Highlights
-
•
We present a case of vulva epithelioid sarcoma, and review the articles.
-
•
The rarity of this disease causes delay in diagnosis and lack of guideline for optimal treatment.
-
•
Physicians should have high suspicions in diagnosing this vulvar disease using prompt biopsy without delay.
Keywords: Vulva, Epithelioid sarcoma, Proximal, Optimal treatment, Young aged women, Prognosis
1. Introduction
Epithelioid sarcoma (ES) is a malignant soft tissue tumor. It is classified into distal or proximal types, based on its occurrence in the upper and lower extremities or in the trunk and pubic regions, respectively. Proximal-type epithelioid sarcoma (PES) of the vulva is an exceedingly rare condition. There are limited reports of this condition in the literature (Iavazzo et al., 2014, Kim et al., 2012, Patrizi et al., 2013). This disease occurs most often in women of reproductive age, and despite its low occurrence poses a significant health issue for women. Due to the rarity of this disease, the guidelines for its optimal treatment are not well established.
We are reporting a case of epithelioid sarcoma in a 32 year-old female treated with radical vulvectomy and reviewing the literature with focus on its treatment in young reproductive aged women.
2. Case report
A 32-year old African American female presented with a palpable nodule in the posterior portion of the right labia majora for 3 months. She was gravida 5 and para 2 and reported no previous gynecologic problems. Her medical history was significant for hypertension and obesity (body mass index 44). She had no personal or family history of cancer. She had seen a dermatologist for bumps on the right vertex scalp and labia majora, and onychomycosis on her left great toenail. She was referred to Gynecology with presumed diagnosis of Bartholin's cyst of right labia majora.
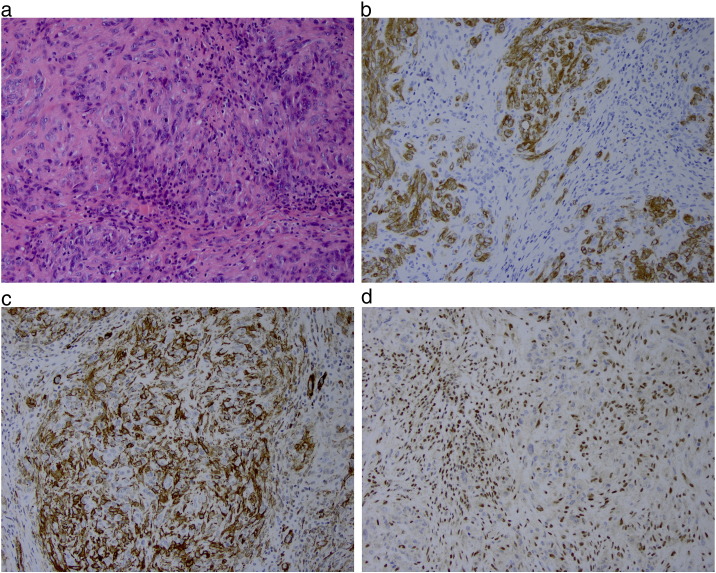
Upon examination, a 1 × 0.5 × 0.5 cm-sized, firm, superficial, and non-tender nodule was seen on the right posterior labia majora. She denied itching or irritation over the lesion. Vulvar biopsy was taken from the lesion, and pathology revealed epithelioid sarcoma with high mitotic feature extending to deep and lateral edges of excisional biopsy specimen. The tumor stained positive for AE1/AE3 and smooth muscle actin (SMA), and the stain for both S-100 and caldesmon was negative. The majority of tumor cells showed the absence of staining for integrase interactor 1 (INI1) (Fig. 1a–d). There was no lymphovascular invasion, and positron emission tomography–computed tomography (PET–CT) did not demonstrate distant metastasis.
Fig. 1.
(a) H&E, × 400, (b) positive staining for AE1/AE3, × 400, (c) positive staining for SMA, × 400, (d) Tumor cells staining negative for the INI1 compared to stromal cells staining positive, × 400.
We treated the patient with radical hemivulvectomy. Final pathology of radical vulvectomy specimen demonstrated 5 mm sized remnant tumor with superficial invasion (less than 1 mm). The margins of excision were negative.
The case was then reviewed at institutional tumor board and consensus reached after reviewing the pathology and imaging was to follow patient with close surveillance. Secondary to the small size, superficial invasion, lack of lymphovascular space invasion and no evidence of metastatic disease on imaging, inguinal lymphadenectomy was not considered necessary. Patient has since then been seen every three months and is currently well, with no evidence of disease nine months postoperatively.
