Abstract
Objectives
To review the most common disorders depicted with conventional videodefecography, and to compare the defecographic abnormalities between symptomatic patients according to their gender and age.
Methods
Conventional videodefecography studies of 300 patients (24 men, 266 women; mean age – 57.7) performed in a 32-month period were reviewed for the following parameters: anorectal angle, movement of the pelvic floor, intussusceptions, incontinence and rectocele. The results were analyzed using the chi-square test.
Results
Normal findings were observed in 16.7% men and 7.5% women. In women, the most frequent pathological findings were rectocele (62%), descending perineum syndrome (42.8%), intussusceptions (33.8%), incontinence (10.5%), dyskinetic puborectalis syndrome (9.4%) and rectal prolapse (4.5%); in men the most frequent pathology was the dyskinetic puborectalis syndrome (37.5%). This syndrome is more likely in men than in women (p = 0.01; OR 5.78); descending perineum syndrome (p = 0.027; OR 2.8) is more likely to occur in women.
Women with perineal descent younger than 50 years frequently present an increased descent during evacuation (81.8%), while those older than 50 years already have a low pelvic floor during rest (60.3%) (p < 0.001; OR 6.8), with little change in evacuation.
Conclusion
Videodefecographic findings vary with age and gender.
Keywords: Defecography, Pelvic floor disorders, Pelvic floor, Rectocele, Constipation
1. Introduction
Conventional videodefecography enables the evaluation of the anatomy of pelvic floor but also the dynamics of rectal emptying, providing important information about anorectal and pelvic floor functions [1], [2], [3], [4], [5]. This technique was first described by Wallden in 1953 [6] but it was not until the 1980s that Mahieu et al. developed a technique that despite modified by opacification of other pelvic anatomic landmarks has now become standard [7], [8].
Since then it has remained a widely available and cost effective procedure of choice for the assessment of anorectal dysfunction [9], despite the increasing role of magnetic resonance imaging (MRI) in the study of evacuation disorders [10].
Currently the major advantage of conventional defecography lies on the fact that it provides a near physiologic evaluation of evacuation, allowing the radiologist to examine the function and anatomy while the patient is in a position similar to the one in which daily maneuvers that generated symptoms are performed [11]. This fluoroscopic method evaluates in real time the morphology of the rectum and anal canal in correlation with pelvic bony components both statically and dynamically. Specifically it provides pelvic measurements at rest and during both squeeze and push, which are used to assess evacuation dynamics. As a result, disorders such as dyskinetic puborectalis syndrome, rectocele, intussusception and perineal descent can be diagnosed [2]. The major indications to perform a videodefecographic examination are constipation, incomplete evacuation or incontinence, perineal pain and as a follow-up examination of patients who have undergone surgery of the pelvic region [12].
Disorders of the posterior pelvic floor are relatively common. They are frequently found in elderly patients and are often caused by morphologic and functional abnormalities due to changes in the musculoaponeurotic support of the pelvic floor.
They are particularly common and well known in women, and some are related to obstetrical sequelae. Although many reports have discussed defecatory disorders in women, little is known about gender influence in symptomatic patients investigated by defecography [13], [14], [15], [16].
The purpose of our study was to review the most common disorders depicted with conventional videodefecography and to compare the defecographic abnormalities between symptomatic patients according gender and age.
2. Materials and methods
2.1. Patients
Over a 32-month period (January 2009 to August 2011), 300 symptomatic patients aged 15–87 years (mean: 57.7 years; 266 females, 24 males) were addressed for conventional defecography and evaluated consecutively in our institution. Patients were referred on the basis of clinical evidence of evacuation disorders.
Ten patients were excluded of our retrospective image analysis because of lack of evacuation.
2.2. Defecography
We applied a standardized protocol to perform and evaluate all defecography examinations.
Two to three-hundred milliliters of barium paste were injected in the rectum by means of a plastic syringe connected to a catheter with the patient lying in the left lateral position. The barium paste was obtained by mixing equal proportions of potato starch and barium solution with water and should had the consistency of normal stool. We did not use suppositories and the rectum was not emptied beforehand. The patient sat on a commode (a special commode with three water-filled annular pillows), which rested on the footrest of a standard digital fluoroscopic table, in the upright position. We did not usually opacified the bladder or routinely used radio-opaque vaginal tampons. Contrast opacification of bladder, vagina, or peritoneum could be useful but are increasingly invasive.
