Abstract
Substance users are at elevated risk for HIV. HIV researchers, particularly at the intersection of HIV and substance use, have requested new methods to better understand and address this important area. New technologies, such as social media and mobile applications, are increasingly being used as research tools in studies on HIV and substance use. These technologies have the potential to build on existing recruitment methods, provide new and improved intervention methods, and introduce novel ways of monitoring and predicting new HIV cases. However, little work has been done to review and broadly explore the types of studies being conducted on the use of technologies to address HIV and substance use. This systematic literature review identified studies on this topic between 2005-2015. We identified 33 studies on this topic after excluding studies that did not fit inclusion criteria. Studies were either observational (n = 24) or interventional (n = 9), with the majority being pilot studies exploring the feasibility of using these new technologies to study HIV and substance use. We discuss the implications of this work along with limitations and recommendations for future research on this topic.
Keywords: technologies, HIV, substance use, social media, mobile apps
Introduction
Substance use is strongly linked to HIV, making it an important area of concern for HIV researchers. The HIV Cost and Service Utilization Study (HSCUS) in the U.S. revealed that 40% of individuals living with HIV disclosed they used illegal drugs in the past year (Chander, Himelhoch, & Moore, 2012). Globally, it is believed that more than 3 million injection drug users are HIV positive (Mathers, Degenhardt, Phillips, Wiessing, Hickman, & Strathdee, et. al, 2008). Thirty-two percent (32%) of all frequent non-injection drug users and 40% of MSM who are injection drug users in the U.S. are HIV positive (Catania, Osmond, Stall, Pollack, Paul, Blower, et. al, 2001).
Two populations, both independent and overlapping, that are at high risk for HIV acquisition and transmission are men who have sex with men (MSM) and substance users. MSM are disproportionately at risk for contracting HIV (Hall, Song, Rhodes, Prejean, An, Lee, et. al, 2008). In particular, African American and Latino MSM are at increased risk for HIV. According to a CDC study focused on MSM, 28% of non-Latino Blacks and 18% of Latinos were infected compared to 16% of non-Latino White MSM (CDC, 2010). Taken together, it is important to address the increased risk for HIV among MSM, especially African Americans and Latinos.
Technology usage in the past decade has increased significantly among the general population as well as more specifically among groups with and at high risk for HIV. Currently, 52% of adults use two or more social media websites, whereas in 2013, only 42% of adults used a social media website (Duggan, Ellison, Lampe, Lenhart, & Madden, 2015). Substance users have adapted to new technologies such as the use of social media sites. In fact, it is common for substance users to publicly document their substance use on social media (Morgan, Snelson, & Elison-Bowers, 2010; Young, Rivers, and Lewis, 2014). In one study on college students, a reported 33% of participants had posted a picture on a social media site showing some type of substance use. In 2009, it was found that 85% of young adults’ MySpace accounts included one or more references to substance use (Morgan et al., 2010). A study examining over 550 million tweets found that people are also discussing their substance use in tweets, and that analyzing these trends and patterns of “social big data” can be used to monitor and predict HIV incidence (Young et al., 2014).
Technologies such as social media sites, online applications (“apps”) and text messaging can be used to both facilitate as well as prevent HIV transmission. For example, smartphone applications for social networking targeted toward MSM can facilitate the transmission of HIV because these sites facilitate MSM finding sexual partners online. Research on a popular smartphone application for MSM found that 62.1% of users reported utilizing the application to find one-on-one sex, 17.1% used the app to find group sex, and 46.1% reported having unprotected anal intercourse in the past 3 months (Landovitz, Tseng, Weissman, Haymer, Mendenhall, Rodgers, et. al, 2012). App users reported using a number of substances during sex, including marijuana (59.7%), amyl nitrite or inhalants (34.8%), MDMA (30.4%), cocaine (27.1%), and methamphetamine (14.4%) (Landovitz, Tseng, Weissman, Haymer, Mendenhall, Rodgers, et. al, 2012). Thus, technology use among certain high-risk populations, such as substance-using MSM, may serve as a vehicle to engage in HIV risk behaviors.
Studies have demonstrated that the use of technology can also serve to prevent HIV transmission. In a study conducted among homeless youth in Los Angeles, people who used online social networks appeared to have better understanding of HIV knowledge and risks (Young & Rice, 2010). Further, in the Harnessing Online Peer Education (HOPE) social media-based intervention, participants were more likely to request an HIV self-testing kit if they were a member of a HOPE intervention group (Young, Cumberland, Nianogo, Menacho, Galea, & Coates, 2014). Additional research has found that text messages can decrease HIV risk behaviors among substance-using MSM. Findings from one text-messaging intervention found that both HIV-positive and HIV-negative MSM without a primary partner had decreased unprotected sex and reported significantly less injected methamphetamine use at two month follow-up evaluations; as 20.8% reported injection methamphetamine use at baseline and 8.3% reported methamphetamine injection use at two month follow-up (Reback, et al, 2012).
Technologies therefore have tremendous potential to address HIV risk among substance users. There are distinct advantages for using technologies in HIV prevention studies. For example, technologies have the capacity to increase participant recruitment by reaching potential participants through online website advertisements, social media sites, smartphone apps, email, and text messages. Technology-based interventions can be tailored to individual characteristics, allowing for a personalized health intervention rather than targeting a large group (Seth, Hulda & Larson, 2009). Given that technology-based interventions can reach large audiences in cost-effective ways (Seth, Hulda & Larson, 2009), they could be used in reducing HIV transmission among populations at risk, including substance users. Because of the increasingly important role that technologies can play in reducing HIV sexual- and drug-related risk behaviors, HIV and substance abuse researchers are investigating the ways in which technologies can be used to reduce or prevent substance use, optimize and expand substance use treatment beyond traditional brick-and-mortar facilities, and reduce or prevent HIV acquisition and transmission. However, a number of concerns may arise during the course of such research. This paper provides an overview of recent and trending research on the use of technologies in HIV-related studies with substance users to help guide researchers’ future efforts.
