Abstract
Objective: To describe the management of pain prevention associated with burn care. Methods: Multi-centre, observational, cross-sectional, descriptive study performed in 4 burn units in Spain. Results: A total of 55 patients undergoing 64 procedures were analysed. Burns were classified as severe (90.4%), third-degree (78.2%) and caused by thermal agents (81.8%). Background analgesia consisted of non-opioid drugs (87.5%) and opioids (54.7%) [morphine (20.3%), morphine and fentanyl (14.1%) or fentanyl monotherapy (15.6%)]. Burn care was performed by experienced nurses (96.9%); 36.5% followed guidelines. The mean duration of procedures was 44 minutes (Statistical Deviation, SD: 20.2) and the mean duration of pain was 27 minutes (SD: 44.6). Procedural pain was primarily managed with opioid analgesics: fentanyl monotherapy and in combination (84%) and fentanyl monotherapy (48%) administered sublingually (89.1%). Patients described pain as different to usual baseline pain (97%), with a mean maximum intensity score of 4.2 points (SD: 3.3) on the VAS scale and a 34% increase in the intensity of pain. The mean patient and healthcare professional satisfaction score per procedure was 6/10 (SD: 1.9) and 5.5/10 (SD: 1.7), respectively. Conclusion: The results of the study describe the management of pain associated with burn care in clinical practice, helping optimise pain control.
Keywords: Burns, pain management, wounds, analgesia
Introduction
Local wound care including therapeutic procedures, wound debridement and dressing changes represents a source of pain and discomfort for burn injured patients. Procedural pain is described by patients as sharp and intense [1] and can be regarded as an exacerbation of background chronic pain [2]. Ineffectively managing procedural pain or the lack of an appropriate pain management plan may lead patients to lose trust in healthcare professionals (HCP), increase pain perception and affect wound healing [3]. Therefore pain management should be integrated as an essential component of the wound management plan in patients with severe burns. However it is not straightforward and a multidisciplinary approach ensuring all the components of pain perception and distress suffered by the burn patient are adequately addressed [4].
Clinical Practice Guidelines and protocols for burn care in place recommend the use of chronic treatments that tackle background pain and acute treatments in the prevention and relief of pain associated with burn care procedures [2,5-9]. Current therapeutic regimens consist of moderate to high potency opioids with rapid onset and short duration of action, administered either intravenously or orally. In this regard, short-acting opioids such as fentanyl or alfentanyl are preferable to long-lasting drugs such as morphine [10]. When difficulty in performing the local procedure is expected, anaesthetics can also be added to therapeutic regimens [1]. Pain can also be treated with simple analgesics (e.g. paracetamol) as well as other drugs such as ketamine [11] or gabapentin [12].
Despite the array of analgesic drugs and procedures available for pain management in burn injured patients that undergo wound care, pain remains insufficiently treated in current clinical practice and its management represents a major challenge for HCPs [12,13]. This phenomenon is commonly associated with the HCP’s fear of prescribing analgesics, however pain is complex in nature and other factors such as a lack of routinely used assessment tools and the involvement of patients’ psychological status (anxiety and fear) may also influence treatment patterns in burn patients [13]. The purpose of the study was to describe the management of pain associated with local care procedures for severely burned patients in current clinical practice and assess patients’ psychological responses (feelings and emotions) and satisfaction with the care received.
Material and methods
Study design
Multi-centre, cross-sectional study in patients with severe burn injuries (at least second-degree) undergoing wound care procedures and the HCP providing care in specialized burn units (BUs) of Spanish Hospitals. The study was performed in the BUs of four Spanish sites distributed across the autonomous community of Murcia, Valencia, Madrid and Aragón; Hospital Virgen de la Arrixaca (HVA), Hospital de la Fe (HF), Hospital de Getafe (HG) and Hospital de Miguel Servet (HMS), respectively. Patients attending the participating BUs to receive local wound care and fulfilling selection criteria were invited to participate in the study. After giving written informed consent by patients at the study visit, HCPs asked through face to face interviews to complete the Case Report Form (CRF) accordingly to the sequence in which it was structured: pre and post-wound care questions. The study included an additional CRF for the HCP performing the procedure. Both CRFs were recorded by the HCP due to patients’ condition. The study was approved by the Ethics Committee of HVA (Murcia). Further approvals were received for HF, HG by the centre and for the HMS by the autonomous community.
