Abstract
Background
Unhealthy alcohol use could impair recovery of older patients after medical or surgical hospitalizations. However, no prior research has evaluated whether older patients who screen positive for unhealthy alcohol use are at increased risk of readmissions or emergency department (ED) visits within 30 days after discharge. This study examined the association between AUDIT-C alcohol screening results and 30-day readmissions or ED visits.
Methods
Veterans Affairs (VA) patients age 65 years or older, were eligible if they were hospitalized for a medical or surgical condition (2/1/2009–10/1/2011) and had an AUDIT-C score documented in their VA electronic medical record in the year before they were hospitalized. VA and Medicare data identified VA or non-VA index hospitalizations, readmissions, and ED visits. Primary analyses adjusted for demographics, comorbid conditions, and past-year health care utilization.
Results
Among 579,330 hospitalized patients, 13.7% were readmitted and 12.0% visited an ED within 30 days of discharge. In primary analyses, high-risk drinking (n = 7167) and nondrinking (n =357,086) were associated with increased probability of readmission (13.8%, 95% CI 13.0–14.6%; and 14.2%, 95% CI 14.1–14.3%, respectively), relative to low-risk drinking (12.9%; 95% CI 12.7–13.0%). Only nondrinkers had increased risk for ED visits.
Conclusions
Alcohol screening results indicating high-risk drinking that were available in medical records were modestly associated with risk for 30-day readmissions and were not associated with risk for ED visits.
Keywords: Alcohol screening, Quality, Unhealthy alcohol use, Emergency department, Readmissions, Post-discharge care
1. Introduction
Efforts to improve the quality of hospital care often focus on readmissions within 30 days of hospital discharge because readmissions can reflect a poor outcome for patients and higher costs for the health care system (Jencks et al., 2009). Hospital readmissions are common among older adults and are an international hospital quality indicator (Blunt et al., 2015; Gerhardt et al., 2014; Jencks et al., 2009; Parker, 2005). In the U.S., the Centers for Medicare and Medicaid Services (CMS) recently implemented the hospital readmission reduction program (Centers for Medicare and Medicaid Services, 2014) and funded implementation of care coordination interventions (Brock et al., 2013; Voss et al., 2011), based on evidence that readmissions can be prevented with proper transitional support and discharge planning (Coleman et al., 2006; Leppin et al., 2014). Use of emergency departments (ED) could also indicate poor transitions following inpatient care (Baier et al., 2013; Kocher et al., 2013), but has received less attention from policy makers and is not currently monitored as a hospital quality metric. However, previous literature has highlighted many complex patient-level characteristics that may contribute to risk for readmissions and ED visits, such as patient age, gender, or socioeconomic status (Amarasingham et al, 2010; Arbaje et al., 2008), which may not be modifiable characteristics within the control of hospitals.
Unhealthy alcohol use is a potentially modifiable health behavior that may be a risk factor for readmissions in the elderly. While several studies have examined the association between unhealthy alcohol use and readmissions (Kartha et al., 2007; Rubinsky et al., 2012; Walley et al, 2012; Wei et al, 2015), no prior study has focused on older adults. Prior studies have also not utilized alcohol screening results documented in the electronic health record (EHR) as part of routine care, and have not examined the association between unhealthy alcohol use and ED visits in the 30 days after discharge. While unhealthy alcohol use is less common among older adults, nearly 9% drink at unhealthy levels based on self-reported consumption (Kirchner et al., 2007), although the exact prevalence is unknown. Older adults are particularly vulnerable to the adverse effects of alcohol (National Institute on Alcohol Abuse and Alcoholism, 2005), but are less likely than younger patients to have alcohol use assessed during clinical care (Burman et al, 2004; Duru et al., 2010).
Routine alcohol screening with the Alcohol Use Disorder Identification Test-Consumption (AUDIT-C) screening questionnaire was implemented in the U.S. Veterans Health Administration (VA) in 2004 (Bradley et al., 2006). The VA is the largest integrated health care system in the U.S. and provides care for over 5 million patients annually (Kizer and Dudley, 2009). VA patients generally have poorer health status and more comorbidities, including mental health conditions, than non-VA patients (Ajmera et al, 2011; Selim et al., 2010). The VA has emerged as a leader in implementation of alcohol screening and other health systems are increasingly implementing alcohol screening as well (Jonas et al., 2012). Yet, it is currently unknown whether available alcohol screening results, collected as part of routine care during outpatient visits, could be useful for identifying hospitalized older adults at increased risk for hospital readmissions and ED visits within 30 days of hospital discharge.
The present study's objectives were to examine whether unhealthy alcohol use, according to AUDIT-C scores documented in the VA's EHR, was associated with (1) increased risk for readmissions or (2) increased risk for ED visits, in the 30 days following a hospitalization for a medical or surgical condition in a national sample of older VA patients. If unhealthy alcohol use was associated with increased 30-day hospital readmissions or ED visits, it could indicate an opportunity for clinicians and health systems to deliver targeted alcohol-related interventions for hospitalized patients in an effort to reduce hospital readmissions or ED use.
2. Methods
2.1. Data sources and study sample
The VA's Corporate Data Warehouse (CDW) provided data for VA acute care hospitalizations, outpatient utilization, AUDIT-C scores, demographics, and date of birth and death. The VA Information Resource Center (VIReC) provided Medicare Inpatient, Outpatient, and Carrier standard analytic files for non-VA inpatient and outpatient utilization.
The study sample included all VA outpatients age 65 or older who were hospitalized for a medical or surgical condition at a VA or non-VA hospital (2/1/2009–12/31/2011) and had at least one AUDIT-C score available in their VA medical record (2/1/2008–12/31/2011). Study eligibility criteria were then applied to this sample based on 30-day readmission measures developed for CMS (Horwitz et al., 2013), with some modifications in order to include only community-dwelling older adults discharged to the community. The study was restricted to patients discharged to the community because the mechanism by which unhealthy alcohol use was hypothesized to impact the risk of readmission or ED visits – decreased medication adherence and self-care, or falls due to drinking after discharge – was unlikely to impact institutionalized patients. Patients were included if they met the following criteria: (1) survived the hospital stay, (2) length of stay <30 days, (3) primary diagnosis not for a psychiatric condition, cancer, or physical rehabilitation, (4) admitted from the community, (5) not discharged to another facility, (6) not discharged against medical advice, (7) discharged before 10/1/2011 (to allow adequate follow-up), and 8) documented AUDIT-C score 1–365 days prior to admission (Fig. 1). Hospitalizations were categorized as medical or surgical based on the Diagnosis Related Group (DRG) code; hospitalizations without a valid DRG were excluded. Finally, patients enrolled in Medicare managed care plans in the year before or 30 days after hospitalization were excluded because information on readmissions and comorbidities would be incomplete. The final study cohort included 579,330 eligible patients (54% of total hospitalized patients; Fig. 1). For patients with multiple eligible hospitalizations, only the first stay was included. This study received human subjects approval, including waivers of informed consent and HIPAA authorization, from the University of Washington and VA Puget Sound Institutional Review Boards.
