Abstract
As leading barriers to specialist care, wait times are at the forefront of the Canadian healthcare policy agenda. However, knowledge is limited about how wait times affect patients' lives. We utilized the 2010 Canadian Community Health Survey to examine the experience of patients requiring a consultation with a medical specialist for a new condition. Multivariate logistic regression predicted the likelihood that a respondent self-reported his or her life was affected. Subsequent cross-tabulations determined the ways in which life was affected. Females, middle-aged respondents, new immigrants and those with low income and poor health status were more likely to report their life was affected. Worry, stress and anxiety were the most frequently reported impacts, followed by pain, stress on family/friends, deterioration of health and loss of work. Our research demonstrates a need to address the impacts of wait times on health and well-being, with a focus on particular subpopulation groups.
Abstract
À titre d'obstacle principal pour l'accès aux services d'un spécialiste, les temps d'attente figurent en tête de liste des programmes d'action pour les services de santé au Canada. Cependant, on connaît peu la façon dont les temps d'attente affectent la vie des patients. À l'aide des données de l'Enquête sur la santé dans les collectivités canadiennes de 2010, nous avons étudié l'expérience des patients qui nécessitent une consultation auprès d'un spécialiste pour un nouvel état de santé. Une analyse de régression logistique multivariable a permis de prédire la probabilité qu'un répondant auto-déclare que sa vie en est affectée. Des tableaux croisés subséquents ont permis de déterminer de quelles façons leur vie était affectée. Les personnes les plus susceptibles d'indiquer que leur vie est affectée sont les femmes, les personnes d'âge moyen, les nouveaux immigrants et les personnes à faible revenu ainsi que celles dont l'état de santé est le plus fragile. Les impacts les plus déclarés sont l'inquiétude, le stress et l'anxiété, suivi de la douleur, du stress sur la famille et les amis, de la détérioration de l'état de santé et de la perte d'emploi. Notre recherche démontre qu'il faut traiter les impacts des temps d'attente sur la santé et le bien-être, en mettant un accent particulier sur des sous-groupes particuliers de la population.
The Canada Health Act (1985) removed financial barriers to healthcare by mandating that access to medically necessary services be available to all Canadians. While this legislation eliminates socio-economic inequities in access, other barriers to medically necessary healthcare services persist. Wait times are consistently identified as leading barriers by patients and providers (Barua and Esmail 2012; Sanmartin et al. 2004, 2007; Wilson and Rosenberg 2004), though less attention has been paid to specialist care. Access to specialist care is fundamentally different than primary care, as patients generally require a referral from a general practitioner or other health professional for access (Dunlop et al. 2000). As part of a gatekeeper model of care, time spent waiting from the referral to initial contact with a specialist represents an important period in the continuum of care (Liddy et al. 2013).
International comparisons reveal that Canadians are more likely to wait for access to specialist care than people in other countries (Bichel et al. 2009; Health Council of Canada 2010; Schoen et al. 2009). Over the past two decades, the total time the average Canadian spends waiting between referral from a general practitioner to consultation with a specialist has increased by 129%, from 3.7 weeks in 1993 to 8.5 weeks in 2012 (Barua and Esmail 2012). Time spent waiting for specialist care is not necessarily problematic in and of itself; however, it is if there are related adverse health effects or other impacts on patients' lives. For example, waiting six months or longer for treatment for chronic pain has been associated with general deterioration in emotional health related to psycho-social outcomes and loss of quality of life (Lynch et al. 2008). As well, longer wait times for adjuvant therapy for cancer have been linked to increased likelihood of cancer recurrence and decreased survival times (Chen et al. 2008; Kulkarni et al. 2009).
Because wait times vary by health need and demographic and socio-economic factors, it is plausible that the impacts of wait times also vary among subpopulation groups, an important area for research. It is also important to understand the diverse range of ways in which people's lives are affected by wait times for specialist care. Thus, the goals of this study are twofold: to examine the reasons that patients might report that their life is affected by time spent waiting for a specialist consultation, and to examine the ways in which patients' lives are affected.
