Abstract
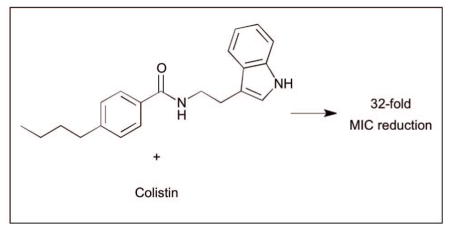
A screen of 20 compounds identified small molecule adjuvants capable of potentiating anitbiotic activty against Francisella philomiragia. Analogue synthesis of an initial hit compound led to the discovery of a potentially new class of small molecule adjuvants containg an indole core. The lead compound was able to lower the MIC of colistin by 32-fold against intrinsically resistant F. philomiragia.
Graphical abstract
Introduction
Francisella are small, facultative Gram-negative bacteria that are responsible for zoonotic disease in which humans are infected, usually from bites or contact with infected blood.1 The most common vectors of disease are ticks and wild rabbits.2 Francisella can also be a highly infectious aerosol and has the potential to be weaponized.3 Encompassed under the Francisella genus are two species of consequence: Francisella philomiragia and Francisella tularensis. Very resilient, the bacteria are capable of surviving multiple weeks in the environment and have been found in water sources around the world.4 Although, not as virulent and somewhat rare in humans,5 F. philomiragia is a potential model organism to study Francisella. Human cases of F. philomiragia are often associated with individuals with weakened immune systems or who have suffered from a near drowning experience.6 F. philomiragia is also the causative agent of the disease francisellosis, most common among various species of fish.7 Francisellosis outbreaks have been responsible for mortality rates of up to 95% within farmed fish.8
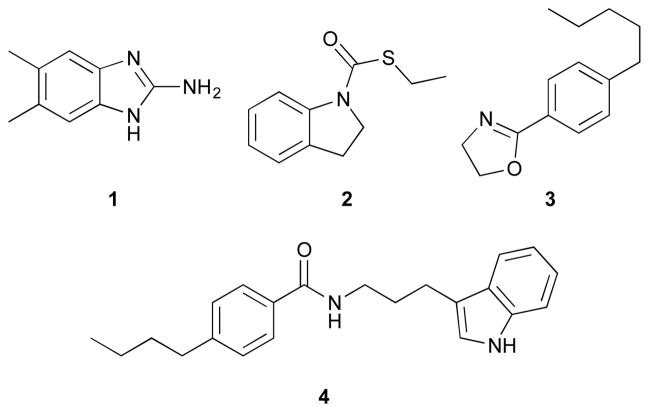
Our laboratory is interested in using small molecule adjuvants to potentiate antibiotic activity. We have shown that 2-aminoimidazoles (2-AIs) are capable of potentiating antibiotic activity against a wide variety of bacteria.9–13 We completed a screen of randomly chosen molecules from our in house library and identified four compounds, all of which, did not contain a 2-AI or 2-ABI core, but another nitrogen containing heterocycle (indole, indoline, or oxazoline) (Fig. 1) that were capable of potentiating antibiotic response in F. philomiragia. A structure activity relationship (SAR) study of compound 4 was carried out to discover potentially more potent leads and to better understand the structural requirements for activity. Herein, we report the discovery of the first example of a potentially new class of lead compounds containing an indole core capable of breaking F. philomiragia resistance to the antibiotic colistin.
Fig. 1.
Lead structures identified from initial screening.
Results and discussion
Adjuvant screen for MIC suppression of antibiotics against F. philomiragia
An initial pilot screen of 20 compounds from our in-house small molecule library14–18 was conducted by first determining the intrinsic antibiotic activity of each molecule by establishing its minimum inhibitory concentration (MIC) against F. philomiragia (Figure 1, Supplementary Information). Following our lab’s previously reported screening protocol,9 the MIC of candidate conventional antibiotics were then determined in the absence or presence of each compound at 25% of the compound’s MIC. Previous studies from our group has established that molecules from our internal library had little (if any) effect on bacterial growth at 25% MIC, allowing us to study non-microbicidal repotentiation of the conventional antibiotics under study. Streptomycin, an aminoglycoside, was chosen as the initial antibiotic to screen for potential adjuvants as it is considered to be the drug of choice for tularemia treatment.19 Initial testing with streptomycin revealed of the 20 compounds screened only compound 1 showed activity, a reduction in MIC of four-fold to 1 μg/mL (Table 1). Gentamicin, another aminoglycoside, has also been shown to be an effective treatment option for patients suffering from tularemia.20 Screening the same library for gentamicin repotentiation gave the same results for streptomycin, with compound 1 lowering the MIC four-fold from 1 μg/mL to 0.125 μg/mL.
