Abstract
Background:
Although endoscopic bilateral stent-in-stent (SIS) placement of self-expandable metallic stents (SEMS) is one of the major palliative treatments for unresectable malignant hilar biliary obstruction, post-endoscopic retrograde cholangiopancreatography (ERCP) cholangitis can occur frequently due to inadequate drainage, especially after contrast injection into the biliary tree. The aim of this study is to evaluate the efficacy and safety of air cholangiography-assisted stenting.
Methods:
This study included 47 patients with malignant hilar biliary obstruction who underwent endoscopic bilateral SEMS placement using the SIS technique. They were divided into two groups, air (n = 23) or iodine contrast (n = 24) cholangiography. We retrospectively compared comprehensive clinical and laboratory data of both groups.
Results:
There were no significant differences found between the two groups with respect to technical success (87% versus 87.5%, air versus contrast group, respectively), functional success (95% versus 95.2%), 30-day mortality (8.3% versus 8.7%) and stent patency. Post-ERCP adverse events occurred in 5 (21.7%) of the patients in the air group and 8 (33.3%) of the patients in the contrast group. Among these, the rate of cholangitis was significantly lower in the air group (4.8% versus 29.2%, p = 0.048). In multivariate analysis, air cholangiography, technical success and a shorter procedure time were significantly associated with a lower incidence of post-ERCP cholangitis.
Conclusions:
Air cholangiography-assisted stenting can be a safe and effective method for endoscopic bilateral SIS placement of SEMS in patients with malignant hilar biliary obstruction.
Keywords: air cholangiography, malignant hilar biliary obstruction, self-expandable metallic stent, stent-in-stent
Introduction
Endoscopic biliary drainage is the palliative treatment of choice for unresectable malignant hilar biliary obstruction. Although the choice of unilateral or bilateral drainage is still controversial [Chang et al. 1998; De Palma et al. 2001], bilateral drainage theoretically provides a more normal and physiological biliary flow through the biliary ductal system than does unilateral drainage [Polydorou et al. 1991; Sherman, 2001]. In addition, recent studies have reported that at least 50% drainage of the liver volume is associated with a sufficient drainage effectiveness or longer survival in patients with malignant hilar obstruction [Vienne et al. 2010; Bulajic et al. 2012].
Endoscopic bilateral drainage using a self-expandable metallic stent (SEMS) can be performed using one of two techniques: the side-by-side technique or the stent-in-stent (SIS) technique [Dumonceau et al. 2011]. Among these, the SIS technique is an alternative endoscopic procedure that allows the deployment of a Y-configuration for bilateral metallic stenting. This technique has a lower complication rate and similar stent patency to the side-by-side technique [Naitoh et al. 2012]. Despite recent innovations in endoscopic technology, endoscopic bilateral SEMS placement using the SIS technique is still considered more technically difficult with a higher risk of adverse events compared with unilateral stenting [Chang et al. 1998; De Palma et al. 2001; Naitoh et al. 2009].
Post-endoscopic retrograde cholangiopancreatography (ERCP) cholangitis can occur frequently due to inadequate drainage, especially after contrast injection into the biliary tree. To prevent post-ERCP cholangitis, some strategies such as a contrast-free method [Singh et al. 2004], magnetic resonance cholangiopancreatography (MRCP) and/or computed tomography (CT)- guided drainage [Hintze et al. 2001; Freeman and Overby, 2003], air cholangiography [Pisello et al. 2009; Singh et al. 2010; Sud et al. 2010] and CO2 cholangiography [Zhang et al. 2013] have recently been introduced. Among these, air cholangiography has been shown to be a safe and effective method for unilateral stenting in malignant hilar biliary obstruction in previous studies, which showed a low incidence of post-ERCP cholangitis [Pisello et al. 2009; Singh et al. 2010; Sud et al. 2010]. However, there has been no study to date evaluating the clinical outcomes of air cholangiography for bilateral metallic stenting, especially the SIS technique.
Therefore, the aim of this study is to evaluate the efficacy and safety of air cholangiography in endoscopic bilateral SIS placement of SEMS for malignant hilar biliary obstruction.