Methods
This study used data from the 2010 Canadian Community Health Survey (CCHS) public use microdata file (Statistics Canada 2012). The CCHS is a cross-sectional telephone survey that collects information regarding the health, health behaviours and healthcare utilization of Canadians over 12 years of age. This study focused on an optional module of the survey related to access to specialist care, collected in Ontario (n=21,536; response rate, 70.0%). The study sample included all respondents who required a visit to a medical specialist for a consultation or diagnosis for a new condition in the year prior to the survey (n=2,516). These respondents also answered follow-up questions about barriers to accessing care and questions related to ensuing impacts on their lives.
Respondents were asked about their experience waiting to visit a specialist, including whether they had visited the specialist already; whether the visit had been cancelled or postponed at any time; and whether the respondent felt that his or her life had been affected by waiting for the specialist visit. The survey then asked how the patient's life was affected, listing the following categories:
1. Worry, anxiety, stress
2. Worry or stress for family or friends
3. Pain
4. Problems with activities of daily living (e.g., dressing, driving)
5. Loss of work
6. Loss of income
7. Increased dependence on relatives/friends
8. Increased use of over-the-counter drugs
9. Overall health deteriorated, condition got worse
10. Health problem improved
11. Personal relationships suffered
12. Other
Independent variables were coded as shown in Table 1. Potential covariates were included per Aday and Andersen's (1974) behavioural model for access to medical care related to predisposing characteristics, enabling characteristics and need. Predisposing characteristics refer to those that guide an individual's propensity to use health services (e.g., age, sex). Enabling characteristics reflect the ability of individuals to engage with health services defined by personal resources, or resources that are available in one's local area, state or country (e.g., income, education, having a family doctor, health region of residence). Income was defined by household income quintiles adjusted by household size and community of residence. Statistics Canada uses health regions as the primary sampling frame for the CCHS, and health regions were re-categorized as “Urban,” “Rural” and “City of Toronto.” Health regions were categorized as urban if they satisfied one of two criteria: the health region had more than 150 people per square kilometre (OECD 1994) or the health region contained a Census Metropolitan Area that represented at least 85% of the population of the region. This definition has been used successfully elsewhere (Harrington et al. 2013).
TABLE 1.
Variable coding scheme
| Determinant type | Variable | Coding |
|---|---|---|
| Predisposing factors | Sex | Female (reference) / Male |
| Age | Under 30 (ref.) / 30–44 / 45–59 / 60+ | |
| Marital status | No partner (ref.) / Living with a partner | |
| Time since immigration | Born in Canada (ref.) / Less than 10 years / More than 10 years | |
| Enabling factors | Education | Less than high school (ref.) / High school / Post-secondary educated |
| Income | Lowest (1st) income quintile (Ref.) / 2nd / 3rd / 4th / 5th | |
| Health region | City of Toronto (ref.) / Urban / Rural | |
| Visited specialist | No – still waiting (ref.) / Yes | |
| Time spent waiting | Less than 1 month (ref.) / 1–3 months / 3–6 months / Over 6 months | |
| Opinion of wait time | Acceptable (ref.) / Not acceptable | |
| Need factors | Chronic conditions | No chronic conditions (ref.) / 1–3 conditions / 4+ conditions |
| Self-rated general health | Good (ref.) / Poor |
Need factors refer to actual or perceived health and are recognized as the most important determinants of healthcare use (Aday and Andersen 1974). Self-rated health was included as a measure of health need, recoded here as good (i.e., excellent, very good or good) or poor (i.e., fair, poor). The CCHS also collects data on a range of self-reported chronic conditions including asthma, arthritis, high blood pressure, chronic obstructive pulmonary disorder (COPD), diabetes, heart disease and cancer, among others. Respondents were classified as having any chronic conditions versus none.
Descriptive statistics were all calculated with population weights provided by Statistics Canada. A weighted multivariate logistic regression model was used to predict the likelihood that respondents' lives were affected during the time spent waiting to visit a specialist. A subsequent analysis based on frequency of response was also used to determine the range of ways in which waiting for a specialist had affected respondents' lives. Analyses are presented with 95% confidence intervals generated using a bootstrap technique. All analyses were performed using R v. 2.15.1 (The R Project for Statistical Computing 2013).
