Abstract
Background
The use of primaquine (PQ) for radical treatment of Plasmodium vivax in carriers of G6PD deficiency (G6PDd) constitutes the main factor associated with severe haemolysis in G6PDd. The current study aimed to estimate the incremental cost-effectiveness ratio of using a rapid diagnostic test (RDT) to detect G6PDd in male patients with P.vivax malaria in the Brazilian Amazon, in comparison with the routine indicated by the Programme for Malaria Control, which does not include this evaluation.
Methods
A cost-effectiveness analysis of estimated RDT use was carried out for the Brazilian Amazon for the year 2013, considering the perspective of the Brazilian Public Health System. Using decision trees, estimates were compared for two different RDT strategies for G6PDd in male individuals infected with P. vivax before being prescribed PQ, with the routine indicated in Brazil, which does not include prior diagnosis of G6PDd. The first strategy considered the combined use of RDT BinaxNOW® G6PD (BX-G6PD) in municipalities with more than 100,000 inhabitants and the routine programme (RP) for the other municipalities. Operational limitations related to the required temperature control and venous blood collection currently restrict the use of RDT BX-G6PD in small municipalities. The second strategy considered the use of the RDT CareStart™ G6PD (CS-G6PD) in 100 % of the municipalities. The analysis was carried out for the outcomes: “adequately diagnosed case” and “hospitalization avoided”.
Results
For the outcome “adequately diagnosed case”, comparing the RDT strategies based on RDT with the routine control programme (RP), the CS-G6PD strategy was the most cost-effective, with BX-G6PD extendedly dominating (the ICER of BX-G6PD compared with RP was higher than the ICER of CS-G6PD compared with RP). CS-G6PD dominated the other strategies for the “hospitalization avoided” outcome.
Conclusion
The CS-G6PD strategy is cost-effective for adequately diagnosing cases and avoiding hospitalization. This information can help in decision-making, both in incorporating prior diagnosis in the use of PQ and to promote greater safety among G6PD deficient individuals in the Brazilian Amazon P. vivax endemic areas.
Keywords: Cost-effectiveness analysis, Glucose-6-phosphate dehydrogenase deficiency, Primaquine, Haemolysis, Malaria, Plasmodium vivax, Economic analysis
Background
The use of primaquine (PQ) for radical treatment of Plasmodium vivax in carriers of G6PD deficiency (G6PDd) constitutes the main factor associated with severe haemolysis, hospitalization and death in G6PDd individuals in Latin America, especially in males; cases of severe adverse events in females induced by PQ, have not been reported in the Brazilian Amazon [1, 2]. In Brazil, PQ is administered to prevent relapses of P. vivax malaria and to reduce its transmission [3]. However, this radical cure treatment of P. vivax malaria with PQ represents a risk for G6PDd carriers, since the Brazilian malaria national control programme does not recommend a routine G6PDd diagnosis before treatment starts. More than 99 % of the 178,600 new Brazilian cases of malaria in 2013 were reported in the Amazon, of which 81 % were caused by P. vivax [4, 5]. The estimates are approximately 6000 hospitalizations per year for individuals with G6PDd as a result of using PQ, creating a substantial burden, of an estimated costing of US$ 4,858,108.87 per year, for the Brazilian Public Health Service (Sistema Único de Saúde/SUS) [6]. In this context, detecting G6PDd before PQ is prescribed could contribute to improving treatment safety in people with G6PDd, preventing harm done to the efforts to control and eliminate malaria. In Brazilian Amazon, the prevalence of G6PDd in males was estimated at 4.5 % [7]. The identification and implementation of a rapid, efficient and feasible diagnostic method in field conditions is a priority [8–11].
The gold standard G6PDd diagnostic test is a quantitative spectrophotometric assay that requires laboratory setting, complex equipment and specialized staff. In less sophisticated settings, the fluorescent spot test has been widely recommended because it is easy to execute. However, this test also requires specialized equipment, such as an ultraviolet bulb, a water bath and a micropipette. Thus, neither of these two tests can be considered appropriate for field conditions in most of the malarial areas in the Amazon region [8, 12–14], and they are not used in routine services.
Two RDTs have been evaluated to detect G6PDd in field conditions under different situations: BinaxNOW® G6PD (BX-G6PD) and CareStart™ G6PD (CS-G6PD). Both are qualitative chromatographic tests that are easily read visually, require minimal training and results can be obtained within 10 min [12, 15, 16].
BX-G6PD presents operational limitations related to temperature, as it provides reliable results only when performed at 18–25 °C range, and the sample required is venous blood [15, 17]. A recently reported multicentre study that included the city of Manaus found a sensitivity of 54.6 % and a specificity of 100 % for this test in malaria patients using a cut-off value corresponding to 60 % of normal activity [16]. The authors mentioned unpublished data for a cut-off of 40 % of normal activity the sensitivity and specificity were, respectively, 66.6 and 100 %.
CS-G6PD requires capillary blood samples collected from sterile finger pricks and results are not affected by high temperatures during its conservation and execution [12]. When this test was used for patients with malaria in Manaus, sensitivity was 45.45 % and specificity 98.71 %, for a cut-off value of 40 % of normal enzyme activity (Brito et al, Personal communication, 2015). In the general population of villages in Cambodia, this cut-off value the test showed a sensitivity and specificity of 93.3 and 97.4 % respectively [18].