Methods
Data Searches
We conducted a systematic database search on the U.S. National Library of Medicine's PudMed and PsycINFO. For database searches, combinations of the following search terms were used: substance use, stimulant use, methamphetamine, injection drug use, cocaine, substance abuse, opioid, HIV/AIDS, technology, social networking sites, social media, phones, smartphones, texts, Internet, websites, and web. Given the paucity of research on this topic within the past 3 years, we expanded the search to include studies published within the past 10 years.
Selection Criteria and Data Extraction
After the initial database search, authors reviewed the articles and selected all relevant studies. To understand current research at the intersection of substance use and HIV, and technology, we included studies that were 1) published in peer-reviewed academic journals within the past 10 years (2005-2015); and, 2) published in English. We included both observational studies (e.g., online survey) and intervention studies (e.g., text-message interventions). This review intends to assess the current state of research on the topic of technology, HIV and substance use; therefore, we did not include white papers or think pieces.
Data Analysis
Following the keyword search, articles were reviewed and input into a database that included title, year published, authorship, technology platforms, target populations, sample size, along with whether the research conducted was an intervention or observational study.
Results
The review included 33 unique studies (Figure 1; Table 1). Most studies were published in 2012 (n=9) and 2013 (n=8). We break these studies down into whether they were interventions or observational studies.
Figure 1.
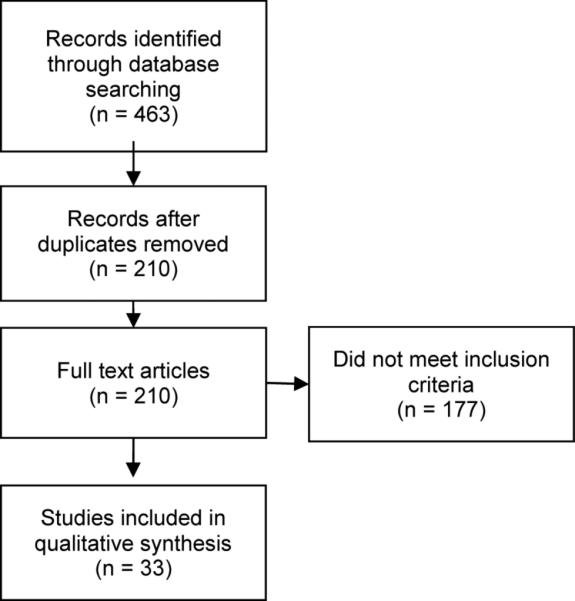
Flow diagram of systematic literature review for online sexual networking and sexual risk behavior [@AU:Please provide brief, descriptive figure legend]
Table 1.
Characteristics of Observational Studies (N=24)
| Author | Year | Platform | Study Sample | Key Findings |
|---|---|---|---|---|
| Fernández et al. | 2005 | HMSM-oriented chatroom | 171 Hispanic MSM | 48.5% had used club drugs in the past 6 months (15.8% cocaine, 11.7% crystal methamphetamines, 31.6% amyl nitrites, 14% ecstasy, 3.5% gamma-hydroxybutyrate, 3.5% ketamine, and 19.3% Viagra) |
| Rhodes et al. | 2007 | Geographically defined Internet chat room and offline | 1189 MSM | 6% reported using methamphetamines during the past 30 days, and methamphetamine use was associated with inconsistent condom use, prior STD, HIV serostatus, and other drug use in the past 30 days. |
| Chiasson et al | 2007 | Online banner ads on 14 gay-oriented websites | 1683 MSM | 24.0% had used drug before sex, 4.3% had used crystal methamphetamine before sex, 7.2% used sildenafil before sex, and 7.1% used nitrite inhalants before sex. |
| Klein | 2009 | MSM-oriented website | 1316 MSM seeking bareback sex | Those who identified to seek for bareback sex were more likely to indicate a desire for having sex while high. |
| Jenness et al. | 2010 | Offline recruitment | 781 MSM | 25% had engaged in frequent binge drinking and 33% used hard drugs. Substance use was associated with meeting partners offline. |
| Lea et al. | 2011 | Facebook, online forums, email referrals, and offline methods | 572 Same-sex attracted youth (18-25) | 4% reported having ever used mephedrone. |
| Klein | 2011 | Telephone survey on 16 different websites (e.g. bareback.com, rawloads.com, men4sexnow.com, and squirt.org) | 332 MSM who use the internet to seek men for unprotected sex | Online participants had much higher percentage of drug use in comparison to average US population. Percent of participants who reported drug use in lifetime and in the last 30 days: cocaine (51.4, 4.5), crack (20.2, 2.4), heroin (12.4, 0.9), hallucinogens (37.5, 0), Ecstasy (36.3, 2.4), any illegal drug use other than marijuana (68.3, 23.0). |
| Wei et al. | 2012 | Gay-oriented website (www.fridae.com) | 10861 MSM | 16.7% reported recreational drug use in the past 6 months. Ecstasy (8.1%) and Viagra (7.9%) was the most prevalent drugs used. HIV positive MSM reported higher levels of drug use compared to HIV negative/unknown MSM. |
| Clark et al. | 2012 | Internet in general | 657 HIV-positive individuals | 35% of homosexual, 26% of heterosexual, and 11% of female participants have reported methamphetamine use in the past year. 29% reported using the Internet to seek sex partners. Internet-users reported having more sexual partners in the past 6 months (4 vs. 1) and higher rates of methamphetamine use (48% vs. 24%) compared to non-Internet users. |
| Ko et al. | 2012 | gay-oriented website (www.fridae.com) | 1645 MSM | 16.0% had used recreational drugs in the previous 6 months. Frequency of drug use was associated with the number of online sexual partners. |
| Wei et al. | 2012 | Gay-oriented website (www.fridae.com) | 416 HIV-positive MSM | Non-disclosure was significantly associated with drug use before sex on a weekly basis. 40.1% have used drug before sex. 40.9% had used alcohol before sex. |
| Whiteley et al. | 2012 | Offline recruitment | 1045 African American adolescents | 6% met sex partners online. Online sex partner seeking was associated with drug use at last sex and cocaine use. 17.7% used alcohol at last sex, 33.9% used other drugs at last sex, 11.3% reported lifetime cocaine use. |