Table 1.
MIC data for the initial lead compounds against F. philomiragia. ND = not determined.
| Compound | MIC (μM) | Concentration tested (μM) | Streptomycin (μg/mL) | Gentamicin (μg/mL) | Azithromycin (μg/mL) | FR900098 (μg/mL) | Colistin (μg/mL) |
|---|---|---|---|---|---|---|---|
| - | - | - | 4 | 0.5 | 4 | 1,024 | 256 |
| 1 | >200 | 50 | 1 | 0.125 | 4 | 1,024 | 32 |
| 2 | >200 | 50 | 4 | 0.5 | 0.5 | 1,024 | 256 |
| 3 | 200 | 50 | 8 | 1 | 2 | 64 | 512 |
| 4 | >200 | 50 | 4 | 0.25 | 2 | ND | 64 |
| 5 | >200 | 50 | 4 | 0.25 | 0.5 | 1,024 | 8 |
Another class of antibiotics tested were macrolides, specifically azithromycin. Azithromycin is an attractive option for treatment because of its ability to concentrate within macrophages, where Francisella replicates at intracellular levels that are even greater than serum levels.21 Upon screening our library, compound 1 exerted no change in azithromycin activity. Another compound (2) displayed an eight-fold reduction in MIC, from 4 μg/mL to 0.5 μg/mL). Compound 2 is of interest because unlike previously reported small molecule adjuvants from our lab it is neither a 2-AI nor 2-ABI, but rather contains an indoline core.
Our screen was further expanded to include a phosphonic acid antibiotic, FR900098. FR900098 has been shown to be effective at inhibiting Francisella sub-species.22 Compound 3 displayed a significant decrease in MIC of 16-fold from 1024 μg/mL to 64 μg/mL.
Finally, we used colistin, a polymyxin antibiotic that is known to be ineffective at treating Francisella infections due to intrinsic resistance.23 The MIC of colistin alone was 256 μg/mL. Library screening revealed an indole containing compound (4) that was also absent of a 2-AI or 2-ABI motif. The indole 4 exhibited a four-fold MIC reduction for colistin to 64 μg/mL.
Library synthesis for structure activity relationship (SAR) study
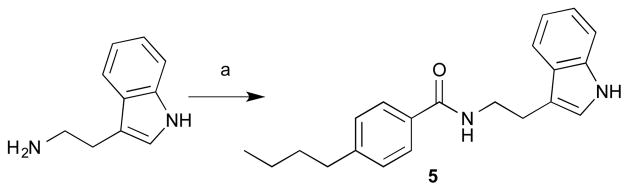
Based on the results of our screen, availability of starting materials and cost of antibiotics, we opted to perform analogue synthesis of the indole 4. We were able to rapidly assemble an 11-membered analogue library of 4 (SI Table 1). The core is structurally similar to tryptamine with the only difference being a shorter 2-carbon linker. Direct reaction of tryptamine and derivatives with a variety of acylating agents in the presence of TEA gave a library of various structural motifs. Testing revealed that shortening the three-carbon linker to two carbons (5) drastically increased potency (Scheme 1.), lowering the MIC of colistin 32-fold to 8 μg/mL. The amide appears to be necessary as any change in functionality: amine, ester, or sulfonamide, results in complete loss in activity (SI Table 1). Alkylation or acylation of the indole nitrogen-1 position, also caused complete loss in MIC suppression. Changes in the alkyl tail length from butyl also gave disappointing results, as methyl, ethyl, and propyl derivatives had no impact on the antibiotic MIC.
Scheme 1.
Synthesis of the most active compound (5). Reagents and conditions: (a) 4-butylbenzoyl chloride, TEA and DCM.