The absence of cost-effectiveness analysis comparing the use of RDTs for G6PDd diagnosis with the status quo, where testing before PQ prescription is not performed, is an important gap that makes it difficult to recommend these tests [13, 14, 19]. The absence of a G6PDd diagnosis also represents an obstacle for the future use of tafenoquine, a new promising 8-aminoquinoline that has shown high efficacy in radical cure of P. vivax malaria when administered as a single dose [6, 19, 20]. Therefore, the present cost-effectiveness study was carried out with the objective of estimating the incremental cost-effectiveness ratio (ICER) of introducing a RDT to detect G6PDd in male patients carrying P. vivax in the Brazilian Amazon, in comparison with the routine programme (RP) of the Brazil’s Malaria Control Programme.
Methods
A cost-effectiveness analysis (CEA) was done from the perspective of the Brazilian Public Health Service (SUS) for 2013. The study area covers the Brazilian Amazon, composed of 775 municipalities distributed in nine States (Acre, Amapá, Amazonas, Maranhão, Mato Grosso, Tocantins, Rondônia, Roraima and Pará), where the population is approximately 21 million, of whom 10 million live in 34 municipalities with more than 100,000 inhabitants [21]. In the region, 427 municipalities registered cases of P. vivax malaria in 2013 [4].
Two G6PDd RDT strategies were compared, in male individuals infected with P. vivax before they were prescribed PQ, with the RP stipulated in Brazil, without prior diagnosis of G6PDd. Females were excluded since in Latin America clinically important manifestations occur mainly in males (cases of severe adverse events induced by PQ, have not been reported in the study region). The first strategy was based on the combined use of BX-G6PD in the municipalities with more than 100,000 inhabitants and the RP in other municipalities (BX-G6PD strategy). Operational limitations related to the required temperature control and venous blood collection restrict the use of RDT BX-G6PD in small municipalities. The second was based on CS-G6PD (strategy CS-G6PD) considering its use in 100 % of the municipalities. The analysis was carried out for the outcomes: “adequately diagnosed case” and “hospitalization avoided”.
Assumptions
This analysis used the assumptions previously detailed by Peixoto et al. [6], related to the diagnosis of malaria, the treatment of P. vivax and assistance to G6PDd carriers with severe adverse events associated with PQ, except the cost of hospital staff. In the current study the total mean cost of the Authorization for Hospitalization (AIH) includes the payment of professional and hospital services done by SUS. It was also assumed that the diagnostic units were able to store and carry out tests at the temperature recommended by the manufacturers, and that the execution of CS-G6PD would be carried out by health agents and that of BX-G6PD by nursing technicians.
The decision model
Decision trees were used to compare the strategies being evaluated (Fig. 1). A hypothetical cohort was simulated from all male patients who presented fever and requested diagnosis for malaria, considering its various probability nodes. After the malaria thick blood smear test, the patient was submitted to the probability of having or not having malaria, followed by the type of malaria—P. vivax or P. falciparum—and then to the probability of carrying out a diagnosis with one of the RDTs for G6PDd or to the RP without G6PDd diagnosis. The individual infected with P. vivax might or might not carry the deficiency, and this estimate was based on the prevalence of G6PDd in the Amazon Region.
Fig. 1.
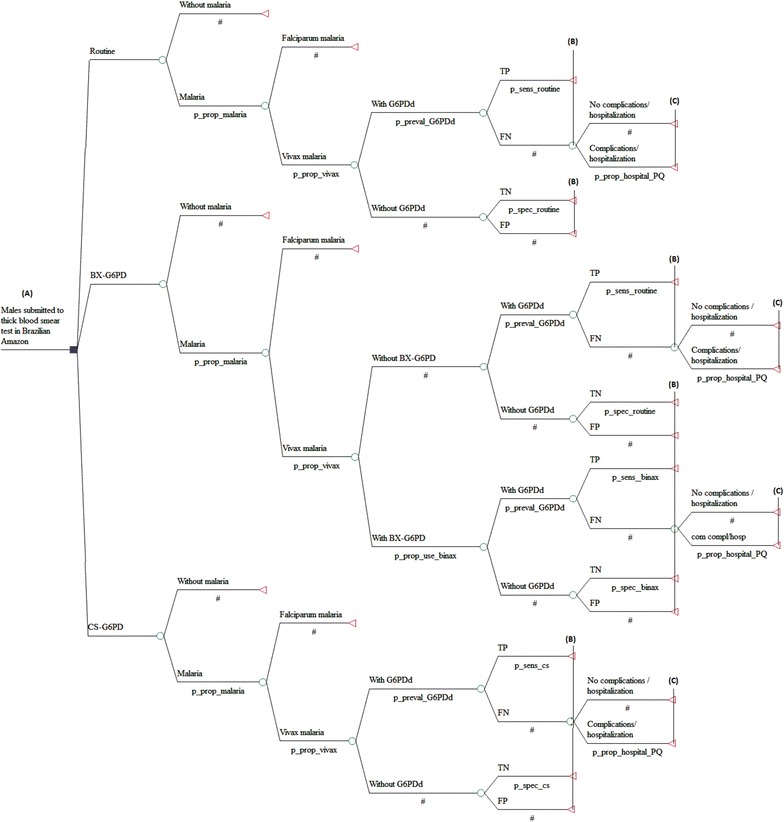
Decision tree for the outcomes: adequately diagnosed case (A–B) and avoided hospitalization (A–C). Brazilian Amazon, 2013
After carrying out one of the tests for G6PDd, the probabilities were taken relative to the sensitivity and specificity of the diagnostic strategy used, with true positives (TP), false positives (FP), true negatives (TN) and false negatives (FN) results. For RP, the model assumes that the strategy is not able to diagnose the G6PDd, since it does not uses diagnostic test for this purpose. After use of the diagnostic test, TP and TN results were considered adequately diagnosed cases, whereas FP and FN were considered incorrectly diagnosed cases. After diagnosis, the hypothetical cohort was analysed by the probability of hospitalization. It was assumed that all individuals classified as FN and TN were submitted to treatment with PQ, and those identified as TP and FP were not. Thus, the carrier of G6PDd who uses PQ (FN) is submitted to the probability of not being hospitalized (hospitalization avoided) or hospitalization due to severe adverse events provoked by the medication. All costs and epidemiological parameters used in the decision model are shown in Tables 1 and 2.