Methods
Patients
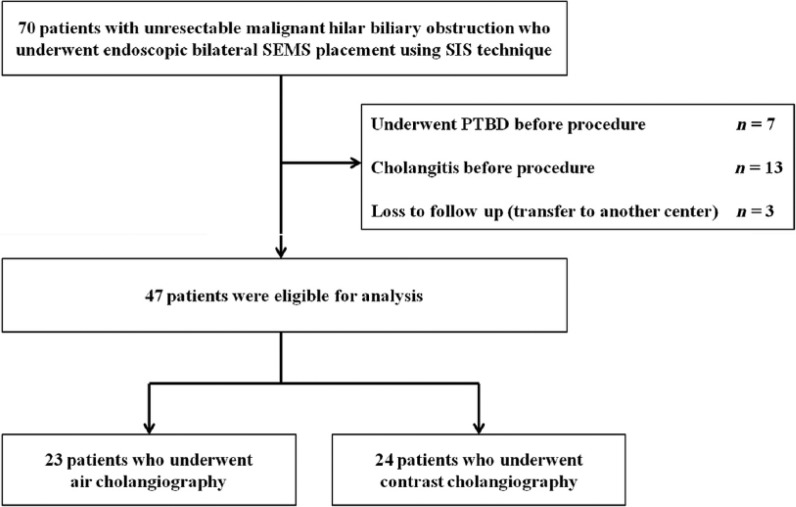
This retrospective study initially included all patients (n = 70) who underwent endoscopic bilateral SEMS placement using the SIS technique for unresectable malignant hilar biliary obstruction at Seoul National University Hospital between January 2011 and December 2013. At our institution, iodine contrast cholangiography had been performed as a primary method for endoscopic bilateral SIS placement of SEMS from January 2011 to June 2012. However, based on the evidence from a previous report showing favorable efficacy of air cholangiography [Sud et al. 2010], air instead of iodine contrast has been used as an initial cholangiography at our institution since July 2012. Patients were excluded for the following reasons: underwent percutaneous transhepatic biliary drainage (PTBD) before the procedure (n = 7); cholangitis before the procedure (n = 13); and loss to follow-up within 6 months following stent insertion (n = 3). A flow chart showing the patient selection for the current study is seen in Figure 1. Finally, a total of 47 patients were included in the analysis and divided into two groups, air (n = 23) or iodine contrast (n = 24) cholangiography. The diagnosis was principally made on the basis of ultrasound, CT and magnetic resonance imaging. MRCPs were performed to identify the Bismuth classification of hilar biliary obstruction. The histological and/or cytological confirmation of malignancy for all patients was established by endoscopic tissue sampling and/or brushing. Follow-ups continued from the stent insertion for 1 month or until the death of the patient. The study protocol was approved by the Institutional Review Board of the Seoul National University Hospital (IRB No. H-1402-037-556).
Figure 1.
Flow chart of patient selection for the study.
PTBD, percutaneous transhepatic biliary drainage; SEMS, self-expandable metallic stent; SIS, stent-in-stent.
Procedure and techniques
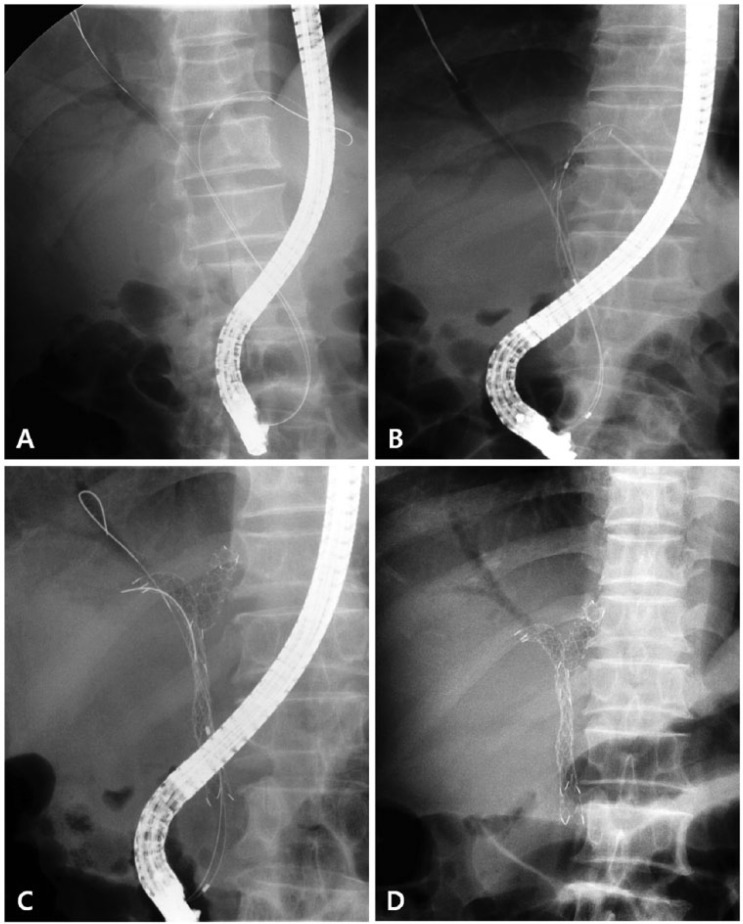
The technique of endoscopic bilateral SIS placement using SEMS was carried out as follows. The decision to perform bilateral stent insertion was based on imaging studies before the initial ERCP. Patients were sedated with intravenous midazolam (0.05 mg/kg) and pethidine under appropriate cardiopulmonary monitoring. The duodenoscopes used for this procedure were TJF-240 or 260V (Olympus Optical Co. Ltd., Tokyo, Japan) with large working channels (4.2 mm). After deep cannulation was achieved, a guidewire (Jag-Wire, Boston Scientific, Natick, Mass; VisiGlide, Olympus Optical Co. Ltd, Tokyo, Japan) was inserted through the malignant stenosis into a preselected duct. An ERCP catheter was then passed over the guidewire across the stenosis until bile was aspirated to confirm the position and to decrease the intraductal pressure. Air cholangiography was then obtained by injecting 10–15 ml of air into the targeted intrahepatic duct, and the opacified ductal system was compared with the intended segment for drainage on MRCP. After visualizing both intrahepatic ducts, guidewires were inserted into both intrahepatic ducts, respectively. The first stent was then inserted and slowly deployed into the left or right intrahepatic duct over the guidewire. After deployment of the first stent across the hilar biliary obstruction, the remaining guidewire across the first stent was carefully withdrawn using an ERCP catheter without pulling it back completely. It was then inserted under fluoroscopic guidance into the undrained intrahepatic duct through the central portion of the first stent. The second stent was deployed through the mesh of the first stent, so that the two stents overlapped in the common hepatic duct and branched into the hepatic ducts, forming a Y-shape. The SEMS used in this study was a small cell-sized stent (BONASTENT M-Hilar; Standard Sci Tech Inc., Seoul, South Korea) or large cell-sized stent (Niti-S large cell D-type biliary stent; Taewoong Medical Co. Ltd, Seoul, South Korea). The same cell-sized stent was bilaterally inserted in each patient (Figure 2).
