Abstract
Objective. To evaluate an interprofessional peer-teaching activity during which physical therapy students instructed undergraduate pharmacy students on 3 ambulatory devices (canes, crutches, walkers).
Design. The pre/post evaluation of 2 pharmacy undergraduate classes included 220 students, 110 per year. After pharmacy students completed a 10-point, knowledge-based pretest, they participated in a hands-on activity with physical therapy students teaching them about sizing, use, and safety of canes, crutches, and walkers. A 10-point posttest was completed immediately afterward.
Assessment. The mean difference of pre/post scores was 3.5 (SD 1.9) for the peer-led teaching, and 3.8 (SD 2.2) for the peer learning group. Students had positive responses regarding the learning exercise and recommended further peer teaching.
Conclusion. The peer-learning activity involving physical therapy students teaching pharmacy students was an effective method of improving knowledge and skills regarding basic ambulatory devices.
Keywords: pharmacy, physical therapy, peer teaching, ambulatory assistive devices, orthopaedic equipment
INTRODUCTION
Pharmacists frequently practice in collaboration with other health professionals, or within multi-disciplinary teams. Interprofessional collaboration within a patient-centered team builds on each member’s professional skills to ensure quality of patient care. To address this professional expectation, interprofessional education has been adopted as an essential element of the education and training of health professionals, prior to entering practice.1 Because of this clinical focus, interprofessional education is of particular interest for curriculum reform in health-care education2 and should be introduced early within training, before negative attitudes can develop,2 and revisited throughout the curriculum.3
According to Reiser, interprofessional and peer interaction should be part of the health professional’s career, and these types of activities should be embedded to ensure continued ethical practice.4 The goal of interprofessional education is not simply efficiency in teaching similar concepts to larger groups of students, but to enhance self-knowledge, communication skills, conflict management, and the ability to work in a team.3,5
A clinical attribute of working within a multi-disciplinary team is peer teaching. Although peer teaching is a widely acceptable approach for the practitioner, peer teaching at the trainee or student level is less commonly embraced. Peer teaching is an alternate approach to didactic instruction. Instead of professors presenting to students, it typically involves other students in the same or adjacent year of a program leading the teaching activity. Near-peers, defined by Evans and colleagues, are from 2 to 5 years ahead in the training program.6 Peer teaching can improve theoretical knowledge and practical skills in higher level education.7
Although examples of peer teaching within health professions are documented,8-10 student peer teaching across health disciplines is less commonly reported. We had an opportunity to examine peer teaching with pharmacy and physical therapy students. This opportunity arose from a survey sent to almost 4000 pharmacists in the Canadian province of Alberta. The survey revealed that knowledge and confidence in the use and fitting of ambulatory assistive devices (AAD) were quite low.11 Although retail of such devices is common in pharmacies, 45% of pharmacists in Alberta reported they had no training in fitting or instruction of canes, crutches, or walkers.11 These basic devices are commonly stocked in community pharmacies and can be sold or rented without assessment by a physical therapist or physician.
An estimated 540 000 Canadians use AAD including braces, crutches, or canes.12 Thirty-two percent of adults older than 85 reported the use of mobility support devices, and 96% of those said a disability was the reason. Because of the aging population, a greater number of older adults will likely go to pharmacies to purchase AAD. However, assistive devices are not only for older adults; injuries account for 55%-60% of people aged 12-44 years who require assistive devices because of an illness or disease.12 Thus, pharmacists have an opportunity within this population to educate and potentially improve patient-care outcomes.
To address this learning need at an undergraduate level, we developed and implemented an AAD peer-teaching module taught to undergraduate pharmacy students by master’s-entry physical therapy students. The objective was to determine whether peer teaching was an effective method of teaching AAD to undergraduate pharmacy students. A secondary objective was to evaluate students’ attitudes before and after the activity. To our knowledge, no peer teaching across physical therapy and pharmacy has been implemented or evaluated.