Study population
Patients attending the BUs of participant centres between November 2012 and April 2013 were sequentially included in the study. Only patients of legal age (≥ 18) with severe burns that presented with severe baseline pain and were to receive local wound care that was expected to cause pain were invited to participate. Patients that as per physician’s discretion did not have the required cognitive ability to understand the study were excluded. Given the exploratory nature of the study, no more recruitment constraints were stated. The sample size finally achieved reflects the amount of workload of this type of procedures in the participating centres during the study period. Data were collected from two populations, patients and health staff. Patients were interviewed by the HCPs to collect socio-demographic data (including addictions), burn characteristics, management (treatment) and pain (Brief Pain Inventory, BPI, and Visual Analogic Scale, VAS) before and after of the wound care session. It was also collected data about anxiety (Hamilton Anxiety Rating Scale, HARS) before the procedure and data about satisfaction after of it. HCPs were characterized according to their role (medical doctor or nurse) and asked about their satisfaction (HARS) after the procedure.
Outcome measures
The primary endpoint of the study was the management of pain related to local care procedures in severe burn injuries. All therapeutic measures and analgesic treatments were recorded in the CRF designed to this end. Pain management was assessed through a categorical variable, each category representing a therapeutic alternative or aggregation of alternatives in periprocedurial analgesic management. As secondary objectives of the study, patient feelings were operationalized as the relative amount of perceived change in pain (RACP) during the procedure (difference between baseline pain and after the procedure); patient emotions as their anxiety during the procedure; and patients’ satisfaction and satisfaction of HCP with the technique used in terms of the difficulty in pain management were assessed. Burn injuries were characterised according to severity, burn injury depth and causative agent [7,14].
Intensity of pain produced during local care procedures; Visual Analog Scale (VAS) and Brief Pain Inventory (BPI)
The intensity of pain produced during burn care procedures was assessed by means of the Visual Analog Scale (VAS) [15] that rates from 0 (no pain) to 10 (maximum intensity of pain), the Brief Pain Inventory (BPI) [16] and an estimate of pain duration in minutes. BPI consists of two dimensions; intensity of pain (pain severity score; 4 items) and interference with daily life activities (pain interference score; 7 items). Each of the 11 items are scored 0 to 10, where 0 represents ‘no pain/interference’ and 10 ‘the worst pain/maximum interference’. The total scores for the pain intensity dimension are calculated by adding the scores of the 4 items, while the interference dimension is estimated by adding the scores for the corresponding items and dividing by 7.
Similarly, a 0 to 10 points VAS was used to assess baseline pain so as procedural pain could be discriminated from usual baseline pain experienced by the patient. The relative change in pain intensity was obtained by deducting the intensity of pain experienced during the procedure to the baseline intensity and dividing the difference by the baseline intensity. The RACP produced was calculated by multiplying the relative change in pain intensity by the proportion of procedure time in which the patient referred having pain. Consequently, the RACP ranged between -10 to +10, with negative values showing increases in pain intensity during the procedure, a value of 0 when there is no pain or change in basal pain, and greater absolute values for greater changes and longer pain periods during the procedure. Consequently, absolute values below 1 represented lower changes in pain intensity and shorter procedure time with pain.
Hamilton Anxiety Rating Scale (HARS)
The Hamilton Anxiety Rating Scale (HARS) [17] is a hetero-applied scale consisting of 14 items; 13 items relative to signs and symptoms of anxiety and the remaining item as an assessment of patient’s behaviour during the interview. The interviewer scores each item from 0 to 4, considering intensity and frequency of pain. The total score is the sum of the scores given to each item (from 0 to 56 points). Additionally, two different scores can be obtained from HARS; psychic anxiety and somatic anxiety.
Patient and healthcare professional satisfaction questionnaires
Patients’ satisfaction with therapeutic measures used in the management of pain was assessed through a questionnaire that consisted of 4 Likert-like questions and 5 response categories ranging from 1 ‘strongly disagree’ to 4 ‘strongly agree’. The first two questions are relative to pain perception while the remaining two are related to the method used. The HCP satisfaction questionnaire consisted of three Likert-like five-category questions. The total score for each of the questionnaires was calculated by adding the scores for the corresponding questions. Four or 3 units, as it corresponds, were deducted to the resulting score for the patients and HCP questionnaires that was subsequently divided by 1.6 or 1.2, respectively. The scores for the two questionnaires have the same rating scales and thus the results are comparable.