Figure 2.
Procedure of air cholangiography and endoscopic bilateral SIS placement of SEMS. (A) Air cholangiography through a papillotome. (B) The first stent was inserted into the left hepatic duct. (C) The guidewire was placed in the right hepatic duct through the stent mesh and the second stent was then inserted. (D) Bilateral metallic stenting was performed using the SIS technique.
SEMS, self-expandable metallic stent; SIS, stent-in-stent.
Definition of events
Technical success (successful stent insertion) was defined as the passage of the stent across the stricture, along with the flow of contrast medium and/or bile through the stent. Functional success (successful drainage) was defined as a decrease in the total bilirubin level to less than 50% of the pretreatment value within the first month. The definitions of post-ERCP adverse events were defined according to the criteria of Cotton and colleagues [Cotton et al. 1991] and Freeman and colleagues [Freeman et al. 1996]. Cholangitis was defined as a new onset of fever (temperature ⩾38°C) without sources of infection outside the biliary tract and persisting for longer than 24 hours after ERCP. Pancreatitis was defined as persistent significant abdominal pain for longer than 24 hours with an elevation of serum amylase and/or lipase more than 3 times the upper limit of normal after ERCP. Significant bleeding was indicated by a decrease in the serum hemoglobin level ⩾2 mg/dl with a requirement for a blood transfusion or hemostatic interventions. Perforation included retroperitoneal or bowel wall perforation documented by any radiographic technique. Stent occlusion was defined as the recurrence of jaundice, an increase in total bilirubin level and dilatation of the intrahepatic bile duct as revealed by imaging. Stent patency was defined as the period after stent insertion until stent occlusion or until the patient’s death. A 30-day mortality was defined as death occurring within 30 days of the first attempt at endoscopic stent insertion, whether successful or unsuccessful.
Study outcomes
The primary outcomes were short-term clinical outcomes including the rate of technical or functional success, post-ERCP adverse events and stent patency. The secondary outcome was to identify the risk factors for post-ERCP cholangitis in endoscopic bilateral SIS placement of SEMS for malignant hilar biliary obstruction.
Statistical analyses
Data are shown as the number (%) for categorical variables, and as median [interquartile range (IQR)] for continuous variables and stent patency period. In univariate analyses, the Mann–Whitney test and the Chi-square test with Fisher’s exact test were used for comparison of continuous or categorical variables, respectively. The Wilcoxon signed rank test was used for the comparison of the total bilirubin level between the baseline and 1 month after the procedure. The cumulative stent patency was estimated by Kaplan–Meier analysis and the curves were compared by the log-rank test. A logistic regression test analysis was used for the multivariate analysis. Age, gender and all variables with a p value <0.1 in the univariate analysis were entered into the multivariate analysis; p < 0.05 for two-sided tests was considered statistically significant. In this study, the odds ratio (OR) is reported together with their 95% confidence intervals (CIs). All statistical analyses were performed using SPSS 20.0 (SPSS Inc., Chicago, IL, USA).
Results
Clinical characteristics of patients
The demographic and clinical characteristics of all 47 patients who underwent an endoscopic bilateral SIS placement of SEMS for malignant hilar biliary obstruction are summarized in Table 1. The median patient age was 69 years (IQR 59–77). The causes of malignant hilar biliary obstruction were cholangiocarcinoma (n = 24), gallbladder cancer (n = 18) and metastatic cancer (n = 5). According to the Bismuth classification, hilar obstructions were type II in 10 patients, type III in 10 and type IV in 27. A total of 38 patients (80.9%) received intravenous antibiotics 1 hour prior to the procedure. There were no significant differences in age, gender, symptoms, diagnosis, Bismuth classification, TNM staging, SEMS type, antibiotic prophylaxis, precut sphincterotomy or laboratory findings between the two groups.
Table 1.