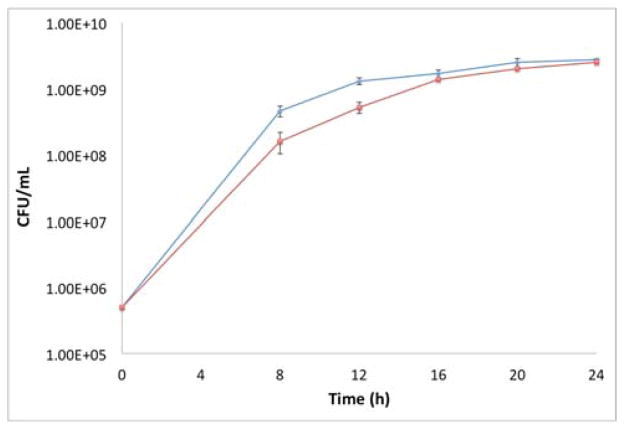
Time kill curve of compound 5
In order to determine whether compound 5 was acting through a toxic or non-toxic mechanism, bacterial growth was measured as a function of time. F. philomiragia was grown with/without compound (50 μM) being present. Bacterial growth was checked at 8, 12, 16, 20, and 24 hr time points (Figure 2). Based on the analysis of the time kill curve, we observe minor growth delay at earlier time points; however growth is identical by 16 hours.
Fig. 2.
Time kill curve of compound 5. Blue diamonds represent bacterial control. Red squares represent bacteria and compound 5 (50 μM).
MIC determination in Francisella novicida
With lead compounds in hand, we then wanted to determine whether compounds retained activity against F. novicida, a subspecies of F. tularensis. As before, the MIC of the active compounds (1, 2, and 5) were determined and then antibiotic MICs were established in the absence or presence of each compound at 25% MIC. Compound 1 showed no change in MIC for any of the antibiotics tested (Table 2). The indole compound 5 displayed a two-fold reduction in MIC for colistin from 1024 μg/mL to 512 μg/mL. The concentration of 5 was increased by 10 μM increments from 50 μM to 100 μM; however the increased concentration of 5 was unable to potentiate colistin in F. novicida further. Compound 2 was the only adjuvant tested to show any significant activity, reducing the MIC of azithromycin 16-fold fro 2 μg/mL to 0.125 μg/mL.
Table 2.
MIC data for active compounds against F. novicida.
| Compound | MIC (μM) | Concentration tested (μM) | Gentamicin (μg/mL) | Azithromycin (μg/mL) | Colistin (μg/mL) |
|---|---|---|---|---|---|
| - | - | - | 1 | 2 | 1,024 |
| 1 | >200 | 50 | 1 | 2 | 1,024 |
| 2 | >200 | 50 | 4 | 0.125 | 1,024 |
| 5 | >200 | 50 | 4 | 1 | 512 |
Experimental section
Materials and methods
All reagents and solvents for synthesis were obtained from Sigma- Aldrich, St. Louis, MO, USA. Triethylamine was dried by refluxing CaH2, followed by distillation and storage over 4Å molecular sieves. Deuterated solvents were acquired from Cambridge Isotope Laboratories (CIL). Purification was performed using 60 mesh standard silica from Sorbtech. 1H NMR (300 MHz) and 13C NMR (100 MHz) spectra were recorded at 25°C on Varian Mercury spectrometers. Chemical shifts (δ) are given in ppm relative to TMS as an internal standard or the respective NMR solvent. Mass spectra were recorded on Thermo Fisher Scientific Exactive Plus MS (ESI).
Synthesis
General procedure for amide, ester, and sulfonamide coupling
In a flame dried round bottom under N2 atmosphere was added tryptamine (300 mg, 1.87 mmol), TEA (777 μL, 5.61 mmol), and anhydrous DCM (10 mL). The reaction mixture was cooled to 0°C and 4-butylbenzoyl chloride (314 μL, 1.68 mmol) was added dropwise. The reaction mixture was stirred until completion as determined by TLC. The reaction mixture was then washed with 1N HCl (1 × 5 mL), brine (1 × 5 mL) and the organic layer was dried over Na2SO4, then filtered. The solvent was removed in-vacuo and the residue was purified by flash chromatography using 4:1 Hex/EtOAc to 2:1 Hex/EtOAc to give a white solid (538mg, 93% yield).
Biological
Bacteria, media, and antibiotics
Francisella philomiragia was obtained from the American Type Culture Collection (ATCC), Manassas, VA, as ATCC # (25015) and Francisella novicida was obtained from BEI Resources as BEI # (U112). F. philomiragia and F. novicida were grown in cation adjusted Mueller Hinton broth (CAMHB) supplemented with 2% IsoVitaleX (BD #211876) enrichment or tryptic soy broth supplemented with 0.1% cysteine (TSB-C) at 37°C with shaking, or on cysteine heart agar supplemented with 5% rabbits blood (Hemostat; DRB050) at 37°C. The bacteria were incubated at 37°C for 24 hr. Antibiotics were purchased from Sigma-Aldrich, St. Louis, MO, USA.
