Abstract
Purpose
Because proposed funding cuts in the Affordable Care Act may impact care for urological patients at safety-net hospitals, we examined utilization, outcomes and costs of inpatient urological surgery at safety-net vs non-safety-net facilities prior to healthcare reform.
Materials and Methods
Using the Nationwide Inpatient Sample, we performed a retrospective cohort study of patients undergoing inpatient urological surgeries from 2007 through 2011. We defined the “safety-net burden” of each hospital based on the proportion of Medicaid and self-pay discharges. We examined the distribution of urologic procedures performed, and compared in-hospital mortality, prolonged length of stay and costs in the highest quartile of burden (safety-net) vs lowest quartile (non-safety-net).
Results
The distribution of urological procedures differs by safety-net status, with less benign prostate (9.1% safety-net vs 11.4% non-safety-net) and major cancer surgery (26.9% vs 34.3%), and more reconstructive surgery (8.1% vs 5.5%) at safety-net facilities (p-values<0.001). Higher mortality at safety-net hospitals was seen for nephrectomy (OR 1.68, 95% CI 1.15–2.45) and TURP (OR 2.17, 95% CI 1.22–3.87). Patients in safety-net hospitals demonstrated greater prolonged LOS after endoscopic stone surgery (OR 1.20, 95% CI 1.01–1.41). Costs were similar across procedures except radical prostatectomy and cystectomy, where the average admission was more expensive at non-safety-net facilities (prostatectomy $9,610 vs $11,457 and cystectomy $24,048 vs $27,875, p-values <0.02).
Conclusions
Reductions in funding to safety-net hospitals with healthcare reform could adversely impact access to care for patients with a broad range of urological conditions, potentially exacerbating existing disparities for vulnerable populations served by these facilities.
Keywords: safety net, disparities, outcomes, healthcare reform
Introduction
As safety net hospitals (SNHs) provide care for vulnerable populations regardless of their ability to pay, these hospitals represent an important source of urological care for many patients. Despite its emphasis on expanding coverage, several provisions in the Affordable Care Act (ACA)1—coupled with subsequent legislative rulings—may paradoxically threaten current levels of funding for safety net facilities. Included among the potential funding cuts are reductions in disproportionate share payments (DSH)2, and changes in reimbursement as a consequence of Medicaid expansion. The growing focus on value and quality based payment incentives will likely further threaten funding of safety net hospitals, as these facilities are more likely to receive penalties related to meaningful use requirements and to have excess readmissions3,4.
Many worry that such funding cuts will compromise care and outcomes for vulnerable patients treated in SNHs, including those with a wide range of urological conditions. However, while certain aspects of specialty care in safety net facilities have been studied, little is known about the utilization and outcomes of urologic care in SNHs and how it compares to that provided in non-safety net facilities5,6. An awareness of such differences is important to anticipating, and perhaps even mitigating, the impact of ACA-directed funding changes for these already resource-poor facilities.
In this context, we compared the utilization, outcomes, and costs of common inpatient urological procedures for patients treated at safety net versus non-safety net facilities prior to implementation of the ACA.
Materials and Methods
Data Sources
We used data from the Nationwide Inpatient Sample (NIS) for years 2007 through 2011 to perform this analysis. The NIS provides data from a 20% sample of inpatient discharges from hospitals in 46 states7. This dataset includes patient demographic information, primary payer, length of stay (LOS), admission type, hospital charges, and diagnosis and procedures codes (which also allow identification of comorbidities) defined by the International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9) and Clinical Classification Software (CCS)8. When possible, we linked the NIS data with the American Hospital Association (AHA) Survey9 from 2011 to obtain additional information on hospital characteristics. Hospital information is obtained nationally through this survey; however, privacy laws prevent linkage between the NIS and AHA in 18 states.