Baseline characteristics of patients with malignant hilar biliary obstruction according to the method of cholangiography.
| Air group (n = 23) | Contrast group (n = 24) | p value | |
|---|---|---|---|
| Age (year)* | 69 (57–76) | 68 (62–77) | 0.717 |
| Gender | 0.676 | ||
| Male | 13 (56.5) | 15 (62.5) | |
| Female | 10 (43.5) | 9 (37.5) | |
| Symptom | |||
| Jaundice | 23 (100) | 24 (100) | >0.99 |
| Pruritus | 23 (100) | 23 (95.8) | >0.99 |
| Fever | 0 (0) | 0 (0) | >0.99 |
| Anorexia | 23 (100) | 24 (100) | >0.99 |
| Weight loss | 23 (100) | 24 (100) | >0.99 |
| Diagnosis | |||
| Cholangiocarcinoma | 12 (52.2) | 12 (50) | 0.557 |
| Gallbladder cancer | 7 (30.4) | 11 (45.8) | 0.371 |
| Metastatic cancer | 4 (17.4) | 1 (4.2) | 0.188 |
| Bismuth classification | |||
| II | 5 (21.7) | 5 (20.8) | >0.99 |
| III | 6 (26.1) | 4 (16.7) | 0.494 |
| IV | 12 (52.2) | 15 (62.5) | 0.561 |
| TMN staging | 0.666 | ||
| IVA | 3 (13.0) | 2 (8.3) | |
| IVB | 20 (87.0) | 22 (91.7) | |
| SEMS type | 0.534 | ||
| Small cell-sized stent | 17 (73.9) | 15 (62.5) | |
| Large cell-sized stent | 6 (26.1) | 9 (37.5) | |
| Antibiotic prophylaxis | 18 (78.3) | 20 (83.3) | 0.724 |
| Precut sphincterotomy | 2 (8.7) | 1 (4.2) | 0.609 |
| Laboratory finding* | |||
| Total bilirubin (mg/dl) | 8.5 (5.2–13.4) | 5.2 (3.8–11.4) | 0.302 |
| ALP (IU/l) | 521 (316–646) | 547 (242–693) | 0.932 |
Values are presented as median (interquartile range). Other values are presented as number (%).
ALP, alkaline phosphatase; IU, international unit; SEMS, self-expandable metallic stent.
Primary outcomes
The clinical outcomes according to the method of cholangiography are summarized in Table 2. Technical success was achieved in 20 of the 23 patients (87%) in the air group and 21 of the 24 patients (87.5%) in the contrast group (p > 0.99). The main reason for unsuccessful stent insertion was that the guidewire could not pass through the malignant hilar biliary obstruction. All patients with a failed procedure were then successfully treated by PTBD. Functional success rate in the air group and contrast group was 95% and 95.2%, respectively (p > 0.99). The median total bilirubin level was significantly reduced from 8.5 mg/dl (IQR 5.2–13.4) to 1.1 mg/dl (IQR 0.8–1.8) in the air group (p < 0.001) and from 5.2 mg/dl (IQR 3.8–11.4) to 1.0 mg/dl (IQR 0.6–1.5) in the contrast group (p = 0.003).
Table 2.
Clinical outcomes of patients with malignant hilar biliary obstruction according to the method of cholangiography.
| Air group (n = 23) | Contrast group (n = 24) | p value | |
|---|---|---|---|
| Technical success | 20/23 (87.0) | 21/24 (87.5) | >0.99 |
| Functional success | 19/20 (95.0) | 20/21 (95.2) | >0.99 |
| Procedure time after cholangiography (minute)* | 30 (24.5–41) | 25 (20–38) | 0.104 |
| Post-ERCP adverse events | 5/23 (21.7) | 8/23 (33.3) | 0.374 |
| Cholangitis | 1/23 (4.3) | 7/24 (29.2) | 0.048 |
| Pancreatitis | 3/23 (13.0) | 1/24 (4.2) | 0.348 |
| Perforation | 1/23 (4.3) | 0/24 (0) | 0.489 |
| Hospital day after procedure* | 6 (3–12) | 6 (2–9) | 0.645 |
| Total bilirubin after 1 month (mg/dl)* | 1.1 (0.8–1.8) | 1.0 (0.6–1.5) | 0.262 |
| 30-day stent occlusion$ | 2/20 (9.1) | 1/21 (4.8) | >0.99 |
| 30-day mortality | 2/23 (8.3) | 2/24 (8.7) | >0.99 |
Values are presented as median (interquartile range). Other values are presented as number (%).
Causes of stent occlusion were tumor ingrowth in all patients.
ERCP, endoscopic retrograde cholangiopancreatography.
Post-ERCP adverse events were observed in 5 patients (21.7%) in the air group and 8 patients (33.3%) in the contrast group (p = 0.517), which were successfully treated with conservative treatments. The rate of cholangitis in the air group was significantly lower than that in the contrast group (4.3% versus 29.2%, p = 0.048). With respect to pancreatitis and perforation, there were no significant differences between the two groups and other adverse events were not found. In the air group, periampullary perforation occurred in one patient who underwent a precut sphincterotomy using a needle-knife as a result of difficult biliary cannulation. This patient was successfully treated with conservative treatment. A stent occlusion within 30 days following the procedure occurred in 2 (9.1%) of the patients in the air group and in 1 (4.8%) of the patients in the contrast group (p > 0.99). The causes of stent occlusion were tumor ingrowth in all patients. A reintervention was successfully performed by PTBD in all patients with stent occlusion. A total of 2 patients (8.3%) in the air group and 2 patients (8.7%) in the contrast group died of disease progression within 30 days after the procedure (p > 0.99).
