Abstract
While the number of reported tuberculosis (TB) cases in the United States has declined over the past two decades, TB morbidity among foreign-born persons has remained persistently elevated. A recent unexpected decline in reported TB cases among foreign-born persons beginning in 2007 provided an opportunity to examine contributing factors and inform future TB control strategies. We investigated the relative influence of three factors on the decline: 1) changes in the size of the foreign-born population through immigration and emigration, 2) changes in distribution of country of origin among foreign-born persons, and 3) changes in the TB case rates among foreign-born subpopulations. Using data from the U.S. National Tuberculosis Surveillance System and the American Community Survey, we examined TB case counts, TB case rates, and population estimates, stratified by years since U.S. entry and country of origin. Regression modeling was used to assess statistically significant changes in trend. Among foreign-born recent entrants (<3 years since U.S. entry), we found a 39.5% decline (-1,013 cases) beginning in 2007 (P<0.05 compared to 2000–2007) and ending in 2011 (P<0.05 compared to 2011–2014). Among recent entrants from Mexico, 80.7% of the decline was attributable to a decrease in population, while the declines among recent entrants from the Philippines, India, Vietnam, and China were almost exclusively (95.5%–100%) the result of decreases in TB case rates. Among foreign-born non-recent entrants (≥3 years since U.S. entry), we found an 8.9% decline (-443 cases) that resulted entirely (100%) from a decrease in the TB case rate. Both recent and non-recent entrants contributed to the decline in TB cases; factors contributing to the decline among recent entrants varied by country of origin. Strategies that impact both recent and non-recent entrants (e.g., investment in overseas TB control) as well as those that focus on non-recent entrants (e.g., expanded targeted testing of high-risk subgroups among non-recent entrants) will be necessary to achieve further declines in TB morbidity among foreign-born persons.
Introduction
Tuberculosis (TB) remains an enormous public health challenge globally, with 9.6 million new cases and 1.5 million deaths each year [1]. Meanwhile, the United States has experienced a steady decline in TB cases over the past 2 decades, with a record low number of TB cases in 2014 [2]. This decline has predominately been among U.S.-born persons; the number of cases among foreign-born persons has remained relatively constant, and the TB case rate among the foreign-born population was 13.4 times greater than that of the U.S.-born population in 2014 [2]. A recent model estimated that TB elimination in the United States will not be achieved within the 21st century, partly because of a persistently elevated rate of TB among foreign-born persons [3].
Recent analyses revealed an unexpected decline in cases among foreign-born persons in the United States that began in 2007 [4, 5]. We investigated the relative influence of three factors on this decline: changes in the size of the foreign-born population through immigration and emigration, changes in the distribution of country of origin among foreign-born persons, and changes in the TB case rates among specific foreign-born subpopulations. We hypothesized that the decline among foreign-born persons was primarily because of a decreased rate of TB among recent entrants into the United States, a decreased number of foreign-born persons living in the United States (particularly recent entrants), and to a lesser extent, a decrease in transmission among foreign-born persons in the United States secondary to the lower number of cases due to the former two reasons.
Methods
Study Population
The study population included all foreign-born persons in the United States during 2000–2014. On the basis of preliminary findings, analyses of the decline focused on the period 2007–2011. Verified cases of reported TB were from the U.S. National Tuberculosis Surveillance System, which includes both laboratory-confirmed cases and clinical cases meeting pre-specified criteria [6]. Cases were classified by the patient’s country of origin and years since U.S. entry. Cases with unknown data regarding the patient’s country of origin or years since U.S. entry were excluded from the analysis. Genotyping data were from the U.S. National Genotyping Service [7]. Population estimates were derived from the American Community Survey 1-year estimates, an ongoing statistical survey that samples approximately 1.9 million households annually [8], and has been utilized for previous studies of TB case rates among foreign-born persons in the United States [9–11]. Individuals are included in the American Community Survey regardless of immigration status [8]. Data from the U.S. Department of Homeland Security [12] and CDC’s Electronic Disease Notification system [13] were used to estimate the number persons who entered into the United States in a given year, stratified by visa type and country of origin.
Data Analysis
Joinpoint regression software, version 4.2.0.2 (National Cancer Institute, Bethesda, Maryland) was used to identify statistically significant changes in trend among TB case counts [14, 15]. Annual TB case rates were calculated by using case counts and population estimates for each year and were expressed as the number of cases per 100,000 persons. Detailed methods used to calculate rates stratified by years since U.S. entry have been described elsewhere [9–11].
Previous studies have established the high morbidity and elevated TB case rates among foreign-born persons during the first few years after entry into the United States [9–11, 16, 17].
To provide greater detail on these first few years, we divided foreign-born persons into the following groups based upon time since U.S. entry: <1 year, ≥1 to <2 years, ≥2 to <3 years, ≥3 to <6 years, and ≥6 years. We then concentrated further subpopulation analyses on recent entrants, defined as foreign-born persons <3 years since U.S. entry, as this represents the population most affected by changes in immigration and emigration [8, 18, 19]. We examined TB cases among recent entrants from the top five countries accounting for the largest number of cases diagnosed in the United States (i.e., Mexico, Philippines, India, Vietnam, and China) [2]. After excluding cases from the top five countries of origin, we categorized the remaining cases of TB among recent entrants according to the TB incidence in the country of origin as follows: low, <15 cases/100,000 persons; medium, 15–99 cases/100,000 persons; or high incidence, ≥100/100,000 persons [1].
To evaluate potential causes of the decline among each foreign-born subpopulation, we estimated the proportion of the case count decrease resulting from changes in the TB case rate versus population shifts using Formula 1 and Formula 2 below. If there was an increase in population from 2007 to 2011, then 100% of the case count decline was assumed to be the result of changes in TB case rate.