| Grov | 2012 | Craigslist.org | 601 MSM | Men recruited from Craigslist reported the least condom use. Men from Craigslist did not show higher levels of substance use in comparison to participants recruited from bathhouses or bars/clubs. Men from Craigslist reported lifetime use of cocaine (40.1%), methamphetamine (13.1%), MDMA (27.5%), GHB (8.9%), ketamine (9.4%), and Viagra (33.2%). 39.6% reported drinking alcohol 2 or more times per week in the last 3 months. |
| Horvath et al. | 2013 | HIV-related websites, Facebook ads, online search and partnership with other organization, email to former research participants | 276 HIV-positive MSM | Stimulant use is much higher in those who missed HIV medical appointments, and stimulant users also deemed HIV medical appointment to be less important (non-engagement in HIV medical care). |
| Young and Shoptaw | 2013 | 118 MSM | High rates of cocaine (17%) and methamphetamine (15.3%) usage (both over 15% in the past year), past 3 months coke (9.8%) and methamphetamine (8.9%). | |
| White et al. | 2013 | Offline recruitment | 197 MSM | Using internet to meet sexual partners was associated with increased odds of using powdered cocaine in the past 12 months. 24%, 17%, 14%, 6%, and 5% reported powdered cocaine, crack cocaine, poppers, crystal methamphetamine, and heroin. |
| Parsons et al. | 2013 | 1) Dating sites for MSM, 2) MSM chat rooms, 3) Craigslist.org, 4) Facebook page, and 5) Facebook ads | 694 MSM | Men recruited online were more likely to have tried a variety of drugs, such as methamphetamine (22.4%), cocaine (32.6%), ecstasy (16.3%), ketamine (6.6%), GHB (11.4%), poppers (42.9%), and at least one club drug (65.3%) |
| Grov et al. | 2013 | Sexual networking site | 1815 MSM | Individuals surveyed online who practices group sexual encounter are more likely to use stimulants (cocaine, methamphetamine, crack), consumed alcohol (5+), spontaneous group sex. |
| Wilkerson et al. | 2013 | 1) Nine mobile websites or apps used primarily by MSM to meet other men, 2) Browser friendly, 3)Email snowball, 4)Facebook page and Twitter page | 343 Methamphetamine-using MSM | Social media strategy was the most effective one with no cost. |
| Margolis et al. | 2014 | Adult MSM-oriented sexual networking websites | 1319 HIV-positive MSM | 32% of men engaged in anal intercourse without condoms with at-risk partners, and substance use in conjunction with sex is associated with both insertive and receptive anal sex. Intercourse, any drug (71.6%), methamphetamine (28.7%), cocaine/crack (29.8%), heroin (1.7%), club/party drug (26.5%), poppers (54.9%), PDE5 inhibitors (46.2%), inject drugs (16.8%) in the past 60 days. |
| Montoya et al. | 2014 | Within-Study Recruitment | 20 HIV-positive methamphetamine users | This qualitative study demonstrates the feasibility of using focus groups to derive patient-centered intervention content to address the health challenge at hand in targeted populations. |
| Young et al. | 2014 | 550+ Million General Public Twitter Users | Geolocated tweets were extracted and used to create a map displaying the geographical location of HIV-related tweets. There was a significant positive relationship (p<.01) between HIV-related tweets and HIV cases. | |
| Mitchell | 2015 | Facebook-recruitment | 172 HIV-positive and HIV-discordant MSM | Other than alcohol most did not use substance with sex (76.7%). At least one partner in the couple (if not both) used amyl nitrate (29.1%) and party drugs (24.4%). |
| Holloway | 2015 | MSM app-based recruitment | 295 MSM | High rates of recent binge drinking (59 %), marijuana use (37 %), and illicit substance use (27 %) were observed among participants. GSN app use greater than 1 year and showing naked chest or abs in a profile picture were positively associated with recent illicit substance use. |
Observational Studies (N=24)
Observational studies primarily used technology for recruitment of participants, and also for assessment using web-surveys. Recruitment methods included postings or advertisements on social media sites such as Facebook, Craigslist, online discussion forums or chat rooms, gay- or MSM-oriented dating or sexual networking websites or mobile apps, and email referrals. Some studies aimed to recruit Internet/app using samples for risk-assessments, and in some cases, comparisons to non-technology using samples.
Twenty-four observational studies were included in the review. Most of the studies targeted MSM (n=19), with a higher percentage of the observational studies using MSM compared to treatment studies (n=17). Several studies included participants from subgroups of MSM affected by HIV, such as HIV-positive MSM, Hispanic/Latino and African American/black MSM, methamphetamine-using MSM, and MSM seeking bareback sex online (condomless anal intercourse). The size of technology-based observational studies varied, with a large share (n=9) having over 1,000 participants. The recruitment methodologies also varied, with MSM-related sites being the most frequently used recruitment platform (n=12). However, a quarter of the studies recruited participants through Facebook and other social media sites (n=6). It is difficult to summarize the prevalence of substance use reported in each study, as each study reported substance use based on a different timeline (i.e., past 60 days, past 6 months, lifetime).