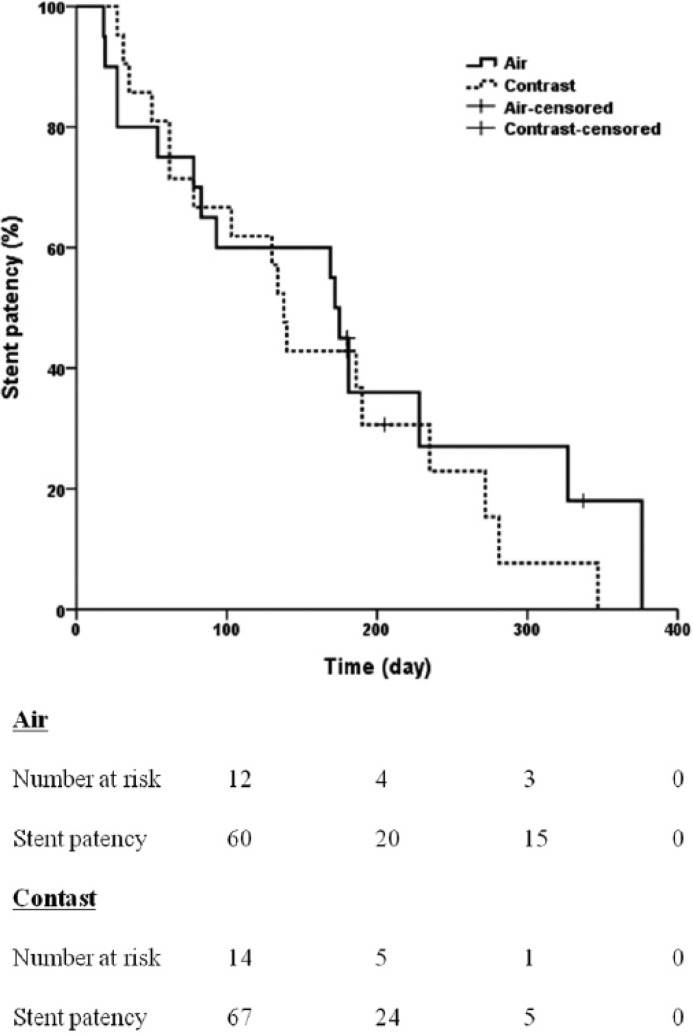
There were no differences in the cumulative stent patency between the two groups (p = 0.533) (Figure 3). The median stent patency period was 172 days (IQR 54–327) in the air group and 138 days (IQR 62–235) in the contrast group.
Figure 3.
Cumulative stent patency curve by Kaplan–Meier analysis showing no differences between the air and contrast groups (p = 0.533).
Secondary outcomes
A total of 47 patients with malignant hilar biliary obstruction were analyzed to determine the risk factors for post-ERCP cholangitis after endoscopic bilateral SIS placement of SEMS. Post-ERCP cholangitis occurred in 8 (17%) patients. Univariate analysis identified that air cholangiography was the only variable showing significant (p < 0.05) association with post-ERCP cholangitis. Multivariate analysis showed that air cholangiography, technical success and a shorter procedure time were significantly associated with a lower incidence of post-ERCP cholangitis (Table 3).
Table 3.
Univariate and multivariate analyses of risk factors for post-ERCP cholangitis in patients with malignant hilar biliary obstruction who underwent endoscopic bilateral SIS placement of SEMS.
| Factor | Univariate analysis |
Multivariate analysis |
|||
|---|---|---|---|---|---|
| Patients with cholangitis (n = 8) | Patients without cholangitis (n = 39) | p value | Odds ratio (95% CI) | p value | |
| Age (year)* | 74 (65–80) | 67 (58–76) | 0.182 | 1.062 (0.929–1.214) |
0.378 |
| Male/female | 5/3 | 23/16 | > 0.99 | 1.271 (0.086–18.786) |
0.861 |
| Air cholangiography | 1 (12.5) | 22 (56.4) | 0.048 | 0.008 (0.000–0.862) |
0.043 |
| Diagnosis | |||||
| Cholangiocarcinoma | 4 (50) | 20 (51.3) | > 0.99 | ||
| Gallbladder cancer | 4 (50) | 14 (35.9) | 0.692 | ||
| Metastatic cancer | 0 (0) | 5 (12.8) | 0.571 | ||
| Bismuth classification | |||||
| II | 1 (12.5) | 9 (23.1) | 0.667 | ||
| III | 2 (25) | 8 (20.5) | 0.494 | ||
| IV | 5 (62.5) | 22 (56.4) | 0.340 | ||
| TNM staging | 0.571 | ||||
| IVA | 0 (0) | 5 (12.8) | |||
| IVB | 8 (100) | 34 (87.2) | |||
| SEMS type | 0.697 | ||||
| Small cell-sized stent | 5 (62.5) | 27 (69.2) | |||
| Large cell-sized stent | 3 (37.5) | 12 (30.8) | |||
| Antibiotic prophylaxis | 5 (62.5) | 33 (84.6) | 0.167 | ||
| Technical success | 5 (62.5) | 36 (92.3) | 0.053 | 0.021 (0.001–0.578) |
0.022 |
| Functional success | 4/5 (80) | 35/36 (97.2) | 0.232 | ||
| Procedure time after cholangiography (minute)* | 45 (23–54) | 26 (22–36) | 0.081 | 1.202 (1.014–1.425) |
0.034 |
| Laboratory finding* | |||||
| Total bilirubin (mg/dl) | 6.6 (4.6–11.3) | 7.0 (3.7–13.4) | 0.749 | ||
| ALP (IU/l) | 493 (226–647) | 542 (288–706) | 0.813 | ||
Values are presented as median (interquartile range). Other values are presented as the number or percentage.
