Abstract
The number of births in the United States declined by 1% between 2012 and 2013, to a total of 3 932 181. The general fertility rate also declined 1% to 62.5 births per 1000 women, the lowest rate ever reported. The total fertility rate was down by 1% in 2013 (to 1857.5 births per 1000 women). The teenage birth rate fell to another historic low in 2013, 26.5 births per 1000 women. Birth rates also declined for women 20 to 29 years, but the rates rose for women 30 to 39 and were unchanged for women 40 to 44. The percentage of all births that were to unmarried women declined slightly to 40.6% in 2013, from 40.7% in 2012. In 2013, the cesarean delivery rate declined to 32.7% from 32.8% for 2012. The preterm birth rate declined for the seventh straight year in 2013 to 11.39%; the low birth weight (LBW) rate was essentially unchanged at 8.02%. The infant mortality rate was 5.96 infant deaths per 1000 live births in 2013, down 13% from 2005 (6.86). The age-adjusted death rate for 2013 was 7.3 deaths per 1000 population, unchanged from 2012. Crude death rates for children aged 1 to 19 years declined to 24.0 per 100 000 population in 2013, from 24.8 in 2012. Unintentional injuries and suicide were, respectively, the first and second leading causes of death in this age group. These 2 causes of death jointly accounted for 45.7% of all deaths to children and adolescents in 2013.
Note to Readers
This will be my last “Annual Summary.” After 20 years as a coauthor, organizer, and editor (1995–2014), it’s time to pass the baton to the next public health pediatrician on the team. Lest the casual reader think that I have overstayed my welcome, I remind you that Myron Wegman, authored this article for 45 years, from 1950 to 1994.
Our greatest accomplishment over this period has been to make the writing of the paper a collaboration between the academic and professional communities; namely, colleagues at the CDC National Center for Health Statistics who now coauthor the paper and assure its accuracy. Thus, many new data sets, features, and analyses were added.
I am gratified that the paper is widely read and quoted every year, and that the published data are far more accessible to the pediatricians than are government publications. Many thanks to the American Academy of Pediatrics, and to editors Jerry Lucey and Lewis First for their support.
I believe that future authors will make even greater strides by using new technologies (electronic birth and death certificate data and rapid communication of events to state agencies) to create more timely birth and death indicators to inform policy-makers and practitioners. Pediatricians need to support such developments, continue to use the information provided, and make their support for excellent national statistics known to policy-makers and agency leaders.
Bernard Guyer, Zanvyl Kreiger Professor of Children’s Health, Emeritus, Johns Hopkins Bloomberg School of Public Health.
INTRODUCTION
This annual article is a long-standing feature in Pediatrics and provides a summary of the most current vital statistics data for the United States. We also include a special feature this year on trends in racial and ethnic disparities in US infant mortality based on data from the linked birth/infant death file.
Methods
The data presented in this report were obtained from vital records: birth certificates, death certificates, and reports of fetal death for residents in all US states and the District of Columbia. More complete descriptions of vital statistics data systems are available elsewhere. 1 – 7
Birth and mortality data for 2013 and fetal mortality data for 2012 were collected by using both the 1989 (unrevised) and 2003 (revised) versions of the US Standard Certificates of Live Birth, the US Standard Certificate of Death, and the US Standard Report of Fetal Death. The 2003 revisions and specifics on the 2012 and 2013 revised and unrevised reporting areas are described in detail elsewhere. 3 , 4 , 8 – 10 All birth and mortality data items presented in this report are considered comparable between revisions, and revised and unrevised data are combined.
Current vital statistics patterns and recent trends are presented according to age, race, and Hispanic origin, as well as other birth and death characteristics. Hispanic origin and race are collected as separate items in vital records. Persons of Hispanic origin may be of any race. A number of reporting areas allow for multiple-race categories on birth and death certificates. However, until all areas revise their certificates to reflect updated reporting standards for race, multiple-race data were modified (the data were “bridged”) back to single-race categories. 1 , 3 , 4 , 11 – 13 For birth data, mother’s marital status was reported directly in all reporting areas except New York in 2013. Details about the reporting of marital status in New York and editing methods and imputations as applied to other items on the birth certificate are presented in publications of the National Center for Health Statistics (NCHS). 14
Cause-of-death statistics in this report are based solely on the underlying cause of death compiled in accordance with the International Classification of Diseases, 10th Revision (ICD- 10). 12 The underlying cause of death is defined as “(a) the disease or injury which initiated the train of morbid events leading directly to death, or (b) the circumstances of the accident or violence which produced the fatal injury.” 15
Ranking for leading causes of death is based on number of deaths. 16 Infant mortality refers to the death of an infant younger than 1 year. Infant mortality rates (IMRs) were computed by dividing the total number of infant deaths in each calendar year by the total number of live births in the same year. 4 Neonatal mortality rates (NMRs) are shown for infant deaths that occurred at <28 days, and postneonatal mortality rates (PNMRs) for infant deaths that occurred 28 days to <1 year of age. 4 The denominator for both rates is the number of live births. Perinatal mortality rates (PMRs) include fetal deaths at ≥28 weeks of gestation and infant deaths at <7 days of age. 2 Fetal mortality rates (FMRs) are shown for fetal deaths at ≥20 and at ≥28 weeks of gestation. 2 FMRs and PMRs were computed by dividing the number of fetal or perinatal deaths by the number of live births plus specified fetal deaths. 2
The latest infant mortality statistics according to race and Hispanic origin are from the 2012 period–linked birth/infant death data. 17 In this data set, the death certificate is linked with the corresponding birth certificate for each infant who died in the United States in 2012. Birth and infant death certificates are linked in each state vital statistics office based on matching of common data fields, such as infant’s name and address, date of birth, and so forth. The quality of the links is validated at NCHS, and records with questionable linkages are sent back to states for correction. Approximately 99% of all infant deaths are linked to their matching birth certificates. A record weight is computed separately by state and age at death, and is used to adjust for the 1% of records that could not be linked to their matching birth certificates. 17 The purpose of this linkage is to use additional variables available from the birth certificate, such as birth weight, to better interpret infant mortality patterns. The linked data also provides improved quality of race and ethnicity reporting because the information is ascertained directly from the mother.
The denominators for the calculation of birth (per 1000 population), death (per 1000 population), and fertility rates (per 1000 women aged 15 to 44 years of age) are population estimates based on the 2010 census as of July 1, 2013, provided by the US Census Bureau and produced under a collaborative arrangement with NCHS. 1 To calculate a consistent series of birth and death rates, the population estimates for multiple-race persons are “bridged” to be consistent with 1977 Office of Management and Budget (OMB) race categories. 18 The modification procedures are described in detail elsewhere. 12 , 13
Data for the international comparisons of births and IMRs were obtained primarily from the 2012 United Nations Demographic Yearbook 19 and Organisation for Economic Co-operation and Development (OECD) iLibrary Health. 20
Natural Increase
In 2013, >1.3 million persons were added to the US population as a result of natural increase, the excess of births over deaths (Table 1). 1 , 3 , 4 The rate of natural increase in 2013 was 4.2 persons per 1000 population.
TABLE 1.
Vital Statistics Measures of Fertility and Mortality in the United States, Selected Years: 1950–2013
| Number | Rate a | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2013 | 2012 | 2011 | 2013 | 2012 | 2011 | 2000 | 1990 | 1980 | 1950 | |
| Live births | 3 932 181 | 3 952 841 | 3 953 590 | 12.4 | 12.6 | 12.7 | 14.4 | 16.7 | 15.9 | 24.1 |
| Fertility rate | NA | NA | NA | 62.5 | 63.0 | 63.2 | 65.9 | 70.9 | 68.4 | 106.2 |
| Deaths | 2 596 993 | 2 543 279 | 2 515 458 | — | 8.1 | 8.1 | 8.5 | 8.6 | 8.8 | 9.6 |
| Age-adjusted rate | NA | NA | NA | — | 7.3 | 7.4 | 8.7 | 9.4 | 10.4 | 14.5 |
| Natural Increase | 1 335 188 | 1 409 562 | 1 438 132 | — | 4.5 | 4.6 | 5.9 | 8.1 | 7.1 | 14.5 |
| Infant mortality | — | 23 629 | 23 985 | — | 5.98 | 6.07 | 6.91 | 9.22 | 12.60 | 29.21 |
| Population base, in thousands | NA | NA | NA | 316 129 | 313 914 | 311 592 | 281 422 | 248 710 | 226 546 | 150 697 |
Populations are as of July 1 for 2013, 2012, and 2011, and as of April 1 in 2010, 2000, 1990, 1980, and 1950. Data sources: Centers for Disease Control and Prevention/NCHS, National Vital Statistics System, and the US Census Bureau. NA, not applicable; —, data not available.