Formula 1. Percent of case count decline resulting from TB case rate change =
R2007 = TB case rate in 2007; R2011 = TB case rate in 2011; P2007 = Population in 2007; P2011 = Population in 2011
Formula 2. Percent of case count decline resulting from population change =
R2007 = TB case rate in 2007; R2011 = TB case rate in 2011; P2007 = Population in 2007; P2011 = Population in 2011
In 2007, CDC updated requirements for overseas TB screening of refugees and persons applying for permanent resident visas to the United States [20, 21]. Among the most important changes was the introduction of routine mycobacterial culture (in addition to the already required sputum-smear microscopy). Those applying for other visa types (e.g., students, exchange visitors, temporary workers, tourists, and business travelers) are not routinely required to undergo overseas TB screening, and those who enter the United States without a visa (e.g., undocumented persons) are not subject to overseas screening. We used data from the U.S. Department of Homeland Security and CDC’s Electronic Disease Notification system to assess the scope of overseas TB screening by estimating the number of persons each year who arrived as refugees or permanent resident applicants. We then used American Community Survey data to estimate the overall population of new entrants, defined as the population that entered the United States within the past year, regardless of visa type (including persons without a visa). For each country, we calculated the proportion of the new entrant population who passed through culture-based overseas TB screening during 2007–2011. For countries where culture-based overseas screening only occurred for part of a year [22], we assumed that the number of refugees and permanent resident applicants was evenly distributed by month and prorated the number screened accordingly.
Finally, focusing on cases among recent entrants (<3 years since U.S. entry), we estimated the number of cases associated with likely recent transmission in the United States. We used a methodology verified against a field-based standard [23], with two alterations. First, we included cases diagnosed <100 days after U.S. entry to avoid underestimating cases possibly due to local transmission shortly after arrival. Second, a case attributed to recent transmission must have had a U.S. entry date before the diagnosis date of the possible source case. The U.S. National Genotyping Service introduced universal 24-locus mycobacterial interspersed repetitive unit–variable number tandem repeat genotyping in 2009 [7]. To ensure a 2-year time interval for a potential source case to be identified, the transmission component of the analysis was limited to cases counted during January 1–September 30, 2011, in the U.S. National Tuberculosis Surveillance System. Cases diagnosed during October 1–December 31, 2011, were excluded to allow an additional 3-month period for belated identification of potential source cases. A given case was classified as due to recent transmission if at least one plausible source case was identified based upon clinical characteristics, genotyping data, and temporal and geographic proximity to the putative secondary case. In addition, we examined the reported origin (U.S.-born versus foreign-born) for each potential source case. Some secondary cases were found to have more than one potential source case; therefore, we generated low and high estimates of possible source cases by origin.
Aside from analyses of Joinpoint regression and changes in trend, all additional analyses were conducted using SAS, version 9.3 (SAS Institute, Inc., Cary, North Carolina). For all statistical tests, results were considered to be significant at P<0.05. CDC reviewed the proposed study and determined that approval by an institutional review board was not required because data were collected and analyzed for this project as part of routine TB surveillance; therefore, the project is not considered research involving human subjects.
Results
Trends in TB Case Counts, 2000–2014
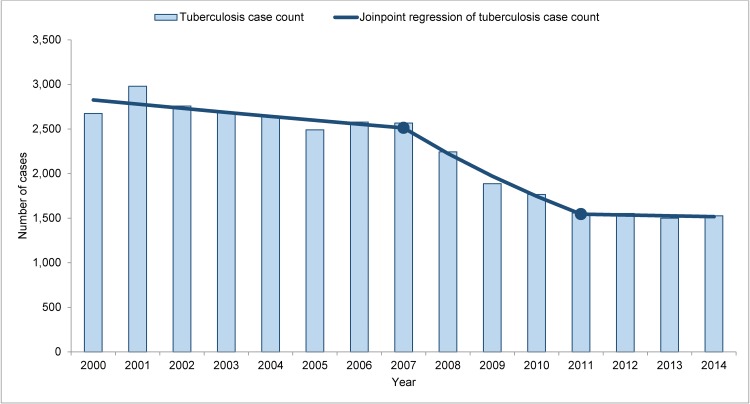
There were 108,944 cases of TB reported among foreign-born persons in the United States during 2000–2014. Data were missing for country of origin or time since U.S. entry for 4,913 persons (4.5%), leaving 104,031 cases for analysis. TB cases among recent entrants (<3 years since U.S. entry) declined by 42.9% (-1,148 cases) during 2000–2014, with statistically significant changes in trend in 2007 and 2011 (Fig 1). In 2014, recent entrants accounted for 26.2% of all cases among foreign-born persons, compared with 37.0% in 2000.
Fig 1. Tuberculosis case counts with Joinpoint regression among recent entrants, 2000–2014.
Shaded bars indicate tuberculosis case counts among recent entrants (foreign-born persons with <3 years since U.S. entry). The solid line represents a Joinpoint regression of tuberculosis case counts. Solid circles represent statistically significant changes in trend in 2007 and 2011 (2000–2007 annual percent change, -1.7% [95% confidence interval {CI}, -3.5%, +0.2%); 2007–2011 annual percent change, -11.4% (95% CI -17.4%, -5.1%)]; 2011–2014 annual percent change, -0.6% [95% CI, -7.3%, +6.5%]).
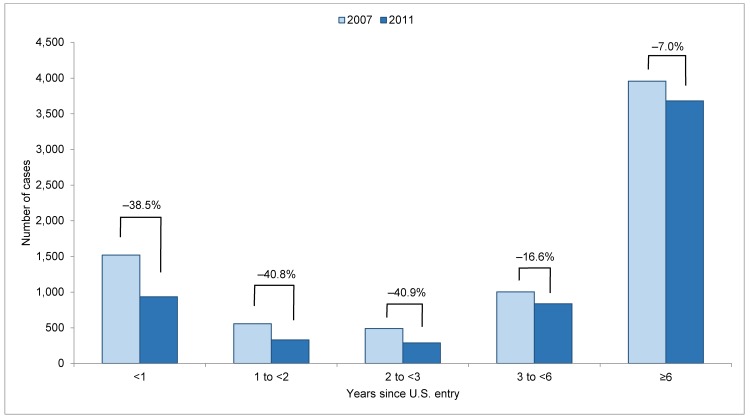
Time since U.S. Entry, 2007–2011
During 2007–2011, there was an overall decline of 1,456 cases (-19.3%) among all foreign-born persons (Table 1). Among recent entrants (<3 years since U.S. entry), there were decreases in case count (-39.5%, -1,013 cases), TB case rate (-30.8%), and population (-12.5%). Among non-recent entrants (≥3 years since U.S. entry), there was a decrease in case count (-8.9%, -443 cases) and TB case rate (-16.6%), but an increase in the non-recent entrant population (+9.1%).