Values in bold are statistically significant.
ALP, alkaline phosphatase; CI, confidence interval; SEMS, self-expandable metallic stent.
Discussion
Post-ERCP cholangitis is a major problem in endoscopic biliary drainage for patients with malignant hilar biliary obstruction, which occurs in 4–57% of cases [Deviere et al. 1988; Figueras et al. 1998]. Inadequate drainage is one of the major causes of post-ERCP cholangitis, especially following contrast injection. Therefore, post-ERCP cholangitis may occur frequently in endoscopic bilateral SIS placement of SEMS for malignant hilar biliary obstruction. For this reason, air cholangiography has been recently investigated as a strategy to prevent post-ERCP cholangitis [Pisello et al. 2009; Singh et al. 2010; Sud et al. 2010]. However, there has been no study to evaluate the clinical outcomes of air cholangiography alone for bilateral metallic stenting, especially the SIS technique for malignant hilar biliary obstruction. The present study shows that air cholangiography-assisted stenting was significantly associated with a lower incidence of post-ERCP cholangitis in endoscopic bilateral SIS placement of SEMS for malignant hilar biliary obstruction.
De Palma and colleagues reported that the rate of post-ERCP cholangitis may be reduced by several factors: minimal injection of contrast media that avoids filling the undrained ducts; adequate antibiotics coverage; single SEMS placement with minimal interventions; and duration of procedure [De Palma et al. 2001]. In addition, they found that bilateral drainage has a significantly higher rate of early cholangitis than does unilateral drainage (16.6% versus 8.8%, p = 0.013) [De Palma et al. 2001]. A recent prospective pilot study demonstrated the feasibility and safety of air cholangiography for unilateral metallic stenting in 17 patients with type II and III malignant hilar obstruction [Sud et al. 2010]. Therefore, we hypothesized that air cholangiography may be applicable in bilateral metallic stenting for malignant hilar biliary obstruction. Our results show no significant differences in short-term clinical outcomes and stent patency between the air and contrast groups, with the exception of post-ERCP cholangitis. Despite technical difficulties of bilateral metallic stenting, these findings are consistent with previous studies related to air cholangiography for unilateral stenting [Pisello et al. 2009; Singh et al. 2010; Sud et al. 2010].
In the current study, the rate of post-ERCP cholangitis was 4.3% in the air group and 29.2% in the contrast group (p = 0.048). This significant difference may be explained by factors associated with pathogenesis of cholangitis. Post-ERCP cholangitis mainly occurred in the presence of contaminated contrast media in the obstructed biliary tract. Despite bilateral metallic stenting, some contrast media may be injected into the undrained biliary tract, which can raise the ductal pressure. The elevation of intrabiliary pressure leads to disruption of the tight junctions between hepatocytes, impaired Kupffer cell function, and lack of clearance of contaminants that occurs with normal bile flow [Sung et al. 1992]. According to the hydrostatic law, the pressure in the system is directly proportional to the density in the system, and the density of contrast media at room temperature is higher than that of air. Therefore, the use of air as a contrast can lead to a lower elevation of the pressure inside the undrained biliary tract compared with conventional contrast media.
Hintze and colleagues reported a high successful drainage (86%) and a low post-ERCP cholangitis (6%) in 35 patients with type III and IV malignant hilar obstruction who underwent MRCP-guided unilateral stenting with minimal contrast injection above the stricture [Hintze et al. 2001]. In addition, Freeman and Overby found that MRCP and/or CT-guided unilateral metallic stenting in 35 patients with malignant hilar biliary obstruction provided safe and effective palliation in most patients [Freeman and Overby, 2003]. Therefore, air cholangiography-assisted stenting could be more effective and safer with the help of MRCP as a preliminary imaging study to obtain the biliary anatomy before ERCP, which is consistent with our findings.
The present study showed that the incidence of cholangitis in the contrast group was relatively high compared with recent reports of bilateral stenting for malignant hilar biliary obstruction [Park Do et al. 2009; Lee et al. 2013; Kogure et al. 2014]. This finding can be explained by the difference in baseline characteristics. Our patients had less Bismuth type II and more Bismuth type IV than the patients of previous studies [Park Do et al. 2009; Lee et al. 2013; Kogure et al. 2014]. Because Bismuth type IV had severe biliary separation, cholangitis could occur frequently due to inadequate drainage, especially after intentional contrast injection into the biliary tree [Pisello et al. 2009; Lee et al. 2015]. In addition, unlike previous studies [Park Do et al. 2009; Lee et al. 2013; Kogure et al. 2014; Lee et al. 2015], our study included patients with technical failure in the analysis. Among seven patients with post-ERCP cholangitis in the contrast group, there was technical failure in three patients.