Rates per 1000 population except for fertility, which is per 1000 women aged 15 to 44 years of age, and infant mortality, which is per 1000 live births.
Births
In 2013, the number of births for the United States was 3 932 181, 1% fewer than in 2012 and 2011 (Table 1). 1 The general fertility rate (the number of births per 1000 women aged 15–44 years) also declined (by 1%) to a record low of 62.5 in 2013, from 63.0 in 2012. In 2013, the total fertility rate (TFR) was 1857.5 births per 1000 women, down 1% compared with the rate in 2012 (1880.5) (Table 2). The TFR estimates the number of births that a hypothetical group of 1000 women would have over their lifetimes, based on the age-specific birth rates observed in a given year. The TFR has been below replacement (2100 per 1000 women; the number of births needed to maintain the size of a population) since 1972, with the exception of 2006 and 2007. 1 Birth rates declined among women age 15 to 29 between 2012 and 2013, reaching historic lows for ages 15 to 19, 20 to 24, and 25 to 29. Rates rose for women age 30 to 34, 35 to 39, and 45 to 49, and remained unchanged for age 40 to 44. 1
TABLE 2.
Age-Specific Birth Rates and TFRs by Race and Hispanic Origin of Mother: United States, 2013
| Age-Specific Birth Rate by Age of Mother a | TFR b | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 15–44 y c | 15–17 y | 18–19 y | 20–24 y | 25–29 y | 30–34 y | 35–39 y | 40–44 y | ||
| Total | 62.5 | 12.3 | 47.1 | 80.7 | 105.5 | 98.0 | 49.3 | 10.4 | 1857.5 |
| Non-Hispanic white | 58.7 | 7.4 | 35.0 | 68.3 | 103.5 | 101.9 | 48.0 | 9.1 | 1751.0 |
| Non-Hispanic black | 64.6 | 18.9 | 67.0 | 105.6 | 102.7 | 77.3 | 40.3 | 9.9 | 1881.5 |
| Native American d , e | 46.4 | 15.9 | 53.3 | 78.9 | 75.6 | 50.4 | 24.7 | 5.5 | 1334.5 |
| Asian or Pacific Islander e | 59.2 | 3.7 | 16.1 | 39.1 | 89.5 | 114.6 | 66.6 | 16.1 | 1681.0 |
| Hispanic f | 72.9 | 22.0 | 70.8 | 107.2 | 119.1 | 94.8 | 52.4 | 13.3 | 2149.0 |
Race and Hispanic origin are reported separately on birth certificates. Persons of Hispanic origin may be of any race. Race categories are consistent with the 1977 OMB standards. Forty-one states and the District of Columbia reported multiple-race data in 2013. Multiple-race data for these states were bridged to the single-race categories of the 1977 OMB standards for comparability with other states. Data source: Centers for Disease Control and Prevention/NCHS, National Vital Statistics System, natality.
Rates per 1000 women in age-specific group.
Sum of age-specific birth rates times 5 (includes rates for ages 10–14, 15–19 and 45–49 y, not shown separately).
Relates the number of births to women of all ages to women aged 15–44 years.
Includes births to Aleuts and Eskimos.
Includes persons of Hispanic, non-Hispanic, and origin not stated according to mother’s reported race.
Includes all persons of Hispanic origin of any race.
Trends in Race- and Ethnicity-Specific Fertility Rates
The general fertility rate decreased for 2 of the 3 largest race and Hispanic-origin groups in 2013, declining 1% for non-Hispanic black women (from 65.0 per 1000 women aged 15 to 44 in 2012) and 2% for Hispanic women (from 74.4 in 2012). 1 The general fertility rate for non-Hispanic white women rose <1% from 58.6 in 2012. The rate for American Indian or Alaska Native women declined 1% in 2013 (from 47.0 in 2012); the rate for Asian or Pacific Islander women declined 5% (from 62.2 in 2012). Fertility rates for these 5 groups ranged from 46.4 births per 1000 women aged 15 to 44 for American Indian or Alaska Native women to a high of 72.9 for Hispanic women in 2013 (Table 2).
Trends in Age-Specific Birth Rates
Teenaged Childbearing
The teenage birth rate (15–19 years) dropped 10% from 2012 to 2013, reaching another historic low for the United States: 26.5 births per 1000 women (Table 3). 1 The teenage birth rate has dropped 36% from 2007 and 57% from 1991, the most recent peak. The birth rate for teenagers aged 15 to 17 years dropped 13% from 2012, to 12.3 per 1000 in 2013, whereas the birth rate for older teenagers aged 18 to 19 years dropped 8% to 47.1 per 1000 (Table 3).
TABLE 3.
Birth Rates for Teens According to Age, Race, and Hispanic Origin, United States, Selected Years: 1991–2013
| Age, Race, and Hispanic Origin of Mother | Birth Rate a | Percent Change | ||||||
|---|---|---|---|---|---|---|---|---|
| 2013 | 2012 | 2011 | 2007 | 1991 | 2012–2013 | 2007–2013 | 1991–2013 | |
| 15–19 y | ||||||||
| All races | 26.5 | 29.4 | 31.3 | 41.5 | 61.8 | −10 | −36 | −57 |
| Non-Hispanic white b | 18.6 | 20.5 | 21.7 | 27.2 | 43.4 | −9 | −32 | −57 |
| Non-Hispanic black b | 39.0 | 43.9 | 47.3 | 62.0 | 118.2 | −11 | −37 | −67 |
| Native American c , d | 31.1 | 34.9 | 36.1 | 49.3 | 84.1 | −11 | −37 | −63 |
| Asian or Pacific Islander d | 8.7 | 9.7 | 10.2 | 14.8 | 27.3 | −10 | −41 | −68 |
| Hispanic b , e | 41.7 | 46.3 | 49.6 | 75.3 | 104.6 | −10 | −45 | −60 |
| 15–17 y | ||||||||
| All races | 12.3 | 14.1 | 15.4 | 21.7 | 38.6 | −13 | −43 | −68 |
| Non-Hispanic white b | 7.4 | 8.4 | 9.0 | 11.9 | 23.6 | −12 | −38 | −69 |
| Non-Hispanic black b | 18.9 | 21.9 | 24.6 | 34.6 | 86.1 | −14 | −45 | −78 |
| Native American c , d | 15.9 | 17.0 | 18.2 | 26.2 | 16.3 | −6 | −39 | −2 |
| Asian or Pacific Islander d | 3.7 | 4.1 | 4.6 | 7.4 | 51.9 | −10 | −50 | −93 |
| Hispanic b , e | 22.0 | 25.5 | 28.0 | 44.4 | 69.2 | −14 | −50 | −68 |
| 18–19 y | ||||||||
| All races | 47.1 | 51.4 | 54.1 | 71.7 | 94.0 | −8 | −34 | −50 |
| Non-Hispanic white b | 35.0 | 37.9 | 39.9 | 50.4 | 70.6 | −8 | −31 | −50 |
| Non-Hispanic black b | 67.0 | 74.1 | 78.8 | 105.2 | 162.2 | −10 | −36 | −59 |
| Native American c , d | 53.3 | 60.5 | 61.6 | 86.4 | 42.2 | −12 | −38 | 26 |
| Asian or Pacific Islander d | 16.1 | 17.7 | 18.1 | 24.9 | 134.2 | −9 | −35 | −88 |
| Hispanic b , e | 70.8 | 77.2 | 81.5 | 124.7 | 155.5 | −8 | −43 | −54 |
Race and Hispanic origin are reported separately on birth certificates. Persons of Hispanic origin may be of any race. Race categories are consistent with the 1977 OMB standards. Forty-one states and the District of Columbia in 2013, 38 states and the District of Columbia in 2010, 33 states and the District of Columbia in 2009, and 27 states in 2007 reported multiple-race data. Multiple-race data for these states were bridged to the single-race categories of the 1977 OMB standards for comparability with other states. Data sources: Centers for Disease Control and Prevention/NCHS, National Vital Statistics System, and the US Census Bureau.