Identification of Safety Net Hospitals
Consistent with previously described methods10,11, we used data from the NIS to determine the “safety net burden” (i.e., the proportion of discharges with a payer status of Medicaid or self-pay) for each hospital. Self-pay claims represent approximately 5% of all discharges. Consistent with the published literature, we include these cases in the calculation of safety net burden because self-pay patients are frequently uninsured and from lower income households. Next, we divided hospitals into quartiles based on this proportion. For analytic purposes, hospitals in the highest quartiles (those with the largest proportion of Medicaid and self-pay discharges) were termed SNHs and those in the lowest quartile were termed non-SNHs.
To validate our definition of safety net hospitals, we compared our classification of hospitals into SNHs vs non-SNHs with America’s Essential Hospitals12, a group of public and non-profit hospitals that report a primary goal of serving vulnerable populations. For those hospital systems that allowed linkage to the AHA survey, 80% of facilities included in America’s Essential Hospitals were in the highest quartile of safety net burden. No hospital systems from this list were in the lowest quartile of safety net burden.
Identification of Urological Procedures
After excluding admissions for patients <18 years of age, we used CCS and ICD-9 procedure codes to identify admissions with major urological procedures performed in an operating room13. We categorized similar procedures into seven mutually exclusive, but clinically relevant groups: endoscopy, urinary incontinence, major oncologic, benign prostatectomy (including TURP and simple open prostatectomies when occurring without a prostate cancer diagnosis), reconstructive, kidney transplantation and other.
Outcome Measures
Using ICD-9 procedure codes, we then identified admissions where patients underwent one of seven specific urologic procedures including transurethral resection of prostate (TURP), urinary incontinence surgery, transurethral resection of bladder tumor (TURBT), endoscopic upper tract stone removal, nephrectomy, radical prostatectomy and cystectomy. For patients undergoing these procedures we measured 3 primary outcomes: 1) in-hospital mortality, 2) prolonged LOS and 3) hospital costs associated with the surgical admission. Length of stay was defined as prolonged if it exceeded the 90th percentile for that procedure. Hospital costs were calculated from surgical admission charges within the NIS. Consistent with established methods to obtain more accurate measures of episode cost, we adjusted charges according to hospital specific cost-to-charge ratios and the primary admitting diagnosis14,15.
Statistical Analysis
For all analyses, we compared hospitals in the highest versus lowest quartiles of safety net burden. In our first step, we used chi-squared and t-tests to compare hospital and patient characteristics for safety net and non-safety net facilities. Next, we compared the overall distribution of urologic procedures performed at SNHs versus non-SNHs. Finally, we fit multivariable regression models (applying sampling weights that account for the complex survey design of the NIS) to compare each of the outcome measures for patients undergoing the seven common urological procedures performed at SNHs versus non-SNHs. In-hospital mortality and prolonged LOS were classified as dichotomous variables and total hospital admission costs were log transformed prior to analysis. We adjusted our models for patient and hospital characteristics that could impact outcomes including age, race, number of comorbidities, median household income, primary payer and admission type (emergent/trauma, urgent, elective). Comorbidities were identified using ICD-9 diagnosis codes. As a sensitivity analysis, we compared mortality and pLOS after specifying SNHs based on deciles or quintiles (rather than quartiles) of safety net burden.
All statistical analyses were performed with SAS version 9.4 software (SAS Institute Inc., Cary, NC) using a 5% significance level. This study was deemed exempt from review by the University of Michigan institutional review board.
Results
We identified more than 260,000 inpatient urologic procedures performed at 746 SNHs and 528 non-SNHs from 2007 through 2011. Despite an equal number of hospitals in each quartile of safety net burden (n=827 per quartile), some hospitals did not provide inpatient urologic surgical care during this time frame and were therefore not included in analysis.
The mean proportion of safety net burden was 40.4% (range 28–100%) and 5.8% (range 0–11%) at SNH and non-SNHs, respectively. Table 1 presents hospital characteristics reported in the AHA survey according to safety net status for those facilities that successfully linked between the AHA and the NIS. On average, safety net facilities have a greater number of beds and higher surgical volume than non-safety net facilities; they are also more likely to be level 1 trauma centers and teaching hospitals.