Statistical analysis
A descriptive analysis of patients included in the participant population set, their burns and previous management of pain, as well as a profile of the professional providing health care was carried out. The procedure population set was used to describe wound care procedures, patients’ feelings and emotions on pain, RACP and patients’ and professionals’ satisfaction with care.
Results
Description of patients
A total of 55 patients with severe burn injuries, fulfilling the selection criteria, that attended the 4 participating centres to undergo burn care were analysed: 22 patients in HVA (40%), 22 in HF (40%), 6 in HG (11%) and the remaining 5 in HMS (9%).
Patients included in the study were mainly male (76.4%), aged 40 or over (63.6%) and caucasian (92.6%). Overall, 50% of patients were employed and the highest level of education achieved was primary education (33.3%). Addictive behaviour was reported in 12 patients (22.2%); among them 41.7% used cannabis, 8.3% opioids and 25% cocaine. Regarding medical history relevant to the procedure, one patient reported blood clotting disorders (1.8%) and five had hypertension (10.9%). Among other medical conditions, type II diabetes was the most frequently reported (4 patients).
Demographic characteristics of study population are summarised in Table 1.
Table 1.
Sociodemographic characteristics of study population
| Total | ||
|---|---|---|
|
|
||
| n | % | |
| Age (years) | ||
| < 30 | 10 | 18.2 |
| 30-39 | 10 | 18.2 |
| 40-49 | 16 | 29.1 |
| ≥ 50 | 19 | 34.5 |
| Total | 55 | 100 |
| Sex | ||
| Males | 42 | 76.4 |
| Females | 13 | 23.6 |
| Total | 55 | 100 |
| Race | ||
| Caucasian | 50 | 92.6 |
| Oriental | 1 | 1.9 |
| Arabic | 3 | 5.6 |
| Total | 54 | 100 |
| Employment status | ||
| Employed | 27 | 50 |
| Unemployed | 7 | 13 |
| Retired | 9 | 16.7 |
| Housewife | 2 | 3.7 |
| Student | 2 | 3.7 |
| On sick leave | 3 | 5.6 |
| Others | 4 | 7.4 |
| Total | 54 | 100 |
| Education level | ||
| No education | 12 | 22.2 |
| Primary education | 18 | 33.3 |
| Secondary education | 11 | 20.4 |
| Vocational training | 8 | 14.8 |
| Higher education | 5 | 9.3 |
| Total | 54 | 100 |
| CMI classification | ||
| Normal | 19 | 38.8 |
| Overweight | 19 | 38.8 |
| Obese | 11 | 22.4 |
| Total | 49 | 100 |
| Addictions | ||
| No | 42 | 77.8 |
| Yes | 12 | 22.2 |
| Total | 54 | 100 |
Description of procedures
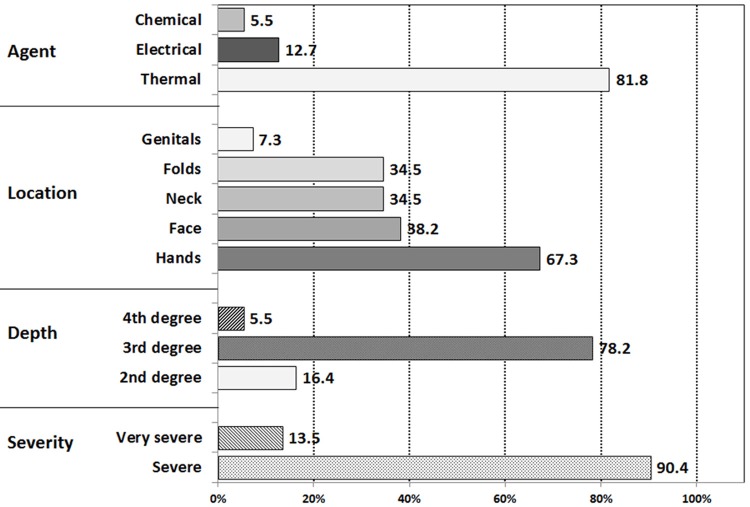
In forty five (81.8%) patients undergoing wound care procedures, burns were caused by thermal agents. Based on the burn surface area, burns in the study were mainly severe (90.4%) and, according to burn depth, third-degree burns were more frequent (78.2%). Hands, at 67.3%, and face, at 38.2%, were the most common locations. The mean time since injury was de 33 days (SD: 32.6). Figure 1 shows the distribution of locations and types of burns.