Static images using a fluoroscopic image capture were obtained during the following maneuvers: at rest, at voluntary and maximal contraction of the sphincter and pelvic floor (“squeeze”) and at straining without defecation (“strain”).
Finally a cine-loop of the evacuation was obtained until the rectum was emptied or at least three 30 s attempts had been made to empty the rectum.
All patients were instructed to empty the rectum completely and without interruption.
All images were analyzed in consensus by two radiologists enrolled in the study.
2.3. Image interpretation
The defecographic measurements were taken at rest and during both squeeze and pushing. There is a wide range of normal values for each parameter [2], [8]. The exact value of any of these isolated parameters is of little consequence if used to compare patients but is of great value if used to provide a basis for relative comparison among rest, squeeze and push values in a single patient.
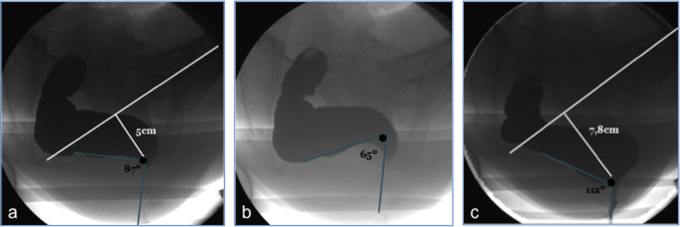
The anorectal angle (ARA) was measured between the longitudinal axis of the anal canal and the posterior rectal line, parallel to the longitudinal axis of the rectum [7], [17], [18]. In resting conditions, its average value is 92°–114° (physiological range, 70°–140°); during muscle contraction, the angle becomes more acute, while during relaxing phase it becomes obtuse [2]. ARA is an indirect indicator of the puborectal muscle activity. Dyskinetic puborectalis syndrome was diagnosed when clear impressions in the puborectalis muscle were shown during defecation, the ARA was not changed in comparison with the angle at rest or rather became smaller, and when defecation was attempted, perineal descent hardly occurred, and the opening of the anal canal and the excretion of more than 80% feces were delayed for more than 30 s.
Perineal descent was quantitatively defined by measuring the vertical distance between the pubococcygeal line (PCL) and the anorectal junction (ARJ).
The PCL was drawn from inferior pubis to the tip of the coccyx and is considered to represent the approximate line of attachment of the pelvic floor muscles. The distance from the PCL to the ARJ was measured on images obtained when the patient was at rest and at maximal pelvic strain, to assess the position of the pelvic floor. The craniocaudal migration of ARJ indirectly represents the elevation and descent of pelvic floor. For the diagnosis of perineal descent at rest (fixed descent), the distance in centimeters between the ARJ and the PCL was measured, and perineal descent at rest was considered when the ARJ and PCL distance was superior to 6 cm. For perineal descent at straining (dynamic descent), the difference in centimeters between the ARJ position at straining and at rest was noted. Perineal descent at straining was defined as a difference of ≥3.5 cm between the two positions (Fig. 1).
Fig. 1.
Normal defecography phases: at rest (a), during forced contraction (b) and during defecation (c). Measurement of the ARA with the patient at rest (a), during maximal contraction (b), and during evacuation (c) (blue lines). The ARA decreases during maximal contraction of the anal sphincter and increases during evacuation, followed by descent of the ARJ (black point at the intersection of the two lines defining the ARA). The descent of the ARJ between resting position and evacuation is less than 3.5 cm in normal conditions.
Anterior rectocele was defined as an outpouching of the anterior rectal wall that persisted on incomplete evacuation. Outpouchings inferior to 2 cm are frequently found in asymptomatic patients and are clinically insignificant. We considered three grades of rectocele: grade I are outpouchings <2 cm in anteroposterior diameter (not clinically significant); grade II are outpouchings between 2 and 4 cm; and grade III are outpouchings with an anteroposterior diameter ≥4 cm.
Intussusception was defined as an invagination of the rectal wall, either intrarectal or intra-anal. More precisely rectal intussusceptions were defined as the rectum showing a funnel-shaped depression within the anal canal during push, while an invagination of the whole circumference of the rectal wall was defined as external rectal prolapse.
2.4. Statistical analysis
Data were analyzed using SPSS version 21.0 software (SPSS Inc., Chicago, IL) and χ2 (chi-square) tests were performed for the comparison of rectocele, dyskinetic puborectalis muscle syndrome, perineal descent and intussusceptions; a p-value <0.05 was regarded as clinically significant.