Table 1.
Cost components and unit costs considered in the analytical model
| Items | Cost per patient (unit costs, US$) | Sources base-case/variations | |
|---|---|---|---|
| Base-case | Variations | ||
| Diagnosis of P. vivax malária | |||
| Thick blood smeara | 1.31 | 0.27–2.00 | [40] / [35]–[40] |
| Microscopea | 0.75 | 0.60–0.90 | [41] /± 20 % |
| Microscope maintenancea | 0.06 | 0.05–0.07 | [41] /± 20 % |
| Health workersa | 3.48 | 2.78–4.18 | [42] /± 20 % |
| Annual training (microscopist)a | 5.67 | 4.54–6.80 | [35] /± 20 % |
| Drug treatment for P. vivax (therapeutic scheme) | |||
| Males without G6PDdb | 0.23 | 0.18–0.28 | [43] /± 20 % |
| Males with G6PDdb | 0.12 | 0.10–0.14 | [43] /± 20 % |
| Males with G6PDd/prophylactic treatmentb | 0.28 | 0.22–0.34 | [43] /± 20 % |
| G6PDd diagnosis | |||
| Training (RDT)c | 0.80 | 0.64–0.96 | [35] /± 20 % |
| CS-G6PD | |||
| Health workerd | 1.74 | 1.39–2.09 | [42] /± 20 % |
| One test | 1.50 | 1.20–1.80 | [44, 45] /± 20 % |
| Suppliese | 0.10 | 0.08–0.12 | [46] / [46]–[46] |
| BX-G6PD | |||
| Health workerd | 2.04 | 1.63–2.45 | [42] /± 20 % |
| One test | 5.88 | 4.70–7.06 | [47] /± 20 % |
| Suppliese | 1.09 | 0.87–1.31 | [45, 46] / [46]–[46] |
| Assistance to carriers of G6PDd treated with PQ | |||
| Pre-admission testsa | 10.69 | 9.65–11.38 | [4, 40] / [4, 40] |
| Medical appointmentsa | 4.63 | – | [48] /– |
| Hospitalization (AIH)f | 198.81 | 159.05–238.57 | [49] /± 20 % |
| Hospital fooda | 68.72 | 54.98–82.46 | [50] /± 20 % |
Brazilian Amazon, 2013
aCosting previously detailed by Peixoto et al. [6]
bTherapeutic schemes: chloroquine for 3 days and PQ for 7 days (males without G6PDd); chloroquine for 3 days (males with G6PDd) and prevention of relapse with chloroquine weekly for 12 weeks (prophylactic treatment)
cBased on the cost of one training period per year per municipality for the diagnosis of malaria with RDT OptiMal® in the Brazilian Amazon
dCost per test based on the average salary of Amazonas State in 2013
eVariation obtained from the minimum and maximum cost identified in the time series of prices of bank (BPS) within the Ministry of Health (MoH) in 2013
fCost obtained through the analysis of 108 files from the Hospital Information System (SIH/SUS) of the Brazilian Amazon in 2013
Table 2.
Epidemiological parameters considered in the analytic models. Brazilian Amazon, 2013
| Parameter | Base-case | Variations | Sources base-case/variations |
|---|---|---|---|
| Proportion of malaria among febrile males seeking diagnosisa | 0.0886 | 0.0881–0.0891 | [4] /IC 95 % |
| Proportion of malaria cases due to P. vivax in male patientsa | 0.835 | 0.833–0.837 | [4] /IC 95 % |
| Prevalence of G6PDd in male patients | 0.045 | 0.025–0.056 | [7] /f]–[7] IC 95 % |
| Proportion of males with G6PDd hospitalized after treatment with PQb | 0.943 | 0.744–1 | [39] /± 20 % |
| Proportion of the use of BX-G6PDc | 0.184 | 0.182–0.187 | [4, 21] /IC 95 % |
| Sensitivity of CS-G6PDd | 0.455 | 0.213–0.720 | f/IC 95 % |
| Specificity of CS-G6PDd | 0.987 | 0.967–0.995 | f/IC 95 % |
| Sensitivity of BX-G6PDd, e | 0.667 | 0.301–0.921 | [16] /IC 95 % |
| Specificity of BX-G6PDd, e | 1 | 0.989–1 | [16] /IC 95 % |
aParameter obtained from the analysis of the databanks from the nine States of the Brazilian Amazon
bParameter obtained from follow-up of patients with G6PDd in FMT-HVD
cProportion corresponding to individuals diagnosed with P. vivax malaria, residents of municipalities with more than 100,000 inhabitants
dThe cutoff point: 40 % of the median enzyme activity in the sample
eThe base-case and the variation considering data from Brazil and Peru
fBrito et al. Personal Communication, 2015
Costs
For the outcome “adequately diagnosed case” the health costs arising from malaria diagnosis among male individuals and the diagnosis of G6PDd in individuals with P. vivax malaria were considered. For the outcome “hospitalization avoided” medication-based treatment for P. vivax malaria and the costs of health assistance for those undergoing severe adverse events associated with the use of PQ in G6PDd carriers were added on (Table 1). The costs obtained in Brazilian currency (reais, R$) were converted to US dollars (US$) using the mean value of the official exchange rate for the year 2013 (R$ 2.16 per dollar) [22]. The costs identified in other years were adjusted based on the official inflation rates estimated by the accumulated National Consumer Price Index (IPCA) [23].
