’Amato G, Cecchi L, D’Amato M, Liccardi G. Urban air pollution and climate change as environmental risk factors of respiratory allergy: an update. J Invest Allergol Clin Immunol. 2010;20:95–102. [PubMed] [Google Scholar]
- Darrow LA, Hess J, Rogers CA, et al. Ambient pollen concentrations and emergency department visits for asthma and wheeze. J Allergy Clin Immunol. 2012;130:630–638. doi: 10.1016/j.jaci.2012.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delfino RJ, Zeiger RS, Seltzer JM, et al. Association of asthma symptoms with peak particulate air pollution and effect modification by anti-inflammatory medication use. Environ Health Perspect. 2002;110:A607–A617. doi: 10.1289/ehp.021100607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delfino RJ, Staimer N, Tjoa T, et al. Associations of primary and secondary organic aerosols with airway and systemic inflammation in an elderly panel cohort. Epidemiology. 2010;21:892–902. doi: 10.1097/EDE.0b013e3181f20e6c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennekamp M, Carey M. Air quality and chronic disease: why action on climate change is also good for health. NSW Public Health Bull. 2010;21:115–121. doi: 10.1071/NB10026. [DOI] [PubMed] [Google Scholar]
- Diaz-Sanchez D, Tsein A, Fleming J, Saxon A. Combined diesel exhaust particulate and ragweed allergen challenge markedly enhances human in vivo nasal ragweed-specific IgE and skews cytokine production to a T helper cell 2-type pattern. J Immunol. 1997;158:2406–2413. [PubMed] [Google Scholar]
- Diaz-Sanchez D, Garcia MP, Wang M, et al. Nasal challenge with diesel exhaust particles can induce sensitization to a neoallergen in the human mucosa. J Allergy Clin Immunol. 1999;104:1183–1188. doi: 10.1016/s0091-6749(99)70011-4. [DOI] [PubMed] [Google Scholar]
- Ebi KL, McGregor G. Climate change, tropospheric ozone and particulate matter, and health impacts. Environ Health Perspect. 2008;116:1449–1455. doi: 10.1289/ehp.11463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis FP, Nelson F. Mortality in the elderly in a heat wave in New York City, August 1975. Environ Res. 1978;15:504–512. doi: 10.1016/0013-9351(78)90129-9. [DOI] [PubMed] [Google Scholar]
- Emberlin J, Detandt M, Gehrig R, et al. Responses in the start of Betula (birch) pollen seasons to recent changes in spring temperatures across Europe. Int J Biometeorol. 2002;46:159–170. doi: 10.1007/s00484-002-0139-x. [DOI] [PubMed] [Google Scholar]
- European Center for Disease Control and Prevention. Assessing the potential impacts of climate change on food- and waterborne diseases in Europe. 2012. [Google Scholar]
- Finlay SE, Moffat A, Gazzard R, et al. Health impacts of wildfires. PLoS Currents. 2012;4 doi: 10.1371/4f959951cce2c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisk WJ, Lei-Gomez Q, Mendell MJ. Meta-analyses of the associations of respiratory health effects with dampness and mold in homes. Indoor Air. 2007;17:284–296. doi: 10.1111/j.1600-0668.2007.00475.x. [DOI] [PubMed] [Google Scholar]
- French J, Ing R, Allmen SV, Wood R. Mortality from flash floods: a review of national weather service reports, 1969–81. Public Health Rep. 1983;98:584–588. [PMC free article] [PubMed] [Google Scholar]
- Galea S, et al. Exposure to hurricane-related stressors and mental illness after Hurricane Katrina. Arch Gen Psychiatry. 2007;64:1427–1434. doi: 10.1001/archpsyc.64.12.1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutiérrez E, González JE, Bornstein R, et al. A new modeling approach to forecast building energy demands during extreme heat events in complex cities. J Sol Energy Eng. 2013;135:040906. [Google Scholar]
- Handmer J, et al. Changes in impacts of climate extremes: human systems and ecosystems. In: Field CB, et al., editors. Managing the Risks of Extreme Events and Disasters to Advance Climate Change Adaptation. A Special Report of Working Grouips I and II of the Intergovernmental Panel on Climate Change. Cambridge: Cambridge University Press; 2012. pp. 231–290. [Google Scholar]
- Harlan SL, Brazel AJ, Prashad L, et al. Neighborhood microclimates and vulnerability to heat stress. Soc Sci Med. 2006;63:2847–2863. doi: 10.1016/j.socscimed.2006.07.030. [DOI] [PubMed] [Google Scholar]