Results
A descriptive summary of the CCHS cohort, compared to the subsample of interest, is presented in Table 2. In terms of accessing specialist services, 26.5% of the population required a visit to a specialist in the previous year. Of these, 44.1% required a specialist visit for a new illness or condition. The mean wait time between scheduling an appointment with a specialist and visiting a specialist for a new illness/condition was 63.3 days (median, 30.0 days). However, those who had already visited the specialist at the time of the survey had shorter average wait times (mean, 56.5 days) than those who were still waiting for their appointment (mean, 139.9 days). Approximately 21.2% of respondents requiring a visit for a new condition reported that their life was affected by the wait to see the specialist.
TABLE 2.
Sample characteristics with 95% confidence intervals
| Attribute | CCHS Ontario (%) | Required a specialist for a new condition (%) |
|---|---|---|
| Female | 51.0 ± 1.2 | 59.6 ± 3.2 |
| Under 30 | 28.0 ± 1.1 | 17.4 ± 2.3 |
| 30–44 | 24.2 ± 1.2 | 23.2 ± 2.6 |
| 45–59 | 26.3 ± 1.2 | 31.6 ± 3.4 |
| 60+ | 21.6 ± 0.8 | 27.8 ± 2.7 |
| Living with partner | 59.0 ± 1.3 | 64.1 ± 3.0 |
| Canadian-born | 67.2 ± 1.3 | 69.1 ± 3.4 |
| Immigrant: < 10 years | 8.2 ± 0.8 | 6.9 ± 2.3 |
| Immigrant: 10+ years | 24.6 ± 1.2 | 24.0 ± 3.3 |
| Less than $20,000 | 7.5 ± 0.7 | 7.6 ± 1.6 |
| $20,000–$39,999 | 15.6 ± 0.8 | 15.5 ± 2.2 |
| $40,000–$59,999 | 16.9 ± 1.0 | 14.1 ± 2.4 |
| $60,000–$79,999 | 16.3 ± 1.2 | 15.6 ± 2.8 |
| $80,000 and more | 43.7 ± 1.4 | 47.1 ±3.5 |
| Less than secondary school | 19.8 ± 0.8 | 12.0 ± 1.9 |
| Has a family doctor | 89.4 ± 0.9 | 95.3 ± 1.2 |
| No chronic conditions | 54.5 ± 1.3 | 37.7 ± 3.1 |
| City of Toronto | 20.9 ± 1.2 | 21.4 ± 3.2 |
| Urban | 56.6 ± 1.3 | 56.2 ± 3.2 |
| Rural | 22.4 ± 0.8 | 22.3 ± 2.4 |
The multivariate logistic regression model (Table 3) revealed a number of significant covariates. In terms of predisposing factors, females were more likely than males, and those from the middle-age groups (i.e., between 30 and 59) were more likely than younger or older respondents, to report that their life had been affected by the wait, though the relationship was significant only for the 30–44 age group. In general, new immigrants were more likely than Canadian-born respondents to report that their life had been affected (OR=1.95).
TABLE 3.
Multivariate logistic regression of life affected by waiting
| Factor | OR | 95% CI | Signif. |
|---|---|---|---|
| Intercept | 0.07 | (0.03, 0.17) | *** |
| Sex (ref: Female) | |||
| Male | 0.74 | (0.54, 0.99) | * |
| Age (ref: Under 30) | |||
| 30–44 | 1.67 | (1.01, 2.80) | * |
| 45–59 | 1.49 | (0.91, 2.50) | |
| 60+ | 0.91 | (0.53, 1.58) | |
| Living arrangement (ref: No partner) | |||
| Partner | 1.18 | (0.84, 1.65) | |
| Time since immigration (ref: Canadian born) | |||
| Less than 10 years | 1.95 | (1.07, 3.55) | * |
| 10 or more years | 1.27 | (0.90, 1.79) | |
| Income (ref: Lowest quintile – 1) | |||
| Quintile 2 | 0.85 | (0.53, 1.37) | |
| Quintile 3 | 0.51 | (0.32, 0.82) | ** |
| Quintile 4 | 0.53 | (0.33, 0.86) | ** |
| Quintile 5 | 0.38 | (0.23, 0.61) | *** |
| Education (ref: Less than high school) | |||
| High school | 2.01 | (1.17, 3.56) | * |
| Self-rated health (ref: Good) | |||
| Poor | 1.47 | (1.01, 2.13) | * |
| Chronic conditions (ref: None) | |||
| 1+ conditions | 2.24 | (1.60, 3.17) | *** |
| Visited specialist (ref: Waiting) | |||
| Visited specialist | 0.24 | (0.16, 0.37) | *** |
| Wait time (ref: <1 month) | |||
| 1–3 months | 1.76 | (1.21, 2.55) | ** |
| 3–6 months | 1.92 | (1.23, 3.00) | ** |
| 6 months or more | 2.78 | (1.54, 5.05) | *** |
| Opinion of wait time (ref: Acceptable) | |||
| Not acceptable | 11.28 | (7.95, 16.19) | *** |
| Health Region (ref: City of Toronto) | |||
| Urban | 0.82 | (0.56, 1.20) | |
| Rural | 0.91 | (0.56, 1.47) | |
Significance codes: p<0.05=*;
p<0.01=**;
p<0.001=***
Respondents who had completed at least a secondary school level of education were more likely than their counterparts who had not completed high school (OR=2.01) to report that their life had been affected waiting for a specialist visit. Income displayed an overall negative association with the odds of reporting life being affected. That is, as level of income increased from the lowest quintile to the highest, the odds of reporting that life was affected by the wait to see a specialist decreased. At the regional level, no differences were found between those living in the City of Toronto, other urban areas or rural regions.