Fig. 1.
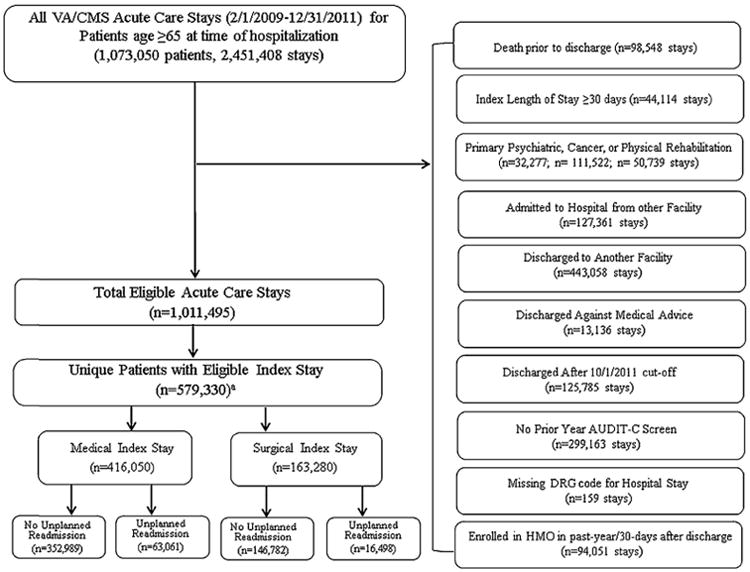
Study flow diagram and eligibility criteria.aThe first eligible index stay is used for patients with multiple potentially eligible index stays.
2.2. Outcomes
This study assessed two outcomes in the 30 days after discharge from the “index” (i.e., initial) hospitalization: (1) any hospital readmission and (2) any ED visit. Readmissions were defined as any unplanned hospital admission within 30 days of discharge. The algorithm for identifying eligible readmissions was adapted from the CMS hospital-wide all-cause readmission measure (Supplementary material 11; Horwitz et al, 2013). Potentially planned procedures were identified based on DRG codes used in a previous study (Jencks et al., 2009) and were excluded unless an acute principal diagnosis was present (Horwitz et al., 2013). ED visits were defined as any treat-and-release ED visit within 30 days of discharge (i.e., ED visits not resulting in re-hospitalization).
2.3. Alcohol risk group
Alcohol risk group was the independent variable of interest, based on each patient's most recent AUDIT-C score in the year before index hospitalization. The AUDIT-C is a brief 3-item screening questionnaire that was validated against in-depth interviews for identifying past-year hazardous drinking and/or DSM-IV alcohol use disorders (AUD; Bradley et al, 2003, 2007; Bush et al., 1998). The AUDIT-C is scored 0–12 points with scores of 0 indicating no past-year alcohol use and increasing scores associated with increasing consumption and probability of AUD (Rubinsky et al., 2013). Patients were assigned to one of four AUDIT-C score categories: nondrinking (0 points), low-risk drinking (1–2 women, 1–3 men), moderate-risk drinking (3–7 women, 4–7 men), and high-risk drinking (8–12). Categories were chosen to reflect gender-specific differences in positive screens for alcohol misuse (≥3 points for women, ≥4 for men; Bradley et al., 2003, 2007) and increased risk associated with scores ≥8 points of hospitalizations for trauma (Williams et al, 2012) and gastrointestinal conditions (Au et al, 2007). Nondrinkers have been consistently shown to have poorer health outcomes relative to low-risk drinkers, including increased risk of trauma (Williams et al., 2012), gastrointestinal conditions (Au et al., 2007), post-operative complications (Bradley et al, 2011b), and mortality (Kinder et al., 2009).
2.4. Covariates
Patient demographic and clinical characteristics that have known associations with alcohol use and acute care utilization were selected as potential covariates. Demographic covariates included age at time of index hospitalization, gender, and race (white/nonwhite). Patients for whom race was unknown/missing were categorized as nonwhite, given that patients missing race/ethnicity in administrative data more often report nonwhite race (Kressin et al., 2003). Measures of prior health care utilization included the number of past-year hospitalizations, number of past-year ED visits, index length of stay, and an indicator for any past-year discharge against medical advice. Year of discharge was included as a covariate to account for potential time trends (2009–2011). Binary indicators of common health conditions from a previously validated comorbidity index (Gagne et al, 2011) were constructed for each patient from inpatient or outpatient diagnoses during the index stay and year prior (listed in Supplementary material 22). The overall comorbidity index score was also calculated to describe the level of comorbidity in the sample. Additional binary indicators for diagnoses of past-year tobacco use disorder and post-traumatic stress disorder (PTSD) were also used. Elapsed time from AUDIT-C screen to the initial hospitalization (0-3, 3-6, 6-12 months) was included to account for potential changes in alcohol use over time. VA copayment status due to disability or low income (copayment exempt vs. copayment required) was used as a proxy for socioeconomic status (SES) and lower health status (Kazis et al., 1998). VA patients are typically exempt from copayments (i.e., receive free VA care) if they have disabilities related to their military service (over 50% of disability is due to military service), or if their incomes are below a minimum threshold. Marital status (married, unmarried, unknown/missing) was used as an indicator of social support.
2.5. Analyses
Analyses were conducted in the total sample and separately for patients with either a medical or surgical index stay, due to known differences in medical and surgical inpatients (Jencks et al, 2009; Rosen et al., 2014). Descriptive analyses summarized patient characteristics, comorbidities, and the most common conditions responsible for index hospitalizations and readmissions across alcohol risk groups. Three models were planned a priori. The primary multivariable logistic regression model adjusted for age, gender, race, tobacco use disorder, PTSD diagnosis, time from AUDIT-C screen to hospitalization, comorbid conditions, number of prior year hospitalizations (or ED visits), index length of stay, any prior year discharge against medical advice, and year of discharge. These covariates were selected a priori for the primary model because they represent types of clinical and demographic characteristics that are often included in 30-day readmission models (Kansagara et al., 2011) and are available in or could be readily generated from administrative data sources. Fixed effects for the VA facility where each patient was screened (n =130) were included to account for unobserved facility-level characteristics that may influence both patients' AUDIT-C scores and health care utilization. In secondary analyses, the primary multivariable logistic regression model was additionally adjusted for marital status and VA copayment exempt status, indicators of social support and SES, respectively. These covariates were not included in the primary analysis because they are thought to characterize the patient's post-discharge environment (Arbaje et al., 2008) and reflect social risk factors often omitted from analyses of 30-day readmissions (Calvillo-King et al., 2013). Finally, analyses that adjusted for age, gender, race, and year of discharge were conducted for comparison with primary and secondary analyses, and in order to account for basic demographic characteristics available to clinicians and thought to have clinical relevance. The method of recycled predictions was used to estimate the average adjusted probability of readmissions and ED visits, for each alcohol risk group (Kleinman and Norton, 2009). Post-estimation Wald tests evaluated differences in outcomes for alcohol risk groups relative to low-risk drinkers. Low-risk drinkers were selected a priori as the referent group rather than nondrinkers because nondrinkers are known to have poorer health outcomes, as above.