- Hogrefe C, Lynn B, Civerolo K, Ku JY, et al. Simulating changes in regional air pollution over the eastern United States due to changes in global and regional climate and emissions. Journal of Geophysical Research: Atmospheres. 2004;109:D22301. [Google Scholar]
- Hsiang SM, Burke M, Miguel E. Quantifying the influence of climate on human conflict. Science. 2013;341:1235367. doi: 10.1126/science.1235367. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (IOM) Climate Change, the Indoor Environment, and Health. Washington, DC: National Academies Press; 2011. [Google Scholar]
- IPCC. 2012: Managing the Risks of Extreme Events and Disasters to Advance Climate Change Adaptation. In: Field CB, Barros V, Stocker TF, Qin D, Dokken DJ, Ebi KL, Mastrandrea MD, Mach KJ, Plattner G-K, Allen SK, Tignor M, Midgley PM, editors. A Special Report of Working Groups I and II of the Intergovernmental Panel on Climate Change. Cambridge University Press; Cambridge, UK, and New York, NY, USA: p. 582. [Google Scholar]
- Ito K, Mathes R, Ross Z, et al. Fine Particulate Matter Constituents Associated with Cardiovascular Hospitalizations and Mortality in New York City. Environmental health perspectives. 2010;119:467–473. doi: 10.1289/ehp.1002667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaakkola JJK, Hwang BF, Jaakkola N. Home dampness and molds, parental atopy, and asthma in childhood: a six-year population-based cohort study. Environ Health Perspect. 2005;113:357–361. doi: 10.1289/ehp.7242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jonkman SN, Kelman I. An analysis of the causes and circumstances of flood disaster deaths. Disasters. 2005;29:75–97. doi: 10.1111/j.0361-3666.2005.00275.x. [DOI] [PubMed] [Google Scholar]
- Kampa M, Castanas E. Human health effects of air pollution. Environ Pollution. 2008;151:362–367. doi: 10.1016/j.envpol.2007.06.012. [DOI] [PubMed] [Google Scholar]
- Kihlström A, Lilja G, Pershagen G, Hedlin G. Exposure to high doses of birch pollen during pregnancy, and risk of sensitization and atopic disease in the child. Allergy. 2003;58:871–877. doi: 10.1034/j.1398-9995.2003.00232.x. [DOI] [PubMed] [Google Scholar]
- Kinney PL. Climate change, air quality, and human health. Am J Prev Med. 2008;35:459–467. doi: 10.1016/j.amepre.2008.08.025. [DOI] [PubMed] [Google Scholar]
- Kistemann T, Rechenburg A, Höser C, et al. Assessing the potential impacts of climate change on food- and waterborne diseases in Europe 2012 [Google Scholar]
- Klein KR, Nagel NE. Mass medical evacuation: Hurricane Katrina and nursing experiences at the New Orleans airport. Disaster Manage Resp. 2007;5:56–61. doi: 10.1016/j.dmr.2007.03.001. [DOI] [PubMed] [Google Scholar]
- Klinenberg E. Heat wave: a social autopsy of disaster in Chicago. Chicago: University of Chicago Press; 2002. [DOI] [PubMed] [Google Scholar]
- Knowlton K, Solomon G, Rotkin-Ellman M. Natural Resources Defense Council (July 2009 Issue Paper) 2009. Fever pitch: Mosquito-borne dengue fever threat spreading in the Americas; p. 22. [Google Scholar]
- Knowlton K, Hogrefe C, Lynn B, et al. Impacts of heat and ozone on mortality risk in the New York City metropolitan region under a changing climate. In: Thomson MC, Garcia-Herrera R, Benniston M, editors. Seasonal Forecasts, Climatic Change and Human Health. Dordrecht: Springer Netherlands; 2008. pp. 143–160. [Google Scholar]
- Knowlton K, Rotkin-Ellman M, King G, et al. The 2006 California heat wave: impacts on hospitalizations and emergency department visits. Environ Health Perspect. 2009;117:61–67. doi: 10.1289/ehp.11594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knowlton K, et al. Assessing ozone-related health impacts under a changing climate. Environ Health Perspect. 2004;112:1557–1563. doi: 10.1289/ehp.7163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lafferty KD. The ecology of climate change and infectious diseases. Ecology. 2009;90:888–900. doi: 10.1890/08-0079.1. [DOI] [PubMed] [Google Scholar]
