Abstract
Objectives:
The aim of this study was to assess and compare the water sorption and flexural strength of thermoplastic and conventional acrylic resins.
Materials and Methods:
Water sorption and flexural strength were compared between a thermoplastic modified polymethyl methacrylate (PMMA) denture base resin (group A) and a heat-polymerized PMMA acrylic resin (group B) as the control group (n=10). A three-point bending test was carried out for flexural strength testing. For water sorption test, 10 disc-shaped samples were prepared. After desiccating, the samples were weighed and immersed in distilled water for seven days. Then, they were weighed again, and desiccated for the second and third times. Differences between the mean values in the two groups were analyzed using Student’s t-test.
Results:
The mean value of water sorption was 14.74±1.36 μg/mm3 in group A, and 19.11±0.90 μg/mm3 in group B; this difference was statistically significant (P< 0.001). The mean value of flexural strength was 88.21±8.63 MPa in group A and 77.77±9.49 MPa in group B. A significant difference was observed between the two groups (P= 0.019).
Conclusion:
Flexural strength of group A was significantly higher than that of group B, and its water sorption was significantly lower. Thus, thermoplastic resins can be a suitable alternative to conventional PMMA acrylic resins as denture base materials.
Keywords: Water; Absorption; Strength, Acrylic resins, denture bases, Polymethyl methacrylate
INTRODUCTION
An ideal denture should have good dimensional stability, fracture resistance, esthetics and tissue compatibility and cause no allergic reaction [1,2]. Polymethyl methacrylate resins are the most commonly used denture base material [3] first introduced in sheet form in 1936 and in the powder form in 1937. This material is available in two forms of heat-activated and chemically-activated based on the method of activation [4]. Considering the polymerization shrinkage of conventional heat-polymerized PMMA, a new injection molding technique was developed. Thermoplastic materials such as Valplast® (Valplast Int. Corp., USA) and Flexiplast (Bredent, Germany) (both polyamides or nylon plastics) were introduced in the 1950s. Then, Acetal, a rapid injection system was introduced in 1971, which was an unbreakable thermoplastic resin. Currently, a new line of thermoplastic Acetal, Acrylic, Nylon and Polycarbonate materials has been introduced. Thermoplastic resins have many advantages over conventional powder or liquid resin systems. They have high flexural and impact strength, flexibility, transparency, high creep resistance, fatigue endurance, excellent wear characteristics and solvent resistance, low water sorption, with no or little residual monomer, and also no porosity, less biologic material build up and less odor and stains and show higher dimensional and color stability. They are free of metal with a microcrystalline structure, which makes finishing and polishing easier as for acrylic resins [4,5].
Water sorption of a material indicates adsorption and absorption of water when in service. The water absorbed by the acrylic resin can act as a plasticizer and cause softening, discoloration [6,7] and loss of mechanical properties of acrylic resin such as hardness, transverse strength and fatigue limit. However, water sorption causes three-dimensional expansion, and can affect the dimensional stability of acrylic resin [8].
Considering the gap of information on this material and its physical and mechanical properties, we aimed to study the water sorption and flexural strength of a thermoplastic PMMA denture base resin in comparison with a heat-polymerized PMMA acrylic resin.
The null hypothesis was that there is no significant difference in the water sorption and flexural strength of the thermoplastic modified PMMA denture base resin and the heat-polymerized PMMA acrylic resin.
MATERIALS AND METHODS
In this study, a thermoplastic denture base resin (Bre.Crystal, Bredent Co., Senden, Germany) (modified PMMA) and a heat-polymerized acrylic resin (Meliodent, Bayer Co., Leverkusen, Germany) (PMMA), as the control group were compared. All the materials tested had a pink shade because of its current use in removable dentures. For water sorption and flexural tests, metal molds were used to fabricate the specimens according to ISO 20795-1: 2008 [9].
The samples were fabricated as instructed by the manufacturers. The PMMA specimens were fabricated in the conventional manner. Polymerization was done in water bath at 70°C for 90 minutes and 100°C for 30 minutes. Thermoplastic specimens were fabricated by the Thermopress 400 injection molding system (Bredent Co., Senden, Germany). The preheating temperature was 260°C and the polymerization was performed at 100°C in 2–3 minutes [10].
The flexural strength and water sorption were tested according to the ADA specification No.12 and ISO No.20795 [6, 9]. For flexural strength testing, 20 samples (10 Bre.Crystal acrylic resin and 10 Meliodent acrylic resin) with dimensions of 2.5×10×65mm were prepared and wet polished using 320–600 grit waterproof silicon carbide abrasive papers (Matador 991A, Soflex, Starcke’s Co., Melle, Germany) as described in ISO 21948: 2001 [11].