Table 1. Changes in tuberculosis case counts, population estimates, and tuberculosis case rates among foreign-born persons in the United States, 2007 and 2011.
| Tuberculosis Case Count | Population Estimatea (Thousands) | Tuberculosis Case Rate (per 100,000 Persons) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2007 | 2011 | Relative Change (%) | 2007 | 2011 | Relative Change (%) | 2007 | 2011 | Relative Change (%) | ||
| Among all foreign born persons | ||||||||||
| 7,529 | 6,073 | -19.3 | 40,148 | 42,917 | +6.9 | 18.8 | 14.2 | -24.5 | ||
| Recent versus non-recent entrantsb | ||||||||||
| Recent | 2,567 | 1,554 | -39.5 | 4,152 | 3,632 | -12.5 | 61.8 | 42.8 | -30.8 | |
| Non-recent | 4,962 | 4,519 | -8.9 | 35,996 | 39,285 | +9.1 | 13.8 | 11.5 | -16.6 | |
| Years since U.S. entry | ||||||||||
| <1 | 1,521 | 935 | -38.5 | 1,449 | 1,318 | -9.1 | 104.9 | 71.0 | -32.4 | |
| 1 to <2 | 557 | 330 | -40.8 | 1,369 | 1,175 | -14.2 | 40.7 | 28.1 | -31.0 | |
| 2 to <3 | 489 | 289 | -40.9 | 1,334 | 1,140 | -14.6 | 36.7 | 25.4 | -30.8 | |
| 3 to <6 | 1,005 | 838 | -16.6 | 4,016 | 3,661 | -8.8 | 25.0 | 22.9 | -8.5 | |
| ≥6 | 3,957 | 3,681 | -7.0 | 31,979 | 35,624 | +11.4 | 12.4 | 10.3 | -16.5 | |
a Source: American Community Survey [8].
b Recent entrants are foreign-born persons with <3 years since U.S. entry; non-recent entrants are foreign-born persons with ≥3 years since U.S. entry.
When examining more discrete groups by years since U.S. entry (Fig 2), case counts declined among all groups, with the smallest relative case count decline among foreign-born persons in the United States ≥6 years (-7.0%, -276 cases). TB case rates also declined among all foreign-born groups, regardless of time since U.S. entry (Table 1). Although the population of foreign-born persons with ≥6 years since U.S. entry increased (+11.4%), decreases in population were seen among all other groups.
Fig 2. Tuberculosis case counts and percent decline among foreign-born persons by years since U.S. entry, 2007 and 2011.
Light shaded bars represent tuberculosis case counts in 2007, and dark shaded bars represent tuberculosis case counts in 2011. Percentages indicate the percent decline in case count for each group during 2007–2011.
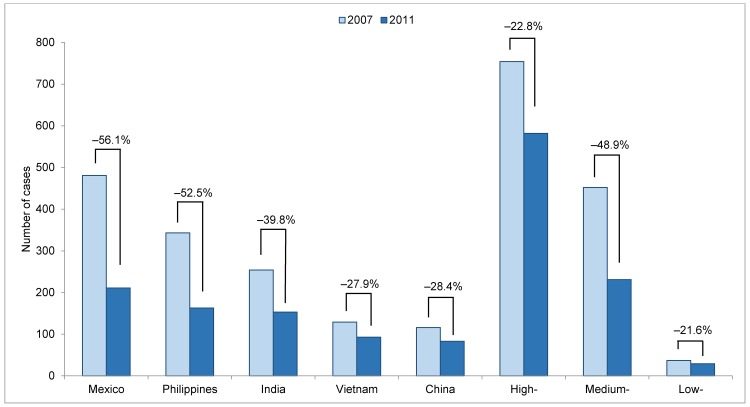
Recent Entrants: Top Five Countries of Origin, 2007–2011
TB case counts among recent entrants from all of the top five countries of origin declined during 2007–2011 (Fig 3). The largest relative declines in case counts were among recent entrants from Mexico (-56.1%, -270 cases), the Philippines (-52.5%, -180 cases), and India (-39.8%, -101 cases).
Fig 3. Tuberculosis case counts and percent decline among recent entrants, by country of origin or tuberculosis incidence in country of origin, 2007 and 2011.
Light shaded bars represent tuberculosis case counts in 2007, and dark shaded bars represent tuberculosis case counts in 2011. Percentages indicate the percent decline in case count for each group during 2007–2011. Recent entrants are foreign-born persons with <3 years since U.S. entry. The top five countries of origin accounting for the greatest number of tuberculosis cases among foreign-born persons in the United States are listed; cases among persons from other countries are classified according to tuberculosis incidence in the country of origin as low (<15 cases/100,000 persons), medium (15–99 cases/100,000 persons), or high (≥100 cases/100,000 persons). Countries with unknown incidence rates were excluded. All incidence rates used to categorize countries of origin are from World Health Organization data [1] and expressed per 100,000 persons.
When examining TB case rates, the greatest relative declines occurred among recent entrants from the Philippines (-51.3%), India (-47.3%), China (-47.0%), and Vietnam (-37.1%), whereas the smallest TB case rate decline was among Mexico-born recent entrants (-12.0%) (Table 2). The population of recent entrants from Mexico decreased (-50.1%), but the populations of recent entrants from China (+35.0%), Vietnam (+14.6%), and India (+14.3%) all increased, and the population of recent entrants from the Philippines remained largely unchanged (-2.4%).