Epidemiological parameters
Epidemiological data and those of services related to malaria and to G6PDd within the context of malaria were obtained from the Malaria Epidemiological Vigilance Information System (SIVEP/Malária) [4], from the scientific literature and from unpublished documents and databanks at the Tropical Medicine Foundation Dr. Heitor Vieira Dourado (FMT-HVD) (Table 2).
Cost-effectiveness and sensitivity analysis
By means of the decision models, the final costs and the effectiveness of the strategies were obtained, as well as the incremental cost-effectiveness ratios (ICER) for “adequately diagnosed case” and “hospitalization avoided”, considering the parameters used in base-case. Univariate and multivariate sensitivity analyses were carried out for all the epidemiological and cost parameters, except for the cost of the specialized medical consultation, which is a fixed cost in the health system and did not undergo alterations during the study period.
Tornado diagrams were based on the individual impact of each of the variables on the ICER to demonstrate the results from univariate analysis. The probabilistic sensitivity analysis (PSA) was carried out by means of the second-order Monte Carlo simulation, which evaluated the simultaneous impact of all the mentioned variables with regard to ICER. The following distributions were attributed to the entry parameters: beta distribution for the probability parameters and gamma or triangular distribution for the cost parameters. Finally, considering the three strategies evaluated for each of the outcomes, 10,000 interactions were carried out to produce acceptability curves based on a willingness to pay of US$ 6480 per additional outcome, which is equivalent to the per capita GDP for the Amazon Region. The software TreeAge Pro® 2013 (TreeAge Pro Inc, Williamstown, MA, USA) was used to construct the decision model, for the calculation of the ICERs and for sensitivity analyses.
Ethical considerations
The research project was submitted to the Ethics Committee of the Faculty of Health Sciences at the University of Brasilia and approved on May 14th 2013 (case number 276,522).
Results
The strategy based on the use of CS-G6PD in 100 % of the population was more cost-effective when compared to RP and the strategy that combines BX-G6PD and RP (BX-G6PD strategy). The BX-G6PD strategy was extendedly dominated (the ICER of BX-G6PD compared with RP was higher than the ICER of CS-G6PD compared with RP) and the strategy CS-G6PD was the most cost-effective for the outcome “adequately diagnosed case”. For “hospitalization avoided”, the RP and BX-G6PD strategies were dominated by the CS-G6PD strategy (Table 3).
Table 3.
Results of the cost-effectiveness analysis of the strategies “RP”, “CS-G6PD” and “BX-G6PD”, according to the outcomes assessed in the Brazilian Amazon, 2013
| Strategy | Effectiveness | Incremental effectiveness | Cost (US$) | Incremental cost (US$) | ICER (US$) |
|---|---|---|---|---|---|
| Outcome: adequately diagnosed case | |||||
| RP | 0 | – | 11.270 | – | – |
| BX-G6PD (vs. RP) | 0.0135 | 0.0135 | 11.404 | 0.134 | 9.96 |
| CS-G6PD (vs. RP) | 0.0716 | 0.0716 | 11.578 | 0.308 | 4.30 |
| CS-G6PD (vs. BX-G6PD) | 0.0716 | 0.0581 | 11.578 | 0.174 | 2.99 |
| Outcome: hospitalization avoided | |||||
| CS-G6PD | 0.0723 | – | 12.078 | – | Dominant |
| BX-G6PD (vs. CS-G6PD) | 0.0712 | −0.0010 | 12.200 | 0.122 | Dominated |
| RP (vs. CS-G6PD) | 0.0708 | −0.0014 | 12.175 | 0.097 | Dominated |
| BX-G6PD (vs. RP) | 0.0712 | 0.0004 | 12.200 | 0.025 | 63.92 |
The univariate sensitivity analyses for the outcome “adequately diagnosed case” showed that variations in the epidemiological and cost parameters did not have an important impact on the ICERs, whose greatest variation was only US$ 0.45. For “hospitalization avoided” the CS-G6PD strategy remained dominant in relation to the BX-G6PD and RP strategies, as evidenced by negative ICERs, supporting a greater effectiveness and lower cost for the CS-G6PD strategy. Exceptions occurred only in the sensitivity analysis of the variables sensitivity of CS-G6PD and prevalence of G6PDd, with positive ICERs (Fig. 2).
Fig. 2.
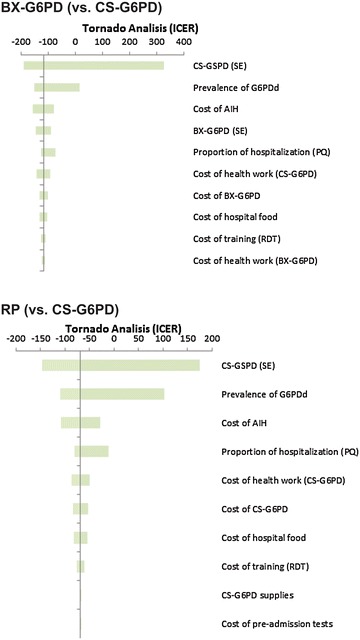
Univariate sensitivity analysis for the outcome hospitalization avoided, based on the individual impact of each of the variables on the ICER. Brazilian Amazon, 2013
Two acceptability curves were generated for the PSA (Fig. 3), for the outcomes “adequately diagnosed case” and “hospitalization avoided” respectively. For both curves, the strategy based on CS-G6PD presented a high probability of being cost-effective, at 10 % of the limit considered in the analysis.