3. Results
Among 579,330 patients included in the study sample, most patients reported nondrinking (61.6%), based on AUDIT-C screening results, and smaller proportions reported low-risk drinking (27.1%), moderate-risk drinking (10.0%), or high-risk drinking (1.2%). Overall, the mean age was 77 (SD = 7.4) and most patients were white, male, married, and exempt from VA copayments. Table 1 shows descriptive analyses comparing patient demographic and clinical characteristics in the four alcohol risk groups. Additional clinical characteristics, including for medical or surgical subgroups, are outlined in Supplementary material 2–33.
Table 1.
Demographic and clinical characteristics of study sample, by alcohol risk group.
| Nondrinker n=357,086 | Low-risk drinking n=156,928 | Moderate-risk drinking n = 58,149 | High-risk drinking n=7167 | Total n=579,330 | |
|---|---|---|---|---|---|
| Age, mean (SD) | 77.4 (7.4) | 76.6 (7.3) | 76.6 (7.3) | 71.1 (6.0) | 77.0 (7.4) |
| Male, n (%) | 350,171(98.1%) | 154,903(98.7%) | 57,324(98.6%) | 7149(99.7%) | 569,547(98.3%) |
| Race, n (%) | |||||
| White | 300,743(84.2%) | 139,499(88.9%) | 53,628(92.2%) | 6011(83.9%) | 499,881(86.3%) |
| Nonwhite | 56,343(15.8%) | 17,429(11.1%) | 4521(7.8%) | 1156(16.1%) | 79,449(13.7%) |
| Marital status, n (%) | |||||
| Unmarried | 122,557(34.3%) | 50,326(32.1%) | 19,259(33.1%) | 3944(55.0%) | 196,086(33.8%) |
| Married | 233,301(65.3%) | 106,084(67.6%) | 38,642(66.5%) | 3202(44.7%) | 381,229(65.8%) |
| Missing/unknown | 1228(0.3%) | 518(0.3%) | 248(0.4%) | 21(0.3%) | 2015(0.3%) |
| Copay exempt status, n (%) | |||||
| Copay required | 99,657(27.9%) | 62,095(39.6%) | 25,087(43.1%) | 1679(23.4%) | 188,518(32.5%) |
| Copay exempt | 255,174(71.5%) | 93,883(59.8%) | 32,728(56.3%) | 5444(76.0%) | 387,229(66.8%) |
| Missing/unknown | 2255(0.6%) | 950(0.6%) | 334(0.6%) | 44(0.6%) | 3583(0.6%) |
| Tobacco, n (%) | 47,292(13.2%) | 22,620(14.4%) | 10,888(18.7%) | 3218(44.9%) | 84,018(14.5%) |
| PTSD, n (%) | 19,842(5.6%) | 7053(4.5%) | 2207(3.8%) | 681(9.5%) | 29,783(5.1%) |
| AUD, n (%) | 10,245(2.9%) | 7422(4.7%) | 9314(16.0%) | 4412(61.6%) | 31,393(5.4%) |
| Comorbidity index, mean (SD)a | 3.7 (3.0) | 3.2 (2.9) | 3.1 (2.8) | 3.3 (2.7) | 3.5 (2.9) |
| Past-yr hospitalizations, mean (SD) | 0.5 (1.0) | 0.3 (0.8) | 0.3 (0.8) | 0.5 (1.1) | 0.4 (0.9) |
| Past-yr ED visits, mean (SD) | 1.2 (2.0) | 0.8 (1.6) | 0.8 (1.5) | 1.3 (2.4) | 1.0 (1.9) |
| Index length of Stay, mean (SD) | 4.0 (3.6) | 3.7 (3.3) | 3.7 (3.4) | 4.4 (4.1) | 3.9 (3.5) |
| Any AMA, n (%) | 2145(0.6%) | 755(0.5%) | 301(0.5%) | 150(2.1%) | 3351(0.6%) |
Note: Differences across the four AUDIT-C groups were statistically significant for all characteristics in this table (p< 0.001), based on Chi-square tests for categorical variables and analysis of variance for continuous variables.
Prevalence of specific comorbid conditions included in primary analyses available in Appendix 2.
In primary analyses for the total sample, high-risk drinkers had significantly increased risk for 30-day readmission (1%), relative to low-risk drinkers (p<0.05; Table 2). This association was attenuated from that in analyses adjusted only for demographics. However, for high-risk drinkers relative to low-risk drinkers, the difference was no longer significant after adjusting for indicators of social support (marital status) and SES (VA copay-exempt). Among patients whose index hospitalization was for a medical condition, high-risk drinking was associated with a significantly higher risk for readmissions (1%), relative to low-risk drinking patients (p <0.05). These associations were no longer significant for high-risk drinkers in secondary analyses. There were no significant differences in readmission rates for surgical patients with high-risk drinking relative to low-risk drinking. In addition, high-risk drinkers did not have significantly higher rates of ED visits relative to low-risk drinkers in primary or secondary analyses, in the total sample or the subset of patients hospitalized for medical or surgical conditions (Table 3).
Table 2.
Probability of post-discharge 30-day hospital readmissions, across AUDIT-C Risk Groups.
| Nondrinking | Low-risk drinking | Moderate-risk drinking | High-risk drinking | |
|---|---|---|---|---|
|
|
||||
| % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | |
| N = 357,086 | N= 156,928 | N = 58,149 | N=7167 | |
| Total 30-day hospital readmissions | ||||
| Unadjusted | 14.7 (14.6–14.9%)*** | 12.1 (11.9–12.2%) | 12.0 (11.7–12.3%) | 14.5 (13.7–15.3%)*** |
| Adjusted for demographicsa | 14.6 (14.5–14.7%)*** | 12.2 (12.0–12.3%) | 12.2 (11.9–12.5%) | 15.4 (14.5–16.3%)*** |
| Primary modelb | 14.2 (14.1–14.3%)*** | 12.9 (12.7–13.0%) | 12.9 (12.6–13.1%) | 13.8 (13.0–14.6%)* |
| Secondary modelc | 14.2 (14.0–14.3%)*** | 12.9 (12.8–13.1%) | 13.0 (12.8–13.3%) | 13.7 (12.9–14.5%) |
| N= 267,746 | N= 105,023 | N = 37,981 | N=5300 | |
| 30-day readmissions after index hospitalization for a medical condition | ||||
| Unadjusted | 16.0 (15.8–16.1%)*** | 13.6 (13.4–13.8%) | 13.7 (13.4–14.1%) | 16.2 (15.2–17.2%)*** |
| Adjusted for demographicsa | 15.9(15.8–16.0%)*** | 13.6 (13.4–13.9%) | 13.8 (13.5–14.2%) | 16.8 (15.8–17.8%)*** |
| Primary modelb | 15.6 (15.5–15.7%)*** | 14.3 (14.0–14.5%) | 14.4 (14.0–14.7%) | 15.3 (14.4–16.3%)* |
| Secondary modelc | 15.5 (15.4–15.7%)*** | 14.3 (14.1–14.6%) | 14.6 (14.2–14.9%) | 15.3 (14.3–16.3%) |
| N= 89,340 | N = 51,905 | N = 20,168 | N= 1867 | |
| 30-day readmissions after index hospitalization for a surgical condition | ||||
| Unadjusted | 11.1 (10.9–11.3%)*** | 9.0 (8.7–9.2%) | 8.8 (8.4–9.2%) | 9.6 (8.3–11.0%) |
| Adjusted for demographicsa | 10.9(10.7–11.2%)*** | 9.1 (8.8–9.3%) | 8.9 (8.5–9.3%) | 10.4 (9.0–11.9%) |
| Primary modelb | 10.5 (10.3–10.7%)*** | 9.6 (9.3–9.9%) | 9.6 (9.2–10.1%) | 9.6 (8.3–11.0%) |
| Secondary modelc | 10.4 (10.2–10.6%)*** | 9.7 (9.4–9.9%) | 9.7 (9.3–10.2%) | 9.6 (8.2–10.9%) |
Adjusted for age, gender, race, year of discharge.
