Abstract
Introduction:
Axillary breast is a common condition that leads to discomfort and cosmetic problems. Liposuction alone and open excision are two techniques used for treatment.
Materials and Methods:
This study assesses the results of treatment in 24 consecutive patients, operated between 2005 and 2015. All patients had Kajava class IV masses. Three were treated by liposuction alone, while 21 were treated by open axillaplasty with limited liposuction.
Results:
One patient treated by liposuction alone had to be re-operated for a residual lump, while with axillaplasty, no major complications were observed and the results were uniformly good.
Discussion:
Certain points of technique emerged as major determinants in obtaining the best results. In brief, these are: a) limited skin excision; b) placing elliptical incisions within the most lax, apical axillary skin, irrespective of the location of the lump; c) raising skin flaps at the level of superficial fascia; d)meticulous dissection and preservation of the nerves, especially the second intercostobrachial; f) judicious liposuction for eliminating dog ears and axillary sculpting only; g) avoiding drains.
Conclusion:
Open axillaplasty with limited liposuction is the best way to minimise complications and produce good results.
KEY WORDS: Axillaplasty, axillary breast, excision of axillary breast
INTRODUCTION
Accessory breast tissue may present as a mass at any place along the embryologic ‘mammary streak’, including the axillae, chest wall or vulva. The face, neck, ear, lateral thigh, buttock or the knee may rarely be the sites of aberrant or ectopic tissue.[1,2] As many as 2-6% of women and 1-3% of men have this congenital condition, and 20% of these are found in the axilla.[3]
Despite the relatively frequent occurrence, this condition has received sparse attention in plastic surgery journals.
In 1915, Kajava published a classification that is still used.[3,4]
Complete glandular breast tissue with areola and nipple
Nipple and glandular tissue, no areola
Areola and glandular tissue without a nipple
Glandular tissue only
Nipple and areola but no gland (pseudomamma)
Nipple only (polythelia)
Areola only (polythelia areolaris)
Patch of hair only (polythelia pilosa)
Clinically, lipoma, lymphadenopathy, hidradenitis, sebaceous cyst, vascular malformation or malignancy may be suspected before axillary breast is diagnosed. Mammogram, ultrasound, magnetic resonance imaging (MRI), needle biopsy or surgical biopsy can be used as diagnostic tools.[3]
Proper choice of treatment technique is critical in order to obtain good results.[4] Liposuction and surgical excision are the two main modalities, both with their own advantages, limitations and complications.
This study retrospectively examines the surgical technique, and results thereof, in 24 consecutive patients presenting with axillary breast lumps and presents the inferences drawn regarding the best surgical approach.
MATERIALS AND METHODS
We present 24 patients treated surgically for axillary breast from 2005 to 2015 and the refinement of technique that we developed during the course of the study. The age group was 18-62 years but the majority of patients were 22-42 years old. All patients had bilateral lumps except 1 [Table 1].
Table 1.
Symptomatology
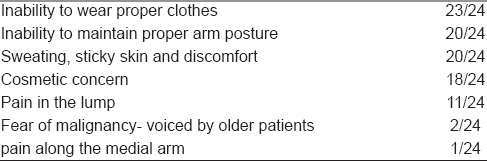
All patients had Kajava IV lumps, i.e., only accessory breast tissue without any cutaneous component in terms of nipple or areola. Ultrasound was used in every patient to evaluate percentages of fatty and breast tissue. All patients had mixed parenchyma on sonography. One patient was diagnosed as pure lipoma on histopathology.
Technique used for liposuction: A blunt, 3-mm cannula and traditional suction were employed.
Technique of axillaplasty:
Preoperative sonography was performed to evaluate the amount of the breast and fatty tissue.
Marking and surgery were done with the arm positioned at right angles.
Limited excision of skin was done with elliptical incisions taken in the direction of maximum laxity, irrespective of relaxed skin tension lines of the axilla [Figure 1a].
Adequately thick flaps at the level of superficial fascia were raised on either side of the excision.
Liposuction was used to treat dog ears and for the sculpting of anterior and posterior axillary folds only.
Nerves were preserved meticulously [Figure 1c].