Fig. 3.
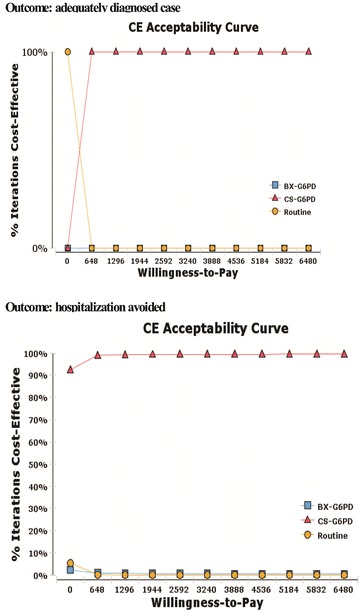
Acceptability curves of the three evaluated strategies in accordance with the outcome. Brazilian Amazon, 2013
Additionally, ICERs were estimated considering the highest (18.6 %) and the lowest (4.3 %) proportion of malaria in individuals submitted to the thick blood smear test among the States evaluated. The results demonstrate that the CS-G6PD strategy continues to be the most cost-effective one for appropriate diagnosis of G6PDd, presenting for both proportions the same ICER as that identified in the base-case when compared to the RP. For the outcome “hospitalization avoided”, the CS-G6PD strategy continued to dominate the others. The second analysis of additional sensitivity simulated the amplification of the use of BX-G6PD for the municipalities with more than 50,000 inhabitants (where 40.9 % of the cases of P. vivax malaria in men occurred). Again, the results did not cause significant modifications in the ICERs, and the CS-G6PD strategy continued to be the most cost-effective for the outcome “adequately diagnosed case” and was dominant for “hospitalization avoided”.
Discussion
Although malaria continues to be one of the main public health problems in the world, there have been some successful results from control efforts in recent years, leading some endemic regions to consider the possibility of malaria eliminating [24]. Tatem et al. showed that the Americas present great potential for elimination of Plasmodium falciparum, as well as operational conditions for controlling P. vivax. In this context, for the regional efforts directed to eliminating malaria to be successful, the strategies directed to combating P. vivax have taken on an even greater importance [9, 25].
The elimination of P. vivax malaria will only be possible with the effective use of an 8-aminoquinoline for the radical treatment of latent P. vivax infections [13, 19]. However, as the use of this type of anti-malarials threatens the safety of G6PDd individuals, previous diagnosis of this condition in patients with P. vivax malaria needs discussion [13, 19], and it is vital that cost-effective diagnostic strategies are identified [1, 6, 11].
The RDTs considered in the study have different accuracies and integrate different strategies. The cost associated with performing each test (training and salary of health workers, test kits and supplies) was also different: US$ 9.81 for BX-G6PD and US$ 4.14 for CS-G6PD.
The present study constitutes the first CEA of strategies based on the two main RDTs for diagnosing G6PDd that are available and feasible under field conditions. These were compared to the routine strategy for prescribing PQ without prior diagnosis of the deficiency in the Brazilian Amazon. The results indicate that the strategy based on the use of CS-G6PD is cost-effective, for the outcome “adequately diagnosis of G6PDd”, whose ICERs were lower than 1 % of the per capita GDP of the region, and also for the outcome “hospitalization avoided”, for which it was dominant.
A hypothetical 2013 cohort of 1,188,523 males presenting with fever and requesting diagnosis for malaria would be administered 87,928 RDT CS-G6PD in males with P. vivax (RDT in 100 % of the municipalities) or 16,179 RDT BX-G6PD in males with P. vivax, based on combined use with RP (RDT in 18.4 % of the municipalities), which could prevent, respectively, 1808 hospitalizations (a cost of US$ 511,522) and 488 hospitalizations (US$ 137,974).
The analysis assumed the values of sensitivity and specificity obtained in studies carried out with patients diagnosed with malaria (Table 2). These estimate a reduction in the accuracy of the RDTs evaluated when compared to the accuracy estimated in studies with the general population. This may occur due to the greater number of new erythrocytes produced as a result of the acute haemolysis provoked by malaria, since new erythrocytes present more G6PD enzymatic activity when compared to mature cells, which may lead to false negative results [16, 26].
A recent study that evaluated the new generation of CS-G6PD demonstrated an improvement in its sensitivity for the general population in Cambodia [18], which could also occur in individuals with malaria, making the strategy even more cost-effective. Corroborating these promising results, another study in an area with high incidence of malaria in Africa recently estimated 100 % sensitivity in the general male population [27].
When the uncertainties concerning epidemiological and cost parameters were tested by means of the univariate analysis of sensitivity, the performance of the strategy based on CS-G6PD was not affected in an important way. The lowest variations in the sensitivity parameter of CS-G6PD and the prevalence parameter of G6PDd altered the dominance relationship of the CS-G6PD strategy for the outcome “hospitalization avoided”, but the strategy remained cost-effective.
The acceptability curves indicate that the probability of the strategy based on CS-G6PD being cost-effective is of approximately 100 %, for both outcomes, at 10 % of the limit of willingness to pay. For the second outcome, when the willingness to pay is US$ 0.00, the probability is over 90 %, demonstrating that the stochastic and simultaneous variation of the parameters for epidemiology and costs used indicates a high probability of the CS-G6PD strategy being cost-effective, despite the uncertainties inherent in the analytical model.