3. Results
Of the 290 patients included, 8.3% (24) were male and 91.7% (266) female; the mean age was 57.7 years (range 15–87 years).
All patients enrolled were symptomatic, being the most frequent referral diagnosis pelvic outlet obstruction and major symptoms of the patients constipation and sensation of incomplete evacuation.
In 8.3% (24) symptomatic patients, no abnormalities were found. In men, 16.7% (4) of the defecography procedures were normal versus 7.5% (20) in women.
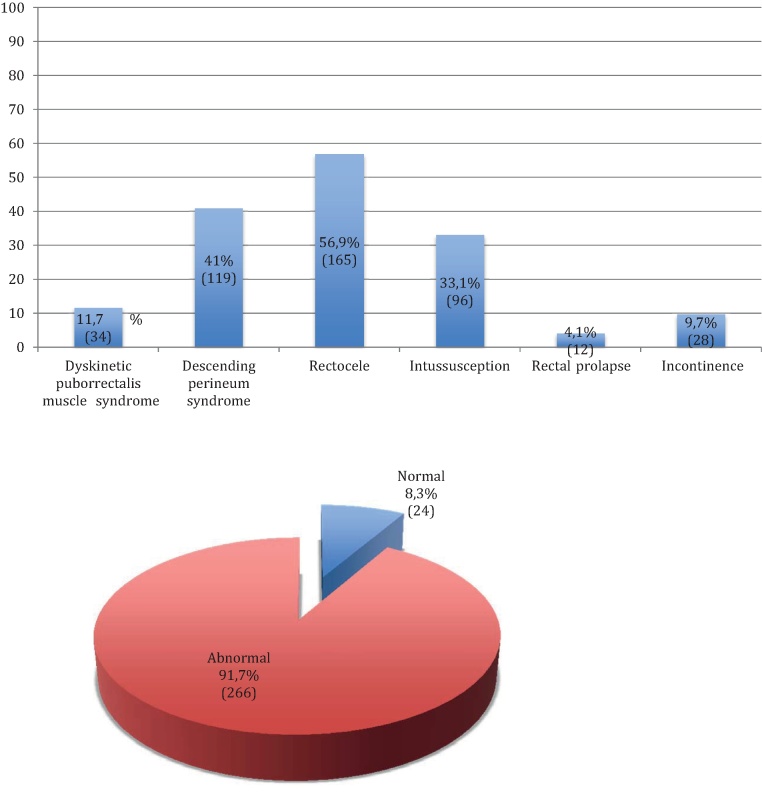
Conventional videodefecography detected abnormalities of normal rectal voiding in 91.7% (266) patients: clinically significant anterior rectocele 56.9% (165 cases), intussusception 33.1% (96 cases), external rectal prolapse 4.1% (12 cases), dyskinetic puborectalis muscle syndrome 11.7% (34 cases), descending perineum syndrome 41.0% (119 cases) and incontinence 9.7% (28 cases) (Fig. 2).
Fig. 2.
Distribution of defecographic findings.
The distribution of defecographic findings regarding gender is summarized in Table 1.
Table 1.
Distribution of defecographic findings according to gender.