Adjusted for age, gender, race, year of discharge, past-year tobacco diagnosis, past-year PTSD diagnosis, comorbid condition indicators, days from AUDIT-C screen to index stay, index length of stay, number of past-year hospitalizations, any past-year discharge AMA.
Adjusted for age, gender, race, year of discharge, past-year tobacco diagnosis, past-year PTSD diagnosis, comorbid condition indicators, days from AUDIT-C screen to index stay, index length of stay, number of past-year hospitalizations, any past-year discharge AMA, VA copay exempt status, marital status.
p<0.001.
p<0.01.
p<0.05 compared low-risk drinking (referent group).
Table 3.
Probability of post-discharge 30-day treat and release ED visits, across AUDIT-C Risk Groups.
| Nondrinking | Low-risk drinking | Moderate-risk drinking | High-risk drinking | |
|---|---|---|---|---|
|
|
||||
| % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | |
| N=357,086 | N= 156,928 | N = 58,149 | N=7167 | |
| 30-day ED treat and release visits | ||||
| Unadjusted | 12.9 (12.8–13.0%)*** | 10.7 (10.5–10.8%) | 10.4 (10.1–10.6%)* | 12.7 (11.9–13.5%)*** |
| Adjusted for demographicsa | 12.8(12.7–12.9%)*** | 10.9 (10.7–11.0%) | 10.5 (10.3–10.8%)* | 12.5 (11.8–13.3%)*** |
| Primary modelb | 12.4 (12.3–12.5%)*** | 11.4 (11.3–11.6%) | 11.2 (10.9–11.4%) | 11.1 (10.4–11.8%) |
| Secondary modelc | 12.3 (12.2–12.5%)*** | 11.5 (11.4–11.7%) | 11.4 (11.1–11.6%) | 11.1 (10.4–11.8%) |
| N= 267,746 | N= 105,023 | N = 37,981 | N = 5300 | |
| 30-day ED visits after index hospitalization for a medical condition | ||||
| Unadjusted | 13.2 (13.1–13.4%)*** | 11.1 (10.9–11.3%) | 10.9 (10.6–11.2%) | 13.8 (12.8–14.7%)*** |
| Adjusted for demographicsa | 13.2 (13.0–13.3%)*** | 11.2 (11.0–11.4%) | 11.0 (10.7–11.3%) | 13.3 (12.4–14.2%)*** |
| Primary modelb | 12.9 (12.7–13.0%)*** | 11.8 (11.6–12.0%) | 11.7 (11.3–12.0%) | 11.9 (11.1–12.8%) |
| Secondary modelc | 12.8 (12.7–12.9%)*** | 11.9 (11.7–12.1%) | 11.8 (11.5–12.2%) | 11.9 (11.0–12.7%) |
| N= 89,340 | N = 51,905 | N = 20,168 | N= 1867 | |
| 30-day ED visits after index hospitalization for a surgical condition | ||||
| Unadjusted | 11.7 (11.5–12.0%)*** | 9.9 (9.7–10.2%) | 9.4 (9.0–9.8%)* | 9.7 (8.4–11.1%) |
| Adjusted for demographicsa | 11.6(11.4–11.9%)*** | 10.0 (9.8–10.3%) | 9.5 (9.1–9.9%)* | 9.8 (8.5–11.2%) |
| Primary modelb | 11.3 (11.1–11.5%)*** | 10.5 (10.2–10.7%) | 10.1 (9.6–10.5%) | 9.0 (7.7–10.3%)* |
| Secondary modelc | 11.2 (11.0–11.4%)*** | 10.5 (10.3–10.8%) | 10.2 (9.7–10.6%) | 9.0 (7.7–10.2%)* |
Adjusted for age, gender, race, year of discharge.
Adjusted for age, gender, race, year of discharge, past-year tobacco diagnosis, past-year PTSD diagnosis, comorbid condition indicators, days from AUDIT-C screen to index stay, index length of stay, number of past-year ED visits, any past-year discharge AMA.
Adjusted for age, gender, race, year of discharge, past-year tobacco diagnosis, past-year PTSD diagnosis, comorbid condition indicators, days from AUDIT-C screen to index stay, index length of stay, number of past-year ED visits, any past-year discharge AMA, VA copay exempt status, marital status.
p< 0.001.
p<0.01.
p<0.05 compared to low-risk drinkers (referent group).
Similar to high-risk drinking patients, nondrinkers in the total sample had significantly increased risk for readmission (1%), relative to low-risk drinking patients (p<0.001). Among patients hospitalized for a medical condition, nondrinkers also had significantly higher risk for readmission (1%), relative to low-risk drinking patients (p<0.001; Table 2). Among patients hospitalized for a surgical condition, nondrinkers had higher readmission rates relative to low-risk drinkers in all analytic models. Nondrinkers had significantly greater risk for 30-day ED visits (1%), relative to low-risk drinkers, in primary analyses for the total sample (p<0.001; Table 3). Among patients hospitalized for surgical conditions, only nondrinkers had significantly higher rates of 30-day ED visits compared to low-risk drinkers in primary analyses (1%; p<0.001).
Reasons for index hospitalization and readmission differed markedly by alcohol risk group and by whether the index hospitalization was for a medical or surgical condition (Supplementary material 4–94). Overall, the most common reason for index hospitalizations was pneumonia, followed by coronary atherosclerosis and cardiac dysrhythmias (Supplementary material 45). The most common reason for both the index hospitalization and readmission among high-risk drinkers was alcohol-related disorders, followed by chronic obstructive pulmonary disease (COPD), while among all other groups the most common condition at readmission was CHF (Supplementary material 4 and 76).