DESIGN
A pre/post evaluation of the interprofessional peer teaching module was administered in the third year of the undergraduate pharmacy program and the second year of a 26-month graduate physical therapy program. The evaluation looked at the implementation of the laboratory activity over 2 years with 2 different cohorts. Ethics approval for this project was obtained through the University of Alberta Health Research Ethics Board.
To plan the 3-hour laboratory activity between 2 programs, a common time within complementary courses was identified. In the Faculty of Pharmacy and Pharmaceutical Sciences, a modular curriculum is used, and in the third year of the program, the bone and joint module was chosen to implement the AAD laboratory activity. Pharmacy admits approximately 130 undergraduate students to its 4-year undergraduate program each year.
The learning objectives of the laboratory activity for the pharmacy students were to understand and demonstrate proper selection, fitting, and safety of canes, crutches, and walkers, which are typical AAD sold in community pharmacies. Students were aware that the material covered would be integrated into their cumulative year-end objective structured clinical examination (OSCE), and the material covered in the exercise was covered on the bone and joint module’s final examination.
Within the Department of Physical Therapy, Faculty of Rehabilitation Medicine, students learn AAD skills in the first year of their master’s entry program and then use those skills within subsequent clinical practice experiences. Approximately 80 students are admitted to the physical therapy graduate program each year. The peer teaching module with pharmacy students was implemented in a second-year physical therapy course looking at professional behaviour. The interprofessional activity was designed as a laboratory assignment to implement interaction with other allied health professions.
The activity required the 2 course instructors to discuss learning objectives of the activity for both professions, teaching content, and logistical issues. The teaching content consisted of similar online module created for continuing education of ADD for pharmacists.11 We also ensured that peer-teaching activity took no additional time in the module compared to formal teaching, meaning no additional burden on students. Although total laboratory time was 3 hours, the activity time for each group was 45 minutes.
These activities were supported by tenure and clinical track faculty members and support staff. We designated faculty “champions” to ensure the activity was conducted consistently year to year to ensure that administrative/scheduling challenges were overcome, and to advocate for the teaching activity. Administratively, a number of meetings were held to prepare for implementation, to ensure teaching quality, and to ensure that curricular outcomes and course/module objectives were addressed for both disciplines.
In the first year of the study, each small group consisting of 10-12 pharmacy students was led by either a physical therapy or an occupation therapy student. Unlike a seminar group, which discusses previously taught didactic material, the peer leaders provided instruction on new material not presented in earlier instructor-led classes. The physical therapy students volunteered to participate. These students met with the investigators to review the prepared handout materials and ensure that all materials would be consistently presented. Approximately 20 minutes were allotted for demonstration, instruction, and practice on canes, crutches, and walkers (total teaching time 60 minutes) and 15 minutes each for the pre/post examinations.
In the second year of the study, we decided the peer learning should be a student learning group activity7 so that more physical therapy students could be involved. Thus, the activity became a required course activity for physical therapy and pharmacy students. Groups of 2-3 physical therapy students were assigned to teach 3-4 pharmacy students at a time. Before the activity, each group of physical therapy students drafted a teaching plan and handout, which was reviewed by the physical therapy course instructor, who evaluated it for content and format.
The best designed handout, as decided by the instructor, was selected to be used by all the groups for the activity. The physical therapy written assignment was designed to ensure that standardized content was being taught during the activity. Each assistive device was introduced by describing the devices and providing instruction on sizing, safety, and use. Pharmacy students practiced using the devices, with feedback and correction offered by the physical therapy students.
Pharmacy students completed a 10-question multiple-choice test before the activity. The questions were case-based and collected the students’ knowledge of canes, crutches, and walkers. Additional questions were asked about demographic background, experience, and beliefs about pharmacists’ role in AAD fitting and counseling. After the laboratory, a posttest was administered to test knowledge and beliefs. The knowledge-based questions and those involving beliefs were the same for the pretest and posttest. However, they were re-ordered to discourage recall. Of the 10 knowledge-based questions administered, 3 questions concerned use of AAD, 3 dealt with sizing of specific AAD, 2 focused on safety, and 2 dealt with device prescriptions. All questions were framed within clinical scenarios. To examine whether the 2 delivery modes of instruction—peer-led teaching and peer learning groups—were effective in improving students’ test scores, these tests were given in person immediately before and after the session.