- Lane K, Charles-Guzman K, Wheeler K, et al. Health effects of coastal storms and flooding in urban areas: a review and vulnerability assessment. J Environ Public Health. 2013a;15:1–13. doi: 10.1155/2013/913064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane K, et al. Extreme heat awareness and protective behaviors in New York City. J Urban Health. 2013b;91:403–414. doi: 10.1007/s11524-013-9850-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavell A, Oppenheimer M, Diop C, et al. 2012: Climate change: new dimensions in disaster risk, exposure, vulnerability, and resilience. In: Field CB, Barros V, Stocker TF, Qin D, Dokken DJ, Ebi KL, Mastrandrea MD, Mach KJ, Plattner G-K, Allen SK, Tignor M, Midgley PM, editors. Managing the Risks of Extreme Events and Disasters to Advance Climate Change Adaptation. Cambridge University Press; Cambridge, UK, and New York, NY, USA: pp. 25–64. A Special Report of Working Groups I and II of the Intergovernmental Panel on Climate Change (IPCC) [Google Scholar]
- Le Tertre A, et al. Impact of the 2003 heatwave on all-cause mortality in 9 French cities. Epidemiology. 2006;17:75–79. doi: 10.1097/01.ede.0000187650.36636.1f. [DOI] [PubMed] [Google Scholar]
- Li T, Horton RM, Kinney PL. Projections of seasonal patterns in temperature-related deaths for Manhattan, New York. Nature Clim Change. 2013;3:717–721. doi: 10.1038/nclimate1902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin S, Luo M, Walker RJ, et al. Extreme high temperatures and hospital admissions for respiratory and cardiovascular diseases. Epidemiology. 2009;20:738–746. doi: 10.1097/EDE.0b013e3181ad5522. [DOI] [PubMed] [Google Scholar]
- Lin S, Hsu WH, Zutphen ARV, et al. Excessive Heat and Respiratory Hospitalizations in New York State: Estimating Current and Future Public Health Burden Related to Climate Change. Environmental Health Perspectives. 2012;120:1571–1577. doi: 10.1289/ehp.1104728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madrigano J. personal communication. 2014.
- Marmor M. Heat wave mortality in New York City, 1949 to 1970. Arch Environ Health. 1975;30:130–136. doi: 10.1080/00039896.1975.10666661. [DOI] [PubMed] [Google Scholar]
- McGregor GR. Human biometeorology. Prog Phys Geography. 2012;36:93–109. [Google Scholar]
- Medina-Ramón M, Schwartz J. Temperature, temperature extremes, and mortality: a study of acclimatisation and effect modification in 50 US cities. Occup Environ Med. 2007;64:827–833. doi: 10.1136/oem.2007.033175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medina-Ramón M, Zanobetti M, Cavanagh DP, Schwartz J. Extreme temperatures and mortality: assessing effect modification by personal characteristics and specific cause of death in a multi-city case-only analysis. Environ Health Perspect. 2006:1331–1336. doi: 10.1289/ehp.9074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metzger KB, Ito K, Matte TD. Summer heat and mortality in New York City: how hot is too hot? Environ Health Perspect. 2010:80–86. doi: 10.1289/ehp.0900906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mudarri D, Fisk WJ. Public health and economic impact of dampness and mold. Indoor Air. 2007;17:226–235. doi: 10.1111/j.1600-0668.2007.00474.x. [DOI] [PubMed] [Google Scholar]
- National Oceanic and Atmospheric Administration (NOAA) US weather related fatalities. 2014 Available online at http://www.nws.noaa.gov/om/hazstats/resources/weather_fatalities.pdf.
- National Weather Service (NWS) US Natural Hazard Statistics. 2013 Available online at http://www.nws.noaa.gov/om/hazstats.shtml.
- New York City Department of Health and Mental Hygiene (NYC DOHMH), cited 2014: NYC Vital Signs Investigation Report. Available online at http://www.nyc.gov/html/doh/downloads/pdf/survey/survey-2006heatdeaths.pdf.
- New York City Department of Health and Mental Hygiene (NYC DOHMH) Epiquery: NYC Interactive Health Data System—Community Health Survey 2007. 2007 Available online at htttp://www.nyc.gov/epiquery.
- New York City Department of Health and Mental Hygiene (NYC DOHMH) NYC Vital Signs Investigation Report. 2014 Available online at http://www.nyc.gov/html/doh/downloads/pdf/survey/survey-2006heatdeaths.pdf.
- NPCC. Building the Knowledge Base for Climate Resiliency: New York City Panel on Climate Change 2015 Report. Rosenzweig C, Solecki W, editors. Ann NY Acad Sci. 2015;1336:1–149. doi: 10.1111/nyas.12653. [DOI] [PubMed] [Google Scholar]
- NYC Environmental Justice Alliance. personal communication. 2014.