Two-layer closure was done using polydiaxanone with shoulder maximally abducted.
Neither a drain nor a pressure garment was used.
Many-tailed elastic tape was used to give compression.
All specimens were subjected to histopathological examination.
Figure 1.
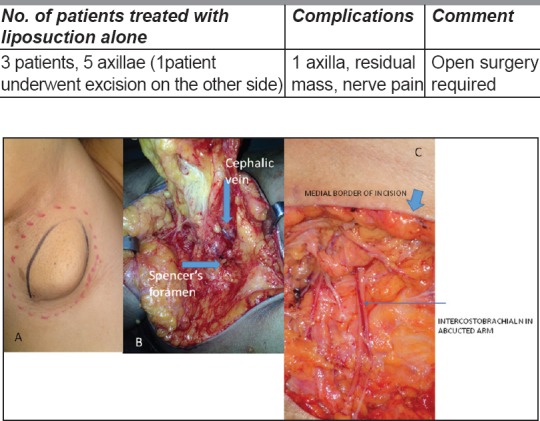
(a) Marking of the incision for limited elliptical skin excision (b) Axillary tail exiting foramen of Spencer (c) Meticulous dissection of nerve with preservation of every twig
All patients were followed up on days 4,8 and 14 postoperatively. Sutures were removed on the 14th postoperative day. Follow-up photographs were taken and the patient's satisfaction about the resulting scar, contour and improvement in symptoms was recorded at 1 month, 3 months and 6 months. The latter was recorded as either unhappy, moderately satisfied or completely satisfied in terms of results. Objective assessment was done noting scar quality, residual dog ear, axillary aesthetics and presence of neuralgia.
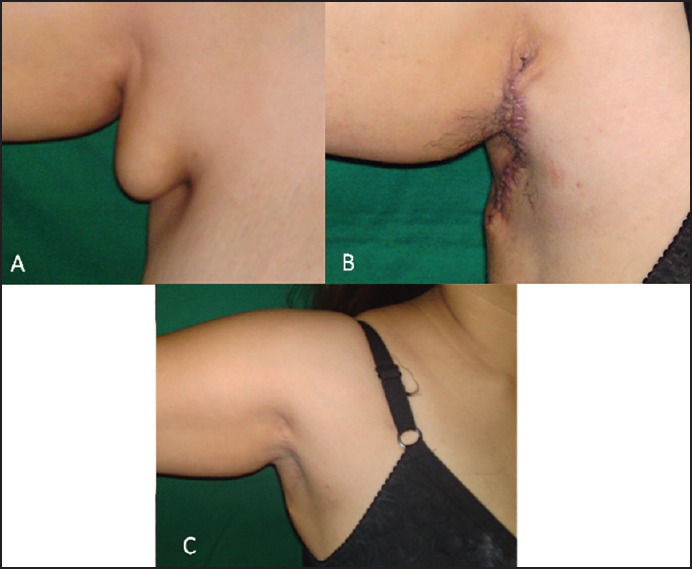
RESULT
Axillaplasty: Open excision with limited liposuction
Number of patients: 21, axillae treated: 41+ 1 (The patient who needed open surgery on one side, from the liposuction group)
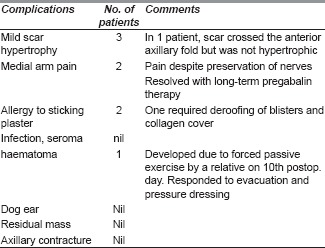
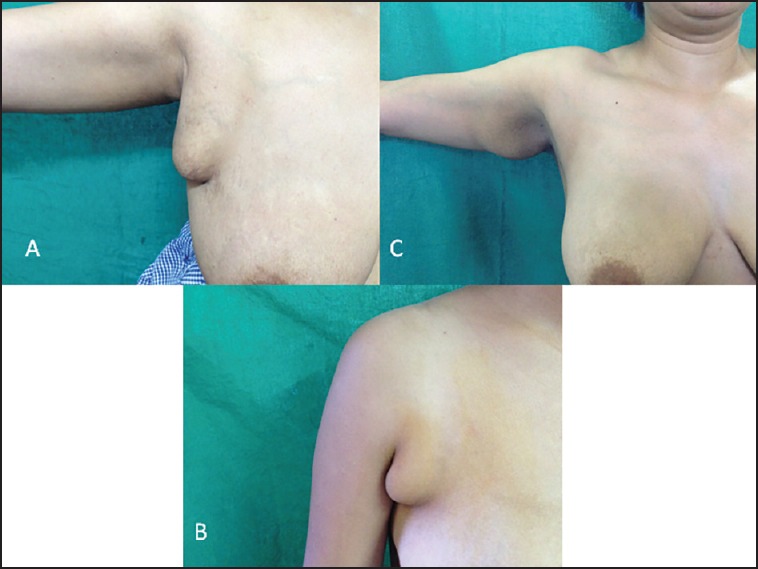
All patients were happy about the aesthetic outcome and relief of symptoms. Relief of symptoms was within the immediate postoperative period. The scars settled within 6months after the procedure [Figure 2].