Several of the observational studies in this review suggested that technology users were more risky than non-technology users or those recruited offline versus online. For example, Parsons et al., (2013) found men recruited online compared to those offline were more likely to have reported trying a variety of drugs, such as methamphetamine (22.4%), cocaine (32.6%), ecstasy (16.3%), ketamine (6.6%), GHB (11.4%), poppers (42.9%), and at least one club drug (65.3%). Other observational studies in this review not comparing technology users found rates of substance use ranging from 5% to 25% depending on the substance (see Table). A study by Holloway (2015) examined correlates of substance use of MSM using a popular geosocial networking application. Of the 295 participants, 59% reported recent binge drinking, 37% reported marijuana use, and 27% reported illicit substance use (i.e., heroin, methamphetamines, ecstasy) in the past 30 days. Using the geosocial networking app for greater than 1 year and showing naked chest or abs in a profile picture were positively associated with recent illicit substance use. In multivariate analyses, the strongest predictors of binge drinking (AOR 3.81; 95 % CI 1.86-7.80), marijuana use (AOR 4.12; 95 % CI 2.22-7.64), and illicit substance use (AOR 6.45; 95 % CI 3.26-12.79) were the presence of a social network member who also engaged in these behaviors.
Intervention Studies (N=9)
Nine of the 33 studies we located were intervention studies. Among the nine intervention studies, most were cellphone/text-based (n=6). The remaining 3 studies were web-based, social media-based, and device-based (web-linked adherence monitoring container), respectively. In general, the interventions focused on reducing HIV risk behaviors and substance use. Four of the interventions involved automatic systems that either call or text participants to solicit responses regarding their sexual risk behavior, well-being, or substance use behaviors, to prompt self-monitoring. While most of the interventions targeted high-risk youth substance users, MSM, and HIV-positive drug users, two studies focused on HIV medication adherence among HIV-positive individuals who also use substances. Recent technology-based intervention applications at the intersection of HIV and substance use have focused on either reducing substance use with HIV-positive and at-risk populations or on HIV prevention with substance-using populations. Below we discuss the intervention studies identified in this review to illustrate the range of technologies used (e.g., IVR calls, apps, text-messaging, and websites) and their applications as adjuncts to person-delivered interventions (e.g., motivational interviewing) or as stand-alone self-directed interventions.
A key example of technology used to enhance person-delivered interventions was the “HealthCall” intervention that tested interactive voice response (IVR) and, more recently smartphone apps, to support motivational interviewing (MI) to reduce substance use in HIV primary care (Aharonovich 2012; Hasin 2013; Hasin 2014). HealthCall utilized daily self-monitoring of substance use and goal progress (and mood, medication adherence, and quality of life) by call into an IVR service to answer brief 1-3 minute surveys, with response data that visualized in time trend graphs and summarized for use in personalized feedback by MI counselors at two 30-day follow-up evaluations. Randomized controlled trial results found greater impact on number of drinking days for MI plus HealthCall compared to MI only and to education only control, with greater effects for alcohol dependent patients compared to non-dependent alcohol users (Hasin, 2013). HealthCall effects were also greatest for patients with lower commitment strength (low motivation, ambivalence), suggesting that daily self-monitoring enhances intervention effects with those most intransigent to change (Aharonovich 2014). A pilot test of a smartphone app version of HealthCall found similar effect to the IVR version but more than 20% greater patient engagement (85% daily participation rates vs. 65%) and high patient satisfaction. Pilot study results of HealthCall on non-injection drug use outcomes suggest similar positive impacts (Aharonovich 2012), however, at 12-month follow-up, ten months after all intervention procedures ended, the trends in effects were similar but had waned and lost statistical significance (Hasin 2013).
The results of the HealthCall intervention speak to the utility of technology for sustaining impacts of brief in-person interventions through self-monitoring. Employing technology for self-monitoring and feedback is scalable and sustainable with relatively low costs compared to follow up counseling sessions. While this has not been tested robustly, there is emerging evidence to support the efficacy of self-monitoring as a self-directed intervention strategy for people living with HIV (PLH) across a range of domains including substance use (Swendeman 2015). The potential efficacy of self-monitoring as a self-directed or adjunct intervention strategy is suggested by consistent findings of “assessment effects” in control groups in substance use intervention studies (Jenkins, 2009) along with qualitative process studies finding that participants recognize this impact and suggest that more frequent assessment (self-monitoring) might result in greater effects (McCambridge, 2009). However, daily self-monitoring is of questionable sustainability in terms of participant burden and burnout (Swendeman et al., 2015), particularly in the absence of a relationship with a service provider, as suggested by decreasing HealthCall app participation when offered after the two-session MI ended.
One key example of technology-delivered and provider-mediated interventions for substance use and HIV outcomes was Project Tech Support (Reback 2012), a text-messaging intervention to reduce methamphetamine use and high-risk sexual behaviors with out-of-treatment MSM. Theory-based messaging content was delivered several times each day by peer health educators (Reback 2015). Results of the two-week intervention pilot of Project Tech Support mediated by health-educators (with up to four text-message conversations per day consisting of up to 20 text-messages each way per conversation) found significant reductions in methamphetamine use and sexual risk behaviors at two-month follow up evaluations (Reback 2015). Pilot study results also suggested that exposure to messages based on the Health Belief Model targeting risk perceptions, and Social Cognitive Theory targeting self-efficacy, were associated with greater efficacy compared to messages based on Social Support Theory. A three-arm randomized controlled trial is currently underway comparing peer health educator mediated messaging to automated messaging and to a weekly text-message self-monitoring survey control condition, over 8 weeks, to examine efficacy and cost-effectiveness over nine months of follow-up. The peer educator-delivered version is tailorable and responsive to participants’ real-time needs for information and support and so is hypothesized to be more efficacious, but is also more costly, compared to the automated and self-monitoring only conditions.