Health status was significant in the model. In particular, respondents with chronic conditions were more than twice as likely to report that their life was affected by the wait (OR=2.24) than those with no chronic conditions, while those with poor self-rated general health were approximately 1.5 times as likely.
There was substantial difference between respondents who had seen the specialist already and those that were still waiting. Specifically, those who had already visited the specialist were approximately 75% less likely to report that their life had been affected by the wait time. Longer wait times exhibited a clear dose–response effect, with the odds of reporting that life had been affected by the wait increasing with the length of time waiting. Compared to respondents who had waited/been waiting for less than a month, the odds ratios associated with waiting for 1–3 months, 3–6 months and more than 6 months climbed from 1.76 to 1.92 and then to 2.78, respectively. Finally, respondents who perceived their time waiting to see a specialist as unacceptable were 11.3 times more likely to report that their life had been affected.
The ways in which respondents reported that their lives were affected by waiting for a specialist visit are presented in Figure 1. Respondents could provide more than one response. The most frequently reported way in which life was affected was worry, stress and anxiety (69.1%). This was followed by pain (42.1%), worry or stress for friends or family (25.2%), reduced activities of daily living (24.3%) and deterioration of health (21.7%). Loss of work, increased use of over-the-counter medication and loss of income were mentioned relatively less frequently, but still by more than 10% of the respondents.
FIGURE 1.
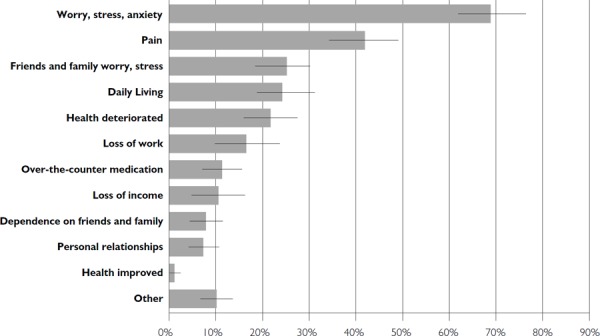
How life was affected by wait to see a specialist: frequencies of responses with 95% confidence intervals
Discussion
Approximately 20% of respondents requiring a visit to a specialist for consultation or diagnosis related to a new condition reported that their life was affected by the time spent waiting from referral to visit. This percentage is comparable with the findings of Sanmartin and colleagues (2006), who reported that 17.7% of Canadians reported that their life had been affected. However, their analysis focused on all visits to a specialist, whereas in this study the focus was on specialist visits for new conditions, potentially explaining the slight difference.
The results indicate that psycho-social effects, including worry, stress and anxiety, were the most frequently reported impacts followed by pain, stress on family and friends and deterioration of health. Psycho-social and physical impacts of wait times have been documented previously (e.g., Lynch et al. 2008; Sanmartin et al. 2007). However, the current study contributes by providing an understanding of a more diverse range of the ways in which life is affected. Specifically, we identify other important impacts including loss of work, increased use of over-the-counter medication and loss of income, all of which could differentially affect low-income households or individuals with part-time or by-the-hour employment. This represents an important area of investigation.