3. Discussion
ES is a malignant soft tissue tumor, which was established as a distinct disease by Enzinger in 1970. The first case of PES of the vulva was described by Pier et al. in 1972 (Piver et al., 1972). PES of the vulva often occurs in the labia majora of young women, and frequently misdiagnosed as benign lesion such as Bartholin's cyst, lipoma, or genital warts. Our patient was also referred to our general gynecologic department for Bartholin's cyst management. Due to its benign appearance as a painless subcutaneous nodule, diagnosis and treatment can often be delayed significantly (Moore et al., 2002, Ulutin et al., 2003).
Microscopic appearance of PES ranges from plump spindle cells to large polygonal cells with deeply acidophilic cytoplasm. It bears a resemblance to epithelioid or squamous cells, which makes diagnosis of PES challenging. The diagnosis can only be confirmed with immunochemical staining, as lack of staining for INI1 protein is one of the characteristic findings (Kim et al., 2012).
The ideal treatment of PES remains unclear. There is no treatment of choice universally accepted for vulvar epithelioid sarcoma (Iavazzo et al., 2014). However, the cornerstone of initial management is surgical excision with a wide margin (Bos et al., 1988). The role and choice of adjuvant therapy also remain unclear owing to the rarity of disease. However, review literature by Argenta et al. reported lower recurrence rates in patients who had adjuvant radiation therapy (Argenta et al., 2007). Based on the literature, adjuvant chemotherapy does not seem to improve the outcome. However, due to the small number of cases available, it remains as an option (Altundag et al., 2004, Moore et al., 2002).
Because optimal management is not well established, our understanding of genetic pathways involved in the tumorigenesis of ES and developing target therapy might provide alternative therapeutic options. SMARCB1/IN1 gene is located at 22q11 and acts as a tumor suppressor gene. Previous studies found that inactivation of SMARCB1/IN1 played a crucial role in tumorigenesis of ES and immunochemistry studies revealed that 85 to 93% of cases have inactivated SMARCB1/IN1 (Hornick et al., 2009; Noujaim et al., 2015). Loss of expression can occur with various mechanisms such as biallelic deletion, single-allelic deletion, point mutation, or epigenetic gene silencing. Target therapy restoring SMARCB1/IN1 gene function could provide new therapy in ES.
The prognosis of ES is not favorable; the lack of symptoms belies its aggressive nature with rapid tendency of metastasis and high recurrence rate. According to previous studies, 38%–69% of patients had recurrence (Halling et al., 1996, Iavazzo et al., 2014, Ross et al., 1997). Ivasazzo et al. reviewed 28 cases PES on the vulva specifically, and reported 42% of recurrence rate with lung and lymph nodes as the most common site of recurrence (Iavazzo et al., 2014).
We analyzed 37 cases of vulva PES from 32 studies (Table S1); the mean age of patients was 38.6 ± 16.3 years (range, 17–84 years). Sixteen patients among thirty-seven patients (43.2%) had recurrence during follow-up, with a mean disease free survival time of 17.2 ± 25.2 months (range, 1–96 months). Ten among sixteen (62.5%) recurrent patients died of disease.
Because overall peak incidence of ES is around 35 years of age and the majority of vulva epithelioid sarcoma patients in previous reports were aged 35 or less (20 out of 37 patients, 54.1%), we compared these young patients with older patients in further analysis (Table S2). Seven patients aged 35 or less (7 out of 20, 38.1%) and nine patients aged 36 or more (9 out of 17, 40.5%) had recurrence. Patients who were aged 35 years or less had 26.4 ± 33.5 months of disease free survival time, whereas patients aged 36 years or more had 10.0 ± 14.7 months of disease free survival time. Three out of seven recurrent patients aged 35 or less (42.9%) died of disease while seven out of nine recurrent patients aged 36 or more (77.8%) died of disease. The mean time from recurrence to death is 15.2 ± 17.2 months in younger patients and 5.6 ± 4.5 months in older patients. This analysis suggested that younger patients might have better prognosis than older patients, but there was no statistical significance (P > 0.05).
As PES of the vulva often develops in reproductive aged women, maintenance of pregnancy and/or fertility should be considered in treating patients (Chiyoda et al., 2011, Moore et al., 2002, Rai et al., 2009). However, the clinical behavior is unfortunately not different from that of other non-pregnant patients, and can lead to a dismal outcome in an effort to avoid surgery during pregnancy (Moore et al., 2002).
As seen with our analysis, a significant amount of patients (62.5%) will die of disease if they have recurrence. Since it seems only an early diagnosis with definite surgical treatment can improve prognosis, physicians should have high suspicions in diagnosing this using prompt biopsy, especially in young women for a potentially better prognosis.
The following are the supplementary data related to this article.
Vulva epithelioid sarcomas published in the literature.
Comparisons between young and old patients in recurrent cases.
