Case report
A 75-year-old woman in a confused mental state was admitted to our psychiatric University Hospital after being encountered in a disorientated state in a shopping centre. A cerebral computed tomography scan showed no intracranial bleeding or ischaemia, but did show cortical atrophy and a macroadenoma of the pituitary gland with a diameter of 11 mm. A cranial magnetic resonance imaging could not be performed due to agitation. Neurological and physical examination were without pathological findings. Blood pressure was 120/75 mmHg, heart rate was 92/min and body temperature was 36.2°C. Urine analysis and laboratory blood examination including thyroid parameters revealed no pathological findings.
On admission, the patient was disoriented regarding time and place and showed disruption of short-term memory, perseveration and confabulation. According to her legal guardian, apart from cognitive deficits, there was no medical history and no chronic medication. She lived in her own flat without accepting any external care.
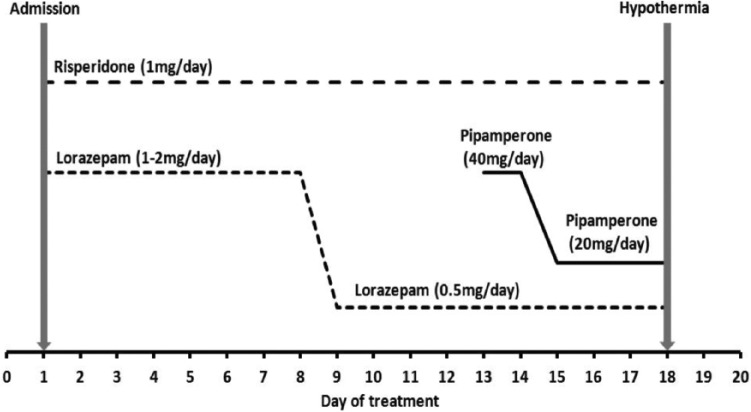
In the days following admission, the patient continued to show an inability to retain new information and in addition presented delusions, visual hallucinations and agitation. On day 1 of treatment, sedation with lorazepam (1–2 mg/day) and antipsychotic medication with risperidone (1 mg/day) were started. Under this medication, psychotic symptoms and psychomotor agitation gradually diminished. On day 13, after reduction of lorazepam to 0.5 mg/day, pipamperone 40 mg/day was added. During the first 2 weeks after admission, no signs of infection, other acute physical illness or dehydration could be detected, while mental function had not improved. Following routine diagnostic procedures, the diagnosis of Alzheimer’s disease (AD) was established according to National Institute of Neurological and Communicative Disorders and Stroke and Alzheimer’s Disease and Related Disorders Association and International Classification of Diseases-10 criteria, respectively, and a medication with donepezil (initial dosage of 5 mg/day) was started.
On the evening of day 18, the patient complained of dizziness, felt cold and was shivering. She had spent the whole day on the ward without being outside. Unexpectedly, a body temperature of 31.9°C was recorded with stable vital signs. Her medication by that time included risperidone 1.0 mg/day, donepezil 5.0 mg/day, torasemide 15 mg/day and lorazepam 0.5 mg/day plus pipamperone 20 mg/day scheduled for the night. Figure 1 illustrates the time course of medication during her stay.
Figure 1.
Temporal relation between drug treatment and hypothermia.
For further management of the hypothermia, the patient was transferred immediately to a medical intensive care unit (ICU). Apart from slight corrected QT interval (QTc) prolongation (125%) in the electrocardiogram, there were no pathological findings (i.e. normal chest/abdomen X-ray, abdomen ultrasound and urine culture). All psychotropic drugs were discontinued and after administration of prewarmed intravenous fluid, body temperature successively stabilized. The patient was transferred back to our psychiatric ward 2 days later. Beforehand, no internal medical condition could be identified as a cause of the hypothermia.
Within the next days, body temperature normalized (> 36.0°C). We prescribed haloperidol 2 mg/day due to recurring psychotic symptoms and restarted medication with donepezil and torasemide. On day 35, we discharged her to a retirement home in a stable psychiatric and medical condition. No further episodes of hypothermia have occurred during a 6 month follow-up.
Discussion
Common causes of hypothermia, defined as a core body temperature lower than 35°C, include prolonged exposure to a cold environment, metabolic disorders (e.g. hypoadrenalism, hypopituitarism or hypothyroidism), burns, head trauma, stroke, ethanol, sepsis and adverse drug effects [McCullough and Arora, 2004].
In this patient, hypothermia occurred at day 18 after admission. Exposure to a cold environment could be excluded as a reason in this case, since the patient has not been outside during the day. Moreover, no signs of infection, metabolic disorder, intoxication, head trauma or neurological disease were present. Upon ICU diagnostic, no medical cause of hypothermia could be detected. The prolonged QTc-time had most likely occurred in direct association with hypothermia [Kreuzer et al. 2012]. Organic brain damage such as in mental retardation and epilepsy is considered to be a risk factor for hypothermia in psychiatric patients and may increase the susceptibility to hypothermia caused by antipsychotics [Kreuzer et al. 2012; van Marum et al. 2007]. We surmise that this also applies to our patient with diagnosed advanced AD. It is unlikely that the detected suprasellar mass caused the hypothermia since, for example, suprasellar pituitary adenomas are known to cause an increase of body temperature rather than a reduction [Behr et al. 1996].