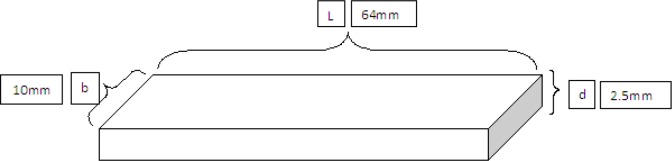
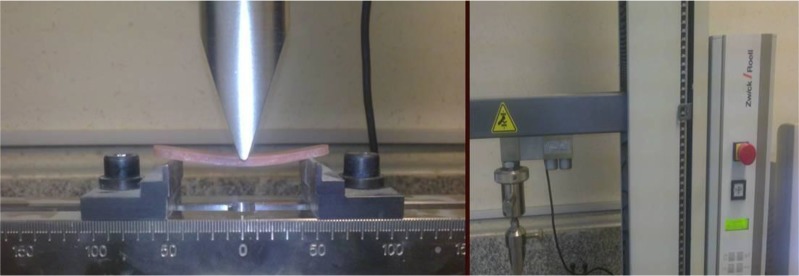
The samples were randomly coded and stored in distilled water at 37±2°C for 50±2 hours using an incubator (Shimifann Co., Tehran, Iran). Each sample was mounted on the jig of a universal testing machine (Z020, Zwick/Roell, Ulm, Germany), load was applied and the load at deflection or fracture of specimens was recorded. A three-point bending test was carried out at a across head speed of 5 mm/min. The formulas provided in the ISO standard were used to calculate the flexural strength (Figs. 1, 2).
- L
length,
- b
width of specimens,
- d
thickness of specimens,
- P
the load at fracture (N)
Fig. 1.
Schematic model of the specimens used for flexural strength testing
Fig. 2.
Universal testing machine for flexural strength testing
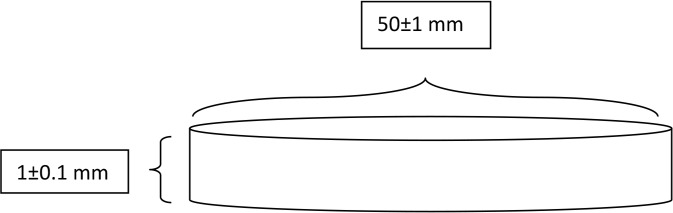
For water sorption testing, the samples were wet-polished with 180–1200-grit waterproof abrasive papers (Matador 991A, Soflex, Starcke’s Co., Melle, Germany) to produce 20 disc-shaped samples (50±1 mm diameter and1±0.1 mm thickness) for both groups. The samples were randomly coded. Then, each sample was placed in a 100 mL round container containing 35g of silica gel (Sorb-It, Sud-Chemie, Rio Grande Industrial Park, Belen, USA) and stored in an incubator (Shimifann Co., Tehran, Iran) at 37±2° for 24 hours for desiccation. Desiccation was repeated until there were no mass changes (0.2 mg or less).
The mass (m0) of each sample was measured using an electronic balance (Sartorius AG, Göttingen, Germany). The samples were then immersed in distilled water at 37±2°C and stored in an incubator for seven days (Shimifann Co., Tehran, Iran). They were removed from the water, wiped with a tissue and the mass of each sample was measured 60 seconds after removal from the water (designated as m1). For the second time, the samples were desiccated in the container containing silica gel, and then we measured the constant weight (m2) [8,12]. The water sorption of the samples was calculated using this formula:
- Wsp
water sorption (μg/mm3),
- V
volume (mm3)
The diameter of the samples was calculated from the mean values of three different points. The mean thickness was measured using the thickness at four equidistant points on the circumference and the thickness at the center of the sample (total of five points).
The volume of each sample (V) was calculated using the mean values for diameter and thickness by a digital caliper (IS11114-150, Insize, China) with an accuracy of 0.01 mm. Testing was repeated three times (Figs. 3 and 4).
Fig. 3.
Schematic model of the specimens used for water sorption testing
Fig. 4.
Samples made of Meliodent conventional acrylic resin and Bre.Crystal thermoplastic acrylic resin for water sorption testing.
Differences between the mean values of the two groups were analyzed using Student’s t-test and PASW18 software.
RESULTS
This study was conducted on 40 samples, including 10 samples made of thermoplastic (Bre.Crystal) and 10 samples made of conventional (Meliodent) acrylic resin to measure flexural strength, and 10 samples made of thermoplastic (Bre.Crystal) and 10 samples made of conventional (Meliodent) acrylic resin for water sorption testing.