Two additional pilot studies have demonstrated the feasibility and acceptability for self-directed text-messaging interventions to increase antiretroviral adherence among HIV-positive substance users (Moore 2013; Ingersoll 2014). The “iTAB” pilot intervention trial study compared a daily text-message self-monitoring control condition to tailored daily text-message adherence reminders with motivational content along with follow-up by study coordinator after three consecutive days of non-response, and both after a brief 30-minute clinic based adherence education session (Moore 2013). Preliminary results at 30-day follow-up indicated about 70% response rates to text-message surveys, and qualitative feedback on perceived helpfulness of the text-messages but intervention effects from the ongoing trial have not been reported to date.
Similarly, the “Treatment Extension by Text (TxText)” intervention pilot study tested automated text-messaging two-way interaction via daily queries on substance use, adherence and mood and personalized text-message responses tailored to the self-monitoring responses. Preliminary findings from the 3-months response rates to self-monitoring queries were about 65% for each domain (Ingersoll 2014). Full results from these two pilot studies, and over their full intervention durations, will make important contributions to the evidence-base on the potential efficacy and sustainability of self-directed text-messaging interventions via daily self-monitoring of co-morbid substance use, medication non-adherence, and mental health symptoms.
Web-based interventions for substance use and HIV risk behaviors have also shown promising results. One randomized pilot study examined an interactive, self-directed, web-based tool following an in-person, 1-hour, education session compared to education alone among substance-using youth (Marsch, 2011). Findings demonstrated that both groups improved HIV-related knowledge, attitudes, and condom use intentions and skills but found no significant intervention differences for nearly all outcomes except for perceived usefulness of the intervention (90% in web-based and about 75% in the education only condition). A non-randomized pilot study of an 8-session MI and cognitive-behavioral intervention delivered via live social-media chats (via Facebook) with high-risk young MSM to reduce substance use and condomless anal sex, demonstrated feasibility, acceptability, and preliminary efficacy for those who self-selected to participate (Lelutiu-Weinberger, 2015).
Discussion
We reviewed studies published over the past 10 years to assess the current state of research on the topic of technology, HIV and substance use. The majority of these studies were observational in nature and those intervention studies largely relied on small samples to pilot test technology-based programs. Observational studies used technology for recruitment and assessment, often with relatively large samples of over 1,000 participants, including one study of over 550 million data points. Collectively, these studies demonstrate the acceptability of technology-based research on sensitive behaviors of substance use and HIV risk, as well as the massive reach and scalability of these methods.
Less than a third of studies (n=9) examined technologies for interventions, either as adjuncts to a counseling intervention (motivational interviewing) or as a purely self-directed strategy. These studies used text-messaging, interactive voice response, social media chats, smartphone apps, and websites to implement some or all intervention activities. Intervention functions or core practice elements involving technologies included self-monitoring, reminders, feedback, automated and tailored messaging, live chats on social media or text-messaging, and social support. Future research should examine the optimal balance and intensities of self-directed (i.e., self-monitoring, information, automated feedback) and/or relationship-based (i.e., coaching, counseling) interventions in conjunction with technology-mediated intervention strategies to synergize the engagement, efficacy, and cost-effectiveness of the novel opportunities afforded by mobile and social media technologies.
The predominance of pilot studies of mobile health and technology-based interventions (Tomlinson 2013) is clearly evident as only one of the intervention studies in this review had a sample size greater than 85 participants (Vidrine 2012). Most had between 30 to 55 participants. Despite numerous previous studies of Internet-based interventions for HIV, intervention developers and researchers using social media and mobile apps focused more on feasibility, acceptability, and potential efficacy via pilot studies due to the differences in these new technologies. This trend was undoubtedly the result of the novelty of technology-based interventions, particularly 10 years ago, and the necessity to demonstrate feasibility, acceptability, and efficacy prior to large-scale trials. However, it is now time to conduct wide-scale trials that focus on scalability and sustainability, which is a benefit of technology-mediated interventions.
In contrast to in-person interventions, the majority of costs in technology-mediated interventions have been invested in the front-end development, not the ongoing delivery of intervention. Funders and peer-reviewers should strongly consider shifting several norms in funding technology-based interventions. First, little additional research is needed on the feasibility of social media and mobile apps as this work has been repeatedly demonstrated across many populations, settings, and disease priorities. Feasibility and acceptability research is only needed if researchers choose to develop novel technologies (e.g., biosensors), novel intervention strategies (i.e., not identified in this review or demonstrated elsewhere), or highly complex intervention protocols. In the latter case, feasibility and acceptability testing would be needed to identify the intervention elements and design features to be implemented and supported with technologies. The important point is that technologies are tools that can be used to provide information and interventions. The success of a study does not depend on the technology being used as much as the intricacies in how the technology is being used. For example, one study found that the HOPE intervention combined with social media was more effective at increasing HIV testing than a social media group that received HIV information alone (Young et al., 2014). This implies that it is not technology itself that leads to the success of the intervention, but the proper incorporation of evidenced-based approaches into technologies. Social media is just a tool. This tool can be successful or unsuccessful in studies depending on how the tool is being used. Second, and related, studies that build new apps often require the majority of resources to be spent on development at the expense of testing the study through a larger sample size and longer follow-up duration. Because many technologies already exist that can be applied to substance use and HIV (e.g., existing social media technologies like Facebook; text-messaging; IVR platforms; existing mobile apps that were designed for other conditions but can be applied to substance use and HIV), these technologies should be used whenever possible so that research costs can be spent on better study design using larger samples and longer follow-up duration.
Conclusions
This review of the literature to date on technology, HIV and substance use provides a background for clinicians and researchers who are interested in learning more about technologies-based studies, their benefits and drawbacks, and how social network sites, apps, and text messaging might be harnessed for the advancement of health behavior research and clinical care. Given that social network sites and other forms of electronic communication have the capacity to be a conduit for high-risk behaviors, these sites, apps, text messaging, and interactive voice response systems (for low-literacy populations) can also be powerful tools to promote sexual health, sex positivity, disease prevention, and linkage to care and treatment, in addition to drug use reductions. Harnessing the power of social network sites for public health and individual health promotion will require new strategies for rapidly evaluating fast-moving technologies systematically and using harmonized outcomes and assessments that will require unparalleled cooperation between funding agencies, researchers, technology experts, communities, and consumers.