Medication known to cause hypothermia are sedative-hypnotics, antithyroid drugs, narcotics and typical as well as atypical antipsychotics [Parris et al. 2001; Schwaninger et al. 1998]. In particular, antipsychotic drugs with strong 5-HT2 antagonism seem to be more frequently associated with hypothermia [Kreuzer et al. 2012].
After remission of hypothermia, we resumed the medication with torasemide and donepezil, and hypothermia did not recur. Hence, both drugs are unlikely to have caused hypothermia in our case. Lorazepam was the patient’s evening medication and was prescribed from day 1 in an initially much higher dosage. Thus, we do not regard it as the cause of hypothermia. Pipamperone, which was started 5 days before the onset of hypothermia, has a half-life of about 17–22 h, and is known to cause hypothermia [Eikenboom et al. 1997; Schwaninger et al. 1998], as well as risperidone [Kreuzer et al. 2012; Perera and Yogaratnam, 2014], which the patient has been receiving on admission in a stable dosage.
Risperidone is a second-generation, atypical antipsychotic drug with antagonistic action on both serotonin 5-HT2 and dopamine D2 receptors. Pipamperone is a butyrophenone derivative with antagonistic action on serotonin 5-HT2 (specifically 5-HT2a) with an additional low affinity to D2 and H1 receptors, respectively. The exact mechanism of antipsychotics causing hypothermia is unknown. It has been considered that drugs with stronger 5-HT2a than D2 antagonism are more likely to induce hypothermia than other antipsychotics [Kreuzer et al. 2012; Perera and Yogaratnam, 2014; van Marum et al. 2007]. In our case, we propose the combination of two drugs with strong 5-HT2 antagonism as the cause. Dopamine D2 receptor antagonism may have been of minor significance since hypothermia did not recur with the subsequent haloperidol treatment. Of course, for ethical reasons, we did not reintroduce risperidone or pipamperone in spite of clinical efficacy prior to the occurrence of the adverse effect.
To our knowledge, this is the seventh publication of risperidone-induced and the third publication of pipamperone-induced hypothermia. To date, no such adverse event after intake of the combination of both drugs has been reported. Taken together, we recommend strict indication for antipsychotic medication, especially when given in combination and in elderly patients. Vital parameters including body temperature should be carefully monitored under such circumstances.
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest statement: The authors declare that there is no conflict of interest.
Contributor Information
Daniel Kamp, Heinrich Heine Universität Duesseldorf, Bergische Landstraße 2, 40629 Duesseldorf, Germany.
Myrella Paschali, Heinrich Heine Universität Duesseldorf, Duesseldorf, Germany.
Tillmann Supprian, Heinrich Heine Universität Duesseldorf, Duesseldorf, Germany.
Christian Lange-Asschenfeldt, Heinrich Heine Universität Duesseldorf, Duesseldorf, Germany.
References
- Behr R., Dietrich C., Brück K., Roosen K. (1996) Comparison of thermoregulatory characteristics of patients with intra- and suprasellar pituitary adenomas. Acta Neurochir Suppl 65: 44–49. [DOI] [PubMed] [Google Scholar]
- Eikenboom H., Janssens A., Rosekrans P., Molendijk W. (1997) [Hypothermia during use of pipamperone.] Ned Tijdschr Geneeskd 141: 301–303. [PubMed] [Google Scholar]
- Kreuzer P., Landgrebe M., Wittmann M., Schecklmann M., Poeppl T., Hajak G., et al. (2012) Hypothermia associated with antipsychotic drug use: a clinical case series and review of current literature. J Clin Pharmacol 52: 1090–1097. [DOI] [PubMed] [Google Scholar]
- McCullough L., Arora S. (2004) Diagnosis and treatment of hypothermia. Am Fam Physician 70: 2325–2332. [PubMed] [Google Scholar]
- Parris C., Mack J., Cochiolo J., Steinmann A., Tietjen J. (2001) Hypothermia in 2 patients treated with atypical antipsychotic medication. J Clin Psychiatry 62: 61–63. [DOI] [PubMed] [Google Scholar]
- Perera M., Yogaratnam J. (2014) De novo delayed onset hypothermia secondary to therapeutic doses of risperidone in bipolar affective disorder. Ther Adv Psychopharmacol 4: 70–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwaninger M., Weisbrod M., Schwab S., Schröder M., Hacke W. (1998) Hypothermia induced by atypical neuroleptics. Clin Neuropharmacol 21: 344–346. [PubMed] [Google Scholar]
- Van Marum R., Wegewijs M., Loonen A., Beers E. (2007) Hypothermia following antipsychotic drug use. Eur J Clin Pharmacol 63: 627–631. [DOI] [PMC free article] [PubMed] [Google Scholar]