4. Discussion
This study is the first to evaluate the association of unhealthy alcohol use and 30-day hospital readmissions or ED visits in older adults. In this large sample of older adults hospitalized for a medical or surgical condition, patients with routine alcohol screening results indicating high-risk drinking had approximately 1% greater risk of readmissions relative to low-risk drinkers, and this was not explained by demographics, comorbidities, or prior health care utilization. The increased risk of readmission associated with unhealthy alcohol use was restricted to the subgroup of patients admitted initially for a medical condition. However, in secondary analyses additionally adjusted for indicators of SES and social support, there was no longer a significant association. This suggests that the increased risk for readmissions among those with high-risk drinking may reflect differences in SES and social support, rather than the acute adverse consequences of high-risk drinking.
Few studies have examined the association between unhealthy alcohol use and readmissions (Kartha et al., 2007; Rubinsky et al., 2012; Walley et al., 2012; Wei et al., 2014). One study examined diagnoses for AUD during index hospitalization as a risk factor for 30-day readmissions, but found a significant association with increased readmissions only among patients with comorbid AUD and substance use disorders (Walley et al, 2012). A hospital quality improvement implementation study reported that inpatients with alcohol-related diagnoses had higher rates of 30-day readmissions than those without (Wei et al., 2014). However, alcohol-related diagnoses under-identify in patients with AUD (Smothers et al, 2004) and as a result, may not adequately characterize alcohol use in inpatients. Two studies examined alcohol use based on the AUDIT-C (Rubinsky et al, 2012) or 10-item AUDIT (Kartha et al, 2007) and risk for readmissions. The first found no significant association between screening scores and readmissions among surgical inpatients (Rubinsky et al., 2012), while the second found no association among general medical inpatients (Kartha et al, 2007). However, neither focused on older adults, assessed 30-day ED visits, or utilized screening results documented in routine care.
This study extends the literature by examining unhealthy alcohol use, as measured by routine outpatient screening, as a potentially modifiable risk factor for 30-day readmissions and ED visits among a large sample of older VA patients. In the present study, almost two-thirds of patients with high-risk drinking had a past-year diagnosis of AUD. In addition, 10% of high-risk drinking patients who were readmitted were hospitalized for alcohol-related conditions during the readmission stay. However, patients with high-risk drinking were a small proportion of hospitalized patients (1%) and in analyses that adjusted for indicators of SES and social support, high-risk drinking was no longer associated with readmission risk. Nevertheless, health systems may be interested in intervening and delivering post-discharge interventions to high-risk drinking patients who may be more likely to return for reasons due to alcohol use. Patients with AUD could be offered evidence-based alcohol interventions (Bradley and Kivlahan, 2014; Jonas et al., 2014). However, because the elevated risk for readmissions among high-risk drinking patients could be explained by other factors (marital status, lower SES), interventions may need to focus on factors other than alcohol use (e.g., in home support and care coordination).
The lack of a significant association between high-risk drinking and readmissions for surgical patients is consistent with one prior study (Rubinsky et al., 2012). Differences in the patient characteristics between medical and surgical inpatients, as well as conditions treated, could explain why associations between high-risk drinking and readmissions were observed only among medical inpatients. Surgical inpatients in our sample and elsewhere were generally younger, had fewer comorbid conditions (including AUD and other mental health conditions; Rosen et al., 2014), and lower readmission rates than medical inpatients (Jencks et al., 2009; Rosen et al., 2014). In the present study, the most common reasons for readmissions among surgical inpatients were complications of care. However, reasons for readmissions among medical inpatients were varied and included conditions that may be more influenced by post-discharge health behaviors (CHF, COPD). Unhealthy alcohol use is associated with poorer adherence to medications (Braithwaite et al., 2005; Bryson et al., 2008) and poorer self-care (Thomas et al., 2012), and may play a greater role in influencing readmission risk for medical inpatients.
As expected based on previous research, patients reporting no alcohol use in the past year were at increased risk for 30-day readmissions and ED visits compared to patients with low-risk drinking. Prior studies have shown patients who report no alcohol use have lower health status (Green and Polen, 2001) and greater all-cause mortality (Bridevaux et al., 2004; Kinder et al., 2009) than current drinkers. Nondrinking based on alcohol screening scores may serve as a marker for poorer health status and greater health care need. Patients who report current nondrinking may have reduced drinking due to prior problems due to drinking or may abstain from alcohol due to health conditions (Green and Polen, 2001; Stranges et al., 2006). In the present study, analyses adjusted for comorbidities and prior utilization, it is likely that residual confounding influenced findings regarding nondrinkers. Nevertheless, patient-reported nondrinking was common among older adults in this study (62%). Given that this group of patients was the largest subgroup of older adults, and that routine alcohol screening conducted prior to admission identified their heightened risk for 30-day readmission, health care providers may want to be aware of nondrinkers' vulnerability for poor outcomes following hospital discharge. Select patients might benefit from additional post-discharge support.
This study has several limitations. First, although analyses included numerous covariates typical of readmission studies, these measures are unlikely to capture all differences correlated with both alcohol use and study outcomes, such as mental health conditions. Second, routinely administered AUDIT-C screens may under-identify patients with unhealthy alcohol use. Approximately 61% of VA patients who screened positive for alcohol misuse on a confidential, mailed survey were not identified during a recent outpatient visit (Bradley et al., 2011a). Therefore, some patients categorized as nondrinkers or low-risk drinkers may have been misclassified and differences in outcomes for alcohol risk groups relative to low-risk drinkers may be attenuated. Third, patients were excluded from the study sample if they did not have an AUDIT-C score in the year prior to hospitalization. Relative to the study sample, VA patients missing AUDIT-C scores had a lower prevalence of some conditions, such as chronic pulmonary disease, psychosis, AUD, and tobacco use disorders (Supplementary material 107), consistent with previous studies of VA care (Liu et al., 2011; Petersen et al., 2010). Thus, AUDIT-C scores do not appear to be missing at random and we do not know whether similar associations would be observed between alcohol risk groups and study outcomes had AUDIT-C scores been available for excluded patients. Study findings may be most generalizable to populations with greater burden of comorbidity. Given that women made up only a small minority of the study sample (2%), results may not be generalizable to women. Future research is needed to understand the association between alcohol screening results and risk for post-discharge readmissions or ED visits among women.
The present study suggests that hospitalized patients who are nondrinkers and those who screen positive for high-risk drinking prior to hospitalization are at greater risk for 30-day readmissions relative to those with low-risk drinking, after adjusting for demographic characteristics, comorbidities, and prior utilization. However, the modest association between high-risk drinking and increased risk of readmissions was restricted to medical patients and appeared to reflect lower social support and SES among those patients. These results suggest that indicators social risk such as marital status and socioeconomic status – when available in health system data – may be of greater utility than alcohol screening results for identifying patients in need of post-discharge support following hospital discharge. Both patients with high-risk drinking and nondrinkers might benefit from such support.
Supplementary Material
Highlights.
Evaluated the association of unhealthy drinking with 30-day readmissions.
Unhealthy drinking identified through routine outpatient alcohol screening.
High-risk drinking associated with 1% greater absolute risk for 30-day readmissions.
Other social risk factors appeared to account for this elevated risk.