Summary statistics were used to describe the characteristics of the students and to assess whether students in the 2 cohorts were comparable in terms of their demographic backgrounds. We conducted independent-samples t tests on demographic features such as age and numbers of years in university. To examine the change over time within each cohort, pre- and postinstructional sessions were examined using a paired t test. Group differences of the 2 cohorts on their baseline test scores and posttest scores were examined using independent t tests. We also assessed whether or not 2 delivery modes generated equal or comparable improvements in test scores, to determine whether both methods improved students’ learning. To quantify the change over time, standardized effect sizes were calculated subtracting the prescore from the postscore using the baseline standard deviation. A positive value for the effect size indicated improvement over the time interval, whereas a negative value indicated deterioration. To further evaluate whether the 2 modes yielded the same improvement, a 2 (instruction modes) by 2 (pretest and postscores) analysis of variance (ANOVA) was conducted. All statistical testing was performed with 2-tailed tests and at a 0.05 level of significance unless otherwise stated. Statistical analyses were performed using SPSS, v22 (IBM, Armonk, NY).
EVALUATION AND ASSESSMENT
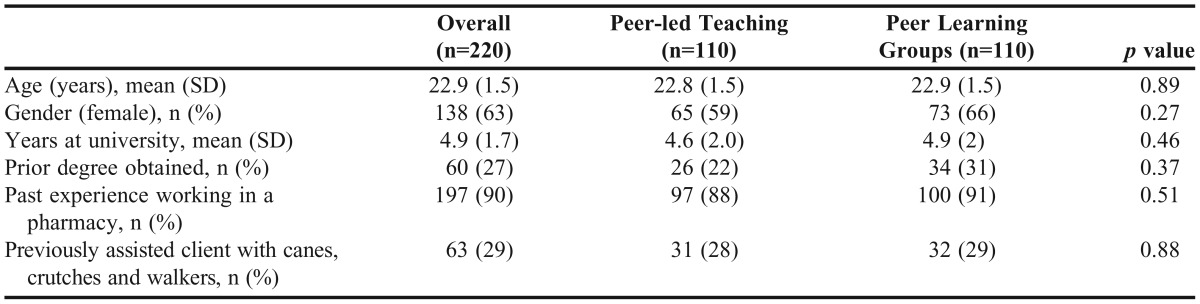
Of the 220 pharmacy students who consented to participate in the evaluation of this activity, 110 students received teaching assistant-led instruction, and 110 received a student peer learning group method of instruction. Participant characteristics are in Table 1. The majority were female (138; 63%). Sixty (27%) had received other undergraduate degrees before their pharmacy program. No significant group differences (p>0.05) were seen between the 2 cohorts in terms of demographic and educational experience.
Table 1.
Characteristics of Pharmacy Student in the Interprofessional Peer-teaching Activity
A 2-way mixed ANOVA (between subjects: cohort; within subjects: pre/post) was performed to examine the effects of cohort and pre/post improvement on test performance. No significant interaction between cohort and pre/post was found to predict examination scores (p>0.05), meaning that the pre/post improvements were consistent between the peer-led teaching and peer learning cohorts. Hence, we could examine the effect of teaching cohort on pretest and posttest scores, respectively. The peer-led teaching cohort had a mean pretest score of 3.5 (SD 1.5), which was not significantly different from the peer learning group (2.7; SD 1.4) (p>0.05).