Table 2. Changes in tuberculosis case counts, population estimates, and tuberculosis case rates among recenta entrants, 2007 and 2011.
| Tuberculosis Case Count | Population Estimateb (Thousands) | Tuberculosis Case Rate (per 100,000 Persons) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2007 | 2011 | Relative Change (%) | 2007 | 2011 | Relative Change (%) | 2007 | 2011 | Relative Change (%) | ||
| County of origin, top five high morbidityc | ||||||||||
| Mexico | 481 | 211 | -56.1 | 1,219 | 608 | -50.1 | 39.5 | 34.7 | -12.0 | |
| Philippines | 343 | 163 | -52.5 | 172 | 167 | -2.4 | 199.9 | 97.3 | -51.3 | |
| India | 254 | 153 | -39.8 | 257 | 294 | +14.3 | 98.7 | 52.0 | -47.3 | |
| Vietnam | 129 | 93 | -27.9 | 68 | 78 | +14.6 | 188.5 | 118.6 | -37.1 | |
| China | 116 | 83 | -28.4 | 195 | 263 | +35.0 | 59.5 | 31.5 | -47.0 | |
| Incidence in countries of origin, excluding the top fived | ||||||||||
| High | 754 | 582 | -22.8 | 449 | 481 | +7.0 | 167.5 | 119.1 | -28.9 | |
| Medium | 452 | 231 | -48.9 | 1,006 | 943 | -6.3 | 44.9 | 23.7 | -47.4 | |
| Low | 37 | 29 | -21.6 | 681 | 690 | +1.3 | 5.4 | 4.2 | -22.6 | |
a Recent entrants are foreign-born persons with <3 years since U.S. entry.
b Source: American Community Survey [8].
c The five countries of origin accounting for the greatest number of tuberculosis cases in the United States. In 2011, the estimated TB incidences in the top five countries were: Mexico (21/100,000 persons), Philippines (303/100,000 persons), India (80/100,000 persons), Vietnam (180/100,000 persons), China (75/100,000 persons) [1].
d Excluding cases from the top five countries of origin, we categorized the remaining cases of tuberculosis among recent entrants according to the tuberculosis incidence in the country of origin: low (<15 cases/100,000 persons), medium (15–99 cases/100,000 persons), or high (≥100 cases/100,000 persons) [1].
Recent Entrants: Country of Origin, Categorized by TB Incidence Rate, 2007–2011
Excluding the top five countries of origin, case count declines occurred among recent entrants from all groups, categorized by TB incidence rate, with the largest relative case count decline from medium-incidence countries (-48.9%, -221 cases) (Fig 3). Recent entrants from all incidence groups also experienced declines in TB case rate (Table 2). The populations of recent entrants from low- (+1.3%) and high-incidence (+7.0%) countries both increased, but the population of recent entrants from medium-incidence countries decreased (-6.3%).
Factors Contributing to the Decline, 2007–2011
Overall, 69.6% of the case count decline was among recent entrants (1,013 of 1,456 cases). Among recent entrants, an estimated 71.1% of the decline was from a decrease in the TB case rate, and the remaining 28.9% was the result of a decrease in the recent entrant population. When stratified by country of origin, 100% of the respective case count declines among recent entrants from China, India, and Vietnam (and 95.5% from the Philippines) were found to be the result of decreases in TB case rate. For recent entrants from Mexico, 80.7% of the case count decline was attributable to the decreased population, and 19.3% was a result of a decrease in TB case rate.
Non-recent entrants (≥3 years since U.S. entry) accounted for 30.4% of the overall foreign-born case count decline (443 of 1,456 cases). Among non-recent entrants, 100% of the case count decline was the result of a decrease in TB case rate—the non-recent entrant population increased during the study period.
Overseas Culture-Based TB Screening by Country of Origin, 2007–2011
During 2007–2011, the proportion of the new entrant population (<1 year since U.S. entry) with overseas culture-based TB screening varied by country of origin (Table 3). India, China, and Mexico had the lowest proportion of new entrants who received overseas TB screening (5.4%, 20.3%, and 23.7%, respectively), despite comprising the largest new entrant populations. The majority of the new entrant population from the Philippines (51.7%) and Vietnam (72.6%) received overseas culture-based TB screening during 2007–2011.
Table 3. Proportion of new entrant populationa with overseas culture-based tuberculosis screening, by country of origin, 2007–2011.
| Country of Origin | Implementation Dateb for Overseas Culture-Based Screening | New Entrant Population Estimatea (Thousands) | Number of New Entrants with Overseas Culture-Based Screeningc (Thousands) | Proportion of New Entrant Population with Overseas Culture-Based Screening (%) |
|---|---|---|---|---|
| Mexico | October 2007 | 1,315 | 311 | 23.7 |
| Philippines | October 2007 | 290 | 150 | 51.7 |
| India | October 2010 | 571 | 31 | 5.4 |
| Vietnam | February 2008 | 135 | 98 | 72.6 |
| China | July 2009 | 441 | 89 | 20.3 |
a Foreign-born persons living in the United States for <1 year, regardless of visa status or mode of entry. Source: American Community Survey [8].
b These dates represent the transition from smear-based to culture-based overseas screening. Source: Centers for Disease Control and Prevention [22].
c Only refugees or persons applying for permanent resident visas must undergo overseas tuberculosis screening. Those applying for other visa types (e.g., students, exchange visitors, temporary workers, tourists, and business travelers) and those who enter the United States without a visa (e.g., undocumented persons) are not required to receive overseas screening. Sources: U.S. Department of Homeland Security [12] and CDC’s Electronic Disease Notification system [13].
World Health Organization estimates [1] from 2007 and 2011 reveal declines in estimated TB incidence in China (-12.8%), India (-10.4%), Vietnam (-10.1%), and the Philippines (-6.8%). In contrast, Mexico had a slight increase in estimated TB incidence (+5.0%) (Table 4).
Table 4. Changes in Estimated Overseas Tuberculosis Incidence for the Top Five Countries of Origina, 2007 and 2011.
| Estimated Tuberculosis Incidenceb (per 100,000 Persons) | Percent Change (%) | |||
|---|---|---|---|---|
| 2007 | 2011 | |||
| Country of origin | ||||
| Mexico | 20 | 21 | +5.0 | |
| Philippines | 325 | 303 | -6.8 | |
| India | 201 | 180 | -10.4 | |
| Vietnam | 168 | 151 | -10.1 | |
| China | 86 | 75 | -12.8 | |
a The five countries of origin accounting for the greatest number of tuberculosis cases among foreign-born persons in the United States.
b Source: World Health Organization [1].
Transmission of TB among Recent Entrants in the United States, 2011
During January 1–September 30, 2011, of the 1,039 cases among recent entrants, 772 (74.3%) had at least one positive culture result (Table 5). Among the 720 (93.3%) cases with a known TB genotype, 30 (4.2%) were likely due to recent transmission and had at least one potential source case identified. We estimated that 12–16 of the 720 cases (1.7%–2.2%) were likely due to transmission from a recent entrant with infectious TB.