Table 2.
Characteristics of Intervention Studies (N=9)
| Author | Year | Platform | Study Sample | Key Findings |
|---|---|---|---|---|
| Marsch et al. | 2011 | Web-based | 56 Youth substance use patients | Web-based HIV, hepatitis and STI prevention program. Self-directed, interactive 25 modules, some modules are designed for HIV/STI positive individuals. Significant increase in HIV/STI prevention knowledge. Online and offline both experienced behavioral change. Participants in the web-based program reported it to be more useful. |
| Vidrine et al. | 2012 | Cell phone-based | 474 HIV-positive individuals (mostly heterosexuals HIV transmission) | Participants in the smoking cessation cell phone intervention were 4.3 times more likely to be abstinent (7 days) compared to usual care smoking cession treatment group. |
| Reback et al. | 2012 | SMS-based | 52 MSM | At follow-up, men reported significant decreases in the frequency of methamphetamine use and unprotected sex while on methamphetamine and a significant increase in self-reported abstinence from methamphetamine use (13.3% vs. 48.9%). |
| Aharonovich et al. | 2012 | Telephone-based | 40 HIV-positive non-injecting drug users | Participants received phone calls from the Health Call program for the next 30 days. The automated interactive voice response system (Health Call) will assess drug use, HIV adherence, and feelings of wellness, stress, and overall quality of the day (for 30 days). Patients responded by pressing numbers on the keypad. Data were then automatically uploaded to a database. |
| Moore et al. | 2013 | Text messaging | 29 HIV-positive methamphetamine users | Participants were able to customize daily adherence reminders and reinforcement text messages. The study sent daily methamphetamine usage assessment to the participants. Participants were asked to respond to the text yes/no. Participants found the intervention to be acceptable, understandable, satisfied, and mostly improving their adherence. |
| Bachman et al. | 2013 | Web-linked adherence monitoring container (Wisepill) | 10 HIV-positive injection drug users | Study staff provided HIV-positive IDU (former and current) with Wisepill device for their ART medications. |
| Ingersoll et al. | 2014 | Text messaging | 31 Substance users who are non-adherent with HIV medications | Three different types of queries: 1) mood, 2) substance use, 3) medication adherence based on schedule and 4) encouraging texts. Participants were required to reply. Messages were sent for three months. It is acceptable and feasible |
| Hasin et al. | 2014 | Smart phone apps | 84 HIV alcohol dependent patients | Smartphone apps: 1) daily greetings/goodbye, 2) self-monitoring of drinking, drug use, adherence, and sexual risk behavior, 3) self-awareness of drinking reduction goals, and 4) graphical representation of the progress. Patients were highly satisfied with the app. |
| Lelutiu-Weinberger et al. | 2014 | 41 Young MSM | Eight one-hour motivational interviewing and cognitive behavioral live chat (Facebook Message) intervention sessions (i.e. sexual risk behavior, drugs, and self-efficacy, self-monitoring). Participants in the intervention group were found to reduce the days of drug and alcohol use in the past month, and instances of anal sex without a condom, and increased in knowledge of HIV-related risks. |
Footnotes
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Contributor Information
Sean D. Young, University of California Institute for Prediction Technology, UCLA Department of Family Medicine, 10880 Wilshire Blvd Suite 1800, Los Angeles, CA 90049.
Dallas Swendeman, UCLA Center for HIV Identification, Prevention, and Treatment Services, UCLA Department of Psychiatry and Biobehavioral Sciences.
Ian W. Holloway, Department of Social Welfare, UCLA Luskin School of Public Affairs.
Cathy J. Reback, Friends Research Institute, Inc., David Geffen School of Medicine, Integrated Substance Abuse Programs, Semel Institute for Neuroscience and Human Behavior, University of California, Los Angeles.
Uyen Kao, UCLA Center for HIV Identification, Prevention, and Treatment Services, UCLA Department of Family Medicine.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- Bachman Desilva M, Gifford AL, Keyi X, Li Z, Feng C, Brooks, et al. Feasibility and Acceptability of a Real-Time Adherence Device among HIV-Positive IDU Patients in China. AIDS Research and Treatment. 2013;2013:957862. doi: 10.1155/2013/957862. [Study staff provided HIV-positive IDU (former and current) with Wisepill device for their ART medications.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catania JA, Osmond D, Stall RD, Pollack L, Paul JP, Blower S, et al. The continuing HIV epidemic among men who have sex with men. American Journal of Public Health. 2001;91(6):907–914. doi: 10.2105/ajph.91.6.907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC Prevalence and awareness of HIV infection among men who have sex with men: 21 cities, United States, 2008. Morbidity and Mortality Weekly Report. 2010 [PubMed] [Google Scholar]
- Chander G, Himelhoch S, Moore R. Substance abuse and psychiatric disorders in HIV-positive patients. Epidemiology and Impact on Antiretroviral Therapy. 2012 doi: 10.2165/00003495-200666060-00004. [DOI] [PubMed] [Google Scholar]
- Duggan M, Ellison NB, Lampe C, Lenhart A, Madden M. Social Media Site Usage 2014 . [September 2, 2015];Pew Research Center’s Internet & American Life Project. 2015 from Pew Research Center http://www.pewinternet.org/2015/01/09/social-media-update-2014.