The peer-led teaching cohort mean postscore improved to 7.1 (SD 1.3) (p<0.01), which was not different from the peer learning group mean postscore 6.4 (SD 1.8). The mean difference in pre/post scores for the peer-led teaching cohort was 3.5 (SD 1.9), and 3.8 (SD 2.2) for the peer earning group. These differences did not differ significantly (p>0.05). Both cohorts showed improvement in scores after the instructional session, with effect sizes of 2.56 for the peer-led teaching cohort, and 2.34 for the peer learning group cohort, which is considered a large effect size, according to Cohen’s standards.13 Questions that dealt with cane use and sizing were commonly answered incorrectly in the pretest and posttest. However, questions that dealt with referral to physical therapists and/or physicians were answered correctly for both tests. No students received a perfect pretest score, although 4.5% (n=10) did not supply any correct answers. Twelve (10.9%) students in the peer-led teaching cohort and 8.2% (n=9) of students in the peer learning group obtained a perfect posttest score. Improvements appear to be identical for the 2 peer instructional modes. The interaction effect of the ANOVA indicated a nonsignificant difference between the 2 groups (p=0.21).
In the pretest, most (99%) pharmacy students stated that pharmacists should be involved in assisting customers with AAD. Using a 7-point Likert scale (1=very uncertain, and 7=very certain), students were asked about their confidence in assisting customers with canes, crutches, and walkers before and after the activity. The mean score in confidence was 1.8 prior to the activity, with a mean increase of 3.5 points after the activity.
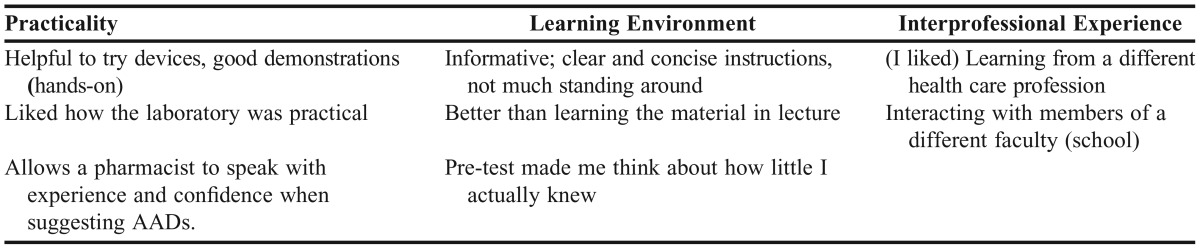
In addition to analyzing test scores, we asked students to comment on the learning activity. Students provided reflective comments, specifically around 3 themes: interprofessional experience, learning environment, and practicality of the activity and information. Representative comments are included in Table 2. In addition, students provided comments on improvements that could be made to the activity. Suggestions for improvements centered on facilities (eg, less noise—other groups talking made it hard to hear instructor), expanding the material covered (eg, more types of AADs), and having pharmacy students provide a reciprocal teaching experience.
Table 2.
Representative Comments from Pharmacy Students Regarding the Interprofessional Peer-teaching Activity
DISCUSSION
Interdisciplinary peer teaching led by physical therapy students for pharmacy students was an effective method of teaching AAD. Pharmacy students were able to learn and demonstrate skills related to AAD as effectively from physical therapy student peer learning groups as they were from a peer led teaching setting. Baseline knowledge of AAD was especially weak for the pharmacy students and revealed the need for educational activities to prepare students for professional practice. Improvement regardless of pretest score was noted in the posttest scores with both modes of instruction. However, no comparison was made to traditional didactic lecturing.
Our earlier survey of practicing pharmacists revealed that only a small minority received formal training with AAD during their undergraduate years.11 Not only did the pharmacy students learn about AAD, the activity was viewed as a positive learning experience. Other studies found that some peer-teaching activities led to higher scores than faculty-taught sessions, although methodological quality of some studies were variable.8,14
Unlike other peer-teaching activities within the same profession, this peer-teaching activity crossed disciplines. The interprofessional collaboration with master’s entry-level physical therapy students was initiated because these students are taught in their first year of study the prescription, use, fitting, and safety of AAD. An earlier survey of Alberta pharmacists reported that the majority of pharmacists believed it was their role to assist clients with AAD.11 However, they did not receive formal instruction on use, fitting, and safety of AAD during their undergraduate pharmacy training. Having physical therapy students instruct pharmacy students allowed both groups to learn: physical therapy students in terms of providing an instructional lesson plan and pharmacy students in terms of acquiring new clinical knowledge.