Rates per 1000 women in specified group.
In 1991 excludes data for New Hampshire, which did not report Hispanic origin on the birth certificate.
Includes births to Aleuts and Eskimos.
Includes persons of Hispanic, non-Hispanic, and origin not stated according to mother’s reported race.
Includes all persons of Hispanic origin of any race.
Childbearing for Women in Their 20s and 30s
The birth rate for women aged 20 to 24 years fell to a record low in the United States in 2013, 80.7 births per 1000 women, a 3% drop from 83.1 in 2012. 1 The rate for women aged 25 to 29 years also fell (1%) in 2013 to 105.5 (Table 2). The birth rate for women aged 30 to 34 rose 1% from 2012 to 2013, from 97.3 to 98.0 births per 1000 women. The birth rate for women aged 35 to 39 rose 2% in 2013, to 49.3 per 1000 women from 48.3 in 2012. 1
Childbearing for Women 40 and Older
The birth rate for women aged 40 to 44 years was 10.4 births per 1000 women in 2013, unchanged from 2012 (Table 2). 1 The rate for women aged 45 to 49 years increased to 0.8 in 2013 from 0.7 in 2012 (data not shown). The rates have slowly, although steadily, increased for both groups since 1990. 1
Unmarried Mothers
The birth rate for unmarried women fell for the fifth consecutive year in 2013, to 44.3 births per 1000 unmarried women aged 15 to 44 years (a decrease of 14% since 2008). 1 The total number of births to unmarried women declined 1% in 2013, to 1 595 873. The percentage of all births to unmarried women was 40.6% in 2013, slightly lower than in 2012 (40.7%). The percentage of births that were to unmarried women declined for non-Hispanic black and Hispanic births, and was statistically unchanged for the remaining population groups between 2012 and 2013 (Table 4). In 2013, unmarried teenagers (age 15 to 19) accounted for 15% of all nonmarital births, the lowest proportion ever reported.
TABLE 4.
Percentage of Births With Selected Characteristics by Race and Hispanic Origin of Mother, United States, Selected Years: 1990, 2012, and 2013
| All Races | Non-Hispanic White | Non-Hispanic Black | Hispanic a | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2013 | 2012 | 1990 | 2013 | 2012 | 1990 | 2013 | 2012 | 1990 b | 2013 | 2012 | 1990 | |
| Mother | ||||||||||||
| <20 y of age | 7.0 | 7.8 | 12.8 | 5.1 | 5.7 | 9.6 | 10.8 | 12.4 | 23.2 | 10.5 | 11.5 | 16.8 |
| ≥40 y of age | 2.8 | 2.8 | 1.2 | 2.9 | 2.9 | 1.2 | 2.6 | 2.5 | 0.8 | 2.9 | 2.7 | 1.2 |
| Unmarried | 40.6 | 40.7 | 28.0 | 29.3 | 29.3 | 16.9 | 71.5 | 72.1 | 66.7 | 53.2 | 53.5 | 36.7 |
| Diabetes during pregnancy | 6.0 | 5.9 | 2.1 | 5.4 | 5.3 | 2.2 | 5.4 | 5.2 | 1.8 | 6.5 | 6.3 | 2.0 |
| Pregnancy-associated | ||||||||||||
| Hypertension | 4.8 | 4.6 | 2.7 | 5.2 | 5.0 | 3.0 | 5.9 | 5.7 | 2.8 | 3.8 | 3.6 | 1.8 |
| Health care utilization | ||||||||||||
| Midwife-attended births c | 8.2 | 7.9 | 3.9 | 8.5 | 8.2 | 3.2 | 7.2 | 7.1 | 4.4 | 8.1 | 8.0 | 6.2 |
| Cesarean delivery rate | 32.7 | 32.8 | 22.7 | 32.0 | 32.3 | 23.4 | 35.8 | 35.8 | 22.1 | 32.2 | 32.2 | 21.2 |
| Weight gain of more than 40 lb d | 21.2 | 21.1 | 15.9 | 23.9 | 23.7 | 16.5 | 21.4 | 21.1 | 14.8 | 16.6 | 16.7 | 14.1 |
| Infant | ||||||||||||
| Birth weight | ||||||||||||
| LBW e | 8.0 | 8.0 | 7.0 | 7.0 | 7.0 | 5.6 | 13.1 | 13.2 | 13.3 | 7.1 | 7.0 | 6.1 |
| VLBW e | 1.4 | 1.4 | 1.3 | 1.1 | 1.1 | 0.9 | 2.9 | 2.9 | 2.9 | 1.2 | 1.2 | 1.03 |
| Gestational age | ||||||||||||
| Preterm birth f | 11.4 | 11.5 | 10.6 | 10.2 | 10.3 | 8.5 | 16.3 | 16.5 | 18.9 | 11.3 | 11.6 | 11.0 |
| Early f | 3.4 | 3.4 | 3.3 | 2.9 | 2.9 | 2.4 | 5.9 | 5.9 | 7.4 | 3.4 | 3.3 | 3.2 |
| Late f | 8.0 | 8.1 | 7.3 | 7.3 | 7.4 | 6.1 | 10.4 | 10.6 | 11.5 | 8.0 | 8.3 | 7.8 |
| Multiple births | ||||||||||||
| Live births in twin deliveries (per 1000 live births) | 33.7 | 33.1 | 22.6 | 36.7 | 36.8 | 22.9 | 38.3 | 36.9 | 26.7 | 23.9 | 20.4 | 18.0 |
| Live births in higher-order multiple deliveries (per 100 000 live births) | 119.5 | 124.4 | 72.8 | 147.2 | 152.9 | 89.8 | 106.7 | 107.8 | 46.2 | 71.4 | 114.4 | 39.4 |
Race and Hispanic origin are reported separately on birth certificates. Persons of Hispanic origin may be of any race. Race categories are consistent with the 1977 OMB standards. Forty-four states and the District of Columbia in 2013 and 41 states and the District of Columbia in 2012 reported multiple-race data. Multiple-race data for these states were bridged to the single-race categories of the 1977 OMB standards for comparability with other states. Data sources: Centers for Disease Control and Prevention/NCHS, National Vital Statistics System, and the US Census Bureau.
Includes all persons of Hispanic origin of any race.
Excludes data for New Hampshire and Oklahoma, which did not report Hispanic origin.
Delivered by certified nurse midwives.
Mother gained >40 pounds during pregnancy.
VLBW, very low birth weight, is birth weight of <1500 g (3 lb, 4 oz), and LBW is birth weight of <2500 g (5 lb, 8 oz).
Preterm indicates birth before 37 completed weeks of gestation, early preterm indicates birth before 34 completed weeks of gestation, and late preterm indicates birth between 34 and 36 completed weeks of gestation.