| Female (n = 266) | Male (n = 24) | Total (n = 290) | |
|---|---|---|---|
| Normal defecographic findings | 20 (7.5%) | 4 (16.7%) | 24 (8.3%) |
| Rectocele | |||
| 1st degree (<2 cm) | 101 (38%) | 24 (100%) | 125 (43.1%) |
| 2nd degree (2–4 cm) | 125 (47%) | 0 | 125 (43.1%) |
| 3rd degree (≥4 cm) | 40 (15%) | 0 | 40 (13.8%) |
| Intussusception | 90 (33.8%) | 6 (25%) | 96 (33.1%) |
| Rectal prolapse | 12 (4.5%) | 0 | 12 (4.1%) |
| Dyskinetic puborectalis syndrome | 25 (9.4%) | 9 (37.5%) | 34 (11.7%) |
| Descending perineum syndrome | |||
| At rest | 53 (19.9%) | 1 (4.2%) | 54 (18.6%) |
| With strain/during evacuation | 58 (21.8%) | 4 (16.7%) | 62 (21.4%) |
| Both | 3 (1.1%) | 0 | 3 (1%) |
| Incontinence | 28 (10.5%) | 0 | 28 (9.7%) |
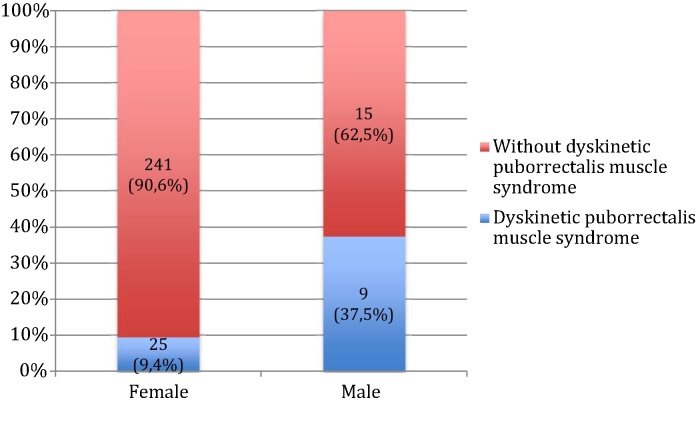
In women the most frequent pathological findings were rectocele (62%), descending perineum syndrome (42.8%), intussusceptions (33.8%), incontinence (10.5%), dyskinetic puborectalis syndrome (9.4%) and rectal prolapse (4.5%); in men was the dyskinetic puborectalis syndrome (37.5%). In our study there was a greater incidence of this syndrome in men than in women (p = 0.01; OR 5.78) (Fig. 3).
Fig. 3.
Dyskinetic puborectalis muscle syndrome according to gender.
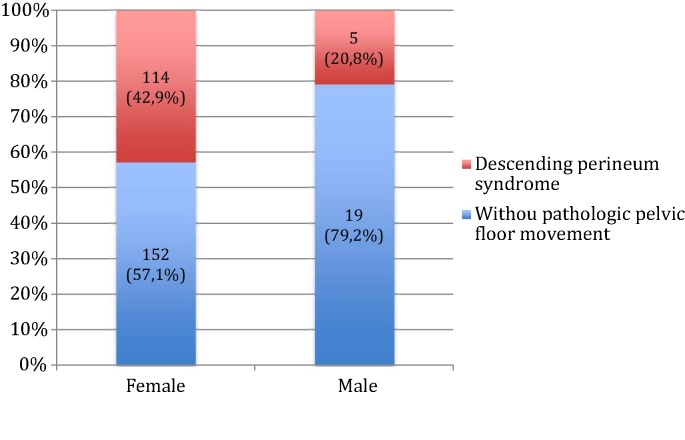
Distance between the pubococcygeal line and the anorectal junction at rest and strain were significantly different between men and women. So, descending perineum syndrome is more likely to occur in women (p = 0.027; OR 2.8) (Fig. 4).
Fig. 4.
Descending perineum syndrome according to gender.
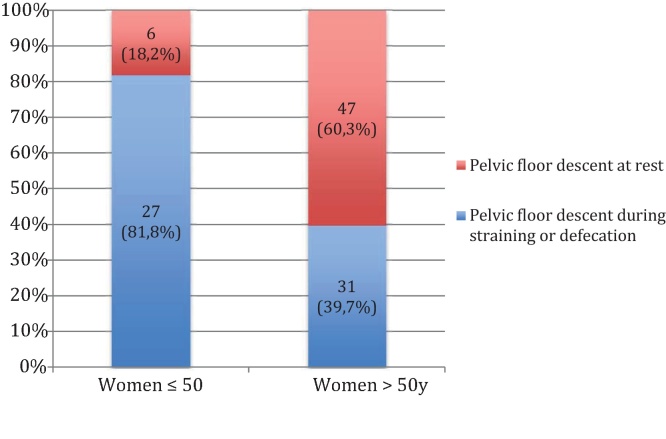
In women with perineal descent, those younger than 50 years frequently present increased descent during evacuation (81.8%), while those older than 50 years already have a pelvic floor in low position during rest (60.3%) (p < 0.001; OR 6.8), with little change in evacuation (Fig. 5).
Fig. 5.
Women pelvic floor descent according to age.
4. Discussion
Conventional videodefecographic studies are mainly performed in women. This is perhaps the major limitation to explore the gender differences in the diagnosis of defecographic abnormalities.