For physical therapy students, peer teaching was a valuable experience because it enhanced the their identity as teachers and expanded the collaboration and team activity typically seen in health care.15 Physical therapy students provided feedback on their experience through course evaluations. Informally, the students reported positive reinforcement of their teaching ability and were satisfied with the experience. Within a clinical team, health professionals are called upon to teach other team members, the patient, and family. This experience provided an opportunity for the physical therapy students to view themselves as teachers, with authority on a subject.16
This interprofessional activity also gave students an appreciation for other health disciplines and an opportunity to demonstrate team care. Students valued the opportunity to learn or relearn the material, “give back” to the classroom, and enjoy developing leadership skills.16,17 Educational skills should be enhanced throughout the curriculum in all the health disciplines, as peer and team education will be part of professional practice.
The benefits of interprofessional activities at the student level can be that students develop friendships that extend beyond the classroom, and live by the mantra “you do like me, so you will respect my profession.”2 Reiser described these types of interactions as foreshadowing how individuals will behave in practice in the future.4
Smaller studies of peer teaching showed attitudes toward peer teachers varied.18,19 Interprofessional activities can produce negative experiences difficult to counteract later in education or professional practice.20 In contrast, pharmacy students in our study reported the activity was rewarding, challenging, and that they appreciated the interaction with physical therapy students. Our findings showed that students can learn about AAD from other students and also about the other profession and how to liaise in a professional setting.
Some interprofessional peer teaching activities have been described.21-24 In the multi-center study by Lai and colleagues, pharmacy students presented lectures on Medicare Part D to health professionals and students in nursing and medicine.24 The pharmacy students were selected competitively, rather than having all pharmacy students participate. Similar to our findings, the overall self-rated knowledge improved, and perception and attitudes toward pharmacists and their role increased, especially in relation to intended collaboration.24
Peer teaching is successful in increasing knowledge and skills, partly because there is social congruence (students can relate to the struggles and challenges of other students), and cognitive congruence (students can explain concepts at the appropriate level).17 While there may be some concern that faculty members have greater knowledge and expertise, and, therefore, would do a superior job of transferring the information, the social and cognitive congruence of a peer teachers compensates for this. Students are better cognitive matches when explaining the “basics,” compared to faculty members, who students can perceive as overestimating student knowledge regarding basic concepts.17
The success of this activity also may be a result of its student-centered design, as it required the students to take an active role in the learning, and shifted the responsibility of organizing and synthesizing the content from professor to student.25 Lockspeiser recommended early introduction of peer teaching, as it was an opportunity for students to experience empathy during a challenging educational experience, especially early in the academic career when transitions occur.17
Organized and supervised peer teaching may reduce some time or resource demands of faculty members, who can shift that time to administrative tasks related to the teaching activity.14 Although Glynn and colleagues suggested using peer-assisted learning as a means of addressing resource shortages, the time demands on faculty members may not change.26,27 No matter the time demands, the role of faculty member moves from information dissemination to process design and management.27 The faculty member also has an important role to ensure the environment is safe, as some student-led activities may be viewed as threatening.26,28
There are challenges to implementing curriculum change, including preconceptions of faculty members, student expectations, infrastructure, and the institutional environment. We ensured that we provided more than a “gilding of interdisciplinarity,” and worked within the curriculum structures of both faculties (schools), not waiting for curriculum or departmental reforms, or an ideal curriculum to work with.29 These sessions demonstrated that collaboration between disciplines can provide structured and effective learning experiences for students without being offered as an elective or extracurricular activity.