Table 5. Transmission of Mycobacterium tuberculosis among recenta entrants, 2011b.
| Number or Estimated Rangec | % | ||
|---|---|---|---|
| Cases among recent entrants | 1,039 | ||
| With at least one positive culture result | 772/1,039 | 74.3 | |
| With a genotype result | 720/772 | 93.3 | |
| Due to recent transmissiond | 30/720 | 4.2 | |
| By origin of source case | |||
| Foreign-born, recent entranta source case | 12–16/720 | 1.7–2.2 | |
| Foreign born, non-recenta entrant source case | 11–14/720 | 1.5–1.9 | |
| U.S.-born source case | 3–4/720 | 0.4–0.6 | |
a Recent entrants are foreign-born persons with <3 years since U.S. entry; non-recent entrants are foreign-born persons with ≥3 years since U.S. entry.
b Cases counted during January 1–September 30, 2011, in the U.S. National Tuberculosis Surveillance System; cases from October 1–December 31, 2011, were excluded to allow an additional 3-month period for belated identification of potential source cases.
c Range reflects low–high estimates. Low estimates include only scenarios where all potential source cases are from a given group (e.g., foreign-born recent entrants). High estimates include scenarios where at least one potential source case is from a given group.
d A given case was classified as due to recent transmission if at least one plausible source case was identified based upon clinical characteristics, genotyping data, and temporal and geographic proximity to the putative secondary case.
Discussion
We found an overall decline of 1,456 cases (-19.3%) among foreign-born persons during 2007–2011. All foreign-born subpopulations, regardless of time since U.S. entry, experienced declines in both TB case count and case rate.
We had hypothesized that the decline in TB cases among foreign-born persons was primarily the result of a decreased TB case rate among recent entrants (<3 years since U.S. entry) and a decreased number of foreign-born persons living in the United States (particularly recent entrants). Our overall findings support these hypotheses. Specifically, we determined that the majority (69.6%) of the case count decline was among recent entrants; 71.1% of the case count decline among recent entrants was the result of decreased TB case rates, and 28.9% was from a population decrease.
When we examined contributing factors to the decline among subpopulations of recent entrants, we identified substantial heterogeneity by country of origin. Among Mexico-born recent entrants, 80.7% of the case count decline was the result of a population decrease, and only 19.3% was from a case rate decline, consistent with previously reported results [11]. These findings imply that if immigration from Mexico were to markedly increase, the number of TB cases among Mexico-born recent entrants would also be expected to increase. In contrast, the case count decline among recent entrants among each of the other top five countries of origin was almost entirely the result of a case rate decline and therefore might be less affected by future immigration trends. These observations become particularly important in the context of ongoing demographic shifts among foreign-born persons in the United States [18, 19, 24].
At least four major factors could explain the observed declines in TB case rates among recent entrants: overseas culture-based TB screening, declining TB morbidity in the countries of origin, changing composition of recent entrants (e.g., a disproportionate decrease in recent entrants from high-incidence countries), and decreased transmission in the United States among recent entrants.
Previous studies have assessed the benefits of culture-based overseas TB screening [25–29], and a recent analysis specifically explored the contribution of culture-based overseas screening to the decline in foreign-born TB incidence in the United States [30]. We found that the proportion of recent entrants who received overseas culture-based TB screening varied greatly by country of origin. During 2007–2011, only 23.7% of the new entrant population from Mexico passed through overseas culture-based TB screening, in contrast with 72.6% of new entrant population from Vietnam. Because we found a stable TB case rate among recent entrants from Mexico and a large case rate decline among recent entrants from Vietnam, these data are consistent with a contribution to TB case reduction from overseas culture-based TB screening, particularly in countries where the screening covered a high percentage of the new entrant population.
However, like Mexico, a smaller proportion of the new entrant population from India (5.4%) and China (20.3%) passed through overseas culture-based TB screening during 2007–2011, and yet recent entrants from India and China also experienced substantial declines in TB case rates. These data demonstrate that, although overseas culture-based TB screening likely contributed to the TB case rate decline for specific countries of origin (e.g., Vietnam and the Philippines), other factors likely played a more prominent role in the TB case rate decline among recent entrants from other countries of origin (e.g., Mexico, India, and China). Prior studies have explored the potential impact of extending overseas TB screening to additional visa categories [28, 31] as well as testing and treating latent TB infection among refugees overseas [32]. While such programs might further reduce TB morbidity in the United States, these efforts would likely have a limited impact on persons originating from Mexico, the vast majority of whom enter the United States with a short-term visa or without a visa altogether [12, 19].
The second factor potentially contributing to the decline in TB case rates among recent entrants is decreased TB incidence in each of the top five countries of origin. From 2007–2011, there were declines in estimated TB incidence in China, India, Vietnam, and the Philippines, but a relatively stable estimated TB incidence in Mexico. Based upon these data, it is possible that declining morbidity in foreign countries contributed to the declining case rates seen among recent entrants from China, Vietnam, India, and the Philippines. However, as recent entrants may not be representative of the general population in the country of origin, the precise contribution of decreasing TB incidence overseas to the decline in TB cases in the United States remains uncertain.
The third factor that could explain the decrease in TB case rates is the changing composition of the recent entrant population. Excluding the top five countries of origin, the population of recent entrants from medium-incidence countries decreased (-6.3%) during the study period, while the population of recent entrants from low-incidence countries remained largely unchanged (+1.3%), and the population of recent entrants from high-incidence countries increased (+7.0%). There was a large decline in the recent entrant population from Mexico, but the recent entrant populations from Vietnam and the Philippines (high-incidence countries) as well as China and India (medium-incidence countries) all experienced increases or no change (Philippines) during 2007–2011. These findings indicate that the changing composition of recent entrants did not substantially contribute to the overall decline in TB case rates among recent entrants.
The fourth factor that could explain a decrease in TB case rates is less TB transmission among recent entrants. However, we found that a limited proportion of cases among recent entrants were likely due to recent transmission (4.2%), and an even smaller proportion (1.7%–2.2%) were likely due to transmission from a recent entrant source case. These findings are consistent with prior studies that established relatively low rates of transmission among foreign-born persons in the United States [33, 34]. Although data on transmission was limited to 2011 (and we could not assess trends over time), the extremely small proportion of cases associated with transmission make it unlikely that a change in transmission was a major contributor to the decline.