Minimum inhibitory concentration (MIC) assay
One day cultures (24 hr) were subcultured to 5 × 105 CFU/mL in CAMHB supplemented with 2% IsoVitaleX (F. philomiragia) or TSB-C (F. novicida). Aliquots (1 mL) of the subcultured media were added to small culture tubes. Compound from a 100 mM stock solution in DMSO was added to the small culture tube to give the desired starting concentration (200 μM or 2–2,048 μg/mL). Rows 2–12 of a 96-well microtiter plate were filled with 100 μL/well of the bacterial subculture. The wells of the first row were filled with 200 μL each of the compound-containing sample. Row 1 wells were mixed a minimum of five times, followed by a 100 μL aliquot to row 2. The process was repeated until the final row, in which the last 100 μL aliquot was discarded. The 96-well plate was then sealed with a plastic lid and incubated under stationary conditions at 37°C for 48hr. The compound MIC was recorded as the lowest concentration at which no bacterial growth was observed.
Antibiotic resensitization assay
One day cultures (24 hr) were subcultured to 5 × 105 CFU/mL in CAMHB supplemented with 2% IsoVitaleX (F. philomiragia) or TSB-C (F. novicida). Aliquots (5 mL) of subcultured media were added to large culture tubes. Compound from a 100 mM stock solution in DMSO was added to the large culture tubes to give the concentration to be tested (25% of the MIC value). One culture tube had nothing added and served as the control. Aliquots (1 mL) were taken from the large culture tubes and added to small culture tubes. Antibiotic was added to the small culture tubes, including the control, to give the desired starting concentration (2–2,048 μg/mL). Rows 2–12 of a 96-well microtiter plate were filled with 100 μL/well of the bacterial subculture with or without compound. The wells of the first row were filled with 200 μL each of the antibiotic dosed samples. Row 1 wells were mixed a minimum of five times, followed by a 100 μL aliquot to the subsequent row. The process was repeated until the final row, in which the last 100 μL aliquot was discarded. The 96-well plate was then sealed with a plastic lid and incubated under stationary conditions at 37°C for 48 hr. The compound MIC was recorded as the lowest concentration at which no bacterial growth was observed.
Time kill curve
F. philomiragia was cultured for 24 hr in CAMHB supplemented with 2% IsoVitaleX. Fresh media was then inoculated with the bacteria to 5 × 105 CFU/mL and aliquots (3 mL) were added to large culture tubes. Compound (25% of the MIC) was added to one set of culture tubes, while the control was bacteria alone. The tubes were incubated at 37°C with shaking. Aliquots (100 μL) were taken at 8, 12, 16, 20, and 24 hr time points. The aliquots were serially diluted and plated on cysteine heart agar supplemented with 5% rabbit’s blood and spread with sterile glass beads. Plates were incubated at 37°C under stationary conditions for 24–36 hr. The number of colonies formed were enumerated.
Conclusions
In summary, a pilot library screen resulted in the identification of several unique small molecule adjuvants, capable of potentiating various classes of antibiotics against F. philomiragia. Analogue synthesis of one lead (4) gave rise to compound 5, which displayed enhanced activity, culminating in a 32-fold MIC reduction to 8 μg/mL for colistin. Bacterial growth over time was measured to elucidate whether compound 5 was bactericidal. The CFUs measured for compound containing samples, correlate strongly with the control providing evidence 5 is acting through a non-toxic mechanism. This is the first example of a small molecule adjuvant able to potentiate F. philomiragia resistance to colistin, and 5 may represent the basis of a new class of small molecule adjuvants. Further exploration of this unique class of compound is currently underway in attempts to break F. novicida resistance.
Supplementary Material
Acknowledgments
The authors would like to thank the National Institutes of Health (R01GM055769 to JC and CM) and DTRA (HDTRA1-11-1-0054 to MVH) for support.