Decision-makers are being faced with increasingly difficult decisions when they consider the addition of new technologies to national malaria control program [28]. Aiming to help in decision-making, various economic studies have examined aspects related to primary prevention, diagnosis and treatment of malaria, with emphasis on vaccines [29, 30], mosquito nets impregnated with insecticides [31, 32], mass screening followed by treatment [33], use of RDTs to diagnose the infection [34, 35] and the use of schemes for chemo-prophylaxis and treatment [36–38]. Although there are no published studies on cost-effectiveness for G6PDd diagnosis in connection with malaria, recent publications have discussed the urgency of evaluating the efficiency of RDTs used to detect G6PDd so as to guarantee safety in the treatment of these patients [11, 13, 14].
This study presents some limitations, such as the fact that some epidemiological and cost parameters arise from one Amazon state arguing that results can be extrapolated to Brazilian Amazon. However, in the analysis of sensitivity, which includes plausible variations for the region studied, there were no important changes in the ICERs. The prevalence of G6PDd, the costs of hospital food and the salaries of the professionals involved in the RDT were generalized from data on the State of Amazonas, and the proportions of hospitalizations (94.29 %) were calculated from a cohort of G6PDd carriers who were monitored at FMT-HVD [39]. This represents the situation at a center of excellence, differing from the context in small towns of the Brazilian Amazon. Thus, the proportion of hospitalizations may have been overestimated, since in these places there is limited access to health services with moderate to high technological density [6].
Within this scope, the present study estimated a cost-effectiveness ratio that is favorable to the use of RDTs for G6PDd in the Brazilian Amazon, in particular CS-G6PD. Decision-makers in the National Programme of Prevention and Control of Malaria in the region should consider implementation of such RDT strategies for G6PDd diagnosis. The incorporation of RDTs will make the use of 8-aminoquinolines safer and may represent an increase in the effectiveness of P. vivax malaria control in Brazil.
Conclusion
The strategy based on CS-G6PD is cost-effective in diagnosing G6PDd and avoiding hospitalization. These results may help in future decision-making related to the use of CS-G6PD in the Brazilian Amazon when considering a safer P. vivax malaria treatment in the region for G6PDd individuals.
Authors’ contributions
HMP and MRFO conceived the study, participated in the design of the study, performed the analysis and drafted the manuscript. GASR, MVGL, WMM and MAMB conceived the study, participated in the design of the study, performed the analysis and participated in its analysis. All authors read and approved the final manuscript.
Acknowledgements
This study was supported by the Brazilian Council for Scientific and Technological Development (CNPq) (MCTI/CNPq No 14/2013), National Institute for Science and Technology for Health Technology Assessment (IATS) and by the Brazilian Ministry of Health (Call No 20/2013—Studies and Researches in Health Surveillance). GASR received a visiting fellowship from the Strategic Program for Science, Technology & Innovation of FAPEAM (PECTI-SAÚDE). MVGL is a level 1 fellow of CNPq.
Competing interests
The authors declare that they have no competing interests.
Abbreviations
- G6PD
glucose-6-phosphate dehydrogenase
- G6PDd
glucose-6-phosphate dehydrogenase deficiency
- PQ
primaquine
- RDT
rapid diagnostic test
- RP
routine programme
- CEA
cost-effectiveness analysis
- SUS
Brazilian Public Health Service
- IPCA
National Consumer Price Index
- ICER
incremental cost-effectiveness ratios
- PSA
probabilistic sensitivity analysis
Contributor Information
Henry M. Peixoto, Email: henrymaiap9@gmail.com
Marcelo A. M. Brito, Email: marceloambrito@gmail.com
Gustavo A. S. Romero, Email: gromero@unb.br
Wuelton M. Monteiro, Email: wueltonmm@gmail.com
Marcus V. G. de Lacerda, Email: marcuslacerda.br@gmail.com
Maria R. F. de Oliveira, Email: reginafernan@gmail.com
References
- 1.Monteiro WM, Franca GP, Melo GC, Queiroz ALM, Brito M, Peixoto HM, et al. Clinical complications of G6PD deficiency in Latin American and Caribbean populations: systematic review and implications for malaria elimination programmes. Malar J. 2014;13:70. doi: 10.1186/1475-2875-13-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lacerda MVG, Fragoso SCP, Alecrim MGC, Alexandre MAA, Magalhães BML, Siqueira AM, et al. Postmortem characterization of patients with clinical diagnosis of Plasmodium vivax malaria: to what extent does this parasite kill? Clin Infect Dis. 2012;55:e67–e74. doi: 10.1093/cid/cis615. [DOI] [PubMed] [Google Scholar]
- 3.Ministério da Saúde: Guia prático de tratamento da malária no Brasil. Brasília; 2010.
- 4.Ministério da Saúde: Sistema de informação de Vigilância Epidemiológica da Malária (SIVEP-Malária) http://portalweb04.saude.gov.br/sivep_malaria/default.asp.
- 5.Ministério da Saúde: Sistema de Informação de Agravos de Notificação (SINAN) http://dtr2004.saude.gov.br/sinanweb/tabnet/dh?sinannet/malaria/bases/malabrnet.def.