A substantial portion of the overall case count decline (30.4%) was among non-recent entrants (≥3 year since U.S. entry), and was therefore not accounted for by our hypotheses. Importantly, the case count decline among non-recent entrants was exclusively the result of a decrease in TB case rates. These decreasing rates might reflect a birth-cohort effect from a lower prevalence of latent TB infection among successive cohorts of immigrants [35]. This is of particular interest, as we must consider that a substantial proportion of the decline observed might be the result of global TB control efforts in foreign countries during the past several decades—a reminder of the importance of domestic returns from investing in TB control overseas [36]. Another factor that could explain the observed decline among non-recent entrants is improved TB control efforts in the United States through targeted testing and treatment of latent TB infection. However, targeted testing has not previously focused on non-recent entrants; therefore, this explanation seems less likely [37].
The substantial decline in TB case rate among non-recent entrants was an unexpected finding, and has implications for future TB morbidity trends in the United States. Despite a substantial decline in TB case rate (-16.6%), an increase in the size of the non-recent entrant population (+9.1%) dampened the reduction in TB cases. Non-recent entrants accounted for 73.8% of all cases among foreign-born persons in 2014, and if current trends continue, can be expected to be the dominant driver of future TB epidemiology in the United States.
Because of the enormous size of the non-recent entrant population (an estimated 41.2 million in 2014) [8], domestic efforts to reduce the TB case rate among this group (i.e., targeted testing and treatment of latent TB infection) could have a profound impact on TB morbidity as a whole in the United States. Although U.S. national guidelines recommend prioritizing testing of foreign-born persons who have been in the United States for <5 years [37], recent evidence suggests that rates of reactivation remain persistently elevated for years after arrival [17, 38]. At the same time, providing targeted testing and treatment to the entirety of the foreign-born population might not be feasible, given current health system resources [39, 40]. Therefore, there is an urgent need to identify a practical, prioritized approach to latent TB infection among foreign-born persons [41]. Studies that examine the cost-effectiveness of targeting foreign-born persons with specific risk factors for reactivation [42] could be used to focus testing and treatment of latent TB infection among this large and growing population.
One of the primary goals of TB surveillance is to understand trends in morbidity and to shape public health policies. However, because of shifts in immigration and changes in the distribution of TB cases among the foreign-born population (especially with respect to duration of time since U.S. entry), the standard approach to interpreting TB case counts and overall TB case rates might not be adequate. For example, if immigration increases in the future, this might result in an increase in foreign-born TB cases and be mistakenly interpreted as a failure of TB control efforts. Conversely, a further reduction in the TB case rate among non-recent entrants might result in an overall decline in cases among foreign-born persons, which might mask a simultaneous increase among recent entrants.
Our analyses have several limitations. First, there is statistical variability in the timing of the Joinpoint regression flexions, indicating the timing of the decline, and as a result, 2007–2011 is an estimate. Second, in the transmission analysis, we included persons diagnosed with TB <100 days after arrival, and therefore, might have misclassified cases as due to recent transmission in the United States that actually were due to transmission prior to U.S. entry. Third, as we were only able to assess transmission for TB cases diagnosed in 2011, we were unable to specifically evaluate changes in transmission during 2007–2011. Fourth, while the American Community Survey does not exclude persons on the basis of immigration status, it is possible that some proportion of undocumented persons are missed. Fifth, although a small proportion (4.5%) of overall cases had unknown years since U.S. entry and/or country of origin, these cases may differ from the overall study population. Sixth, persons may have passed through Mexico en route from another Latin American country to the United States, and could have been misclassified as Mexico-born.
Overall, we found that during 2007–2011, there was an abrupt decline in reported TB cases among foreign-born persons living in the United States, and this decline was evident among both recent and non-recent entrants. Among recent entrants, the decline was associated with a decrease in TB case rate as well as a decrease in population, but this varied by country of origin. In addition, non-recent entrants also substantially contributed to the decline, exclusively as a result of a decreasing TB case rate. Future TB morbidity trends among recent entrants may be closely linked to patterns of immigration and emigration. Strategies that impact both recent and non-recent entrants (e.g., investment in overseas TB control) as well as those that focus on non-recent entrants (e.g., targeted testing of high-risk subpopulations among non-recent entrants) will be necessary to achieve further declines in TB morbidity among foreign-born persons.
Acknowledgments
The authors gratefully acknowledge local and state public health departments, which collected the National Tuberculosis Surveillance System data included in these analyses.
The findings in this report are those of the authors and do not necessarily represent the official position of the U.S. Centers for Disease Control and Prevention.
Data Availability
The data contain information abstracted from the national tuberculosis (TB) case report form called the Report of Verified Case of Tuberculosis (RVCT) (OMB No. 0920-0026). These data have been reported voluntarily to CDC by state and local health departments, and are protected under the Assurance of Confidentiality (Sections 306 and 308(d) of the Public Health Service Act, 42 U.S.C. 242k and 242m(d)), which prevents disclosure of any information that could be used to directly or indirectly identify patients. For more information, see the CDC/ATSDR Policy on Releasing and Sharing Data (at http://www.cdc.gov/maso/Policy/ReleasingData.pdf). A limited dataset is available at http://wonder.cdc.gov/TB-v2013.html. Researchers seeking additional data may apply to analyze National TB Surveillance System data at CDC headquarters by contacting Dr. Thomas Navin (trn1@cdc.gov).
Funding Statement
The authors received no specific funding for this work, but are employees of the U.S. Centers for Disease Control and Prevention.