Cesarean Delivery
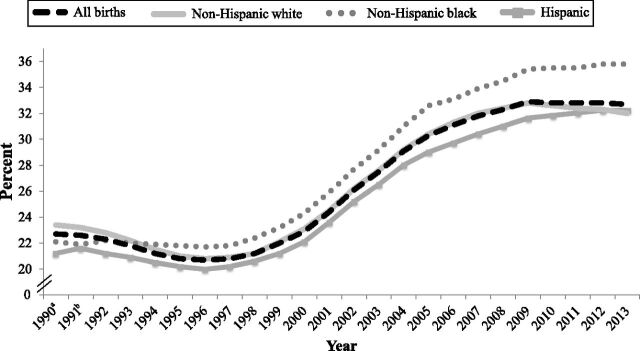
The cesarean delivery rate declined to 32.7% in 2013 from 32.8% for 2012 (Table 4). The rate peaked at 32.9% in 2009, following steady increases from 1996. 1 The decline in cesarean delivery rates was a continuation of the trend for the fourth consecutive year for non-Hispanic white women (to 32.0%), but rates were unchanged for non-Hispanic black (35.8%) and Hispanic (32.2%) women (Fig 1). For the first time in 2013, non-Hispanic white women have a lower cesarean delivery rate than Hispanic women; since 1994, non-Hispanic black women have had the highest rates of cesarean delivery. 1
FIGURE 1.
Cesarean delivery rates, by race and Hispanic origin: United States, 1990–2013. aExcludes data for New Hampshire and Oklahoma, which did not report data by Hispanic origin. Oklahoma did not report method of delivery. bExcludes data for New Hampshire, which did not report data by Hispanic origin. Source: Centers for Disease Control and Prevention/NCHS, National Vital Statistics System.
Multiple Births
In 2013, the twin birth rate rose 2% to 33.7 twins per 1000 total births, from 33.1 in 2012 (Table 4); the rate has been relatively stable since 2009. 1 The twin birth rate rose steadily by 76% overall from 1980 to 2009. The rate increased nearly 3% annually during the 1990s but slowed to less than one-half of 1% annually since the mid-2000s. 1 The triplet/+ rate (the number of births in triplet and higher-order multiples per 100 000 total births) was 119.5 per 100 000 total births in 2013, a drop of 4% from 2012 (119.5) (Table 4), and the lowest since 1995. The triplet/+ rate increased by 400% during the 1980s and 1990s, but has declined 38% since the 1998 peak (193.5).
Infants in multigestation pregnancies are much more likely to be born earlier and smaller than those born in singleton pregnancies. Accordingly, they are at greater risk of early death, with twins ∼5 times and triplets ∼10 times as likely to die in infancy. 21 In 2013, >1 of every 2 twins, and 9 of 10 triplets were delivered preterm, compared with ∼1 in 10 singletons. 1
Preterm Birth
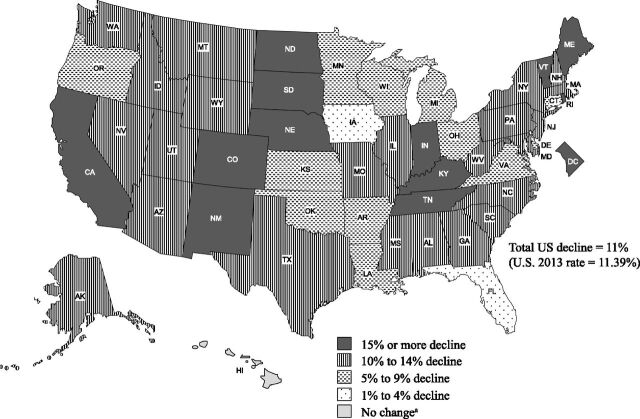
In 2013, the preterm birth rate (infants delivered at <37 completed weeks of gestation per 100 births) was 11.39%, down for the seventh straight year. 1 The rate was 11.55% in 2012. The preterm rate rose until 2006, increasing by more than one-third from 1981 to 2006. 1 Although the lowest level in more than a decade, the 2013 rate of preterm birth is still higher than rates during the 1980s and most of the 1990s. Since 2006, state-specific declines in preterm birth rates have been widespread (Fig 2), with decreases in 49 states and the District of Columbia. Rates for 12 states and the District of Columbia declined 15% or more during this time, rates for 23 additional states declined 10% to 14%. 1
FIGURE 2.
Percent change in preterm birth rates by state: United States, 2006 and 2013. aChange not significant at P = .05. Note: Preterm is <37 completed weeks of gestation. Source: Centers for Disease Control and Prevention/NCHS, National Vital Statistics System.
Low Birth Weight
The LBW (<2500 g) rate was 8.02% in 2013, essentially unchanged from 2012 (Table 4). The percentage of infants born LBW increased more than 20% from the mid-1980s through 2006, but has declined slowly, by 3%, from 2006 through 2013. 1 The very low birth weight (<1500 g) rate was essentially stable at 1.41% in 2013, whereas the moderately low birth weight (1500 to 2499 g) rate increased slightly to 6.61%. The LBW rate increased slightly between 2012 and 2013 for Hispanic infants, but was not significantly changed for non-Hispanic white and non-Hispanic black infants (Table 4).
Notwithstanding the small decrease in the percentage of births at <2500 g from 2006 to 2013, the US birth weight distribution has shifted downward over the past 2 decades, reflecting increases in births <3500 g and declines in births at >3500 g. 1
Fetal and Perinatal Mortality
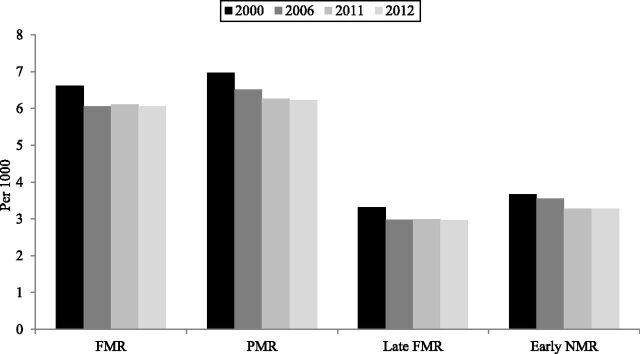
In 2012, 24 073 fetal deaths of ≥20 weeks of gestation were reported in the United States. The 2012 FMR (fetal deaths per 1000 live births plus fetal deaths) was 6.05 per 1000 live births plus fetal deaths, not significantly different from the 2011 level of 6.11. No significant changes were observed between 2011 and 2012 in either early- (3.11 for 2012) or late fetal mortality (2.96). Following declines from 1990 to 2006, the overall FMR was unchanged from 2006 through 2012 (see Fig 3). 2
FIGURE 3.
Fetal mortality, perinatal mortality, late-fetal mortality, and early NMRs: 2000, 2006, 2011, and 2012. Note: FMR indicates fetal deaths per 1000 live births plus fetal deaths; early FMR, early-fetal deaths (20–27 weeks) per 1000 live births plus fetal deaths; late FMR, late fetal deaths (≥28 weeks) per 1000 live births plus fetal deaths; PMR, late-fetal deaths and early neonatal (<7 days of age) deaths per 1000 live births plus fetal deaths; early NMR, early-neonatal (<7 days of age) deaths per 1000 live births. Source: Centers for Disease Control and Prevention/NCHS, National Vital Statistics System.
The 2012 PMR was 6.22, statistically unchanged from 6.26 in 2011 but down 4% from 2006 and 11% from 2000 (Fig 3). The decline in the PMR for 2006–2012 was almost entirely the result of declines in early neonatal mortality (3.55 in 2006 and 3.22 in 2012), as the late-fetal mortality rate was unchanged over this period.
Infant Mortality
In 2013, a total of 23 440 infant deaths were reported in the United States with approximately two-thirds of infant deaths occurring during the neonatal period. 3 The IMR was 5.96 infant deaths per 1000 live births (IMR was 5.98 in 2012); NMR was 4.04 neonatal deaths per 1000 live births (NMR was 4.01 in 2012) (Table 5); and PNMR was 1.93 postneonatal deaths per 1000 live births (PNMR was 1.97 in 2012) (data not shown). The changes in IMRs between 2012 and 2013 were not significant. The IMR fell slowly but steadily between 2005 and 2013, however. Over this period, the IMR decreased 13.2%, the NMR decreased 11.0%, and the PNMR decreased 17.5%.