- Grov C, Rendina HJ, Ventuneac A, Parsons JT. HIV risk in group sexual encounters: an event-level analysis from a national online survey of MSM in the U.S. The Journal of Sexual Medicine. 2013;10(9):2285–2294. doi: 10.1111/jsm.12227. [Individuals surveyed online who practice group sexual encounter are more likely to use stimulants (cocaine, methamphetamine, crack), consumed alcohol (5+), and have spontaneous group sex.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall H, Song R, Rhodes P, Prejean J, An Q, Lee L. Estimation of HIV incidence in the United States. The Journal of the American Medical Association. 2008 doi: 10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Aharonovich E, O'Leary A, Greenstein E, Pavlicova M, Arunajadai S. Reducing heavy drinking in HIV primary care: a randomized trial of brief intervention, with and without technological enhancement. Addiction. 2013;108(7):1230–1240. doi: 10.1111/add.12127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Aharonovich E, Greenstein E. HealthCall for the smartphone: technology enhancement of brief intervention in HIV alcohol dependent patients. Addiction Science & Clinical Practice, 9, 5. Smartphone apps: 1) daily greetings/goodbye, 2) self-monitoring of drinking, drug use, adherence, and sexual risk behavior, 3) self-awareness of drinking reduction goals, and 4) graphical representation of the progress. Patients were highly satisfied with the app. 2014 doi: 10.1186/1940-0640-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holloway IW. Substance Use Homophily Among Geosocial Networking Application Using Gay, Bisexual and Other Men Who Have Sex With Men. Archives of Sexual Behavior. 2015;44(7):1799–811. doi: 10.1007/s10508-015-0581-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horvath KJ, Carrico AW, Simoni J, Boyer EW, Amico KR, Petroll AE. Engagement in HIV Medical Care and Technology Use among Stimulant-Using and Nonstimulant-Using Men who have Sex with Men. AIDS Research and Treatment. 2013;2013:121352. doi: 10.1155/2013/121352. [Stimulant use is much higher in those who missed HIV medical appointments, and stimulant users also deemed HIV medical appointment to be less important (nonengagement in HIV medical care). 18.97 prevalence for stimulant use.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingersoll K, Dillingham R, Reynolds G, Hettema J, Freeman J, Hosseinbor S, Winstead-Derlega C. Development of a personalized bidirectional text messaging tool for HIV adherence assessment and intervention among substance abusers. Journal of Substance Abuse Treatment. 2014;46(1):66–73. doi: 10.1016/j.jsat.2013.08.002. [Four different types of queries: 1) mood, 2) substance use, 3) medication adherence based on schedule and 4) encouraging texts. Participants were required to reply. Messages were sent for three months. It is acceptable and feasible.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins RJ, McAlaney J, McCambridge J. Change over time in alcohol consumption in control groups in brief intervention studies: systematic review and meta-regression study. Drug Alcohol Depend. 2009;100:107–114. doi: 10.1016/j.drugalcdep.2008.09.016. [DOI] [PubMed] [Google Scholar]
- Landovitz R, Tseng C, Weissman M, Haymer M, Mendenhall B, Rodgers K. Epidemiology, sexual risk behavior, and HIV prevention practices of men who have sex with men using GRINDR in Los Angeles, California. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2012;90(4) doi: 10.1007/s11524-012-9766-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lelutiu-Weinberger C, Pachankis JE, Gamarel KE, Surace A, Golub SA, Parsons JT. Feasibility, Acceptability, and Preliminary Efficacy of a Live-Chat Social Media Intervention to Reduce HIV Risk Among Young Men Who Have Sex With Men. AIDS and Behavior. 2015;19(7):1214–1227. doi: 10.1007/s10461-014-0911-z. [Eight one-hour motivational interviewing and cognitive behavioral live chat (Facebook Message) intervention sessions (i.e. sexual risk behavior, drugs, and self-efficacy, self-monitoring). Participants in the intervention group were found to reduce the days of drug and alcohol use in the past month, and instances of anal sex without a condom, and increased knowledge of HIV-related risks.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenhart A. Teens, social media, & technology overview 2015. Pew Research Center; 2015. [Google Scholar]
- Lenhart A, Purcell K, Smith A, Zichuhr K. Social media & mobile internet use among teens and young adults. Pew Internet & American Life Project. 2010 [Google Scholar]
- Lightfoot M, Rotheram-Borus MJ, Comulada S, et al. Self-monitoring of behaviour as a risk reduction strategy for persons living with HIV. AIDS Care. 2007;19:757–763. doi: 10.1080/09540120600971117. [DOI] [PubMed] [Google Scholar]
- Margolis AD, Joseph H, Hirshfield S, Chiasson MA, Belcher L, Purcell DW. Anal intercourse without condoms among HIV-positive men who have sex with men recruited from a sexual networking web site, United States. Sexually Transmitted Diseases. 2014;41(12):749–755. doi: 10.1097/OLQ.0000000000000206. [32% of men engaged in AI without condoms with at-risk partners, and substance use in conjunction with sex is associated with both insertive and receptive sex. Intercourse, any drug (71.6%), methamphetamine (28.7%), cocaine/crack (29.8), heroin (1.7), club/party drug (26.5%), poppers (54.9%), PDE5 inhibitors (46.2%), inject drugs (16.8) in the past 60 days.] [DOI] [PubMed] [Google Scholar]
- Mathers B, Degenhardt L, Phillips B, Wiessing L, Hickman M, Strathdee S. Global epidemiology of injecting drug use and HIV among people who inject drugs: A systematic review. The Lancet. 2008;372(9651):1733–1745. doi: 10.1016/S0140-6736(08)61311-2. [DOI] [PubMed] [Google Scholar]
- McCambridge J. [Commentary] Research assessments: instruments of bias and brief interventions of the future? Addiction. 2009;104:1311–1312. doi: 10.1111/j.1360-0443.2009.02684.x. [DOI] [PubMed] [Google Scholar]