Time spent waiting, and perceived acceptability of wait times, clearly emerged as important covariates. These results support the impact of longer wait times on patients and their families, as reported previously (Chen et al. 2008; Kulkarni et al. 2009; Lynch et al. 2008; Sanmartin et al. 2007). As well, those who had visited the specialist already – versus those still waiting – were much less likely to report that their lives were affected. On the one hand, this result may indicate some recall bias in the population who had already visited the specialist. That is, these respondents may not recall the ways in which their lives were affected, whereas those still waiting could have been more apt to articulate the specific ways in which their life was currently being affected. On the other hand, this result speaks to the importance of ensuring timely access to specialists.
People who found their wait times to be unacceptable were more than 11 times as likely to report that their life was affected. Previous work has suggested that impacts on patients' lives are primary determinants of perceived acceptability of wait times (Sanmartin et al. 2007). We suggest that the direction of this relationship remains ambiguous. Is it more likely that people who consider their wait time unacceptable have experienced related secondary impacts? Or, alternatively, that those who have experienced secondary impacts on their life consider their wait time unacceptable? At this time, it is impossible to comment definitively on the nature of this relationship. Deeper investigation into the relationship between these highly correlated variables presents an opportunity for future research.
Given that older people are more likely to access specialist care, have multiple specialists and experience more barriers to access (Chan and Austin 2008; Hopley et al. 2009), the relationship with age might seem counter-intuitive, though previous research has reported that older individuals are less likely to complain about quality of care than their younger counterparts (e.g., Bismark et al. 2006). This result may reflect the fact that the specialist visits examined here were limited to new conditions. In this case, those in the middle-age range could be accessing specialist care for the first time in their lives and thus may perceive the time spent waiting to have greater impacts. Another possible interpretation is that middle-aged respondents are more likely to be in the workforce, more sensitive to time issues (e.g., taking time off work to see a specialist) and therefore, more sensitive to waiting to see a specialist, in contrast to older individuals, who are more likely to be retired and have more flexible schedules. Older individuals, alternatively, may have more experience with accessing healthcare in general and specialty care in particular. This may attenuate older patients' perceptions of the impact on their lives, as the result could reflect the expectation that there will be at least some time spent waiting to access care.
The relationship with the sex of respondents may reflect the difference in average wait times between men and women (Thind et al. 2012) or differences in type of specialist care needed. Indeed, women have been found to have significantly longer wait times than men with respect to specialist consultations (Carrière and Sanmartin 2010), increasing the potential for impact on their lives.
Respondents who had been living in Canada for less than 10 years were almost twice as likely as Canadian-born respondents to report that their lives had been affected by wait times. There is growing evidence that newcomers face unique difficulties in accessing primary care upon arrival (Asanin and Wilson 2008; Harrington et al. 2012; Sanmartin and Ross 2006). The results suggest that waiting for access to specialist care also affects this population more severely. We suggest two possible explanations. First, recent immigrants are more likely to experience difficulties negotiating the healthcare system in Canada upon arrival because of language barriers, cultural differences and a lack of information about or familiarity with the administrative processes inherent in accessing care (Leclere et al. 1994). Access to specialist care may present additional difficulties and therefore have a greater impact on patients' lives. Alternatively, this is an important finding in the context of the “healthy immigrant effect,” a theory that suggests that upon arrival to a host country, immigrants typically enjoy better health than the general population, particularly with respect to chronic conditions. These rates tend to converge with those of the host country following an acculturation period of 10 years (Newbold 2005). Thus, during an immigrant's first 10 years in Canada, specialist consultations are more likely for acute conditions that require more urgent care (e.g., orthopaedic surgery to repair skeletal damage) than for chronic conditions such as cardiovascular disease or cancer. The increased impacts reported by this population, then, may reflect the types of specialist care that newcomers access relative to the Canadian-born population. However, as analysis by type of specialist was not available using the CCHS public use file, we cannot comment on this difference with certainty.