TABLE 5.
Percent Preterm and Percent LBW, IMR, and NMR, United States and Each State, 2013
| State of Residence | Preterm a | LBW b | IMR c | NMR d |
|---|---|---|---|---|
| United States | 11.39 | 8.02 | 5.96 | 4.04 |
| Alabama | 15.10 | 9.99 | 8.61 | 5.54 |
| Alaska | 10.03 | 5.75 | 5.59 | 2.53 |
| Arizona | 11.64 | 6.90 | 5.27 | 3.41 |
| Arkansas | 12.71 | 8.76 | 7.61 | 4.44 |
| California | 8.83 | 6.82 | 4.76 | 3.33 |
| Colorado | 10.30 | 8.80 | 5.09 | 3.68 |
| Connecticut | 9.83 | 7.82 | 4.68 | 3.19 |
| Delaware | 12.41 | 8.31 | 6.28 | 4.34 |
| District of Columbia | 13.32 | 9.43 | 6.78 | 4.84 |
| Florida | 13.55 | 8.52 | 6.16 | 4.02 |
| Georgia | 12.71 | 9.45 | 6.94 | 4.75 |
| Hawaii | 12.55 | 8.23 | 6.53 | 4.58 |
| Idaho | 10.46 | 6.91 | 5.63 | 3.66 |
| Illinois | 11.75 | 8.22 | 6.00 | 4.07 |
| Indiana | 10.99 | 7.91 | 7.22 | 4.58 |
| Iowa | 11.06 | 6.55 | 4.14 | 2.69 |
| Kansas | 10.81 | 7.01 | 6.44 | 4.33 |
| Kentucky | 12.63 | 8.70 | 6.38 | 3.91 |
| Louisiana | 15.10 | 10.92 | 8.65 | 5.09 |
| Maine | 9.32 | 7.13 | 7.04 | 4.23 |
| Maryland | 11.88 | 8.47 | 6.63 | 4.54 |
| Massachusetts | 10.01 | 7.70 | 4.15 | 3.08 |
| Michigan | 11.65 | 8.23 | 7.04 | 4.80 |
| Minnesota | 9.85 | 6.37 | 5.05 | 3.59 |
| Mississippi | 16.57 | 11.54 | 9.65 | 5.88 |
| Missouri | 11.3 | 8.02 | 6.52 | 4.34 |
| Montana | 10.55 | 7.38 | 5.66 | 2.91 |
| Nebraska | 10.57 | 6.45 | 5.33 | 3.68 |
| Nevada | 12.60 | 8.02 | 5.45 | 3.65 |
| New Hampshire | 9.01 | 6.79 | 5.65 | 4.03 |
| New Jersey | 11.51 | 8.26 | 4.48 | 3.19 |
| New Mexico | 11.63 | 8.88 | 5.46 | 4.02 |
| New York | 10.72 | 7.96 | 4.92 | 3.51 |
| North Carolina | 12.01 | 8.77 | 6.99 | 5.03 |
| North Dakota | 9.90 | 6.41 | 6.13 | 4.81 |
| Ohio | 12.06 | 8.51 | 7.33 | 5.20 |
| Oklahoma | 12.79 | 8.06 | 6.82 | 4.07 |
| Oregon | 9.33 | 6.29 | 4.96 | 3.43 |
| Pennsylvania | 10.71 | 8.01 | 6.66 | 4.82 |
| Rhode Island | 10.20 | 6.91 | 6.48 | 4.26 |
| South Carolina | 13.75 | 9.69 | 6.85 | 4.63 |
| South Dakota | 10.82 | 6.26 | 6.53 | 3.92 |
| Tennessee | 12.61 | 9.14 | 6.80 | 4.18 |
| Texas | 12.29 | 8.31 | 5.84 | 3.91 |
| Utah | 10.17 | 7.00 | 5.16 | 3.59 |
| Vermont | 8.12 | 6.72 | 4.35 | — e |
| Virginia | 11.02 | 8.01 | 6.21 | 4.41 |
| Washington | 9.72 | 6.41 | 4.48 | 3.03 |
| West Virginia | 12.48 | 9.40 | 7.59 | 4.51 |
| Wisconsin | 10.37 | 7.01 | 6.24 | 4.49 |
| Wyoming | 11.57 | 8.64 | 4.58 | 2.88 |
Data source: Centers for Disease Control and Prevention/NCHS, National Vital Statistics System, natality and mortality.
Preterm birth is <37 wk of completed gestation.
LBW is <2500 g.
Infant deaths (<1 y) per 1000 live births.
Neonatal deaths (<28 d) per 1000 live births.
Figure does not meet standards of reliability or precision; based on fewer than 20 deaths in the numerator.
Geographic Variation in Infant Outcomes
For 2013, Mississippi had the highest LBW (11.5%) and preterm (16.6%) rates, whereas Alaska had the lowest LBW (5.8%) rate and Vermont the lowest preterm rate (8.1%) (Table 5). States in the southeastern United States had the highest infant and NMRs. In 2013, state IMRs ranged from 4.14 per 1000 in Iowa to 9.65 in Mississippi. The IMR for the District of Columbia was 6.78. These geographic patterns have been observed for many years.
Leading Causes of Infant Death
In 2013, 56.6% of all infant deaths (Table 6) were attributable to 5 leading causes: congenital malformations, deformations, and chromosomal abnormalities (20.3%); disorders related to short gestation and LBW, not elsewhere classified (17.9%); newborn affected by maternal complications of pregnancy (6.8%); sudden infant death syndrome (6.7%); and accidents (unintentional injuries) (4.9%). 3 These 5 leading causes of infant death are the same as in 2012. 4 Newborns affected by maternal complications of pregnancy, the fourth leading cause in 2012, became the third leading cause in 2013, whereas sudden infant death syndrome, the third leading cause in 2012, became the fourth leading cause in 2013.
TABLE 6.
Deaths, Percentages of Total Deaths, and Mortality Rates for the 10 Leading Causes of Infant Death: United States, 2013 and 2012
| Causes of Death and ICD-10 Codes 12 | Rank a | 2013 | 2012 | ||||
|---|---|---|---|---|---|---|---|
| n | % | Rate b | n | % | Rate b | ||
| All causes | — | 23 440 | 100.0 | 596.1 | 23 629 | 100.0 | 597.8 |
| Congenital malformations, deformations and chromosomal abnormalities (Q00–Q99) | 1 | 4758 | 20.3 | 121.0 | 4939 | 20.9 | 124.9 |
| Disorders related to short gestation and LBW, not elsewhere classified (P07) | 2 | 4202 | 17.9 | 106.9 | 4202 | 17.8 | 106.3 |
| Newborn affected by maternal complications of pregnancy (P01) | 3 | 1595 | 6.8 | 40.6 | 1507 | 6.4 | 38.1 |
| Sudden infant death syndrome (R95) | 4 | 1563 | 6.7 | 39.7 | 1679 | 42.5 | 42.5 |
| Accidents (unintentional injuries) (V01–X59) | 5 | 1156 | 4.9 | 29.4 | 1169 | 4.9 | 29.6 |
| Newborn affected by complications of placenta, cord, and membranes (P02) | 6 | 953 | 4.1 | 24.2 | 1018 | 4.3 | 25.8 |
| Bacterial sepsis of newborn (P36) | 7 | 578 | 2.5 | 14.7 | 566 | 2.4 | 14.3 |
| Respiratory distress of newborn (P22) | 8 | 522 | 2.2 | 13.3 | 504 | 2.1 | 12.8 |
| Diseases of the circulatory system (I00-I99) | 9 | 458 | 2.0 | 11.6 | 492 | 2.1 | 12.4 |
| Neonatal hemorrhage (P50–P52,P54) | 10 | 389 | 1.7 | 9.9 | 422 | 1.8 | 10.7 |
Data source: Centers for Disease Control and Prevention / NCHS, National Vital Statistics System: mortality, 2013 and 2012 ( www.cdc.gov/nchs/deaths.htm ). —, data are not applicable.