The clinically relevant topic of AAD is a basic, core knowledge for physical therapy students, so significant training or teaching was not necessary to teach this skill. The greatest challenge was scheduling (finding time when the physical therapy and pharmacy students could be scheduled together), and facilities (ensuring adequate numbers of AAD were available and a large enough room could be booked for all the students at one time). The teacher and learner role should be evaluated in peer-teaching activities to ensure that both parties are benefiting from the experience.
The success of the educational activity is evidenced by its full integration as a standard part of the undergraduate curriculum for pharmacy students at the University of Alberta. Physical therapy students continue to provide learning materials and act as peer teachers as a required part of their curriculum. Peer teaching activities by pharmacy students to physical therapy students are being developed, focusing on inhaler devices, pain management, and NSAIDs. Evaluation of these exercises is planned.
SUMMARY
Pharmacy students can effectively learn about canes, crutches, and walkers from their peers in physical therapy through interprofessional peer teaching, whether delivered as peer-led teaching or peer learning. Students enjoyed the interprofessional peer teaching, and it was effectively implemented with adequate support, leadership, and planning. Peer teaching across disciplines is a supportive activity that helps prepare students to become active members within multidisciplinary health care teams.
REFERENCES
- 1.Hammick M. Interprofessional education: evidence from the past to guide the future. Med Teach. 2000;22:461–467. doi: 10.1080/01421590050110713. [DOI] [PubMed] [Google Scholar]
- 2.Hoffman SJ, Rosenfield D, Gilbert JH, Oandasan IF. Student leadership in interprofessional education: benefits, challenges and implications for educators, researchers and policymakers. Med Educ. 2008;42:654–661. doi: 10.1111/j.1365-2923.2008.03042.x. [DOI] [PubMed] [Google Scholar]
- 3.Areskog NH. The need for multiprofessional health education in undergraduate studies. Med Educ. 1988;22:251–252. doi: 10.1111/j.1365-2923.1988.tb00749.x. [DOI] [PubMed] [Google Scholar]
- 4.Reiser SJ. The ethics of learning and teaching medicine. Acad Med. 1994;69:872–876. doi: 10.1097/00001888-199411000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Castro RM. Defining, supporting, and maintaining interprofessional education. J Educ Policy. 1993;8:153–155. [Google Scholar]
- 6.Evans DJR, Cuffe T. Near-peer teaching in anatomy: an approach for deeper learning. Anatomical Sci Educ. 2009;2:227. doi: 10.1002/ase.110. [DOI] [PubMed] [Google Scholar]
- 7.Goldschmid B, Goldschmid ML. Peer Teaching in Higher Education: A Review. Higher Educ. 1976;33 [Google Scholar]
- 8.El-Sayed SH, Gouda Metwally F, Abdeen Abdeen M. Effect of peer teaching on the performance of undergraduate nursing students enrolled in nursing administration course. J Nurs Educ Practice. 2013;3:156–166. [Google Scholar]
- 9.Atayee RS, Singh RF, Best BM, Freedman BA, Morello CM. An active-learning assignment involving peer-to-peer presentations to improve pharmacy students: attitudes and knowledge of dietary supplements. Am J Pharm Educ. 2012;76(6) doi: 10.5688/ajpe766113. Article 113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hudson JN, Tonkin AL. Clinical skills education: outcomes of relationships between junior medical students, senior peers and simulated patients. Med Educ. 2008;42:901–908. doi: 10.1111/j.1365-2923.2008.03107.x. [DOI] [PubMed] [Google Scholar]
- 11.Lam A, Molnar R, Vu T, Sadowski CA, Jones CA. Online continuing education module for community pharmacists: assisting clients with ambulatory devices. Currents Pharm Teach Learn. 2009;1:87–92. [Google Scholar]
- 12.Shields M. Use of wheelchairs and other mobility support devices. Health Report. 2004;15:37–41. [PubMed] [Google Scholar]
- 13.Cohen J. Statistical Power Anaylsis for the Behavioral Sciences. Hillsdale, NJ: Lawerence Erlbaum Associates; 1988. [Google Scholar]
- 14.Santee J, Garavalia L. Peer tutoring programs in health professions schools. Am J Pharm Educ. 2006;70(3) doi: 10.5688/aj700370. Article 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Drew CP. Are You Spoon-Feeding Your Students? A Paper on Facilitating a Collaborative Learning Experience. Conference Proceedings. The Third Annual Conference on Student Retention in Two Year Colleges. Trenton, NJ, 1990.