Acknowledgments
Role of funding source: Ms. Chavez's work on this study was supported by anAgency for Healthcare Research and Quality (AHRQ) Dissertation Grant (NIH 1R36HS022800-01). Dr. Bradley's and Ms. Rubinsky's time on this study was supported by the Center of Excellence for Substance Abuse Treatment and Education (CESATE) at VA Puget Sound. Dr. Bradley's NIAAA R21 (5R21AA020894-02) supported the collection of the data used in this study. Dr. Clark is supported by NIH grant K23 AA 021814.
Footnotes
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:10.1016/j.drugalcdep.2015.11.008.
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:10.1016/j.drugalcdep.2015.11.008.
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:10.1016/j.drugalcdep.2015.11.008.
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:10.1016/j.drugalcdep.2015.11.008.
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:10.1016/j.drugalcdep.2015.11.008.
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:10.1016/j.drugalcdep.2015.11.008.
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:10.1016/j.drugalcdep.2015.11.008.
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:10.1016/j.drugalcdep.2015.11.008.
Author disclosures: Disclaimer: Views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs, the United States Government, or any of the authors' institutions.
Contributors: Ms. Chavez led the study design, conducted analyses, and drafted the manuscript. All co-authors gave input on statistical analyses, interpretation of results, and contributed to and approved the final manuscript.
Conflict of interest statement: No conflicts of interest.
Appendix A. Supplementary data: Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.drugalcdep.2015.11.008.
Contributor Information
Laura J. Chavez, Email: ljchavez@uw.edu, ljchavez@u.washington.edu.
Chuan-Fen Liu, Email: chuan-fen.liu@va.gov.
Nathan Tefft, Email: ntefft@bates.edu.
Paul L Hebert, Email: paul.hebert2@va.gov.
Brendan J. Clark, Email: brendan.clark@ucdenver.edu.
Anna D. Rubinsky, Email: anna.rubinsky@va.gov.
Gwen T. Lapham, Email: lapham.g@ghc.org.
Katharine A. Bradley, Email: bradley.k@ghc.org.
References
- Ajmera M, Wilkins TL, Sambamoorthi U. Dual Medicare and Veteran Health Administration use and ambulatory care sensitive hospitalizations. J Gen Intern Med. 2011;26(Suppl. 2):669–675. doi: 10.1007/s11606-011-1788-4. http://dx.doi.org/10.1007/s11606-011-1788-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amarasingham R, Moore BJ, Tabak YP, Drazner MH, Clark CA, Zhang S, Reed WG, Swanson TS, Ma Y, Halm EA. An automated model to identify heart failure patients at risk for 30-day readmission or death using electronic medical record data. Med Care. 2010;48:981–988. doi: 10.1097/MLR.0b013e3181ef60d9. http://dx.doi.org/10.1097/MLR.0b013e3181ef60d9. [DOI] [PubMed] [Google Scholar]
- Arbaje AI, Wolff JL, Yu Q, Powe NR, Anderson GF, Boult C. Postdischarge environmental and socioeconomic factors and the likelihood of early hospital readmission among community-dwelling Medicare beneficiaries. Gerontologist. 2008;48:495–504. doi: 10.1093/geront/48.4.495. [DOI] [PubMed] [Google Scholar]
- Au DH, Kivlahan DR, Bryson CL, Blough D, Bradley KA. Alcohol screening scores and risk of hospitalizations for GI conditions in men. Alcohol Clin Exp Res. 2007;31:443–451. doi: 10.1111/j.1530-0277.2006.00325.x. http://dx.doi.org/10.1111/j.1530-0277.2006.00325.x. [DOI] [PubMed] [Google Scholar]
- Baier RR, Gardner RL, Coleman EA, Jencks SF, Mor V, Gravenstein S. Shifting the dialogue from hospital readmissions to unplanned care. Am J Manag Care. 2013;19:450–453. [PubMed] [Google Scholar]
- Blunt I, Bardsley M, Grove A, Clarke A. Classifying emergency 30-day readmissions in England using routine hospital data 2004-2010: what is the scope for reduction? Emerg Med J. 2015;32(1):44–50. doi: 10.1136/emermed-2013-202531. http://dx.doi.org/10.1136/emermed-2013-202531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley K, Kivlahan D. Medications for alcohol use disorder—reply. JAMA. 2014;312:1352. doi: 10.1001/jama.2014.10167. http://dx.doi.org/10.1001/jama.2014.10167. [DOI] [PubMed] [Google Scholar]
- Bradley KA, Bush KR, Epler AJ, Dobie DJ, Davis TM, Sporleder JL, Maynard C, Burman ML, Kivlahan DR. Two brief alcohol-screening tests From the Alcohol Use Disorders Identification Test (AUDIT): validation in a female Veterans Affairs patient population. Arch Intern Med. 2003;163:821–829. doi: 10.1001/archinte.163.7.821. http://dx.doi.org/10.1001/archinte.163.7.821. [DOI] [PubMed] [Google Scholar]
- Bradley KA, DeBenedetti AF, Volk RJ, Williams EC, Frank D, Kivlahan DR. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol Clin Exp Res. 2007;31:1208–1217. doi: 10.1111/j.1530-0277.2007.00403.x. http://dx.doi.org/10.1111/j.1530-0277.2007.00403.x. [DOI] [PubMed] [Google Scholar]
- Bradley KA, Lapham GT, Hawkins EJ, Achtmeyer CE, Williams EC, Thomas RM, Kivlahan DR. Quality concerns with routine alcohol screening in VA clinical settings. J Gen Intern Med. 2011a;26:299–306. doi: 10.1007/s11606-010-1509-4. http://dx.doi.org/10.1007/s11606-010-1509-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley KA, Rubinsky AD, Sun H, Bryson CL, Bishop MJ, Blough DK, Henderson WG, Maynard C, Hawn MT, Tonnesen H, Hughes G, Beste LA, Harris AH, Hawkins EJ, Houston TK, Kivlahan DR. Alcohol screening and risk of postoperative complications in male VA patients undergoing major non-cardiac surgery. J Gen Intern Med. 2011b;26:162–169. doi: 10.1007/s11606-010-1475-x. http://dx.doi.org/10.1007/s11606-010-1475-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley KA, Williams EC, Achtmeyer CE, Volpp B, Collins BJ, Kivlahan DR. Implementation of evidence-based alcohol screening in the Veterans Health Administration. Am J Manag Care. 2006;12:597–606. [PubMed] [Google Scholar]
- Braithwaite RS, McGinnis KA, Conigliaro J, Maisto SA, Crystal S, Day N, Cook RL, Gordon A, Bridges MW, Seiler JF, Justice AC. A temporal and dose-response association between alcohol consumption and medication adherence among veterans in care. Alcohol Clin Exp Res. 2005;29:1190–1197. doi: 10.1097/01.alc.0000171937.87731.28. [DOI] [PubMed] [Google Scholar]
- Bridevaux IP, Bradley KA, Bryson CL, McDonell MB, Fihn SD. Alcohol screening results in elderly male veterans: association with health status and mortality. J Am Geriat Soc. 2004;52:1510–1517. doi: 10.1111/j.1532-5415.2004.52414.x. http://dx.doi.org/10.1111/j.1532-5415.2004.52414.x. [DOI] [PubMed] [Google Scholar]
- Brock J, Mitchell J, Irby K, Stevens B, Archibald T, Goroski A, Lynn J. Association between quality improvement for care transitions in communities and rehospitalizations among Medicare beneficiaries. JAMA. 2013;309:381–391. doi: 10.1001/jama.2012.216607. http://dx.doi.org/10.1001/jama.2012.216607. [DOI] [PubMed] [Google Scholar]
- Bryson CL, Au DH, Sun H, Williams EC, Kivlahan DR, Bradley KA. Alcohol screening scores and medication nonadherence. Ann Intern Med. 2008;149:795–804. doi: 10.7326/0003-4819-149-11-200812020-00004. [DOI] [PubMed] [Google Scholar]
- Burman ML, Kivlahan D, Buchbinder M, Broglio K, Zhou XH, Merrill JO, McDonell MB, Fihn SD, Bradley KA, Bradley KA Ambulatory Care Quality Improvement Project Investigators. Alcohol-related advice for Veterans Affairs primary care patients: who gets it? Who gives it? J Stud Alcohol. 2004;65:621–630. doi: 10.15288/jsa.2004.65.621. [DOI] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 1998;158:1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- Calvillo-King L, Arnold D, Eubank KJ, Lo M, Yunyongying P, Stieglitz H, Halm EA. Impact of social factors on risk of readmission or mortality in pneumonia and heart failure: systematic review. J Gen Intern Med. 2013;28:269–282. doi: 10.1007/s11606-012-2235-x. http://dx.doi.org/10.1007/s11606-012-2235-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services. Readmissions Reduction Program. 2014 Retrieved from ( http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.htmL.
- Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166:1822–1828. doi: 10.1001/archinte.166.17.1822. http://dx.doi.org/10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- Duru OK, Xu H, Tseng CH, Mirkin M, Ang A, Tallen L, Moore AA, Ettner SL. Correlates of alcohol-related discussions between older adults and their physicians. J Am Geriatr Soc. 2010;58:2369–2374. doi: 10.1111/j.1532-5415.2010.03176.x. http://dx.doi.org/10.1111/j.1532-5415.2010.03176.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gagne JJ, Glynn RJ, Avorn J, Levin R, Schneeweiss S. A combined comorbidity score predicted mortality in elderly patients better than existing scores. J Clin Epidemiol. 2011;64:749–759. doi: 10.1016/j.jclinepi.2010.10.004. http://dx.doi.org/10.1016/jjclinepi.2010.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerhardt G, Yemane A, Apostle K, Oelschlaeger A, Rollins E, Brennan N. Evaluating whether changes in utilization of hospital outpatient services contributed to lower Medicare readmission rate. Medicare Medicaid Res Rev. 2014;4 doi: 10.5600/mmrr2014-004-01-b03. http://dx.doi.org/10.5600/mmrr2014-004-01-b03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green CA, Polen MR. The health and health behaviors of people who do not drink alcohol. Am J Prev Med. 2001;21:298–305. doi: 10.1016/s0749-3797(01)00365-8. [DOI] [PubMed] [Google Scholar]
- Horwitz L, Grady JN, Lin Z, Nwosu C, Keenan M, Bhat KR, et al. 2013 Measure Updates and Specifications Report: Hospital-Wide All-Cause Unplanned Readmission Measure (Version 2.0) 2013 Retrieved from ( http://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier4&cid=1219069855841)
- Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. http://dx.doi.org/10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- Jonas DE, Amick HR, Feltner C, Bobashev G, Thomas K, Wines R, Kim MM, Shanahan E, Gass CE, Rowe CJ, Garbutt JC. Pharmacotherapy for adults with alcohol use disorders in outpatient settings: a systematic review and meta-analysis. JAMA. 2014;311:1889–1900. doi: 10.1001/jama.2014.3628. http://dx.doi.org/10.1001/jama.2014.3628. [DOI] [PubMed] [Google Scholar]
- Jonas DE, Garbutt JC, Amick HR, Brown JM, Brownley KA, Council CL, Viera AJ, Wilkins TM, Schwartz CJ, Richmond EM, Yeatts J, Evans TS, Wood SD, Harris RP. Behavioral counseling after screening for alcohol misuse in primary care: a systematic review and meta-analysis for the U.S. Preventive Services Task Force. Ann Intern Med. 2012 doi: 10.7326/0003-4819-157-9-201211060-00544. http://dx.doi.org/10.7326/0003-4819-157-9-201211060-00544. [DOI] [PubMed]
- Kansagara D, Englander H, Salanitro A, Kagen D, Theobald C, Freeman M, Kripalani S. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306:1688–1698. doi: 10.1001/jama.2011.1515. http://dx.doi.org/10.1001/jama.2011.1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kartha A, Anthony D, Manasseh CS, Greenwald JL, Chetty VK, Burgess JF, Culpepper L, Jack BW. Depression is a risk factor for rehospitalization in medical inpatients. Prim Care Companion J Clin Psychiatry. 2007;9:256–262. doi: 10.4088/pcc.v09n0401. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/17934548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazis LE, Miller DR, Clark J, Skinner K, Lee A, Rogers W, Spiro A, 3rd, Payne S, Fincke G, Selim A, Linzer M. Health-related quality of life in patients served by the Department of Veterans Affairs: results from the Veterans Health Study. Arch Intern Med. 1998;158:626–632. doi: 10.1001/archinte.158.6.626. [DOI] [PubMed] [Google Scholar]
- Kinder LS, Bryson CL, Sun H, Williams EC, Bradley KA. Alcohol screening scores and all-cause mortality in male Veterans Affairs patients. J Stud Alcohol Drugs. 2009;70:253–260. doi: 10.15288/jsad.2009.70.253. [DOI] [PubMed] [Google Scholar]
- Kirchner JE, Zubritsky C, Cody M, Coakley E, Chen H, Ware JH, Oslin DW, Sanchez HA, Durai UNB, Miles KM, Llorente MD, Costantino G, Levkoff S, Levkoff S. Alcohol consumption among older adults in primary care. J Gen Intern Med. 2007;22:92–97. doi: 10.1007/s11606-006-0017-z. http://dx.doi.org/10.1007/s11606-006-0017-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kizer KW, Dudley RA. Extreme makeover: transformation of the veterans health care system. Annu Rev Public Health. 2009;30:313–339. doi: 10.1146/annurev.publhealth.29.020907.090940. http://dx.doi.org/10.1146/annurev.publhealth.29.020907.090940. [DOI] [PubMed] [Google Scholar]
- Kleinman LC, Norton EC. What's the risk? A simple approach for estimating adjusted risk measures from nonlinear models including logistic regression. Health Serv Res. 2009;44:288–302. doi: 10.1111/j.1475-6773.2008.00900.x. http://dx.doi.org/10.1111/j.1475-6773.2008.00900.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kocher KE, Nallamothu BK, Birkmeyer JD, Dimick JB. Emergency department visits after surgery are common for Medicare patients, suggesting opportunities to improve care. Health Aff (Millwood) 2013;32:1600–1607. doi: 10.1377/hlthaff.2013.0067. http://dx.doi.org/10.1377/hlthaff.2013.0067. [DOI] [PubMed] [Google Scholar]