Rank is based on 2013 data.
IMRs are per 100 000 live births.
See the special discussion later in this article on infant mortality by race and ethnicity for more detail on infant mortality.
International Comparisons
The number of births for 2011 and IMRs for 2010, 2011, and 2012 are shown in Table 7 for the United States and 28 other countries with at least 40 000 births and an IMR less than the US rate in the years for which data were available. The number of births for 2011 was obtained from the United Nations Demographic Yearbook 2011–2012; IMRs were obtained from OECD, the United Nations Demographic Yearbook 2011–2012, and from individual country Web sites. 19 , 20 , 22 , 23 Births are shown for 2011 because data were available for all countries included in the table for 2011 but were not available for 9 countries in 2012. The table shows countries ordered from the lowest to highest IMR in 2012. Twenty-six countries with at least 40 000 births had lower IMRs than the United States in 2012. Eight countries had an IMR less than half the US rate in 2012, and only 1 country besides the United States reported an IMR >5 infant deaths per 1000 live births. Although differences in the reporting of live births continue to play a role in infant mortality differences, other factors may contribute to the higher US IMR as well, including the higher percentage of preterm births in the United States and higher IMRs for infants born at 37 weeks of gestation or more. 24 – 28
TABLE 7.
Number of Live Births for 2011 and IMRs for 2010, 2011, and 2012 for 29 Countries
| Country | No. of Births in 2011 a | IMR b | ||
|---|---|---|---|---|
| 2012 | 2011 | 2010 | ||
| Per 1000 Live Births | ||||
| Japan | 1 050 806 | 2.2 | 2.3 | 2.3 |
| Finland | 59 676 | 2.4 | 2.4 | 2.3 |
| Norway | 60 220 | 2.5 | 2.4 | 2.8 |
| Sweden | 111 770 | 2.6 | 2.1 | 2.5 |
| Czech Republic | 108 673 | 2.6 | 2.7 | 2.7 |
| Italy | 546 607 | 2.9 | 2.9 | 3.2 |
| Republic of Korea | 471 265 | 2.9 | 3.0 | 3.2 |
| Greece | 106 428 | 2.9 | 3.4 | 3.8 |
| Spain | 470 553 | 3.1 | 3.2 | 3.2 |
| Austria | 78 109 | 3.2 | 3.6 | 3.9 |
| Germany | 662 685 | 3.3 | 3.6 | 3.4 |
| Australia | 301 617 | 3.3 | 3.8 | 4.1 |
| Portugal | 98 856 | 3.4 | 3.1 | 2.5 |
| Denmark | 58 998 | 3.4 | 3.5 | 3.4 |
| France | 792 996 | 3.5 | 3.5 | 3.6 |
| Ireland | 74 650 | 3.5 | 3.5 | 3.6 |
| Israel | 166 296 | 3.6 | 3.5 | 3.7 |
| Switzerland | 80 808 | 3.6 | 3.8 | 3.8 |
| Netherlands | 180 060 | 3.7 | 3.6 | 3.8 |
| Belgium | 128 678 | 3.8 | 3.4 | 3.6 |
| United Kingdom | 807 776 | 4.1 | 4.3 | 4.2 |
| Cuba | 133 067 | 4.2 c | 4.9 a | 4.5 a |
| Croatia | 41 197 | — d | 5.3 a | 4.5 a |
| New Zealand | 61 403 | 4.6 e | 5.2 | 5.5 |
| Poland | 388 416 | 4.6 | 4.7 | 5.0 |
| Canada | 377 636 | — d | 4.8 | 5.0 |
| Hungary | 88 049 | 4.9 | 4.9 | 5.3 |
| Slovak Republic | 60 813 | 5.8 | 4.9 | 5.7 |
| United States | 3 953 590 f | 6.0 f | 6.1 f | 6.1 f |
Deaths
There were a total of 2 596 993 deaths in the United States in 2013 (Table 1), 53 714 more than in 2012. Age-adjusted death rates are better indicators of the risk of mortality over time than crude death rates, because they control for changes in the age distribution of the US population, especially given increases in the elderly population. The age-adjusted death rate of 7.3 deaths per 1000 US standard population. 3
The 2013 life tables show a difference in life expectancy at birth by gender, race, and Hispanic origin. Hispanic women have the highest life expectancy at birth (83.8 years), followed by non-Hispanic white women (81.2 years), Hispanic men (79.1 years), non-Hispanic black women (78.1), non-Hispanic white men (76.5), and non-Hispanic black men (71.8). 3 The estimated life expectancy at birth for a given year represents the average number of years that a group of infants would be expected to live if, throughout their lifetime, they were to experience the age-specific death rates that prevailed during the year of their birth.
Deaths Among Children
A total of 18 888 children and adolescents aged 1 to 19 years died in the United States in 2013 (Table 8). The death rate for children aged 1 to 19 years was 24.0 per 100 000 population in 2013, and was significantly different from the rate of 24.8 in 2012.
TABLE 8.
Deaths and Death Rates for the 5 Leading Causes of Childhood Death in Specified Age Groups, United States, 2013 and 2012
| Age, Causes of Death, and ICD-10 Codes 12 | Rank a | 2013 | 2012 | ||||
|---|---|---|---|---|---|---|---|
| n | % | Rate b | n | % | Rate b | ||
| Total: 1–19 y | |||||||
| All causes | — | 18 888 | 100.0 | 24.0 | 19 492 | 100.0 | 24.8 |
| Accidents (unintentional injuries) (V01–X59,Y85–Y86) | 1 | 6489 | 34.4 | 8.3 | 6898 | 35.4 | 8.8 |
| Intentional self–harm (suicide) (*U03,X60–X84,Y87.0) | 2 | 2143 | 11.3 | 2.7 | 2093 | 10.7 | 2.7 |
| Assault (homicide) (*U01–*U02,X85–Y09,Y87.1) | 3 | 2021 | 10.7 | 2.6 | 2264 | 11.6 | 2.9 |
| Malignant neoplasms (C00–C97) | 4 | 1850 | 9.8 | 2.4 | 1932 | 9.9 | 2.5 |
| Congenital malformations, deformations and chromosomal abnormalities (Q00–Q99) | 5 | 982 | 5.2 | 1.2 | 1029 | 5.3 | 1.3 |
| Diseases of heart (I00–I09,I11,I13,I20–I51) | 6 | 639 | 3.4 | 0.8 | 631 | 3.2 | 0.8 |
| Influenza and pneumonia (J09–J18) | 7 | 303 | 1.6 | 0.4 | 225 | 1.2 | 0.3 |
| Chronic lower respiratory diseases (J40–J47) | 8 | 279 | 1.5 | 0.4 | 224 | 1.1 | 0.3 |
| Cerebrovascular diseases (I60–I69) | 9 | 183 | 1.0 | 0.2 | 204 | 1.0 | 0.3 |
| Septicemia (A40–A41) | 10 | 150 | 0.8 | 0.2 | 154 | 0.8 | 0.2 |
| 1–4 y | — | ||||||
| All causes | 4068 | 100.0 | 25.5 | 4218 | 100.0 | 26.3 | |
| Accidents (unintentional injuries) (V01–X59,Y85–Y86) | 1 | 1316 | 32.4 | 8.3 | 1353 | 32.1 | 8.4 |
| Congenital malformations, deformations and chromosomal abnormalities (Q00–Q99) | 2 | 476 | 11.7 | 3.0 | 501 | 11.9 | 3.1 |
| Assault (homicide) (*U01–*U02,X85–Y09,Y87.1) | 3 | 337 | 8.3 | 2.1 | 339 | 8.0 | 2.1 |
| Malignant neoplasms (C00–C97) | 4 | 328 | 8.1 | 2.1 | 392 | 9.3 | 2.4 |
| Diseases of heart (I00–I09,I11,I13,I20–I51) | 5 | 169 | 4.2 | 1.1 | 154 | 3.7 | 1.0 |
| 5–9 y | — | ||||||
| All causes | 2427 | 100.0 | 11.8 | 2334 | 100.0 | 11.4 | |
| Accidents (unintentional injuries) (V01–X59,Y85–Y86) | 1 | 746 | 30.7 | 3.6 | 743 | 31.8 | 3.6 |