Consent
Written informed consent was obtained from the patient for publication of this case report. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Conflict of interest
There is no conflict of interest.
References
- Altundag K., Dikbas O., Oyan B., Usubutun A., Turker A. Epithelioid sarcoma of vulva: a case report and review of the literature. Med. Oncol. 2004;21:367–372. doi: 10.1385/MO:21:4:367. [DOI] [PubMed] [Google Scholar]
- Argenta P.A., Thomas S., Chura J.C. Proximal-type epithelioid sarcoma vs. malignant rhabdoid tumor of the vulva: a case report, review of the literature, and an argument for consolidation. Gynecol. Oncol. 2007;107:130–135. doi: 10.1016/j.ygyno.2007.05.045. [DOI] [PubMed] [Google Scholar]
- Bos G.D., Pritchard D.J., Reiman H.M., Dobyns J.H., Ilstrup D.M., Landon G.C. Epithelioid sarcoma. An analysis of fifty-one cases. J. Bone Joint Surg. Am. 1988;70:862–870. [PubMed] [Google Scholar]
- Chiyoda T., Ishikawa M., Nakamura M., Ogawa M., Takamatsu K. Successfully treated case of epithelioid sarcoma of the vulva. J. Obstet. Gynaecol. Res. 2011;37:1856–1859. doi: 10.1111/j.1447-0756.2011.01637.x. [DOI] [PubMed] [Google Scholar]
- Halling A.C., Wollan P.C., Pritchard D.J., Vlasak R., Nascimento A.G. Epithelioid sarcoma: a clinicopathologic review of 55 cases. Mayo Clin. Proc. 1996;71:636–642. doi: 10.1016/S0025-6196(11)63000-0. [DOI] [PubMed] [Google Scholar]
- Hornick J.L., Dal Cin P., Fletcher C.D. Loss of INI1 expression is characteristic of both conventional and proximal-type epithelioid sarcoma. Am. J. Surg. Pathol. 2009;33:542–550. doi: 10.1097/PAS.0b013e3181882c54. [DOI] [PubMed] [Google Scholar]
- Iavazzo C., Gkegkes I.D., Vrachnis N. Dilemmas in the management of patients with vulval epithelioid sarcoma: a literature review. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014;176:1–4. doi: 10.1016/j.ejogrb.2014.02.013. [DOI] [PubMed] [Google Scholar]
- Kim H.J., Kim M.H., Kwon J., Kim J.Y., Park K., Ro J.Y. Proximal-type epithelioid sarcoma of the vulva with INI1 diagnostic utility. Ann. Diagn. Pathol. 2012;16:411–415. doi: 10.1016/j.anndiagpath.2011.04.002. [DOI] [PubMed] [Google Scholar]
- Moore R.G., Steinhoff M.M., Granai C.O., DeMars L.R. Vulvar epithelioid sarcoma in pregnancy. Gynecol. Oncol. 2002;85:218–222. doi: 10.1006/gyno.2002.6610. [DOI] [PubMed] [Google Scholar]
- Noujaim J., Thway K., Bajwa Z., Bajwa A., Maki R.G., Jones R.L. Epithelioid sarcoma: opportunities for biology-driven targeted therapy. Front. Oncol. 2015;5:186. doi: 10.3389/fonc.2015.00186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrizi L., Corrado G., Saltari M., Perracchio L., Scelzo C., Piccione E. Vulvar “proximal-type” epithelioid sarcoma: report of a case and review of the literature. Diagn. Pathol. 2013;8:122. doi: 10.1186/1746-1596-8-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piver M.S., Tsukada Y., Barlow J. Epithelioid sarcoma of the vulva. Obstet. Gynecol. 1972;40:839–842. [PubMed] [Google Scholar]
- Rai H., Odunsi K., Kesterson J., Morrison C., Chan A., Mhawech-Fauceglia P. Epithelioid sarcoma of the vulva in a 17-year-old pregnant woman. Appl. Immunohistochem. Mol. Morphol. 2009;17:270–273. doi: 10.1097/PAI.0b013e31818eca8b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross H.M., Lewis J.J., Woodruff J.M., Brennan M.F. Epithelioid sarcoma: clinical behavior and prognostic factors of survival. Ann. Surg. Oncol. 1997;4:491–495. doi: 10.1007/BF02303673. [DOI] [PubMed] [Google Scholar]
- Ulutin H.C., Zellars R.C., Frassica D. Soft tissue sarcoma of the vulva: a clinical study. Int. J. Gynecol. Cancer. 2003;13:528–531. doi: 10.1046/j.1525-1438.2003.13305.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Vulva epithelioid sarcomas published in the literature.
Comparisons between young and old patients in recurrent cases.