Footnotes
Electronic Supplementary Information (ESI) available: [details of any supplementary information available should be included here]. See DOI: 10.1039/x0xx00000x
Notes and references
- 1.Petersen JM, Mead PS, Schriefer ME. Vet Res. 2009;40:7. doi: 10.1051/vetres:2008045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mani RJ, Metcalf JA, Clinkenbeard KD. PLoS One. 2015;10:e0130513. doi: 10.1371/journal.pone.0130513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fritz DL, England MJ, Miller L, Waag DM. Comp Med. 2014;64:341–350. [PMC free article] [PubMed] [Google Scholar]
- 4.Parker RR, Steinhaus EA, Kohls GM, Jellison WL. Bull Natl Inst Health. 1951;193:1–161. [PubMed] [Google Scholar]
- 5.Mailman TL, Schmidt MH. Can J Infect Dis Med Microbiol. 2005;16:245–248. doi: 10.1155/2005/486417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wenger JD, Hollis DG, Weaver RE, Baker CN, Brown GR, Brenner DJ, Broome CV. Ann Intern Med. 1989;110:888–892. doi: 10.7326/0003-4819-110-11-888. [DOI] [PubMed] [Google Scholar]
- 7.Verhoeven AB, Durham-Colleran MW, Pierson T, Boswell WT, Van Hoek ML. Biol Bull. 2010;219:178–188. doi: 10.1086/BBLv219n2p178. [DOI] [PubMed] [Google Scholar]
- 8.Chern RS, Chao CB. Fish Pathol. 1994;29:61–71. [Google Scholar]
- 9.Rogers SA, Huigens RW, 3rd, Cavanagh J, Melander C. Antimicrob Agents Chemother. 2010;54:2112–2118. doi: 10.1128/AAC.01418-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harris TL, Worthington RJ, Melander C. Angew Chem Int Ed Engl. 2012;51:11254–11257. doi: 10.1002/anie.201206911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harris TL, Worthington RJ, Hittle LE, Zurawski DV, Ernst RK, Melander C. ACS Chem Biol. 2014;9:122–127. doi: 10.1021/cb400490k. [DOI] [PubMed] [Google Scholar]
- 12.Worthington RJ, Bunders CA, Reed CS, Melander C. ACS Med Chem Lett. 2012;3:357–361. doi: 10.1021/ml200290p. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brackett CM, Melander RJ, An IH, Krishnamurthy A, Thompson RJ, Cavanagh J, Melander C. J Med Chem. 2014;57:7450–7458. doi: 10.1021/jm501050e. [DOI] [PubMed] [Google Scholar]
- 14.Rogers SA, Whitehead DC, Mullikin T, Melander C. Org Biomol Chem. 2010;8:3857–3859. doi: 10.1039/c0ob00063a. [DOI] [PubMed] [Google Scholar]
- 15.Huigens RW, Reyes S, Reed CS, Bunders C, Rogers SA, Steinhauer AT, Melander C. Bioorganic & Medicinal Chemistry. 2010;18:663–674. doi: 10.1016/j.bmc.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 16.Su Z, Rogers SA, McCall WS, Smith AC, Ravishankar S, Mullikin T, Melander C. Organic & Biomolecular Chemistry. 2010;8:2814–2822. doi: 10.1039/c001479f. [DOI] [PubMed] [Google Scholar]
- 17.Reed CS, Huigens RW, 3rd, Rogers SA, Melander C. Bioorg Med Chem Lett. 2010;20:6310–6312. doi: 10.1016/j.bmcl.2010.08.075. [DOI] [PubMed] [Google Scholar]
- 18.Rogers SA, Melander C. Angewandte Chemie International Edition. 2008;47:5229–5231. doi: 10.1002/anie.200800862. [DOI] [PubMed] [Google Scholar]
- 19.Enderlin G, Morales L, Jacobs RF, Cross JT. Clin Infect Dis. 1994;19:42–47. doi: 10.1093/clinids/19.1.42. [DOI] [PubMed] [Google Scholar]
- 20.Hassoun A, Spera R, Dunkel J. Antimicrob Agents Chemother. 2006;50:824. doi: 10.1128/AAC.50.2.824.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ahmad S, Hunter L, Qin A, Mann BJ, van Hoek ML. BMC Microbiol. 2010;10:123. doi: 10.1186/1471-2180-10-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McKenney ES, Sargent M, Khan H, Uh E, Jackson ER, San Jose G, Couch RD, Dowd CS, van Hoek ML. PLoS One. 2012;7:e38167. doi: 10.1371/journal.pone.0038167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Llewellyn AC, Zhao J, Song F, Parvathareddy J, Xu Q, Napier BA, Laroui H, Merlin D, Bina JE, Cotter PA, Miller MA, Raetz CR, Weiss DS. Mol Microbiol. 2012;86:611–627. doi: 10.1111/mmi.12004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.