- 6.Peixoto HM, Brito MA, Romero GA, Monteiro WM, Lacerda MV, Oliveira MRF. G6PD deficiency in male individuals infected by Plasmodium vivax malaria in the Brazilian Amazon: a cost study. Malar J. 2015;14:126. doi: 10.1186/s12936-015-0647-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Santana MS, Monteiro WM, Siqueira AM, Costa MF, Sampaio V, Lacerda MV, et al. Glucose-6-phosphate dehydrogenase deficient variants are associated with reduced susceptibility to malaria in the Brazilian Amazon. Trans R Soc Trop Med Hyg. 2013;107:301–306. doi: 10.1093/trstmh/trt015. [DOI] [PubMed] [Google Scholar]
- 8.Kahn M, Larue N, Bansil P, Kalnoky M, McGray S, Domingo GJ. Cryopreservation of glucose-6-phosphate dehydrogenase activity inside red blood cells: developing a specimen repository in support of development and evaluation of glucose-6-phosphate dehydrogenase deficiency tests. Malar J. 2013;12:286. doi: 10.1186/1475-2875-12-286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gething PW, Elyazar IRF, Moyes CL, Smith DL, Battle KE, Guerra CA, et al. A long neglected world malaria map: Plasmodium vivax endemicity in 2010. PLoS Negl Trop Dis. 2012;6:e1814. doi: 10.1371/journal.pntd.0001814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The malERA Consultative Group on Drugs A research agenda for malaria eradication: drugs. PLoS Med. 2011;8:e1000402. doi: 10.1371/journal.pmed.1000402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Monteiro WM, Val FF, Siqueira AM, Franca GP, Sampaio VS, Melo GC, et al. G6PD deficiency in Latin America: systematic review on prevalence and variants. Mem Inst Oswaldo Cruz. 2014;109:553–568. doi: 10.1590/0074-0276140123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim S, Nguon C, Guillard B, Duong S, Chy S, Sum S, et al. Performance of the carestart™ G6PD deficiency screening test, a point-of-care diagnostic for primaquine therapy screening. PLoS One. 2011;6:e28357. doi: 10.1371/journal.pone.0028357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Domingo GJ, Satyagraha AW, Anvikar A, Baird K, Bancone G, Bansil P, Carter N, et al. G6PD testing in support of treatment and elimination of malaria: recommendations for evaluation of G6PD tests. Malar J. 2013;12:391. doi: 10.1186/1475-2875-12-391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Von Seidlein L, Auburn S, Espino F, Shanks D, Cheng Q, McCarthy J, et al. Review of key knowledge gaps in glucose-6-phosphate dehydrogenase deficiency detection with regard to the safe clinical deployment of 8-aminoquinoline treatment regimens: a workshop report. Malar J. 2013;12:112. doi: 10.1186/1475-2875-12-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tinley KE, Loughlin AM, Jepson A, Barnett ED. Evaluation of a rapid qualitative enzyme chromatographic test for glucose-6-phosphate dehydrogenase deficiency. Am J Trop Med Hyg. 2010;82:210–214. doi: 10.4269/ajtmh.2010.09-0416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Osorio L, Carter N, Arthur P, Bancone G, Gopalan S, Gupta SK, et al. Performance of BinaxNOW G6PD deficiency point-of-care diagnostic in P. vivax-infected subjects. Am J Trop Med Hyg. 2015;92:22–27. doi: 10.4269/ajtmh.14-0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eziefula AC, Gosling R, Hwang J, Hsiang MS, Bousema T, von Seidlein L, et al. Rationale for short course primaquine in Africa to interrupt malaria transmission. Malar J. 2012;11:360. doi: 10.1186/1475-2875-11-360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roca-Feltrer A, Khim N, Kim S, Chy S, Canier L, Kerleguer A, et al. Field trial evaluation of the performances of point-of-care tests for screening G6PD deficiency in Cambodia. PLoS One. 2014;9:e116143. doi: 10.1371/journal.pone.0116143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Recht J, Ashley E, White N. Safety of 8-aminoquinoline antimalarial medicines. Geneva: World Health Organization; 2014. http://www.who.int/malaria/publications/atoz/9789241506977/en/.
- 20.Llanos-Cuentas A, Lacerda MV, Rueangweerayut R, Krudsood S, Gupta SK, Kochar SK, et al. Tafenoquine plus chloroquine for the treatment and relapse prevention of Plasmodium vivax malaria (DETECTIVE): a multicentre, double-blind, randomised, phase 2b dose-selection study. Lancet. 2014;383:1049–1058. doi: 10.1016/S0140-6736(13)62568-4. [DOI] [PubMed] [Google Scholar]
- 21.Superintendência do Desenvolvimento da Amazônia: Amazônia Legal http://www.sudam.gov.br/amazonia-legal/demografia/50-amazonialegal.
- 22.Banco Central do Brasil: Taxas de Câmbio http://www4.bcb.gov.br/pec/taxas/port/ptaxnpesq.asp?id=txcotacao.
- 23.Ministério do Planejamento Orçamento e Gestão: Sistema Nacional de Índices de Preços ao Consumidor http://www.ibge.gov.br/home/estatistica/indicadores/precos/inpc_ipca/defaultseriesHist.shtm.