The mean value of water sorption was 14.74±1.36 μg/mm3 for thermoplastic acrylic resin (Bre.Crystal) samples and 19.11±0.90 μg/mm3 for the conventional acrylic resin (Meliodent) samples, which were significantly different (P< 0.001). Also, the mean value of flexural strength was 88.21±8.63 MPa for Bre.Crystal acrylic resin and 77.77±9.49 MPa for Meliodent acrylic resin. A significant difference was observed between the two groups (P= 0.019). All acrylic resin samples fractured after the bending test (Table 1).
Table 1.
Descriptive statistics of water sorption (μg/mm3) and flexural strength (MPa) of Meliodent and thermoplastic acrylic resins
| Resin | Minimum | Maximum | Mean | SD | |
|---|---|---|---|---|---|
| Water sorption | Meliodent | 17.74 | 20.56 | 19.11 | 0.90 |
| Thermoplastic | 12.21 | 16.69 | 14.74 | 1.36 | |
| Flexural strength | Meliodent | 60.15 | 92.12 | 77.77 | 9.49 |
| Thermoplastic | 72.12 | 104.76 | 88.21 | 8.63 |
DISCUSSION
Based on the results of the present study, the null hypothesis was refuted. A statistically significant difference in flexural strength (P= 0.019) and water sorption (P< 0.001) was observed between the Meliodent and Thermoplastic (Bre.Crystal) specimens.
The Bre.Crystal thermoplastic material is a modified PMMA indicated for use as a denture base material for partial and complete dentures and also for hard, clear occlusal appliances.
The properties of this material make it a suitable choice for allergic patients as well [10]. The flexural strength of Meliodent conventional acrylic resin in our study was similar to the value reported by other researchers [13–17]. Also, our results showed that the flexural strength and water sorption of Bre.Crystal thermoplastic acrylic resin met the claims of the manufacturer [10]. High water sorption may be due to cross-linking agents, plasticizers, unreacted monomers, initiators or soluble materials [7]. Curing under higher pressure produces specimens with lower water sorption and solubility [18]. The maximum water sorption specified by the ADA is 0.8 mg/cm2 [6] and the maximum value listed by the Institute of Standards and Industrial Research of Iran and ISO is 32 μg/mm3 [19]; our results showed that the water sorption mean values were 14.74±1.36 μg/mm3 for thermoplastic acrylic resin (Bre.Crystal) samples and 19.11±0.90 μg/mm3 for conventional acrylic resin (Meliodent) samples; thus, both groups showed acceptable results. Different results were found in the current study compared to other studies for flexural strength. Ucar et al. [20] demonstrated that the flexural strength of injection-molded PMMA base material (SR-Ivocap) was lower than the conventional PMMA (Meliodent) and polyamide-based, injection molded denture material (Deflex); however, conventional and injection molded PMMA in their study similar to our study fractured after the bending test. Hamanaka et al. [21] demonstrated that all the injection-molded thermoplastic resins had significantly lower flexural strength at the proportional limit (FS-PL), lower elastic modulus, and higher or similar impact strength compared to the conventional PMMA. Four types of other thermoplastic resins were used in their study, and in contrast to our study, the samples deformed after the bending test and did not break.
In another study conducted by Takabayashi [12], six thermoplastic resins and a conventional acrylic resin were examined and the results exhibited that they had lower flexural strength and elastic modulus than conventional PMMA; however, the six thermoplastic resins never broke, although permanent deformation occurred. On the contrary, all acrylic resin specimens broke. Pfeiffer et al. [22] studied the flexural strength of hypoallergenic denture base materials and showed that Polyan (thermoplastic, modified methacrylate) and Promysan (thermoplastic, enterephthalate-based) did not differ significantly from Paladon 65 (heat-polymerized, methacrylate, control group). In accordance with the current study, Negrutiu et al. [5] stated that thermoplastic acrylic resin had low impact resistance and also optimal flexural and tensile strength. The water sorption findings in our study were consistent to those reported by Pfeiffer et al [2]. They stated that the water sorption in thermoplastic group was significantly lower than that of the PMMA control group. Also, Takabayashi [12] stated that there were significant differences in the water sorption of six thermoplastic resins and a conventional PMMA, except for one polyamide resin (Lucitone) that had higher water sorption than the maximum ISO standard values of water sorption for denture base materials 32 μg/mm3 [19]. This material alleviates pain due to denture use because of its high flexural strength and flexibility, providing retention in undercuts of the remaining teeth. Also, due to the lower water sorption and lower solubility of these thermoplastic resins, they have more applications and can be a suitable alternative to conventional PMMA acrylic resins as denture base materials.
This in vitro study had some limitations such as difficult simulation of the oral environment. Further in vitro and in vivo investigations are necessary on the new line of thermoplastic Acetal, Acrylic, Nylon and Polycarbonate materials and their mechanical and chemical properties such as tensile strength, color stability and the amount of residual monomer.