References
- 1.World Health Organization. Global tuberculosis report 2015 Geneva: World Health Organization; 2015. Available: http://www.who.int/tb/publications/global_report/en/. Accessed 1 Dec 2015. [Google Scholar]
- 2.Scott C, Kirking HL, Jeffries C, Price SF, Pratt R; Centers for Disease Control and Prevention (CDC). Trends in tuberculosis—United States, 2014. MMWR Morb Mortal Wkly Rep. 2015. March 20;64(10):265–9. Available: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6410a2.htm. Accessed 1 Dec 2015. [PMC free article] [PubMed] [Google Scholar]
- 3.Hill AN, Becerra J, Castro KG. Modelling tuberculosis trends in the USA. Epidemiol Infect. 2012. October;140(10):1862–72. 10.1017/S095026881100286X [DOI] [PubMed] [Google Scholar]
- 4.Woodruff RS, Winston CA, Miramontes R. Predicting U.S. tuberculosis case counts through 2020. PLoS One. 2013. June 13;8(6):e65276 10.1371/journal.pone.0065276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Winston CA, Navin TR, Becerra JE, Chen MP, Armstrong LR, Jeffries C, et al. Unexpected decline in tuberculosis cases coincident with economic recession—United States, 2009. BMC Public Health. 2011. November 7;11:846 10.1186/1471-2458-11-846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Reported tuberculosis in the United States, 2014. Atlanta, GA: US Department of Health and Human Services, CDC; 2015. Available: http://www.cdc.gov/tb/statistics/reports/2014/pdfs/tb-surveillance-2014-report.pdf. Accessed 1 Dec 2015. [Google Scholar]
- 7.Ghosh S, Moonan PK, Cowan L, Grant J, Kammerer S, Navin TR. Tuberculosis genotyping information management system: enhancing tuberculosis surveillance in the United States. Infect Genet Evol. 2012. June;12(4):782–8. 10.1016/j.meegid.2011.10.013 [DOI] [PubMed] [Google Scholar]
- 8.United States Census Bureau. American Community Survey. Washington, DC: US Department of Commerce, Census Bureau; 2015. Available: http://www.census.gov/acs/www/. Accessed 1 Dec 2015.
- 9.Cain KP, Haley CA, Armstrong LR, Garman KN, Wells CD, Iademarco MF, et al. Tuberculosis among foreign-born persons in the United States: achieving tuberculosis elimination. Am J Respir Crit Care Med. 2007. January1;175(1):75–9. [DOI] [PubMed] [Google Scholar]
- 10.Cain KP, Benoit SR, Winston CA, Mac Kenzie WR. Tuberculosis among foreign-born persons in the United States. JAMA. 2008. July 23;300(4):405–12. 10.1001/jama.300.4.405 [DOI] [PubMed] [Google Scholar]
- 11.Baker BJ, Jeffries CD, Moonan PK. Decline in tuberculosis among Mexico-born persons in the United States, 2000–2010. Ann Am Thorac Soc. 2014. May;11(4):480–8. 10.1513/AnnalsATS.201402-065OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.United States Department of Homeland Security, Office of Immigration Statistics; 2015. Available: http://www.dhs.gov/data-statistics. Accessed 1 Dec 2015.
- 13.Lee D, Philen R, Wang Z, McSpadden P, Posey DL, Ortega LS, et al. ; Centers for Disease Control and Prevention. Disease surveillance among newly arriving refugees and immigrants—Electronic Disease Notification System, United States, 2009. MMWR Surveill Summ. 2013. November 15;62(7):1–20. Available: http://www.cdc.gov/mmwr/preview/mmwrhtml/ss6207a1.htm. Accessed 1 Dec 2015. [PubMed] [Google Scholar]
- 14.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000. February 15;19(3):335–51. [DOI] [PubMed] [Google Scholar]
- 15.Clegg LX, Hankey BF, Tiwari R, Feuer EJ, Edwards BK. Estimating average annual percent change in trend analysis. Stat Med. 2009. December 20;28(29):3670–82. 10.1002/sim.3733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zuber PL, McKenna MT, Binkin NJ, Onorato IM, Castro KG. Long-term risk of tuberculosis among foreign-born persons in the United States. JAMA. 1997. July 23–30;278(4):304–7. [PubMed] [Google Scholar]
- 17.Walter ND, Painter J, Parker M, Lowenthal P, Flood J, Fu Y, et al. ; Tuberculosis Epidemiologic Studies Consortium. Persistent latent tuberculosis reactivation risk in United States immigrants. Am J Respir Crit Care Med. 2014. January 1;189(1):88–95. 10.1164/rccm.201308-1480OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Passel J, Cohn D, Gonzalez-Barrera A. Net migration from Mexico falls to zero—and perhaps less. Pew Research Center, Washington, D.C. Available: http://www.pewhispanic.org/files/2012/04/PHC-Net-Migration-from-Mexico-Falls-to-Zero.pdf. Accessed 1 Dec 2015.
- 19.Gonzalez-Barrera A, Lopez MH, Rohal M. More Mexicans leaving than coming to the U.S. Pew Research Center, Washington, D.C. Available: http://www.pewhispanic.org/files/2015/11/2015-11-19_mexican-immigration__FINAL.pdf. Accessed 1 Dec 2015.
- 20.Centers for Disease Control and Prevention. Notice to readers: revised technical instructions for tuberculosis screening and treatment for panel physicians. MMWR Morb Mortal Wkly Rep. 2008;57:292–3. Available: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5711a5.htm. Accessed 1 Dec 2015. [Google Scholar]
- 21.Centers for Disease Control and Prevention (CDC)/National Center for Emerging and Zoonotic Infectious Diseases. CDC immigration requirements: technical instructions for tuberculosis screening and treatment Atlanta, GA: US Department of Health and Human Services, CDC; 2009. Available: http://www.cdc.gov/immigrantrefugeehealth/pdf/tuberculosis-ti-2009.pdf. Accessed 1 Dec 2015. [Google Scholar]
- 22.Centers for Disease Control and Prevention (CDC)/Division of Global Migration and Quarantine. Tuberculosis screening and treatment technical instructions (TB TIs) using cultures and directly observed therapy (DOT) implementation Atlanta, GA: US Department of Health and Human Services, CDC; 2013. Available: http://www.cdc.gov/immigrantrefugeehealth/exams/ti/panel/tuberculosis-implementation.html. Accessed 1 Dec 2015. [Google Scholar]
- 23.France AM, Grant J, Kammerer JS, Navin TR. A field-validated approach using surveillance and genotyping data to estimate tuberculosis attributable to recent transmission in the United States. Am J Epidemiol. 2015. November 1;182(9):799–807. 10.1093/aje/kwv121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lopez MH, Passel J, Rohal M. Modern Immigration Wave Brings 59 Million to U.S., Driving Population Growth and Change Through 2065. Pew Research Center, Washington, D.C. Available: http://www.pewhispanic.org/files/2015/09/2015-09-28_modern-immigration-wave_REPORT.pdf. Accessed 1 Dec 2015.