Figure 1.
Classification of burns based on agent, location, depth and severity.
Complications due to the burn itself (20%) and local infections (12.5%) were the most frequently reported complications.
A total of 96.9% of HCP performing the burn care procedure at the study visit were nurses with a mean of 20 years of experience (SD: 8.1). Overall, 36.5% of HCP participating in the study performed the procedures following clinical guidelines or protocols.
Baseline pain management and pain scores
A total of 64 burn care procedures were included in the present study. Forty nine were single procedures in different participants; four patients provided data on two procedures and two participants on three.
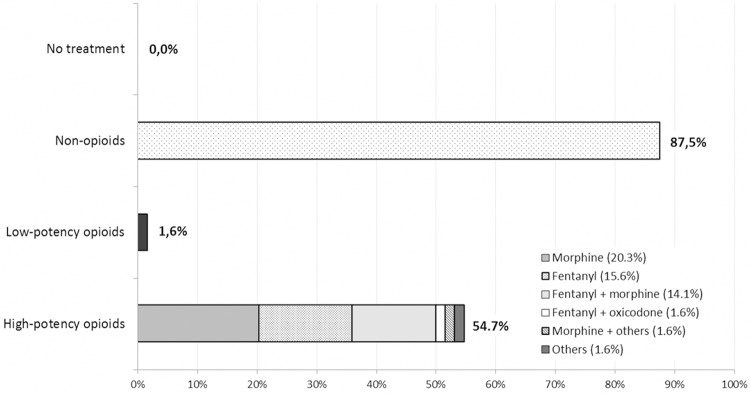
The mean intensity of baseline pain was 3.8 (SD: 2.6). As it is shown in Figure 2, among the treatments used alone or in combination with other treatments used, 87.5% of procedures used with non-opioids, mainly paracetamol with metamizol (35.7%) and metamizol (26.8%), and 54.7% with opioids. The most frequently reported opioids used for baseline pain were morphine monotherapy (20.3%), fentanyl monotherapy in 15.6% and 14.1% receiving fentanyl and morphine in combination.
Figure 2.
Analgesic medication used in baseline pain management.
Intra-procedure pain management and pain scores
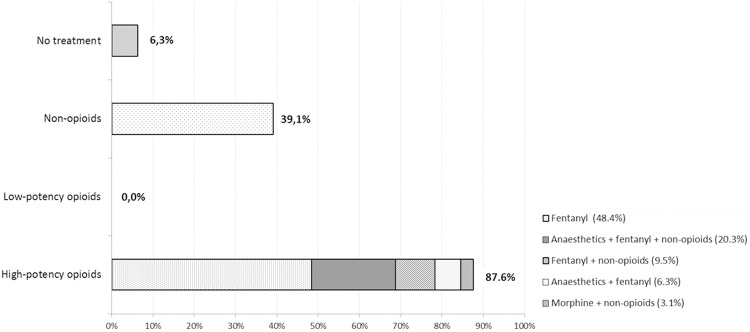
During burn care performed in the study visit, 6.3% procedures did not receive any treatment, opioids were given in 54.6% procedures, non-opioids alone in 6.1% and 33.0% received a combination of opioids and non-opioids (39.1%) (Figure 3). Primary management of pain was with opioids such as fentanyl monotherapy (48.4%) and in combination (36.1%), and morphine (3.1%). As shown in Figure 4, fentanyl was usually administered sublingually (89.1%). Additionally, 26.6% of the procedures were performed with anaesthetics.
Figure 3.
Analgesic medication used in the management of pain related to wound care procedures.
Figure 4.