In the current study, air embolism was not observed as a complication in the air group. However, air embolism is a rare but lethal complication of air insufflations in the bile duct during ERCP, which may bring concerns about the use of air cholangiography. For this reason, Zhang and colleagues reported the safety of CO2 cholangiography in endoscopic biliary drainage for malignant hilar biliary obstruction [Zhang et al. 2013]. Thus, further work needs to be carried out to evaluate the efficacy and safety of CO2 cholangiography-assisted stenting.
Our study has some limitations. Firstly, it was conducted in a nonrandomized retrospective manner, without a predefined follow-up protocol. Secondly, the study was conducted in a highly experienced single center with a high prevalence of malignant hilar biliary obstruction; technical and functional success rates may differ in nonspecialist centers. Therefore, a further prospective multicenter randomized study is needed to confirm the current observations.
Conclusion
Air cholangiography-assisted stenting can be a safe and effective method for endoscopic bilateral SIS placement of SEMS in patients with malignant hilar biliary obstruction. To the best of our knowledge, our work is the first study identifying the clinical usefulness of air cholangiography for endoscopic bilateral SIS placement of SEMS. These results may be helpful to other endoscopists who are concerned about post-ERCP cholangitis in bilateral metallic stenting.
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest statement: The authors declare no conflicts of interest in preparing this article.
Contributor Information
Jae Min Lee, Departments of Internal Medicine and Liver Research Institute, Seoul National University College of Medicine, Seoul National University Hospital, Seoul, Korea; Department of Internal Medicine, Gyeongsang National University College of Medicine, Gyeongsang National University Hospital, Jinju, Korea.
Sang Hyub Lee, Departments of Internal Medicine and Liver Research Institute, Seoul National University College of Medicine, Seoul National University Hospital, 101 Daehak-ro, Jongno-gu, Seoul 110-744, Korea.
Dong Kee Jang, Departments of Internal Medicine and Liver Research Institute, Seoul, Korea; National University College of Medicine, Seoul National University Hospital, Seoul, Korea.
Kwang Hyun Chung, Departments of Internal Medicine and Liver Research Institute, Seoul, Korea; National University College of Medicine, Seoul National University Hospital, Seoul, Korea.
Jin Myung Park, Department of Internal Medicine, Kangwon National University School of Medicine, Kangwon National University Hospital, Chuncheon, Korea.
Woo Hyun Paik, Department of Internal Medicine, Inje University Ilsan Paik Hospital, Goyang, Korea.
Jun Kyu Lee, Department of Internal Medicine, Dongguk University Ilsan Hospital, Dongguk University College of Medicine, Goyang, Korea.
Ji Kon Ryu, Departments of Internal Medicine and Liver Research Institute, Seoul, Korea; National University College of Medicine, Seoul National University Hospital, Seoul, Korea.
Yong-Tae Kim, Departments of Internal Medicine and Liver Research Institute, Seoul, Korea; National University College of Medicine, Seoul National University Hospital, Seoul, Korea.
References
- Bulajic M., Panic N., Radunovic M., Scepanovic R., Perunovic R., Stevanovic P., et al. (2012) Clinical outcome in patients with hilar malignant strictures type II Bismuth-corlette treated by minimally invasive unilateral versus bilateral endoscopic biliary drainage. Hepatobiliary Pancreat Dis Int 11: 209–214. [DOI] [PubMed] [Google Scholar]
- Chang W., Kortan P., Haber G. (1998) Outcome in patients with bifurcation tumors who undergo unilateral versus bilateral hepatic duct drainage. Gastrointest Endosc 47: 354–362. [DOI] [PubMed] [Google Scholar]
- Cotton P., Lehman G., Vennes J., Geenen J., Russell R., Meyers W., et al. (1991) Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc 37: 383–393. [DOI] [PubMed] [Google Scholar]
- De Palma G., Galloro G., Siciliano S., Iovino P., Catanzano C. (2001) Unilateral versus bilateral endoscopic hepatic duct drainage in patients with malignant hilar biliary obstruction: results of a prospective, randomized, and controlled study. Gastrointest Endosc 53: 547–553. [DOI] [PubMed] [Google Scholar]
- Deviere J., Baize M., De Toeuf J., Cremer M. (1988) Long-term follow-up of patients with hilar malignant stricture treated by endoscopic internal biliary drainage. Gastrointest Endosc 34: 95–101. [DOI] [PubMed] [Google Scholar]
- Dumonceau J., Heresbach D., Deviere J., Costamagna G., Beilenhoff U., Riphaus A., et al. (2011) Biliary stents: models and methods for endoscopic stenting. Endoscopy 43: 617–626. [DOI] [PubMed] [Google Scholar]