Figure 2.
(a) Preop. Picture (b) 1 month postop.(c) 6 months postop. with imperceptible scar
DISCUSSION
Axillary breast is a not uncommon malady suffered by women, often silently. The fear of malignancy; inability to wear proper clothes leading to sweating, stickiness and discomfort; and inability to maintain proper arm posture are common symptoms.[1] Lack of awareness about the possibility of treatment results in under-reporting, which is common to all breast problems, including cancer. Many of the reports in literature are written by radiologists.[5]
Although axillary breast is congenital in origin, enlargement is often associated with hormonal surges such as menarche or pregnancy. In our series, most of the patients presented in the 30-45 years (average 36) age group, though the lump had started around puberty or pregnancy. In the series of 9 patients by Bartsich and Sophie, the average age at presentation was 42 years.[4]
Axillary breast is but one of the many sites where accessory breast tissue can be present. Of all the accessory breast tissues, 20% are axillary[3]. The extra breast tissue can be present in developed form or any combination of glandular tissue, nipple and areola (Kajava classification). In our series, all the patients had only breast tissue. None had nipple or areola. This tissue can not only undergo cyclical hormonal changes and secrete milk, but can also be affected by any type of benign or malignant breast pathology. Thus, it can be the seat of duct ectasia, cystic disease and malignancy. Patients reported by radiologists have been diagnosed on ultrasound or MRI. In such a series, Shetty and Radswiki found other Kajava types as well.[5]
In our series, none suffered from any benign or malignant pathology, though 1 patient who suffered from tuberculosis and was treated previously for the same, turned out to have lymph node along with the breast tissue. The lymph node showed changes of chronic granulomatous inflammation. No treatment was required as per medical opinion sought. Thus, it is important to carry out imaging to rule out breast as well as axillary pathology before embarking upon treatment.
Anatomy of the axilla is well understood. The salient points are as follows. It is a pyramidal structure with a concave floor. This makes it difficult to use pressure garments. When the arm is in abduction, the neurovascular structures lying near the roof are displaced downwards, thus making them liable to be injured during liposuction. The aesthetic landmarks of the axilla have not been discussed in the literature. The anterior and posterior axillary folds are the boundaries which should not be violated during the procedure. Lipo-sculpting of these folds gives better contour. The concavity of the floor takes the priority in contouring.
We suggest a sub-classification of Kajava type IV breast, by location as follows [Figure 3]:
Figure 3.
Sub-classification of Kajava IV axillary breast (a)Para-mammary (b) Central axillary (c) Medial arm
Para-mammary
Central axillary
Medial arm
This is important in diagnosis when considering masses in medial arm or para-mammary location. In any case, the incision needs to be placed in the axilla and not on the mass directly. This is aesthetically beneficial.
Liposuction and excision are two well-known options for management of axillary breast.
The distinct advantages of liposuction would be smaller scars and feathering of tissues for better contour; tissue, however, would not be available for histopathology.[4] Liposuction, used alone, often leaves a residual mass, mostly comprising breast tissue. Attempts to avoid leaving any residual mass would require the use of a sharp cannula as used in gynaecomastia. This is not feasible in the axilla, with important neurovascular structures passing through the mass.[4]
The maintenance of adequate flap thickness prevents depressions. Most women are happy to lose the hair-bearing area during excisional surgery. This hairy skin is also tough and non-retractile. Thus, it prevents achievement of concave contour postoperatively, if liposuction alone is used for large masses.[4]
We found it difficult to provide proper pressure by using either pressure garment or figure-of-8 dressing. A pressure garment also causes pain and numbness due to compression at the sleeve edge.