- Nixdorf-Miller A, Hunsaker DM, Hunsaker JC., III Hypothermia and hyperthermia medicolegal investigation of morbidity and mortality from exposure to environmental temperature extremes. Arch Pathol Lab Med. 2006;130:1297–1304. doi: 10.5858/2006-130-1297-HAHMIO. [DOI] [PubMed] [Google Scholar]
- Ogden NH, Lindsay RL, Morshed M, et al. The emergence of Lyme disease in Canada. CMAJ. 2009;180:1221–1224. doi: 10.1503/cmaj.080148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden NH, et al. Active and passive surveillance and phylogenetic analysis of Borrelia burgdorferi elucidate the process of Lyme disease risk emergence in Canada. Environ Health Perspect. 2010;118:909–914. doi: 10.1289/ehp.0901766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Neill MS, Zanobetti A, Schwartz J. Disparities by race in heat-related mortality in four US cities: the role of air conditioning prevalence. J Urban Health. 2005;82:191–197. doi: 10.1093/jurban/jti043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parris A. How Hurricane Sandy tamed the bureaucracy. Issues Sci Technol. 2014;30 [Google Scholar]
- Patz JA, Vavrus SJ, Uejio CK, McLellan SL. Climate change and waterborne disease risk in the Great Lakes region of the U.S. Am J Prev Med. 2008;35:451–458. doi: 10.1016/j.amepre.2008.08.026. [DOI] [PubMed] [Google Scholar]
- Petkova EP, Gasparrini A, Kinney PL. Heat and mortality in New York City since the beginning of the 20th century. Epidemiology. 2014;25:554–560. doi: 10.1097/EDE.0000000000000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrzak RH, et al. Resilience in the face of disaster: prevalence and longitudinal course of mental disorders following Hurricane Ike. PLoS ONE. 2012;7:e38964. doi: 10.1371/journal.pone.0038964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polvani LM, Waugh DW, Correa GJP, Son SW. Stratospheric ozone depletion: the main driver of twentieth-century atmospheric circulation changes in the southern hemisphere. J Climate. 2011;24:795–812. [Google Scholar]
- Porsbjerg C, Linstow ML, Nepper-Christensen SC, et al. Allergen sensitization and allergen exposure in Greenlander Inuit residing in Denmark and Greenland. Respir Med. 2002;96:736–744. doi: 10.1053/rmed.2002.1341. [DOI] [PubMed] [Google Scholar]
- Reiss NM, Kostic SR. Pollen season severity and meteorologic parameters in central New Jersey. J Allergy Clin Immunol. 1976;57:609–614. doi: 10.1016/0091-6749(76)90013-0. [DOI] [PubMed] [Google Scholar]
- Rose JB, Epstein PR, Lipp EK, et al. Climate variability and change in the United States: potential impacts on water- and foodborne diseases caused by microbiologic agents. Environ Health Perspect. 2001;109(Suppl 2):211–221. doi: 10.1289/ehp.01109s2211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenzweig C, Solecki CW, DeGaetano A, et al., editors. Responding to climate change in New York State: The ClimAID integrated assessment for effective climate change adaptation in New York State. Ann NY Acad Sci. 2011;1244:1–460. doi: 10.1111/j.1749-6632.2011.06331.x. [DOI] [PubMed] [Google Scholar]
- Rosenzweig C, et al. Mitigating New York City’s heat island: integrating stakeholder perspectives and scientific evaluation. Bull Am Meteorol Soc. 2009;90:1297–1312. [Google Scholar]
- Rotkin-Ellman M, Solomon G, Gonzales CR, et al. Arsenic contamination in New Orleans soil: temporal changes associated with flooding. Environ Res. 2010;110:19–25. doi: 10.1016/j.envres.2009.09.004. [DOI] [PubMed] [Google Scholar]
- Ruckart PZ, Orr MF, Lanier K, Koehler A. Hazardous substances releases associated with Hurricanes Katrina and Rita in industrial settings, Louisiana and Texas. J Hazard Mater. 2008;159:53–57. doi: 10.1016/j.jhazmat.2007.07.124. [DOI] [PubMed] [Google Scholar]
- Semenza JC, Suk JE, Estevez V, et al. Mapping climate change vulnerabilities to infectious diseases in Europe. Environ Health Perspect. 2012;120:385–392. doi: 10.1289/ehp.1103805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semenza JC, Rubin CH, Falter KH, et al. Heat-related deaths during the July 1995 heat wave in Chicago. N Engl J Med. 1996;335:84–90. doi: 10.1056/NEJM199607113350203. [DOI] [PubMed] [Google Scholar]