Table 1.
Hospital Characteristics (NIS and AHA 2007–2011) n=1,208
| Characteristic | Non-SNH
|
SNH
|
p-value |
|---|---|---|---|
| Rural (%) | 22.1 | 34.4 | <0.001 |
| Hospital Region (%)* | <0.001 | ||
| Northeast | 26.0 | 16.0 | |
| Northwest | 30.0 | 12.0 | |
| South | 14.5 | 30.7 | |
| West | 29.5 | 41.4 | |
| Teaching Hospital (%)^ | 17.4 | 31.6 | <0.001 |
| Hospital Ownership (%)* | <0.001 | ||
| Public | 10.3 | 21.2 | |
| Non-profit | 68.5 | 61.1 | |
| For profit | 21.1 | 17.7 | |
| Critical Access Hospital (%)* | 22.9 | 10.9 | <0.001 |
| ACS approved Cancer Program (%)* | 32.0 | 32.3 | 0.93 |
| Level 1 Trauma Center (%)∘ | 14.1 | 39.8 | <0.001 |
| Mean number of beds (SD)§ | 93 (4.2) | 122 (3.5) | <0.001 |
| Mean number of Operating Rooms (SD)^ | 8.4 (0.4) | 10.9 (0.4) | <0.001 |
| Mean number of total surgical cases (SD)* | 6110 (297) | 7742 (309) | <0.001 |
n=745
n=334
n=696
n=658
Critical Access Hospital: hospital with ≤25 acute care beds and ≥35 miles (or ≥15 miles by secondary road) from nearest hospital.
Patients undergoing an inpatient urologic procedure at SNHs were younger and more frequently non-white and in the lowest income quartile. Table 2 summarizes patient demographics for those undergoing an inpatient urologic procedure at SNHs versus non-SNHs.
Table 2.
Patient Characteristics (NIS 2007–2011) n=260,391
| Characteristic | Non-SNH
|
SNH
|
p-value |
|---|---|---|---|
| Mean Age (SE) | 62.3 (0.2) | 57.7 (0.2) | <0.001 |
| Race (%)* | <0.001 | ||
| White | 79.8 | 61.4 | |
| Black | 6.7 | 15.7 | |
| Hispanic | 7.4 | 15.7 | |
| Other | 6.1 | 7.2 | |
| Male gender (%)^ | 63.7 | 57.5 | <0.001 |
| Income (quartile %)∘ | <0.001 | ||
| <$39,000 | 10.6 | 34.0 | |
| $39,000–47,999 | 17.2 | 25.0 | |
| $48,000–62,999 | 25.7 | 22.5 | |
| ≥$63,000 | 46.5 | 18.5 | |
| Admission Type (%)§ | <0.001 | ||
| Elective | 74.9 | 63.5 | |
| Trauma | 0.1 | 0.5 | |
| Emergent | 18.0 | 22.3 | |
| Urgent | 7.0 | 13.7 | |
| Comorbid conditions (%) | <0.001 | ||
| 0 | 27.6 | 28.3 | |
| 1 | 29.0 | 26.7 | |
| ≥2 | 43.4 | 45.0 |
n=226,766
n=259,431
n=253,609
n=210,708
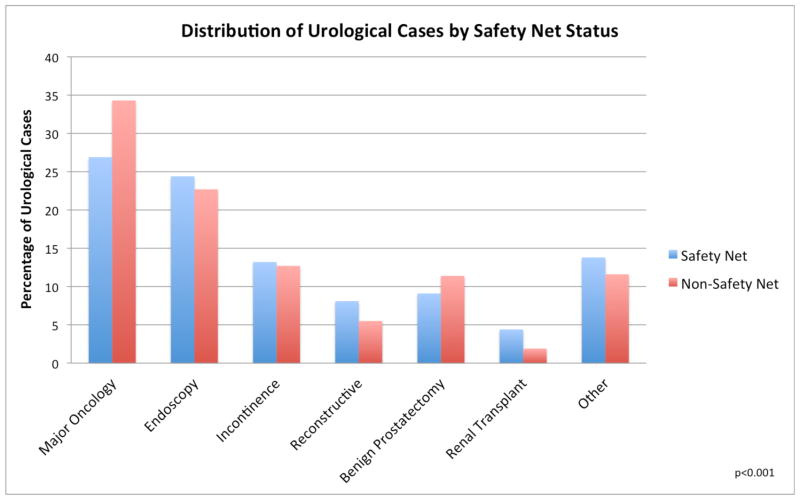
The distribution of urologic procedures differs by safety-net status (p<0.001, Figure 1). Safety net facilities perform less BPH (9.1% SNH vs 11.4% non- SNH) and major cancer surgery (26.9% vs 34.3%), and more reconstructive procedures (8.1% vs 5.5%).