- Figueras J., Llado-Garriga L., Lama C., Pujol-Rafols J., Navarro M., Martinez-Villacampa M., et al. (1998) [Resection as elective treatment of hilar cholangiocarcinoma (Klatskin tumor)]. Gastroenterol Hepatol 21: 218–223. [PubMed] [Google Scholar]
- Freeman M., Nelson D., Sherman S., Haber G., Herman M., Dorsher P., et al. (1996) Complications of endoscopic biliary sphincterotomy. N Engl J Med 335: 909–918. [DOI] [PubMed] [Google Scholar]
- Freeman M., Overby C. (2003) Selective MRCP and CT-targeted drainage of malignant hilar biliary obstruction with self-expanding metallic stents. Gastrointest Endosc 58: 41–49. [DOI] [PubMed] [Google Scholar]
- Hintze R., Abou-Rebyeh H., Adler A., Veltzke-Schlieker W., Felix R., Wiedenmann B. (2001) Magnetic resonance cholangiopancreatography-guided unilateral endoscopic stent placement for Klatskin tumors. Gastrointest Endosc 53: 40–46. [DOI] [PubMed] [Google Scholar]
- Kogure H., Isayama H., Nakai Y., Tsujino T., Matsubara S., Yashima Y., et al. (2014) High single-session success rate of endoscopic bilateral stent-in-stent placement with modified large cell Niti-S stents for malignant hilar biliary obstruction. Dig Endosc 26: 93–99. [DOI] [PubMed] [Google Scholar]
- Lee J., Lee S., Chung K., Park J., Paik W., Woo S., et al. (2015) Small cell- versus large cell-sized metal stent in endoscopic bilateral stent-in-stent placement for malignant hilar biliary obstruction. Dig Endosc 27: 692–699. [DOI] [PubMed] [Google Scholar]
- Lee T., Moon J., Kim J., Park D., Lee S., Choi H., et al. (2013) Primary and revision efficacy of cross-wired metallic stents for endoscopic bilateral stent-in-stent placement in malignant hilar biliary strictures. Endoscopy 45: 106–113. [DOI] [PubMed] [Google Scholar]
- Naitoh I., Hayashi K., Nakazawa T., Okumura F., Miyabe K., Shimizu S., et al. (2012) Side-by-side versus stent-in-stent deployment in bilateral endoscopic metal stenting for malignant hilar biliary obstruction. Dig Dis Sci 57: 3279–3285. [DOI] [PubMed] [Google Scholar]
- Naitoh I., Ohara H., Nakazawa T., Ando T., Hayashi K., Okumura F., et al. (2009) Unilateral versus bilateral endoscopic metal stenting for malignant hilar biliary obstruction. J Gastroenterol Hepatol 24: 552–557. [DOI] [PubMed] [Google Scholar]
- Park Do H., Lee S., Moon J., Choi H., Cha S., Kim J., et al. (2009) Newly designed stent for endoscopic bilateral stent-in-stent placement of metallic stents in patients with malignant hilar biliary strictures: multicenter prospective feasibility study (with videos). Gastrointest Endosc 69: 1357–1360. [DOI] [PubMed] [Google Scholar]
- Pisello F., Geraci G., Modica G., Sciume C. (2009) Cholangitis Prevention in endoscopic Klatskin tumor palliation: air cholangiography technique. Langenbecks Arch Surg 394: 1109–1114. [DOI] [PubMed] [Google Scholar]
- Polydorou A., Cairns S., Dowsett J., Hatfield A., Salmon P., Cotton P., et al. (1991) Palliation of proximal malignant biliary obstruction by endoscopic endoprosthesis insertion. Gut 32: 685–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman S. (2001) Endoscopic drainage of malignant hilar obstruction: is one biliary stent enough or should we work to place two? Gastrointest Endosc 53: 681–684. [DOI] [PubMed] [Google Scholar]
- Singh V., Singh G., Gupta V., Gupta R., Kapoor R. (2010) Contrast-free air cholangiography-assisted unilateral plastic stenting in malignant hilar biliary obstruction. Hepatobiliary Pancreat Dis Int 9: 88–92. [PubMed] [Google Scholar]
- Singh V., Singh G., Verma G., Singh K., Gulati M. (2004) Contrast-free unilateral endoscopic palliation in malignant hilar biliary obstruction: new method. J Gastroenterol Hepatol 19: 589–592. [DOI] [PubMed] [Google Scholar]
- Sud R., Puri R., Hussain S., Kumar M., Thawrani A. (2010) Air cholangiogram: a new technique for biliary imaging during ERCP. Gastrointest Endosc 72: 204–208. [DOI] [PubMed] [Google Scholar]
- Sung J., Costerton J., Shaffer E. (1992) Defense system in the biliary tract against bacterial infection. Dig Dis Sci 37: 689–696. [DOI] [PubMed] [Google Scholar]
- Vienne A., Hobeika E., Gouya H., Lapidus N., Fritsch J., Choury A., et al. (2010) Prediction of drainage effectiveness during endoscopic stenting of malignant hilar strictures: the role of liver volume assessment. Gastrointest Endosc 72: 728–735. [DOI] [PubMed] [Google Scholar]
- Zhang R., Zhao L., Liu Z., Wang B., Hui N., Wang X., et al. (2013) Effect of CO2 cholangiography on post-ercp cholangitis in patients with unresectable malignant hilar obstruction - a prospective, randomized controlled study. Scand J Gastroenterol 48: 758–763. [DOI] [PubMed] [Google Scholar]