Respondents with secondary school education were more likely to report that their lives had been affected. Education has been inversely related to access to primary care (Hendryx et al. 2002), though the results found here might perhaps be linked to a difference in perceived expectations of the healthcare system. Sanmartin and colleagues (2007) reported that those without a secondary school education were almost half as likely as those with higher levels of education to report that wait times for specialist visits were unacceptable. Income was inversely related to impact on life, with those with household incomes in the lowest quintile the most likely to report that their lives had been affected. The suggestion that secondary health impacts of wait times are socio-economically inequitable runs counter to previous studies that have found no socio-economic differences with respect to the length of time spent waiting (Sanmartin et al. 2006; Thind et al. 2012). Thus, despite the importance of the Canada Health Act for removing direct financial barriers to accessing medically necessary specialist services, our results provide evidence to suggest that time spent waiting for specialist care may be particularly burdensome for low-income individuals and their families.
The findings on education level and income might represent two sets of social processes operating in opposite directions. Education and employment status are closely associated. More highly educated individuals who are more likely to hold higher-status employment might be more time-sensitive than individuals who are less educated and in lower-status employment, underemployed or unemployed. On the other hand, those in the lowest income quintile are more likely to be in poor health, need specialist care and therefore be more time-sensitive to wait times.
Those in poorer health were more likely to report that their life had been affected. These results suggest that those accessing the healthcare system at a higher frequency are affected more by wait times than the general population. Though previous work has found no differences in wait times for those with chronic conditions and time spent waiting in Canada (Ho and Morris 2008), similar to the experience of the low-income population, there are inequities in the ways in which these wait times affect the lives of Ontario's sickest individuals.
Limitations
Our results need to be interpreted in the context of some of the limitations of the research. CCHS is a cross-sectional survey, and as such the direction or the changing intensity of the causal relationships over time cannot be determined. The data do not allow for analysis of someone who sees multiple specialists or how waiting between specialist visits affects everyday life. Nor do the categories of how life is affected provide any sense of how everyday life is affected experientially. Dealing with these issues requires longitudinal data that would combine the timeliness of administrative data with the health, health behaviours and healthcare use data of surveys such as CCHS and qualitative studies to analyze how wait times affect everyday life. Secondly, the CCHS is based on self-reported measures and may be subject to recall bias. Third, wait times and perceived impacts may vary by type of health condition being addressed. It is possible that impacts may be greater for life-threatening conditions (e.g., cancer) versus those that are less serious (e.g., a skin condition). Fourth, the analysis does not take into account the availability of specialists within local communities.
Finally, for the 2010 cycle of the CCHS, questions specific to access to specialist healthcare services were optional content, which only the province of Ontario chose to have administered. Though these data have yielded important knowledge with respect to access to specialist services in Ontario, it is impossible to generalize these findings to the national level. This limitation highlights the importance of continued routine collection of population-level data related to access to specialist healthcare across Canada. In the context of an aging Canadian population that will likely increase the demand for specialist services, it will be increasingly important to understand issues related to access, barriers to specialist services and wait times for specialist care, and how these change over time. The CCHS is an ideal tool for ensuring these data are available and can be analyzed towards improving healthcare delivery in Canada only if the questions on access to specialist care are made part of the core content and asked in every part of Canada.
Conclusions
This research makes an important contribution to understanding access to specialist care in Ontario. While previous work has suggested that inequalities in wait times are limited, it is clear from our research that the impacts of these wait times are in some ways inequitable, i.e., there is clear evidence that the lives of some populations are affected more by wait times than others.
Though wait times are, and should continue to be, related to urgency of care, the differential impacts on the health and well-being of these groups warrant consideration from a policy perspective. We echo the recommendations forwarded by others in the Canadian context (e.g., Sanmartin et al. 2007) that in addition to continuing efforts to reduce wait times, policy actions aimed at attenuating these impacts for vulnerable groups may contribute positively to patient health and quality of life, and overall satisfaction with the healthcare system. Potential interventions could include procedures for monitoring and responding to impacts on patients' health throughout the time spent waiting for contact with a specialist. Consistent communication with those waiting to see a specialist could also help to draw together patient expectations of the healthcare system with the realities of providing timely access to care, potentially curtailing patients' perceptions of the impacts of wait times.
The federal, provincial and territorial governments of Canada have made the reductions in waiting times for all health services a priority (Health Canada 2006). Reducing waiting times is illusory if it also means growing inequities related to the impacts of wait times on Canadians depending on age, sex, socio-economic status, citizenship or health need. This research reminds us of the complexities in achieving both efficiency (with respect to effort, time and cost) and equity in the Canadian healthcare system.
Contributor Information
Daniel W. Harrington, Department of Geography, Queen's University Kingston, ON.