Excision alone can lead to long unsightly scars (Lesavoy) and dog ears.
Our technique combines both the modalities in an attempt to give the best aesthetic results and avoid postoperative discomfort. Dog ears should not be chased but suctioned to limit extension of the scar on to the anterior and posterior folds. Reservations about scarring are eliminated as the length of the scar is reduced by using liposuction for the dog ears and the scar becomes imperceptible by the end of 6 months, as shown in 21 out of 24 patients. By avoiding liposuction inside the axilla, the nerves are preserved, along with the axillary pad of fat that protects the major nerves [Figure 4] and vessels that are thrown into the surgical field in the position of 90-degree abduction of the shoulder.
Figure 4.
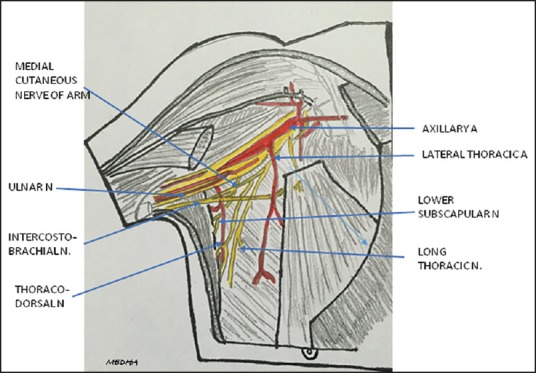
Nerves and vessels of axilla adapted from Gray's Anatomy
Liposuction of the posterior axillary fold is important to prevent the bulk of the fold shifting to the axilla and masking the concavity achieved by excision.
We managed to avoid drains, which are uncomfortable for patients, by using strategically cut Elastoplast that could hug the contours of the axilla and provide good compression. Of course, when in doubt, drains might need to be used. Bartsich et al. recommend the use of closed suction drains, well-designed incisions and direct excision of tissues to minimise morbidity. They enumerate complications such as neurovascular and intercostal nerve injury, and recommend that the same can be avoided with meticulous dissection.[4]
CONCLUSION
Traditional liposuction is neither sufficient nor efficient to treat symptomatic axillary breast. The reasons are: Difficulty in removal of the tough breast tissue, the need to protect the nerves and vessels, and difficulty in applying pressure dressing. Open surgery is the better choice, with limited liposuction used only for contouring. Incisions should be marked in the position of maximum abduction of the shoulder joint. Irrespective of the location of the axillary breast, (para-mammary, central axillary or medial arm), the incision is best placed on the hair-bearing skin at the apex of the axilla. Careful dissection of involved nerves is mandatory to avoid postoperative neurologic symptoms. Scars in the axilla heal exceptionally well despite the presence of hair.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Lesavoy MA, Gomez-Garcia A, Nejdl R, Yospur G, Syiau TJ, Chang P. Axillary breast tissue: Clinical presentation and surgical treatment. Ann Plast Surg. 1995;35:356–60. [PubMed] [Google Scholar]
- 2.Warwick R, Williams PL. Embryology of mammary glands. In: Warwick R, Williams PL, editors. Gray's Anatomy. 35th ed. Longman group ltd, Great Britain; 1973. p. 126. [Google Scholar]
- 3.Sahu SK, Hussain M, Sachan PK. Bilateral accessory breast? Int J Surg. 2007;17:?. [Google Scholar]
- 4.Bartsich SA, Ofodile FA. Accessory breast tissue in the axilla: Classification and treatment. Plast Reconstr Surg. 2011;128:35e–6e. doi: 10.1097/PRS.0b013e3182173f95. [DOI] [PubMed] [Google Scholar]
- 5.Shetty A, Radswiki Accessory breast tissue. Radiopaedia.org, rID 11125 [Google Scholar]