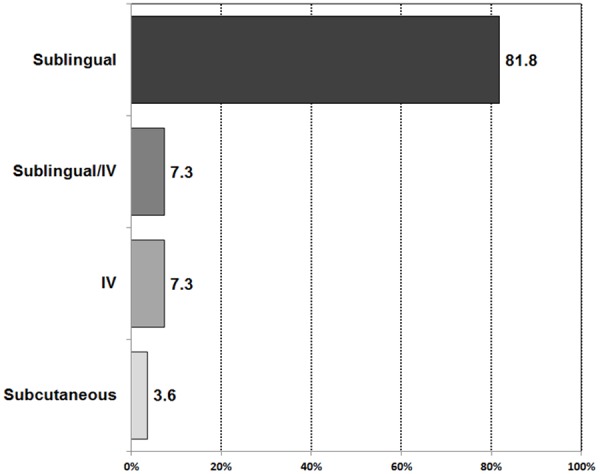
Routes of administration of fentanyl.
According to the BPI questionnaire, mean score of pain intensity produced during procedures was 16/40 points (SD: 8.4) and interference with daily life activities was 6/10 (SD: 2.4). In 96.9% of burns pain was described as being different to usual baseline pain. The mean intensity of maximum pain was 4.2 points in the VAS scale. The mean duration of the burn care procedures performed was 44 minutes (SD: 20.2), ranging from a minimum of 15 to a maximum of 110 minutes and the mean duration of pain was 27.2 minutes (SD: 44.6). The mean ratio of time with pain during procedure was 35% (SD: 21), there was a change of -34% (IC95%: -77.7, 9.7) which means an increase in the intensity of pain experienced with the 95% confidence interval including the value of 0. The mean relative amount of pain of -0.33 (IC95%:-0.63,-0.03). In the HARS scale, a mean score of 8.7 (SD: 7.7) was obtained; 5.7 (SD: 5.2) for psychic anxiety and 3.2 for somatic anxiety (SD: 3.5).
Patient and health staff satisfaction
Overall, the mean patient satisfaction score per procedure was 6/10 (SD: 1.9); a score of 3.8 for the intensity of pain, 3.8/5 for the effectiveness of pharmacologic treatment (SD: 1.1), a score of 3/5 for the management of wound careby the HCP (SD: 0.7) and 2.9/5 for satisfaction with the duration of the procedure (SD: 0.8). The mean HCP satisfaction score was 5.5/10 (SD: 1.7) and the mean scores for individual items were 3/5 (SD: 0.7) for satisfaction with the management of the burn patient, 3.8/5 (SD: 0.9) for satisfaction with the duration of the procedure and 2.8/5 (SD: 1.1) for satisfaction with analgesic control.
Discussion
The results of the study provide a description of the current management of pain related to wound care procedures in severe burn patients.
Pain management in burn patients is complex and individual therapeutic approaches combining both acute and chronic pharmacologic treatments need to be incorporated into therapeutic regimens, addressing procedural and baseline pain, respectively. The management of baseline pain usually requires long-term analgesia consisting of long-acting drugs that provide chronic pain relief. In contrast, short-acting analgesic drugs with rapid onset of action are used to minimise acute pain produced during wound care [10]. Treatment guides in place recommend the use of opioids for rapid pain relief in burn patients that undergo wound care [2,5,8,9,18].
The results of the study describe the range of therapeutic measures currently used to manage the analgesic treatment of burn patients in the long term and during the episodes of wound care, in order to minimise their pain and anxiety, improve the procedural performance and shorten its duration; mainly severe third-degree burn injuries, caused by thermal agents. In the study, the majority of patients were treated with background non-opioid pain-killers and over half of them received opioids. During wound care, opioids were administered in 9 out of 10 patients, being fentanyl the most frequently used among them, which was mainly administered sublingually. In average, patients reported moderate intra-procedural pain intensity during approximately 35% of the time undergoing the procedure. Compared with the baseline pain, there seems to be a slight increase in the intensity of pain during wound care. As 0 is included in the CI, an increase in the intensity of pain cannot be claimed. According to the HARS scale, the levels of anxiety were moderate and predominantly psychic, whereas other studies report higher levels of anxiety [19,20]. The approaches to pain and anxiety management should be multifactorial [20]. Patient and HCP ratings on satisfaction were very similar (5.5 vs. 6 point over 10). Overall, the mean patient and HCP satisfaction score was moderate, as it was for patients’ satisfaction with wound care duration and with the HCP. Higher satisfaction values were observed for patients’ satisfaction with pain intensity and with treatment effectiveness. These findings are consistent with results obtained in similar studies that investigate the influence of different factors on general patients’ satisfaction [21]. HCP reported more satisfaction with wound care duration and management, and less satisfaction with analgesic control. Burn injury care was predominantly performed by experienced nurses, only 1 of every 3 followed guidelines. This may result in a certain degree of variability in clinical practice among study sites, and may indicate poor knowledge of recently introduced techniques and analgesic recommendations [22].