CONCLUSION
Although both groups fractured beyond their proportional limit, the flexural strength of the thermoplastic acrylic resin (Bre.Crystal) was significantly higher than that of Meliodent group. Also, the former had significantly lower water sorption.
REFERENCES
- 1-. Zarb GA, Hobkirk JA, Eckert SE, Jacob RF. Prosthodontic treatment for edentulous patients, complete dentures and implant-supported prostheses. 13th ed, St. Louis, Mosby Inc., 2013: 133– 139. [Google Scholar]
- 2-. Pfeiffer P, Rosenbauer EU. Residual methyl methacrylate monomer, water sorption, and water solubility of hypoallergenic denture base materials. J Prosthet Dent. 2004. July; 92 (1): 72– 8. [DOI] [PubMed] [Google Scholar]
- 3-. Craig RG, Powers JM, Wataha JC. Dental materials, properties and manipulation. 8th Ed., St. Louis, Mosby Inc., 2004: 121. [Google Scholar]
- 4-. Tandon R, Gupta S, Agarwal SK. Denture base materials: from past to future. Ind J Dent Sci. 2010; 2 (2): 33– 9. [Google Scholar]
- 5-. Negrutiu M, Sinescu C, Romanu M, Pop D, Lakatos S. Thermoplastic resins for flexible framework removable partial dentures. Timisoara M J. 2005; 55 (3): 295– 99. [Google Scholar]
- 6-. American National Standards Institute/American Dental Association Specification No. 12-2002, Denture Base Polymers.
- 7-. Craig RG, Powers JM, Sakaguchi RL. Craig's restorative dental materials. 13th ed. St. Louis: Mosby Elsevier; 2011: 51– 52. [Google Scholar]
- 8-. Golbidi F, Taherian A. Comparison of water sorption and solubility of Acropars and Meliodent heat cure acrylic resins. J Dent Med TUMS. 2006; 19 (1): 55– 63. [Google Scholar]
- 9-. ISO 20795-1: 2008, Dentistry-Denture base polymers. International Organization for Standardization. [Google Scholar]
- 10-. www.Bredent.com. Thermopress 400. Information brochure 2009.
- 11-. ISO 21948: 2001, coated abrasives - Plain sheets.
- 12-. Takabayashi Y. Characteristics of denture thermoplastic resins for non-metal clasp dentures. Dent Mater J. 2010. August; 29 (4): 353– 61. [DOI] [PubMed] [Google Scholar]
- 13-. Golbidi F, Jalali O. An evaluation of the Flexural Properties of Meliodent and Acropars Heat Polymerized Acrylic Resins. J Dent Med TUMS. 2007; 4: 55– 63. [Google Scholar]
- 14-. Stipho HD. Repair of acrylic resin denture base reinforced with glass fiber. J Prosthet Dent. 1998. November; 80 (5): 546– 50. [DOI] [PubMed] [Google Scholar]
- 15-. Uzun G, Keyf F. The effect of woven, chopped and longitudinal glass fibers reinforcement on the transverse strength of a repair resin. J Biomater Appl. 2001. April; 15 (4): 351– 8. [DOI] [PubMed] [Google Scholar]
- 16-. Jagger DC, Alshumailin YR, Harrison A, Rees JS. The effect of the addition of poly (methyl methacrylate) fibres on the transverse strength of repaired heat-cured acrylic resin. J Oral Rehabil. 2003. September; 30 (9): 903– 8. [DOI] [PubMed] [Google Scholar]
- 17-. Jagger D, Harrison A, Jagger R, Milward P. The effect of the addition of poly (methyl methacrylate) fibres on some properties of high strength heat-cured acrylic resin denture base material. J Oral Rehabil. 2003. March; 30 (3): 231– 5. [DOI] [PubMed] [Google Scholar]
- 18-. Rejab LT. The effect of the Thermopress curing technique on the water sorption and solubility of the cold and heat–cured acrylic resins. Al–Rafidain Dent J. 2008; 8 (1): 11– 17. [Google Scholar]
- 19-. ISO 1567; 2005, Dentistry-Denture base polymers, International Organization for Standardization. [Google Scholar]
- 20-. Ucar Y, Akova T, Aysan I. Mechanical properties of polyamide versus different PMMA denture base materials. J Prosthodont. 2012. April; 21 (3): 173– 6. [DOI] [PubMed] [Google Scholar]
- 21-. Hamanaka I, Takahashi Y, Shimizu H. Mechanical properties of injection-molded thermoplastic denture base resins. Acta Odontol Scand. 2011. March; 69 (2): 75– 9. [DOI] [PubMed] [Google Scholar]
- 22-. Pfeiffer P, Rolleke C, Sherif L. Flexural strength and moduli of hypoallergenic denture base materials. J Prosthet Dent. 2005. April; 93 (4): 372– 7. [DOI] [PubMed] [Google Scholar]