- 16.Bos S. Perceived benefits of peer leadership as described by junior baccalaureate nursing students. J Nurs Educ. 1998;37:189–191. doi: 10.3928/0148-4834-19980401-13. [DOI] [PubMed] [Google Scholar]
- 17.Lockspeiser TM, O’Sullivan P, Teherani A, Muller J. Understanding the experience of being taught by peers: the value of social and cognitive congruence. Adv Health Sci Educ. 2008;13:361–12. doi: 10.1007/s10459-006-9049-8. [DOI] [PubMed] [Google Scholar]
- 18.Knobe M, Munker R, Sellei RM, et al. Peer teaching: a randomised controlled trial using student-teachers to teach musculoskeletal ultrasound. Med Educ. 2010;44:148–155. doi: 10.1111/j.1365-2923.2009.03557.x. [DOI] [PubMed] [Google Scholar]
- 19.Weidner TG, Popp JK. Peer-assisted learning and orthopaedic evaluation psychomotor skills. J Athl Train. 2007;42:113–119. [PMC free article] [PubMed] [Google Scholar]
- 20.Rosenfield D, Oandasan I, Reeves S. A participatory approach to interprofessional education research: students researching with their peers. J Interprof Care. 2009;23:676–678. doi: 10.3109/13561820802675897. [DOI] [PubMed] [Google Scholar]
- 21.Mouradian WE, Reeves A, Kim S, et al. A new oral health elective for medical students at the University of Washington. Teach Learn Med. 2006;18:336–342. doi: 10.1207/s15328015tlm1804_11. [DOI] [PubMed] [Google Scholar]
- 22.Lanning SK, Ranson SL, Willett RM. Communication skills instruction utilizing interdisciplinary peer teachers: program development and student perceptions. J Dent Educ. 2008;72:172–182. [PubMed] [Google Scholar]
- 23.Lipton HL, Lai CJ, Cutler TW, Smith AR, Stebbins MR. Peer-to-peer interprofessional health policy education for Medicare Part D. Am J Pharm Educ. 2010;74(6):102. doi: 10.5688/aj7406102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lai CJ, Smith AR, Stebbins MR, Cutler TW, Lipton HL. Promoting interprofessional collaboration: pharmacy students teaching current and future prescribers about Medicare Part D. J Manage Care Pharm. 2011;17:439–448. doi: 10.18553/jmcp.2011.17.6.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brush T, Saye J. Implementation and evaluation of a student-centered learning unit: a case study. Educ Technol Res Develop. 2000;48:79–100. [Google Scholar]
- 26.Glynn LG, MacFarlane A, Kelly M, Cantillon P, Murphy AW. Helping each other to learn – a process evaluation of peer assisted learning. BMC Med Educ. 2006;6:18. doi: 10.1186/1472-6920-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dollman J. A new peer instruction method for teaching practical skills in the health sciences: an evaluation of the “learning trail.”. Adv Health Sci Educ. 2005;10:125–128. doi: 10.1007/s10459-004-2321-x. [DOI] [PubMed] [Google Scholar]
- 28.Kommalage M, Imbulgoda N. Introduction of student-led physiology tutorial classes to a traditional curriculum. Adv Physiol Educ. 2010;34:65. doi: 10.1152/advan.00010.2010. [DOI] [PubMed] [Google Scholar]
- 29.Luckie DB, Bellon R, Sweeder RD. The BRAID: experiments in stitching together disciplines at a Big Ten university. J STEM Educ: Innov and Res. 2012;13:6–9. [Google Scholar]