This study presents some strengths and limitations associated with the study design that should be acknowledged. The cross-sectional design of the study was appropriate to describe the characteristics of pain management in patients with burns and to characterise the different analgesic alternatives used with special interest in the association with the procedure, pain management and pain experienced by the patient [23]. Selected scales and questionnaires allowed assessing the intensity of pain produced during wound care. In particular, the BPI questionnaire was originally developed to be used in epidemiological and clinical studies aimed at evaluating the effectiveness of analgesic treatments. Similar studies also utilise the EVA scale and BPI questionnaire [24]. One of the limitations of the study is the reduced sample size that limits the study power. However, these samples sizes are frequent among studies performed in burn patients [25] and the aim of the study was mainly descriptive. Regarding the selection criteria, other limitation is that a precise definition of ‘severe baseline pain’ was not provided. Therefore the minimum intensity of baseline pain was determined by the doctor based on medical criteria rather than an objective assessment tool. This has resulted into the inclusion of patients whose baseline-referred values for pain intensity were 0. However, it should be borne in mind that when patients are treated for wound care they are already on strong analgesic treatments. Indeed, if patients are treated as current guidelines recommend their level of pain should be close to 0 [2,5,8,9,18,26]. In these circumstances, medical criteria based on the characteristics of burns and their severity may suffice to assess if the patient is candidate to suffer from pain during the manipulation.
Conclusions
The results of the study help understand how burn pain associated with wound care is managed in current clinical practice, helping optimise pain control and management and therefore improving the quality of care delivered to burn patients. Studies of this nature contribute to identify the analgesic alternatives that are available to relief procedural pain in burn patients and assess the application of guidelines in clinical practice.
Acknowledgements
The authors wish to acknowledge the staff of the centres that participated in the study (Hospital Virgen de la Arrixaca, Hospital de la Fe, Hospital de Getafe and Hospital de Miguel Servet).
Abbreviations
- BPI
Brief Pain Inventory
- BU
burn unit
- CRF
case report form
- HARS
Hamilton Anxiety Rating Scale
- HCP
Healthcare Professionals
- HVA
Hospital Virgen de la Arrixaca
- HF
Hospital de la Fe
- HG
Hospital de Getafe
- HMS
Hospital de Miguel Servet
- RACP
relative amount of perceived change in pain
- SD
Standard Deviation
- VAS
Visual Analog Scale
Disclosure of conflict of interest
None.