We found that clinically significant rectocele is most commonly found in females, as all patients with this pathology were women. This could be explained because of laxity of the rectovaginal septum, usually caused by obstetrical trauma or surgical procedures. In fact, studies report that it is present in 78–99% of women who have given birth [19].
Nonrelaxing puborectalis syndrome here designated as dyskinetic puborectalis syndrome is a poorly understood entity characterized by contraction rather than relaxation of the puborectalis in a paradoxical way during attempted evacuation. The etiology of this dysfunction remains unknown. Nevertheless an association with sexual abuse is suggestive of a psychologic basis [20], [21]. To our knowledge there were not studies comparing the frequency of this syndrome regarding gender. Although further studies with larger numbers of men enrolled are required, in our analysis dyskinetic puborectalis syndrome has a greater incidence in men than in women. Despite we do not have a definitive explanatory answer to this occurrence, we believe that psychological dyskinesia factors could affect more men than women and explain this difference between genders. Also, voluntary contraction of the pelvic floor due to embarrassment or reluctance to evacuate in front of others, may simulate a functional disorder on videodefecography and cause false positive findings of dyskinetic puborectalis syndrome [22].
Descending perineum syndrome represents a condition of pelvic floor muscle hypotonia and is usually found in elderly women because the main risk factors are perineal trauma, multiparity, and surgical procedures [23].
Our results suggest that fixed perineal descent in women shows significant correlation to age. This can be explained by the fact that in younger women the position of the pelvic floor is higher at rest with greater descent on evacuation, whereas the opposite applies in the elderly with more descent at rest and less change on evacuation [24].
Despite newer techniques, such as magnetic resonance videodefecograhphy, conventional videodefecography remains a valuable exam in the identification of morphological and functional changes related to evacuation.
References
- 1.Maglinte D.D., Bartram C.I., Hale D.A., Park J., Kohli M.D., Robb B.W. Functional imaging of the pelvic floor. Radiology. 2011;258(January (1)):23–39. doi: 10.1148/radiol.10092367. [DOI] [PubMed] [Google Scholar]
- 2.Jorge J.M., Habr-Gama A., Wexner S.D. Clinical applications and techniques of cinedefecography. Am J Surg. 2001;182(1):93–101. doi: 10.1016/s0002-9610(01)00660-2. [DOI] [PubMed] [Google Scholar]
- 3.Kelvin F.M., Maglinte D.D., Hornback J.A., Benson J.T. Pelvic prolapse: assessment with evacuation proctography (defecography) Radiology. 1992;184:547–551. doi: 10.1148/radiology.184.2.1620863. [DOI] [PubMed] [Google Scholar]
- 4.Agachan F., Pfeifer J., Wexner S.D. Defecography and proctography. Results of 744 patients. Dis Colon Rectum. 1996;39:899–905. doi: 10.1007/BF02053989. [DOI] [PubMed] [Google Scholar]
- 5.Mellgren A., Bremmer S., Johansson C., Dolk A., Udén R., Ahlbäck S.O. Defecography. Results of investigations in 2,816 patients. Dis Colon Rectum. 1994;37:1133–1141. doi: 10.1007/BF02049817. [DOI] [PubMed] [Google Scholar]
- 6.Wallden L. Roentgen examination of the deep rectogenital pouch. Acta Radiol. 1953;39:105–116. doi: 10.3109/00016925309136693. [DOI] [PubMed] [Google Scholar]
- 7.Mahieu P.H., Pringot J., Bodart P. Defecography 1. Description of a new procedure and results in normal patients. Gastrointest Radiol. 1984;9:247–251. doi: 10.1007/BF01887845. [DOI] [PubMed] [Google Scholar]
- 8.Mahieu P.H., Pringot J., Bodart P. Defecography 2. Contribution to the diagnosis of defecation disorders. Gastrointest Radiol. 1984;9:253–261. doi: 10.1007/BF01887846. [DOI] [PubMed] [Google Scholar]