- Sheffield PE, Knowlton K, Carr JL, Kinney PL. Modeling of regional climate change effects on ground-level ozone and childhood asthma. Am J Prev Med. 2011a;41:251–257. doi: 10.1016/j.amepre.2011.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheffield PE, Weinberger KR, Ito K, et al. The association of tree pollen concentration peaks and allergy medication sales in New York City: 2003–2008. ISRN Allergy. 2011b;2011:7. doi: 10.5402/2011/537194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheffield PE, Weinberger KR, Kinney PL. Climate change, aeroallergens, and pediatric allergic disease. Mt Sinai J Med. 2011c;78:78–84. doi: 10.1002/msj.20232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer BD, Ziska LH, Frenz DA, et al. Increasing Amb a 1 content in common ragweed (Ambrosia artemisiifolia) pollen as a function of rising atmospheric CO2 concentration. Functional Plant Biol. 2005;32:667–670. doi: 10.1071/FP05039. [DOI] [PubMed] [Google Scholar]
- Smith KR, et al. Public health benefits of strategies to reduce greenhouse-gas emissions: health implications of short-lived greenhouse pollutants. Lancet. 2009;374:2091–2103. doi: 10.1016/S0140-6736(09)61716-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spengler JD. Climate change, indoor environments, and health. Indoor Air. 2012;22:89–95. doi: 10.1111/j.1600-0668.2012.00768.x. [DOI] [PubMed] [Google Scholar]
- Tsai DH, Wang JL, Wang CH, Chan CC. A study of ground-level ozone pollution, ozone precursors and subtropical meteorological conditions in central Taiwan. J Environ Monit. 2008;10:109–118. doi: 10.1039/b714479b. [DOI] [PubMed] [Google Scholar]
- U.S. EPA. Final report. Washington, DC: EPA; 2008. A review of the impact of climate variability and change on aeroallergens and their associated effects. [Google Scholar]
- Vandentorren S, et al. August 2003 heat wave in France: risk factors for death of elderly people living at home. Eur J Public Health. 2006;16:583–591. doi: 10.1093/eurpub/ckl063. [DOI] [PubMed] [Google Scholar]
- Villeneuve PJ, Doiron MS, Stieb D, et al. Is outdoor air pollution associated with physician visits for allergic rhinitis among the elderly in Toronto, Canada? Allergy. 2006;61:750–758. doi: 10.1111/j.1398-9995.2006.01070.x. [DOI] [PubMed] [Google Scholar]
- Walsh J, Wuebbles D, Hayhoe K, et al. Our changing climate. In: Melillo JM, Richmond TTC, Yohe GW, editors. Climate Change Impacts in the United States: The Third National Climate Assessment. U.S. Global Change Research Program; 2014. pp. 19–67. [Google Scholar]
- Whitman S, Good G, Donoghue ER, et al. Mortality in Chicago attributed to the July 1995 heat wave. Am J Public Health. 1997;87:1515–1518. doi: 10.2105/ajph.87.9.1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson K. Climate change and the spread of infectious ideas. Ecology. 2009;90:901–902. doi: 10.1890/08-2027.1. [DOI] [PubMed] [Google Scholar]
- Wolf J, O’Neill NR, Rogers CA, et al. Elevated atmospheric carbon dioxide concentrations amplify Alternaria alternata sporulation and total antigen production. Environ Health Perspect. 2010;118:1223–1228. doi: 10.1289/ehp.0901867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziska LH, Caulfield FA. Rising CO2 and pollen production of common ragweed (Ambrosia artemisiifolia L.), a known allergy-inducing species: implications for public health. Aust J Plant Physiol. 2000;27:893–898. [Google Scholar]
- Ziska LH, Gebhard DE, Frenz DA, et al. Cities as harbingers of climate change: common ragweed, urbanization, and public health. J Allergy Clin Immunol. 2003;111:290–295. doi: 10.1067/mai.2003.53. [DOI] [PubMed] [Google Scholar]
- Ziska L, et al. Recent warming by latitude associated with increased length of ragweed pollen season in central North America. Proc Natl Acad Sci USA. 2011;108:4248–4251. doi: 10.1073/pnas.1014107108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoraster RM. Vulnerable populations: Hurricane Katrina as a case study. Prehosp Disaster Med. 2010;25:74–78. doi: 10.1017/s1049023x00007718. [DOI] [PubMed] [Google Scholar]