| Malignant neoplasms (C00–C97) | 2 | 447 | 18.4 | 2.2 | 440 | 18.9 | 2.1 |
| Congenital malformations, deformations and chromosomal abnormalities (Q00–Q99) | 3 | 179 | 7.4 | 0.9 | 167 | 7.2 | 0.8 |
| Assault (homicide) (*U01–*U02,X85–Y09,Y87.1) | 4 | 125 | 5.2 | 0.6 | 138 | 5.9 | 0.7 |
| Chronic lower respiratory diseases (J40–J47) | 5 | 75 | 3.1 | 0.4 | 63 | 2.7 | 0.3 |
| 10–14 y | — | ||||||
| All causes | 2913 | 100.0 | 14.1 | 2866 | 100.0 | 13.9 | |
| Accidents (unintentional injuries) (V01–X59,Y85–Y86) | 1 | 775 | 26.6 | 3.8 | 807 | 28.2 | 3.9 |
| Malignant neoplasms (C00–C97) | 2 | 448 | 15.4 | 2.2 | 472 | 16.5 | 2.3 |
| Intentional self–harm (suicide) (*U03,X60–X84,Y87.0) | 3 | 386 | 13.3 | 1.9 | 306 | 10.7 | 1.5 |
| Congenital malformations, deformations and chromosomal abnormalities (Q00–Q99) | 4 | 161 | 5.5 | 0.8 | 160 | 5.6 | 0.8 |
| Assault (homicide) (*U01–*U02,X85–Y09,Y87.1) | 5 | 152 | 5.2 | 0.7 | 173 | 6.0 | 0.8 |
| 15–19 y | — | ||||||
| All causes | 9480 | 100.0 | 44.8 | 10 074 | 100.0 | 47.2 | |
| Accidents (unintentional injuries) (V01–X59,Y85–Y86) | 1 | 3652 | 38.5 | 17.3 | 3995 | 39.7 | 18.7 |
| Intentional self–harm (suicide) (*U03,X60–X84,Y87.0) | 2 | 1748 | 18.4 | 8.3 | 1782 | 17.7 | 8.3 |
| Assault (homicide) (*U01–*U02,X85–Y09,Y87.1) | 3 | 1407 | 14.8 | 6.6 | 1614 | 16.0 | 7.6 |
| Malignant neoplasms (C00–C97) | 4 | 627 | 6.6 | 3.0 | 628 | 6.2 | 2.9 |
| Diseases of heart (I00–I09,I11,I13,I20–I51) | 5 | 297 | 3.1 | 1.4 | 302 | 3.0 | 1.4 |
Data source: Centers for Disease Control and Prevention /NCHS, National Vital Statistics System: mortality, 2013 and 2012 (www.cdc.gov/nchs/deaths.htm) and unpublished tabulations. —, data are not available.
Rank is based on 2013 data.
Rate per 100 000 population in specified group.
For all children aged 1 to 19 years, the leading cause of death was accidents (unintentional injuries), which accounted for 34.4% of all deaths in 2013 and 35.4% in 2012. The second leading cause of death was suicide, accounting for 11.3% of all deaths in 2013 and 10.7% in 2012. Between 2012 and 2013, the death rate decreased significantly for unintentional injuries and homicide. Suicide, the third leading cause in 2012, became the second leading cause in 2013, whereas homicide, the second leading cause in 2012, became the third leading cause in 2013. Rates did not change significantly for the other leading causes of death among children.
Feature: Trends in Racial and Ethnic Disparities in US IMRs
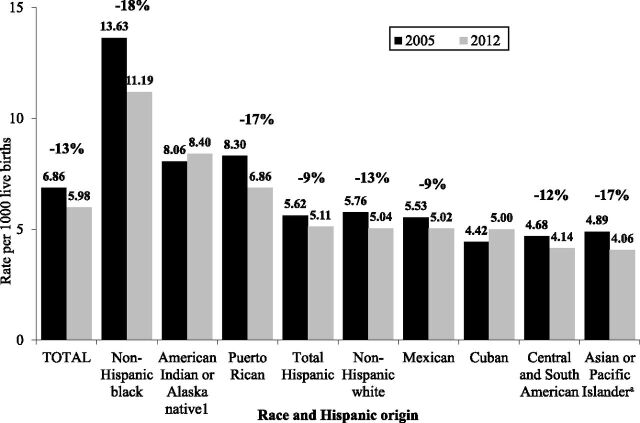
Although there have been recent declines in US infant mortality, large disparities in infant mortality by race and ethnicity persist. In particular, infant mortality for black women has been much higher than for white women ever since statistics on these measures began to be collected a century ago. 29 This difference is often measured via the “IMR ratio”: the ratio of non-Hispanic black to non-Hispanic white IMRs. This ratio is an important measure of health inequality, and has remained between 2.3 and 2.5 since at least 1995 (data available on request). 30 However, there are recent indications that this may be changing. From 2005 to 2012, declines in US infant mortality were larger for infants of non-Hispanic black (18%) than for non-Hispanic white (13%) mothers (Fig 4). This led to the first decrease in a generation in the IMR ratio (the ratio of non-Hispanic black/non-Hispanic white IMRs). This ratio fell from 2.4 in 2005 to 2.2 in 2012. 17 , 30
FIGURE 4.
IMRs by race and Hispanic origin of mother: United States, 2005 and 2012. aIncludes persons of Hispanic and non-Hispanic origin. Note: Percent change indicates statistically significant change between 2005 and 2012. Source: Linked birth/infant death data set, NCHS, Centers for Disease Control and Prevention.
In addition to the declines for non-Hispanic white and non-Hispanic black women, the IMR for Asian or Pacific Islander women also declined by 17% during this period; however, infant mortality for American Indian or Alaska Native women did not improve during this time frame.
IMRs also declined for Hispanic women from 2005 to 2012. The rate declined by 9% for the overall Hispanic category and for Mexican women. For Puerto Rican women, who have traditionally had the highest IMRs among the Hispanic origin subgroups, the decline was larger (17%). IMRs also declined by 12% for Central and South American women; there was no significant change for Cuban women (Fig 4).
Infant mortality declines were greatest among geographic and race/ethnic groups that have traditionally had higher-than-average IMRs. For example, a recent report found that infant mortality declines from 2005 to 2010 were most rapid (20% or more) among selected southeastern states (Louisiana, Georgia, North Carolina, and South Carolina) and the District of Columbia with historically high IMRs, when compared with the US average. 30 Although these states still had higher-than-average infant mortality, disparities in IMRs between states have been reduced. 31
Conclusions
Vital statistics are a valuable tool for monitoring the health of the US population. There are efforts under way to assess and improve the quality of vital statistics data, particularly the birth medical and health information. 32 As these efforts take effect, the quality of the data are expected to improve.
Acknowledgments
We thank Joyce A. Martin, Brady E. Hamilton, Sally C. Curtin, Elizabeth C.W. Gregory, Jiaquan Xu, and Sherry L. Murphy for contributions to the manuscript and Sharon Kirmeyer for content review.
Footnotes
Ms Osterman contributed to the concept and design of the manuscript, analyzed and/or assembled data and drafted numerous segments of the manuscript and compiled segments from other authors, and reviewed and approved the final manuscript as submitted; Mr Kochanek, and Dr Strobino contributed to the concept and design of the manuscript, analyzed and/or assembled data and drafted various segments of the manuscript and approved the final manuscript as submitted; Dr MacDorman analyzed data and drafted a segment of the manuscript and reviewed content written by other authors; and Dr Guyer contributed to the concept and design of the manuscript and approved the final manuscript as submitted.