Kathi Wilson, Department of Geography, University of Toronto Mississauga Mississauga, ON.
Mark W. Rosenberg, Department of Geography, Queen's University Kingston, ON.
References
- Aday L.A., Andersen R. 1974. “A Framework for the Study of Access to Medical Care.” Health Services Research 9: 208–20. [PMC free article] [PubMed] [Google Scholar]
- Asanin J., Wilson K. 2008. “‘I Spent Nine Years Looking for a Doctor’: Exploring Access to Health Care among Immigrants in Mississauga, Ontario, Canada.” Social Science and Medicine 66(6): 1271–83. [DOI] [PubMed] [Google Scholar]
- Barua B., Esmail N. 2012. “Waiting Your Turn: Wait Times for Health Care in Canada.” Retrieved April 3, 2014. <http://www.fraserinstitute.org/research-news/research/publications/Waiting-Your-Turn-Wait-Times-for-Healthcare-in-Canada,-2013-Report/>. [Google Scholar]
- Bichel A., Erfle S., Wiebe V., Axelrod D., Conly J. 2009. “Improving Patient Access to Medical Services: Preventing the Patient from Being Lost in Translation.” Healthcare Quarterly 13 (Special Issue 1): 61–68. [DOI] [PubMed] [Google Scholar]
- Bismark M.M., Brennan T.A., Paterson R.J., Davis P.B., Studdert D.M. 2006. “Relationship between Complaints and Quality of Care in New Zealand: A Descriptive Analysis of Complainants and Non-Complainants Following Adverse Events.” Quality and Safety in Health Care 15(1): 17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canada Health Act. 1985. RSC, 1985, c. C-6. [Google Scholar]
- Carrière G., Sanmartin C. 2010. “Waiting Time for Medical Specialist Consultations in Canada, 2007.” Cat. no. 82-003-X. Ottawa: Statistics Canada; Retrieved April 3, 2014. <http://www.statcan.gc.ca/pub/82-003-x/2010002/article/11144-eng.pdf>. [PubMed] [Google Scholar]
- Chen Z., King W., Pearcey R., Kerba M., Mackillop M.J. 2008. “The Relationship between Waiting Time for Radiotherapy and Clinical Outcomes: A Systematic Review of the Literature.” Radiotherapy and Oncology 87: 3–16. [DOI] [PubMed] [Google Scholar]
- Dunlop S., Coyte P.C., McIsaac W. 2000. “Socio-Economic Status and the Utilization of Physicians' Services: Results from the Canadian National Population Health Survey.” Social Science and Medicine 51: 123–33. [DOI] [PubMed] [Google Scholar]
- Harrington D.W., Wilson K., Bell S., Muhajarine N., Ruthart J. 2012. “Realizing Neighbourhood Potential? The Role of the Availability of Health Care Services on Contact with a Primary Care Physician.” Health and Place 18: 814–23. [DOI] [PubMed] [Google Scholar]
- Harrington D.W., Wilson K., Rosenberg M., Bell S. 2013. “Access Granted! Barriers Endure: Determinants of Difficulties Accessing Specialist Care When Required in Ontario, Canada.” BMC Health Services Research 13: 146. 10.1186/1472-6963-13-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Canada. 2006. “A 10-Year Plan to Strengthen Health Care.” Retrieved April 3, 2014. <http://www.hc-sc.gc.ca/hcs-sss/delivery-prestation/fptcollab/2004-fmm-rpm/index-eng.php>. [Google Scholar]
- Health Council of Canada. 2010. “How Do Canadians Rate the Health Care System? Results from the 2010 Commonwealth Fund International Health Policy Survey.” Canadian Health Care Matters – Bulletin 4. Retrieved April 3, 2014. <http://publications.gc.ca/collections/collection_2011/ccs-hcc/H173-1-4-2010-eng.pdf>. [Google Scholar]
- Hendryx M.S., Ahern M.M., Lovrich N.P., McCurdy A.H. 2002. “Access to Health Care and Community Social Capital.” Health Services Research 37(1): 85–101. [PubMed] [Google Scholar]