- Mitchell JW. Relationship characteristics differ based on use of substances with sex among an urban internet sample of HIV-discordant and HIV-positive male couples. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2015;92(1):136–150. doi: 10.1007/s11524-014-9926-z. [Other than alcohol most did not use substance with sex (76.7%). At least one partner in the couple (if not both) used amtl nitrate (29.1%), EDM (34.95), party drugs (24.4%).] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore DJ, Montoya JL, Blackstone K, Rooney A, Gouaux B, Georges S, Tmarc Group, T. Preliminary Evidence for Feasibility, Use, and Acceptability of Individualized Texting for Adherence Building for Antiretroviral Adherence and Substance Use Assessment among HIV-Infected Methamphetamine Users. AIDS Research and Treatment. 2013;2013:585143. doi: 10.1155/2013/585143. [Participants were able to customize daily adherence reminders and reinforcement text messages. In addition, the study sent daily methamphetamine usage assessment to the participants. Participants were asked to respond to the text yes/no. In general, participants found the intervention to be acceptable, understandable, satisfied, and mostly improving their adherence.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montoya JL, Georges S, Poquette A, Depp CA, Atkinson JH, Moore DJ, Translational Methamphetamine AIDS Research Center (TMARC) Group Refining a personalized mHealth intervention to promote medication adherence among HIV+ methamphetamine users. AIDS Care. 2014;26(12):1477–1481. doi: 10.1080/09540121.2014.924213. [Researchers conducted two focus-groups with 20 HIV+/Abusing Methamphetamine (MA) users in a text-based health information program. Adherence barriers included: misguided beliefs about ART adherence and perceived stigma. Facilitators of adherence included cognitive compensatory strategies.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan E, Snelson C, Elison-Bowers P. Image and video disclosure of substance use on social media websites. Computers in Human Behavior. 2010;26(6):1405–1411. [Google Scholar]
- Parsons JT, Vial AC, Starks TJ, Golub SA. Recruiting drug using men who have sex with men in behavioral intervention trials: a comparison of internet and field-based strategies. AIDS and Behavior. 2013;17(2):688–699. doi: 10.1007/s10461-012-0231-0. [Men recruited online were more likely to have tried a variety of drugs, such as methamphetamine (22.4%), cocaine (32.6%), ecstasy (16.3%), ketamine (6.6%), GHB (11.4%), poppers (42.9%), and at least one club drug (65.3%).] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reback CJ, Grant DL, Fletcher JB, Branson CM, Shoptaw S, Bowers JR, Mansergh G. Text messaging reduces HIV risk behaviors among methamphetamine-using men who have sex with men. AIDS and Behavior. 2012;16(7):1993–2002. doi: 10.1007/s10461-012-0200-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reback CJ, Fletcher JB, Shoptaw S, Mansergh G. Exposure to Theory-driven Text Messages is Associated with HIV Risk Reduction among Methamphetamine-using Men who have Sex with Men. AIDS & Behavior. 2015;19:S130–S141. doi: 10.1007/s10461-014-0985-7. [DOI] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Swendeman D, Chorpita BF. Disruptive innovations for designing and diffusing evidence-based interventions. American Psychologist. 2012;67(6):463. doi: 10.1037/a0028180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seth N, Hulda B, Larson P. Efficacy of computer technology-based HIV prevention interventions: A meta-analysis. AIDS. 2009;23(1):107–115. doi: 10.1097/QAD.0b013e32831c5500. [DOI] [PubMed] [Google Scholar]
- Swendeman D, Ramanathan N, Baetscher L, Medich M, Scheffler A, Comulada WS, Estrin D. Smartphone Self-Monitoring to Support Self-Management Among People Living With HIV: Perceived Benefits and Theory of Change From a Mixed-Methods Randomized Pilot Study. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2015;69:S80–S91. doi: 10.1097/QAI.0000000000000570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swendeman D, Rotheram-Borus MJ. Innovation in sexually transmitted disease and HIV prevention: Internet and mobile phone delivery vehicles for global diffusion. Current opinion in psychiatry. 2010;23(2):139. doi: 10.1097/YCO.0b013e328336656a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomlinson M, Rotheram-Borus MJ, Swartz L, Tsai AC. Scaling up mHealth: where is the evidence? PLoS Medicine. 2013;10(2):e1001382. doi: 10.1371/journal.pmed.1001382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White JM, Mimiaga MJ, Reisner SL, Mayer KH. HIV sexual risk behavior among black men who meet other men on the internet for sex. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2013;90(3):464–481. doi: 10.1007/s11524-012-9701-y. [Using internet to meet sexual partners was associated with increased odds of using powdered cocaine in the past 12 months. In general, 24%, 17%, 14%, 6%, and 5% reported powdered cocaine, crack cocaine, poppers, crystal methamphetamine, and heroin.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkerson JM, Shenk JE, Grey JA, Simon Rosser BR, Noor SW. Recruitment Strategies of Methamphetamine-Using Men Who Have Sex with Men into an Online Survey. Journal of Substance Use. 2015;20(1):33–37. doi: 10.3109/14659891.2013.868936. [Social media strategy was the most effective one with no cost.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young S, Cumberland W, Nianogo R, Menacho L, Galea J, Coates T. The HOPE social media intervention for global prevention in Peru: A cluster randomized controlled trial. The Lancet HIV. 2014;2(1):e27–e32. doi: 10.1016/S2352-3018(14)00006-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young S, Rice E. Online social networking technologies, HIV knowledge, and sexual risk and testing behaviors among homeless youth. AIDS and Behavior. 2010;15(2):253–260. doi: 10.1007/s10461-010-9810-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young S, Rivers C, Lewis B. Methods of using real-time social media technologies for detection and remote monitoring of HIV outcomes. Preventive Medicine. 2014;63:112–115. doi: 10.1016/j.ypmed.2014.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young SD, Shoptaw S. Stimulant use among African American and Latino MSM social networking users. Journal of Addictive Diseases. 2013;32(1):39–45. doi: 10.1080/10550887.2012.759859. [High rates of cocaine (17%) and methamphetamine (15.3%) usage (both over 15% in the past year), past 3 months coke (9.8%) and methamphetamine (8.9%).] [DOI] [PMC free article] [PubMed] [Google Scholar]