- 9.Karulf R.E., Coller J.A., Bartolo D.C.C., Bowden D.O., RobertsPL, Murray J.J. Anorectal physiology testing: a survey of availability and use. Dis Colon Rectum. 1991;34:464–468. doi: 10.1007/BF02049930. [DOI] [PubMed] [Google Scholar]
- 10.Roos J.E., Weishaupt D., Wildermuth S., Willmann J.K., Marincek B., Hilfiker P.R. Experience of 4 years with open MR defecography: pictorial review of anorectal anatomy and diseases. Radiographics. 2002;22:817–832. doi: 10.1148/radiographics.22.4.g02jl02817. [DOI] [PubMed] [Google Scholar]
- 11.Maglinte D.D., Bartram C. Dynamic imaging of posterior compartment pelvic floor dysfunction by evacuation proctography: techniques, indications, results and limitations. Eur J Radiol. 2007;61(March (3)):454–461. doi: 10.1016/j.ejrad.2006.07.031. [DOI] [PubMed] [Google Scholar]
- 12.Faccioli N., Comai A., Mainardi P., Perandini S., Moore F., Pozzi-Mucelli R. Defecography: a practical approach. Diagn Interv Radiol. 2010;16(September (3)):209–216. doi: 10.4261/1305-3825.DIR.2584-09.1. [DOI] [PubMed] [Google Scholar]
- 13.Cavallo G., Salzano A., Grassi R., Zanatta P., Tuccillo M. Rectocele in males: clinical, defecographic, and CT study of singular cases. Dis Colon Rectum. 1991;34:964–966. doi: 10.1007/BF02049958. [DOI] [PubMed] [Google Scholar]
- 14.Chen H.H., Iroatulam A., Alabaz O., Weiss E.G., Nogueras J.J., Wexner S.D. Associations of defecography and physiologic findings in male patients with rectocele. Tech Coloproctol. 2001;5:157–161. doi: 10.1007/s101510100018. [DOI] [PubMed] [Google Scholar]
- 15.Savoye-Collet C., Savoye G., Koning E., Leroi A.M., Dacher J.N. Gender influence on defecographic abnormalities in patients with posterior pelvic floor disorders. World J Gastroenterol. 2010;16(January (4)):462–466. doi: 10.3748/wjg.v16.i4.462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tomita R., Igarashi S., Fujisaki S., Koshinaga T. Significance of defecography in the diagnosis and evaluation of male patients with defecation disorders. Hepatogastroenterology. 2010;57(March–April (98)):220–223. [PubMed] [Google Scholar]
- 17.Bartram C.I., Mahieu P.H.G. Evacuation proctography and anal endosonography. In: Henry M.M., Swash M., editors. Coloproctology and the pelvic floor. Butterworth; London: 1991. pp. 146–172. [Google Scholar]
- 18.Jorge J.M.N., Wexner S.D., Marchetti F., Rosato G.O., Sullivan M.L., Jagelman D.G. How reliable are currently available methods of measuring the anorectal angle? Dis Colon Rectum. 1992;35:332–338. doi: 10.1007/BF02048110. [DOI] [PubMed] [Google Scholar]
- 19.Kenton K., Shott S., Brubaker L. The anatomic and functional variability of rectoceles in women. Int Urogynecol J Pelvic Floor Dysfunct. 1999;10(2):96–99. doi: 10.1007/pl00004019. [DOI] [PubMed] [Google Scholar]
- 20.Leroi A.M., Berkelmans I., Denis P., Hémond M., Devroede G. Anismus as a marker of sexual abuse. Consequences of abuse on anorectal motility. Dig Dis Sci. 1995;40(July (7)):1411–1416. doi: 10.1007/BF02285184. [DOI] [PubMed] [Google Scholar]
- 21.Leroi A.M., Bernier C., Watier A., Hémond M., Goupil G., Black R. Prevalence of sexual abuse among patients with functional disorders of the lower gastrointestinal tract. Int J Colorectal Dis. 1995;10(4):200–206. doi: 10.1007/BF00346219. [DOI] [PubMed] [Google Scholar]
- 22.Kuijpers H.C., Bleijenberg G. The spastic pelvic floor syndrome: a cause of constipation. Dis Colon Rectum. 1985;28:6669–6672. doi: 10.1007/BF02553449. [DOI] [PubMed] [Google Scholar]
- 23.Jorge J.M.N., Wexner S.D., Ehrenpreis E.D., Nogueras J.J., Jagelman D.G. Does perineal descent correlate with pudendal neuropathy? Dis Colon Rectum. 1993;36:475–483. doi: 10.1007/BF02050014. [DOI] [PubMed] [Google Scholar]
- 24.Pinho M., Yoshioka K., Ortiz J., Oya M., Keighley M.R. The effect of age on pelvic floor dynamics. Int J Colorectal Dis. 1990;5(4):207–208. doi: 10.1007/BF00303277. [DOI] [PubMed] [Google Scholar]