References
- 1.Richardson P, Mustard L. The management of pain in the burns unit. Burns. 2009;35:921–36. doi: 10.1016/j.burns.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 2.European wound managemnt association. Pain at wound dressing changes-Position document. 2007 [Google Scholar]
- 3.Weddell R. Improving pain management for patients in a hospital burns unit. Nurs Times. 2004;100:38–40. [PubMed] [Google Scholar]
- 4.Esfahlan AJ, Lotfi M, Zamanzadeh V, Babapuor J. Burn pain and patients’ responses. Burns. 2010;36:1129–33. doi: 10.1016/j.burns.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 5.Organización Médica Colegial de España. Guía de buena práctica clínica en Dolor y su tratamiento. 2004 [Google Scholar]
- 6.Latenser BA. Critical Care of the Burn Patient: The First 48 Hours. Crit Care Med. 2009;37:2819–26. doi: 10.1097/CCM.0b013e3181b3a08f. [DOI] [PubMed] [Google Scholar]
- 7.Servicio Andaluz de Salud. Manejo del Paciente Quemado. 2000 [Google Scholar]
- 8.Tsirigotou S. Acute and chronic pain resulting from burn injuries. Annu Mediterr Burn Club. 1993:6. [Google Scholar]
- 9.Servicio Andaluz de Salud. Guía de práctica clínica para el cuidado de personas que sufren. 2011 [Google Scholar]
- 10.De Castro RJA, Leal PC, Sakata RK. Pain management in burn patients. Brazilian J Anesthesiol. 2013;63:149–53. doi: 10.1016/j.bjane.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 11.López-Millán JM, Sánchez-Blanco C. Dolor y medicina basada en la evidencia. Rev Soc Española Del Dolor. 2007;1:45–65. [Google Scholar]
- 12.Gray P, Williams B, Cramond T. Successful use of gabapentin in acute pain management following burn injury: a case series. Pain Med. 2008;9:371–6. doi: 10.1111/j.1526-4637.2006.00149.x. [DOI] [PubMed] [Google Scholar]
- 13.Summer GJ, Puntillo KA, Miaskowski C, Green PG, Levine JD. Burn injury pain: the continuing challenge. J Pain. 2007;8:533–48. doi: 10.1016/j.jpain.2007.02.426. [DOI] [PubMed] [Google Scholar]
- 14.Connor-Ballard PA. Understanding and managing burn pain: Part 1. Am J Nurs. 2009;109:48–56. doi: 10.1097/01.NAJ.0000348604.47231.68. [DOI] [PubMed] [Google Scholar]
- 15.Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP) Arthritis Care Res (Hoboken) 2011;63(Suppl 1):S240–52. doi: 10.1002/acr.20543. [DOI] [PubMed] [Google Scholar]
- 16.Badia X, Muriel C, Gracia A, Núñez-olarte JM, Método PAY. [Validation of the Spanish version of the Brief Pain Inventory in patients with oncological pain] Med Clin (Barc) 2003;120:52–9. doi: 10.1016/s0025-7753(03)73601-x. [DOI] [PubMed] [Google Scholar]
- 17.Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32:50–5. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 18.Molina VS, Barranco CO, Martín Muñoz F, FJ D la MD. Protocolo de actuación y manejo del paciente quemado en el Servicio de Urgencias. 2005 [Google Scholar]
- 19.Carrougher GJ, Ptacek JT, Honari S, Schmidt AE, Tininenko JR, Gibran NS, Patterson DR. Self-reports of anxiety in burn-injured hospitalized adults during routine wound care. J Burn Care Res. 2006;27:676–81. doi: 10.1097/01.BCR.0000238100.11905.AB. [DOI] [PubMed] [Google Scholar]
- 20.Byers JF, Bridges S, Kijek J, LaBorde P. Burn patients’ pain and anxiety experiences. J Burn Care Rehabil. 2001;22:144–9. doi: 10.1097/00004630-200103000-00011. [DOI] [PubMed] [Google Scholar]
- 21.Carrougher GJ, Ptacek JT, Sharar SR, Wiechman S, Honari S, Patterson DR, Heimbach DM. Comparison of patient satisfaction and self-reports of pain in adult burn-injured patients. J Burn Care Rehabil. 2003;24:1–8. doi: 10.1097/00004630-200301000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Love T. Variation in medical practice: literature review and discussion About Sapere Research Group Limited. 2013 [Google Scholar]
- 23.Levin KA. Study design III: Cross-sectional studies. Evid Based Dent. 2006;7:24–5. doi: 10.1038/sj.ebd.6400375. [DOI] [PubMed] [Google Scholar]
- 24.Jaywant SS, Pai AV. A comparative study of pain measurements scales in acute burn patients. Indian J Occup Heal. 2003:XXXV. [Google Scholar]
- 25.Zhou B, Zhou X, Ouyang L, Huang XY, Zhang PH, Zhang MH, Ren LC, Liang PF. An epidemiological analysis of paediatric burns in urban and rural areas in south central China. Burns. 2014;40:150–6. doi: 10.1016/j.burns.2013.04.020. [DOI] [PubMed] [Google Scholar]
- 26.Martí Minguiz A, López Alarcón MD, Palomar F, De Andrés J. Protocolo terapéutico multidisciplinar del tratamiento del dolor en pacientes con úlceras cutáneas dolorosas. Enfermería Dermatológica. 2010;11:35–9. [Google Scholar]