- 25.Maloney SA, Fielding KL, Laserson KF, Jones W, Nguyen TN, Dang QA, et al. Assessing the performance of overseas tuberculosis screening programs: a study among US-bound immigrants in Vietnam. Arch Intern Med. 2006. January 23;166(2):234–40. [DOI] [PubMed] [Google Scholar]
- 26.Liu Y, Weinberg MS, Ortega LS, Painter JA, Maloney SA. Overseas screening for tuberculosis in U.S.-bound immigrants and refugees. N Engl J Med. 2009. June 4;360(23):2406–15. 10.1056/NEJMoa0809497 [DOI] [PubMed] [Google Scholar]
- 27.Lowenthal P, Westenhouse J, Moore M, Posey DL, Watt JP, Flood J. Reduced importation of tuberculosis after the implementation of an enhanced pre-immigration screening protocol. Int J Tuberc Lung Dis. 2011. June;15(6):761–6. 10.5588/ijtld.10.0370 [DOI] [PubMed] [Google Scholar]
- 28.Liu Y, Painter JA, Posey DL, Cain KP, Weinberg MS, Maloney SA, et al. Estimating the impact of newly arrived foreign-born persons on tuberculosis in the United States. PLoS One. 2012;7(2):e32158 10.1371/journal.pone.0032158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Posey DL, Naughton MP, Willacy EA, Russell M, Olson CK, Godwin CM, et al. ; Centers for Disease Control and Prevention (CDC). Implementation of new TB screening requirements for U.S.-bound immigrants and refugees—2007–2014. MMWR Morb Mortal Wkly Rep. 2014. March 21;63(11):234–6. Available: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6311a3.htm. Accessed 1 Dec 2015. [PMC free article] [PubMed] [Google Scholar]
- 30.Liu Y, Posey DL, Cetron MS, Painter JA. Effect of a culture-based screening algorithm on tuberculosis incidence in immigrants and refugees bound for the United States: a population-based cross-sectional study. Ann Intern Med. 2015. March 17;162(6):420–8. 10.7326/M14-2082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wingate LT, Coleman MS, Posey DL, Zhou W, Olson CK, Maskery B, et al. Cost-effectiveness of screening and treating foreign-born students for tuberculosis before entering the United States. PLoS One. 2015. April 29;10(4):e0124116 10.1371/journal.pone.0124116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wingate LT, Coleman MS, de la Motte Hurst C, Semple M, Zhou W, Cetron MS, et al. A cost-benefit analysis of a proposed overseas refugee latent tuberculosis infection screening and treatment program. BMC Public Health. 2015. December 1;15(1):1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chin DP, DeRiemer K, Small PM, de Leon AP, Steinhart R, Schecter GF, et al. Differences in contributing factors to tuberculosis incidence in U.S. -born and foreign-born persons. Am J Respir Crit Care Med. 1998. December;158(6):1797–803. [DOI] [PubMed] [Google Scholar]
- 34.Baker BJ, Moonan PK. Characterizing tuberculosis genotype clusters along the United States-Mexico border. Int J Tuberc Lung Dis. 2014. March;18(3):289–91. 10.5588/ijtld.13.0684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Winston CA, Navin TR. Birth cohort effect on latent tuberculosis infection prevalence, United States. BMC Infect Dis. 2010. July 13;10:206 10.1186/1471-2334-10-206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schwartzman K, Oxlade O, Barr RG, Grimard F, Acosta I, Baez J, et al. Domestic returns from investment in the control of tuberculosis in other countries. N Engl J Med. 2005. September 8;353(10):1008–20. [DOI] [PubMed] [Google Scholar]
- 37.Targeted tuberculin testing and treatment of latent tuberculosis infection. American Thoracic Society. MMWR Recomm Rep. 2000. June 9;49(RR-6):1–51. Available: http://www.cdc.gov/mmwr/PDF/rr/rr4906.pdf. Accessed 1 Dec 2015. [PubMed] [Google Scholar]
- 38.Patel S, Parsyan AE, Gunn J, Barry MA, Reed C, Sharnprapai S, et al. Risk of progression to active tuberculosis among foreign-born persons with latent tuberculosis. Chest. 2007. June;131(6):1811–6. [DOI] [PubMed] [Google Scholar]
- 39.Sterling TR, Bethel J, Goldberg S, Weinfurter P, Yun L, Horsburgh CR; Tuberculosis Epidemiologic Studies Consortium. The scope and impact of treatment of latent tuberculosis infection in the United States and Canada. Am J Respir Crit Care Med. 2006. April 15;173(8):927–31. [DOI] [PubMed] [Google Scholar]
- 40.Campbell J, Marra F, Cook V, Johnston J. Screening immigrants for latent tuberculosis: do we have the resources? CMAJ. 2014. March 4;186(4):246–7. 10.1503/cmaj.131025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Baker BJ, Jeffries CD, Moonan PK. Latent tuberculosis infection among foreign-born persons: a prioritized approach. Ann Am Thorac Soc. 2014. October;11(8):1335 10.1513/AnnalsATS.201406-291LE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mazurek GH, Jereb J, Vernon A, LoBue P, Goldberg S, Castro K; IGRA Expert Committee; Centers for Disease Control and Prevention (CDC). Updated guidelines for using Interferon Gamma Release Assays to detect Mycobacterium tuberculosis infection—United States, 2010. MMWR Recomm Rep. 2010. June 25;59(RR-5):1–25. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data contain information abstracted from the national tuberculosis (TB) case report form called the Report of Verified Case of Tuberculosis (RVCT) (OMB No. 0920-0026). These data have been reported voluntarily to CDC by state and local health departments, and are protected under the Assurance of Confidentiality (Sections 306 and 308(d) of the Public Health Service Act, 42 U.S.C. 242k and 242m(d)), which prevents disclosure of any information that could be used to directly or indirectly identify patients. For more information, see the CDC/ATSDR Policy on Releasing and Sharing Data (at http://www.cdc.gov/maso/Policy/ReleasingData.pdf). A limited dataset is available at http://wonder.cdc.gov/TB-v2013.html. Researchers seeking additional data may apply to analyze National TB Surveillance System data at CDC headquarters by contacting Dr. Thomas Navin (trn1@cdc.gov).