- Kressin NR, Chang BH, Hendricks A, Kazis LE. Agreement between administrative data and patients' self-reports of race/ethnicity. Am J Public Health. 2003;93:1734–1739. doi: 10.2105/ajph.93.10.1734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leppin AL, Gionfriddo MR, Kessler M, Brito JP, Mair FS, Gallacher K, Wang Z, Erwin PJ, Sylvester T, Boehmer K, Ting HH, Murad MH, Shippee ND, Montori VM. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174:1095–1107. doi: 10.1001/jamainternmed.2014.1608. http://dx.doi.org/10.1001/jamainternmed.2014.1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu CF, Manning WG, Burgess JF, Jr, Hebert PL, Bryson CL, Fortney J, Perkins M, Sharp ND, Maciejewski ML. Reliance on Veterans Affairs outpatient care by Medicare-eligible veterans. Med Care. 2011;49:911–917. doi: 10.1097/MLR.0b013e31822396c5. http://dx.doi.org/10.1097/MLR.0b013e31822396c5. [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. A Clinican's Guide, Updated 2005 Edition. NIAAA; Rockville, MD: 2005. Helping Patients Who Drink Too Much. [Google Scholar]
- Parker SG. Do current discharge arrangements from inpatient hospital care for the elderly reduce readmission rates, the length of inpatient stay or mortality, or improve health status? WHO; Geneva: 2005. Retrieved from ( http://www.euro.who.int/Document/E87542.pdf) [Google Scholar]
- Petersen LA, Byrne MM, Daw CN, Hasche J, Reis B, Pietz K. Relationship between clinical conditions and use of Veterans Affairs health care among Medicare-enrolled veterans. Health Serv Res. 2010;45:762–791. doi: 10.1111/j.1475-6773.2010.01107.x. http://dx.doi.org/10.1111/j.1475-6773.2010.01107.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen AK, Chen Q, Shin MH, O'Brien W, Shwartz M, Mull HJ, Cevasco M, Borzecki AM. Medical and surgical readmissions in the Veterans Health Administration: what proportion are related to the index hospitalization? Med Care. 2014;52:243–249. doi: 10.1097/MLR.0000000000000081. http://dx.doi.org/10.1097/MLR.0000000000000081. [DOI] [PubMed] [Google Scholar]
- Rubinsky AD, Dawson DA, Williams EC, Kivlahan DR, Bradley KA. AUDIT-C scores as a scaled marker of mean daily drinking, alcohol use disorder severity, and probability of alcohol dependence in a U.S. general population sample of drinkers. Alcohol Clin Exp Res. 2013;37:1380–1390. doi: 10.1111/acer.12092. http://dx.doi.org/10.1111/acer.12092. [DOI] [PubMed] [Google Scholar]
- Rubinsky AD, Sun H, Blough DK, Maynard C, Bryson CL, Harris AH, Hawkins EJ, Beste LA, Henderson WG, Hawn MT, Hughes G, Bishop MJ, Etzioni R, Tonnessen H, Kivlahan DR, Bradley KA. AUDIT-C alcohol screening results and postoperative inpatient health care use. J Am Coll Surg. 2011;214:296–305. doi: 10.1016/j.jamcollsurg.2011.11.007. http://dx.doi.org/10.1016/j.jamcollsurg.11.2012007(e291) [DOI] [PubMed] [Google Scholar]
- Selim AJ, Berlowitz D, Kazis LE, Rogers W, Wright SM, Qian SX, Rothendler JA, Sprio A, 3rd, Miller D, Selim BJ, Fincke BG. Comparison of health outcomes for male seniors in the Veterans Health Administration and Medicare Advantage plans. Health Serv Res. 2010;45:376–396. doi: 10.1111/j.1475-6773.2009.01068.x. http://dx.doi.org/10.1111/j.1475-6773.2009.01068.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smothers BA, Yahr HT, Ruhl CE. Detection of alcohol use disorders in general hospital admissions in the United States. Arch Intern Med. 2004;164:749–756. doi: 10.1001/archinte.164.7.749. http://dx.doi.org/10.1001/archinte.164.7.749. [DOI] [PubMed] [Google Scholar]
- Stranges S, Notaro J, Freudenheim JL, Calogero RM, Muti P, Farinaro E, Russell M, Nochajski TH, Trevisan M. Alcohol drinking pattern and subjective health in a population-based study. Addiction. 2006;101:1265–1276. doi: 10.1111/j.1360-0443.2006.01517.x. http://dx.doi.org/10.1111/j.1360-0443.2006.01517.x. [DOI] [PubMed] [Google Scholar]
- Thomas RM, Francis Gerstel PA, Williams EC, Sun H, Bryson CL, Au DH, Bradley KA. Association between alcohol screening scores and diabetic self-care behaviors. Fam Med. 2012;44:555–563. [PubMed] [Google Scholar]
- Voss R, Gardner R, Baier R, Butterfield K, Lehrman S, Gravenstein S. The care transitions intervention: translating from efficacy to effectiveness. Arch Intern Med. 2011;171:1232–1237. doi: 10.1001/archinternmed.2011.278. http://dx.doi.org/10.1001/archinternmed.2011.278. [DOI] [PubMed] [Google Scholar]
- Walley AY, Paasche-Orlow M, Lee EC, Forsythe S, Chetty VK, Mitchell S, Jack BW. Acute care hospital utilization among medical inpatients discharged with a substance use disorder diagnosis. J Addict Med. 2012;6:50–56. doi: 10.1097/ADM.0b013e318231de51. http://dx.doi.org/10.1097/ADM.0b013e318231de51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei J, Defries T, Lozada M, Young N, Huen W, Tulsky J. An inpatient treatment and discharge planning protocol for alcohol dependence: efficacy in reducing 30-day readmissions and emergency department visits. J Gen Intern Med. 2014 doi: 10.1007/s11606-014-2968-9. http://dx.doi.org/10.1007/s11606-014-2968-9. [DOI] [PMC free article] [PubMed]
- Wei J, Defries T, Lozada M, Young N, Huen W, Tulsky J. An inpatient treatment and discharge planning protocol for alcohol dependence: efficacy in reducing 30-day readmissions and emergency department visits. J Gen Intern Med. 2015;30:365–370. doi: 10.1007/s11606-014-2968-9. http://dx.doi.org/10.1007/s11606-014-2968-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams EC, Bryson CL, Sun H, Chew RB, Chew LD, Blough DK, Au DH, Bradley KA. Association between alcohol screening results and hospitalizations for trauma in Veterans Affairs outpatients. Am J Drug Alcohol Abuse. 2012;38:73–80. doi: 10.3109/00952990.2011.600392. http://dx.doi.org/10.3109/00952990.2011.600392. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