FUNDING: No external funding.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1. Martin JA , Hamilton BE , Osterman MJK , Curtin SC , Matthews TJ . Births: final data for 2013. Natl Vital Stat Rep. 2015;64(1):1–65. Available at: www.cdc.gov/nchs/data/nvsr/nvsr64/nvsr64_01.pdf. Accessed November 10, 2014 [PubMed] [Google Scholar]
- 2.Gregory ECW, MacDorman MF, Martin JA. Trends in fetal and perinatal mortality in the United States, 2006-2012. NCHS data brief. 2014;169. Available at: www.cdc.gov/nchs/data/databriefs/db169.pdf. Accessed November 24, 2014 [PubMed]
- 3. Murphy SL , Xu JQ , Kochanek KD , et al. Deaths: final data for 2012. Natl Vital Stat Rep. 2015;63(9) [PubMed] [Google Scholar]
- 4. Xu JQ , Murphy SL , Kochanek KD , et al. Deaths: final data for 2013. Natl Vital Stat Rep. 2015;64(2) [PubMed] [Google Scholar]
- 5.National Center for Health Statistics. Natality public use file and CD-ROM. Hyattsville, MD: National Center for Health Statistics. Published annually. Available at: www.cdc.gov/nchs/data_access/VitalStatsOnline.htm. Accessed November 10, 2014
- 6.National Center for Health Statistics. Mortality public use file and CD-ROM. Hyattsville, MD: National Center for Health Statistics. Published annually. Available at: www.cdc.gov/nchs/data_access/VitalStatsOnline.htm. Accessed November 14, 2014
- 7.National Center for Health Statistics. NCHS data release and access policy for micro-data and compressed vital statistics files. Hyattsville, MD. 2000. Available at: www.cdc.gov/nchs/nvss/dvs_data_release.htm. Accessed November 10, 2014
- 8.National Center for Health Statistics. US standard certificate of live birth, 2003 revision. Available at: www.cdc.gov/nchs/data/dvs/birth11-03final-ACC.pdf. Accessed November 10, 2014
- 9.National Center for Health Statistics. Report of the panel to evaluate the US standard certificates and reports. Available at: www.cdc.gov/nchs/data/dvs/panelreport_acc.pdf. Accessed November 10, 2014
- 10.National Center for Health Statistics. User guide to the 2012 fetal death public use file. Hyattsville, MD. Available at: www.cdc.gov/nchs/data_access/Vitalstatsonline.htm#Fetal_Death. Accessed November 24, 2014
- 11.Office of Management and Budget. Revisions to the standards for the classification of federal data on race and ethnicity. Federal Register 62FR58781-58790, October 30, 1997. Available at: www.whitehouse.gov/omb/fedreg_1997standards. Accessed November 10, 2012
- 12. Ingram DD , Parker JD , Schenker N , et al. United States Census 2000 population with bridged race categories. Vital Health Stat 2. 2003;(135):1–55 [PubMed] [Google Scholar]
- 13. Schenker N , Parker JD . From single-race reporting to multiple-race reporting: using imputation methods to bridge the transition. Stat Med. 2003;22(9):1571–1587 [DOI] [PubMed] [Google Scholar]
- 14.National Center for Health Statistics. User guide to the 2013 natality public use file. Hyattsville, MD. Available at: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/DVS/natality/UserGuide2013.pdf. Accessed November 24, 2014
- 15.World Health Organization. International Statistical Classification of Diseases and Related Health Problems, Tenth Revision. 2008 ed. Geneva, Switzerland: World Health Organization; 2009. [Google Scholar]
- 16. Heron M . Deaths: leading causes for 2010. Natl Vital Stat Rep. 2013;62(6):1–96 [PubMed] [Google Scholar]
- 17.National Center for Health Statistics. User Guide for the 2012 period linked birth/infant death data set. Hyattsville, MD: National Center for Health Statistics. 2014. Available at: www.cdc.gov/nchs/data_access/VitalStatsOnline.htm. Accessed November 24, 2014
- 18.Office of Management and Budget. Race and ethnic standards for federal statistics and administrative reporting. 1977. Statistical Policy Directive 15. Available at: http://wonder.cdc.gov/wonder/help/populations/bridged-race/directive15.html. Accessed November 10, 2014 [PubMed]
- 19. United Nations . Tables 9 and 15. In: United Nations Demographic Yearbook, 2012. New York, NY: United Nations; 2013: 311–24, 389–401 [Google Scholar]
- 20.OECD. iLibrary. Health: Key Tables from OECD. ISSN 2075-8480. OECD 2011. Available at: www.oecd-ilibrary.org/social-issues-migration-health/health-key-tables-from-oecd_20758480;jsessionid=3rlpr57wud5fl.x-oecd-live-02. Accessed December 2, 2014
- 21.Mathews JK, MacDorman MF. Infant mortality statistics from the 2010 period linked birth/infant death data set. National vital statistics reports; vol 62 no 8. Hyattsville, MD: National Center for Health Statistics. 2013. [PubMed] [Google Scholar]
- 22.Oficina Nacional de Estadistica e Informacion. Anuario Estadistico de Cuba 2013: Table 19.21. 2014. Available at: www.one.cu/aec2013/esp/19_tabla_cuadro.htm. Accessed December 2, 2014
- 23.Statistics New Zealand. Births and deaths: year ended December 2012. 2013. Available at: www.stats.govt.nz/browse_for_stats/population/births/BirthsAndDeaths_HOTPYeDec12.aspx. Accessed December 2, 2014
- 24. MacDorman MF , Matthews TJ , Mohangoo AD , Zeitlin J . International comparisons of infant mortality and related factors: United States and Europe, 2010. Natl Vital Stat Rep. 2014;63(5):1–6. Available at: www.cdc.gov/nchs/data/nvsr/nvsr63/nvsr63_05.pdf. Accessed December 1, 2014 [PubMed] [Google Scholar]
- 25. Kramer MS , Platt RW , Yang H , Haglund B , Cnattingius S , Bergsjo P . Registration artifacts in international comparisons of infant mortality. Paediatr Perinat Epidemiol. 2002;16(1):16–22 [DOI] [PubMed] [Google Scholar]
- 26. MacDorman MF , Mathews TJ . Behind international rankings of infant mortality: how the United States compares with Europe. Int J Health Serv. 2010;40(4):577–588 [DOI] [PubMed] [Google Scholar]
- 27.Mohangoo AD, Buitendijk SE, Szamotulska K, et al. Gestation age patterns of fetal and neonatal mortality in Europe: Results from the Euro-Peristat project. PLoS One. 2011;6(11):e24727 [DOI] [PMC free article] [PubMed]
- 28. Graafmans WC , Richardus JH , Macfarlane A , et al. EuroNatal Working Group . Comparability of published perinatal mortality rates in Western Europe: the quantitative impact of differences in gestational age and birthweight criteria. BJOG. 2001;108(12):1237–1245 [DOI] [PubMed] [Google Scholar]
- 29.National Center for Health Statistics. Vital statistics of the United States, 1993, vol II, mortality, part A. Hyattsville, MD: National Center for Health Statistics; 2002 [Google Scholar]
- 30.National Center for Health Statistics. User Guide for the period linked birth/infant death data set. Selected years. Hyattsville, MD: National Center for Health Statistics. Available at: www.cdc.gov/nchs/data_access/VitalStatsOnline.htm. Accessed November 24, 2014
- 31.MacDorman MF, Hoyert DL, Mathews TJ. Recent declines in infant mortality in the United States, 2005-2011. NCHS data brief. 2013;120:1–7. Available at: www.cdc.gov/nchs/data/databriefs/db120.pdf. Accessed December 1, 2014 [PubMed]
- 32. Martin JA , Wilson EC , Osterman MJK , Saadi EW , Sutton SR , Hamilton BE . Assessing the quality of medical and health data from the 2003 birth certificate revision: results from two states. Natl Vital Stat Rep. 2013;62(2):1–19. Available at: www.cdc.gov/nchs/data/nvsr/nvsr62/nvsr62_02.pdf. Accessed December 2, 2014 [PubMed] [Google Scholar]