- Ho T., Morris K. 2008. “Canadians with Health Problems: Their Use of Specialized Services and Their Waiting Experiences.” Healthcare Policy 4(1): 51–58. [PMC free article] [PubMed] [Google Scholar]
- Hopley M., Horsburgh M., Peri K. 2009. “Barriers to Accessing Specialist Care for Older People with Chronic Obstructive Pulmonary Disease in Rural New Zealand.” Journal of Primary Health Care 1(3): 207–14. [PubMed] [Google Scholar]
- Kulkarni G.S., Urbach D.R., Austin P.C., Fleshner N.E., Laupacis A. 2009. “Longer Wait Times Increase Overall Mortality in Patients with Bladder Cancer.” Journal of Urology 182: 1318–24. [DOI] [PubMed] [Google Scholar]
- Leclere F.B., Jensen L., Biddlecom A.E. 1994. “Health Care Utilization, Family Context and Adaptation among Immigrants to the United States.” Journal of Health and Social Behavior 35(4): 370–84. [PubMed] [Google Scholar]
- Liddy C., Rowan M.S., Afkham A., Maranger J., Keely E. 2013. “Building Access to Specialist Care through e-Consultation.” Open Medicine 7(1) Retrieved April 3, 2014. <http://www.openmedicine.ca/article/view/551>. [PMC free article] [PubMed] [Google Scholar]
- Lynch M.E., Campbell F., Clark A.J., Dunbar M.J., Goldstein D., Peng P. et al. 2008. “A Systematic Review of the Effect of Waiting for Treatment for Chronic Pain.” Pain 136: 97–116. [DOI] [PubMed] [Google Scholar]
- Newbold K.B. 2005. “Self-Rated Health Within the Canadian Immigrant Population: Risk and the Healthy Immigrant Effect.” Social Science and Medicine 60: 1359–70. [DOI] [PubMed] [Google Scholar]
- Organisation for Economic Co-operation and Development (OECD). 1994. “Creating Rural Indicators for Shaping Territorial Policy.” Paris: Author. [Google Scholar]
- Sanmartin C., Berthelot J.-M., McIntosh C.N. 2007. “Determinants of Unacceptable Waiting Times for Specialized Services in Canada.” Healthcare Policy 2(3): e140–54. [PMC free article] [PubMed] [Google Scholar]
- Sanmartin C., Gendron F., Berthelot J.M., Murphy K. 2004. “Access to Health Care Services in Canada, 2003.” Cat. no. 82-575-XIE. Ottawa: Statistics Canada; Retrieved April 3, 2014. <http://publications.gc.ca/Collection/ Statcan/82-575-X/82-575-XIE2003001.pdf>. [Google Scholar]
- Sanmartin C., Pierre F., Tremblay S. 2006. “Waiting for Care in Canada: Findings from the Health Services Access Survey.” Healthcare Policy 2(2): 43–51. [PMC free article] [PubMed] [Google Scholar]
- Sanmartin C., Ross N. 2006. “Experiencing Difficulties Accessing First-Contact Health Services in Canada.” Healthcare Policy 1(2): 103–9. [PMC free article] [PubMed] [Google Scholar]
- Schoen C., Osborn R., Doty M.M., Squires D., Peugh J., Applebaum S. 2009. “A Survey of Primary Care Physicians in 11 Countries, 2009: Perspectives on Care, Cost and Experiences.” Health Affairs 28(6): w1171–83. Retrieved April 3, 2014. <http://content.healthaffairs.org/content/28/6/w1171.full>. [DOI] [PubMed] [Google Scholar]
- Statistics Canada. 2012. Canadian Community Health Survey – Annual Component (CCHS). Retrieved April 3, 2014. <http://www23.statcan.gc.ca/imdb-bmdi/instrument/3226_Q1_V9-eng.pdf>. [Google Scholar]
- The R Project for Statistical Computing. 2013. R (version 2.15.1). Retrieved April 3, 2014. <http://www.r-project.org>. [Google Scholar]
- Thind A., Stewart M., Manuel D., Freeman T., Terry A. 2012. “What Are Wait Times to See a Specialist? An Analysis of 26,942 Referrals in Southwestern Ontario.” Healthcare Policy 8(1): 80–91. [PMC free article] [PubMed] [Google Scholar]
- Wilson K., Rosenberg M.W. 2004. “Accessibility and the Canadian Health Care System: Squaring Perceptions and Realities.” Health Policy 67(2): 137–48. [DOI] [PubMed] [Google Scholar]