- 24.WHO . From malaria control to malaria elimination: a manual for elimination scenario planning. Geneva: World Health Organization; 2014. [Google Scholar]
- 25.Tatem AJ, Smith DL, Gething PW, Kabaria CW, Snow RW, Hay SI. Ranking of elimination feasibility between malaria-endemic countries. Lancet. 2010;376:1579–1591. doi: 10.1016/S0140-6736(10)61301-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cappellini MD, Fiorelli G. Glucose-6-phosphate dehydrogenase deficiency. Lancet. 2008;371:64–74. doi: 10.1016/S0140-6736(08)60073-2. [DOI] [PubMed] [Google Scholar]
- 27.Adu-Gyasi D, Asante KP, Newton S, Dosoo D, Amoako S, Adjei G, et al. Evaluation of the diagnostic accuracy of CareStart G6PD deficiency rapid diagnostic test (RDT) in a malaria endemic area in Ghana, Africa. PLoS One. 2015;10:e0125796. doi: 10.1371/journal.pone.0125796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moorthy VS, Hutubessy R, Newman RD, Hombach J. Decision-making on malaria vaccine introduction: the role of cost-effectiveness analyses. Bull World Health Organ. 2012;90:864–866. doi: 10.2471/BLT.12.107482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Seo MK, Baker P, Ngo KN-L. Cost-effectiveness analysis of vaccinating children in Malawi with RTS, S vaccines in comparison with long-lasting insecticide-treated nets. Malar J. 2014;13:66. doi: 10.1186/1475-2875-13-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tediosi F, Maire N, Penny M, Studer A, Smith TA. Simulation of the cost-effectiveness of malaria vaccines. Malar J. 2009;8:127. doi: 10.1186/1475-2875-8-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hanson K, Kikumbih N, Armstrong Schellenberg J, Mponda H, Nathan R, Lake S, et al. Cost-effectiveness of social marketing of insecticide-treated nets for malaria control in the United Republic of Tanzania. Bull World Health Organ. 2003;81:269–276. [PMC free article] [PubMed] [Google Scholar]
- 32.Paintain SL, Awini E, Addei S, Kukula V, Nikoi C, Sarpong D, et al. Evaluation of a universal long-lasting insecticidal net (LLIN) distribution campaign in Ghana: cost effectiveness of distribution and hang-up activities. Malar J. 2014;13:71. doi: 10.1186/1475-2875-13-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Crowell V, Briët OJ, Hardy D, Chitnis N, Maire N, Di Pasguale A, et al. Modeling the cost-effectiveness of mass screening and treatment for reducing Plasmodium falciparum malaria burden. Malar J. 2012;11:19. doi: 10.1186/1475-2875-11-S1-P19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Oliveira MRF, Giozza SP, Peixoto HM, Romero GAS. Cost-effectiveness of diagnostic for malaria in extra-Amazon Region. Brazil Malar J. 2012;11:390. doi: 10.1186/1475-2875-11-390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Oliveira MRF, Gomes AC, Toscano CM. Cost effectiveness of OptiMal® rapid diagnostic test for malaria in remote areas of the Amazon Region. Brazil Malar J. 2010;9:277. doi: 10.1186/1475-2875-9-277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lubell Y, Riewpaiboon A, Dondorp AM, von Seidlein L, Mokuolu OA, Nansumba M, et al. Cost-effectiveness of parenteral artesunate for treating children with severe malaria in sub-Saharan Africa. Bull World Health Organ. 2011;89:504–512. doi: 10.2471/BLT.11.085878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kyaw S, Drake T, Ruangveerayuth R, Chierakul W, White NJ, Newton PN, et al. Cost of treating inpatient falciparum malaria on the Thai-Myanmar border. Malar J. 2014;13:416. doi: 10.1186/1475-2875-13-416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Massad E, Behrens BC, Coutinho FAB, Behrens RH. Cost risk benefit analysis to support chemoprophylaxis policy for travellers to malaria endemic countries. Malar J. 2011;10:130. doi: 10.1186/1475-2875-10-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fundação de Medicina Tropical Dr. Heitor Vieira Dourado (FMT-HVD). Banco de dados—deficiência da glicose-6-fosfato-desidrogenase (2009–2011). Manaus: FMT-HVD; 2011.
- 40.Macauley C. Aggressive active case detection: a malaria control strategy based on the Brazilian model. Soc Sci Med. 2005;60:563–573. doi: 10.1016/j.socscimed.2004.05.025. [DOI] [PubMed] [Google Scholar]
- 41.Oliveira MRF. Cost-effectiveness analysis of rapid test for the diagnosis of new malaria cases in twelve endemic municipalities of the State of Pará. PhD thesis. Universidade de São Paulo, Faculdade de Saúde Pública; 2009.
- 42.Secretaria de Estado da Saúde do Amazonas (SES/AM). Tabela de vencimentos e gratificação de saúde. Manaus: SES/AM; 2013.
- 43.Secretaria de Vigilância em Saúde do Ministério da Saúde. Relação de compras de medicamentos para malária. Brasília, 2013.
- 44.Bosman A, Cunningham J. Proposal for an Evidence Review Group (ERG) on G6PD testing to support increased access to primaquine for radical cure of Plasmodium vivax and for malaria chemoprophylaxis. Geneva: World Health Organization; 2013. [Google Scholar]
- 45.Fundação de Medicina Tropical Dr. Heitor Vieira Dourado (FMT-HVD): Relação de compras de insumos laboratoriais. Manaus; 2013.
- 46.Ministério da Saúde: Banco de Preços em Saúde http://aplicacao.saude.gov.br/bps/login.jsf.
- 47.Alere™: Informação fornecida pela chefia de produtos usados em doenças crônicas. São Paulo; 2014.
- 48.Ministério da Saúde: Sistema de Gerenciamento da Tabela de Procedimentos, Medicamentos e OPM do SUS http://sigtap.datasus.gov.br/tabela-unificada/app/sec/inicio.jsp.
- 49.Ministério da Saúde: Sistema de Informação Hospitalar Descentralizados do SUS http://www2.datasus.gov.br/SIHD/.
- 50.Fundação de Medicina Tropical Dr . Heitor Vieira Dourado (FMT-HVD): Custos com a nutrição hospitalar. Manaus: FMT-HVD; 2013. [Google Scholar]