Figure 1.
Distribution of inpatient urological cases according to safety net status.
Across all seven procedures evaluated, patients treated at SNHs had a higher adjusted likelihood of in-hospital mortality (OR 1.61, 95% CI 1.28–2.02) and prolonged LOS (OR 1.23, 95% CI 1.07–1.42). For the individual procedures, higher mortality at SNHs was seen for TURP (OR 2.17, 95% CI 1.22–3.87) and nephrectomy (OR 1.68, 95% CI 1.15–2.45). Patients treated in SNHs had a higher likelihood of prolonged LOS only after endoscopic stone surgery (OR 1.20, 95% CI 1.01–1.41) (Table 3). Our principal findings for in hospital mortality and pLOS for urologic procedures did not change substantively when we specified SNHs based on deciles or quintiles (rather than quartiles) of safety net burden. Specific procedure counts and number of inpatient deaths are summarized in Appendix Table 1.
Table 3.
Inpatient Procedural Mortality and Prolonged LOS (NIS 2007–2011)
| Procedure | Mortality | Prolonged LOS |
|---|---|---|
|
| ||
| Adjusted SNH OR (95% CI) | Adjusted SNH OR (95% CI) | |
| TURP | 2.17 (1.22–3.87) | 1.17 (0.85–1.62) |
| TURBT | 1.26 (0.91–1.73) | 1.13 (0.96–1.33) |
| Endoscopic Stone Removal | 1.41 (0.81–2.46) | 1.20 (1.01–1.41) |
| Radical Prostatectomy | 1.58 (0.56–4.43) | 1.11 (0.83–1.50) |
| Incontinence | § | 1.20 (0.90–1.60) |
| Nephrectomy | 1.68 (1.15–2.45) | 1.02 (0.79–1.32) |
| Cystectomy | 1.28 (0.78–2.11) | 1.00 (0.76–1.31) |
| Overall | 1.61 (1.28–2.02) | 1.23 (1.07–1.42) |
Adjusted for age, gender (where appropriate), race, admission type, payer, income, comorbidities
Due to low mortality for this procedure, a multivariable model could not be fit Referent group is non-SNH
Appendix Table 1.
Inpatient Mortality and Procedure Counts (NIS 2007–2011)
| Procedure | Total Cases | Inpatient Deaths |
|---|---|---|
| TURP | 55,505 | 154 |
| TURBT | 30,435 | 370 |
| Endoscopic Stone Removal | 51,140 | 120 |
| Radical Prostatectomy | 79,072 | 31 |
| Incontinence | 17,128 | § |
| Nephrectomy | 60,925 | 488 |
| Cystectomy | 12,404 | 239 |
| Overall | 306,609 | 1,402 |
The NIS prohibits reporting cell sizes <10 as a privacy precaution.
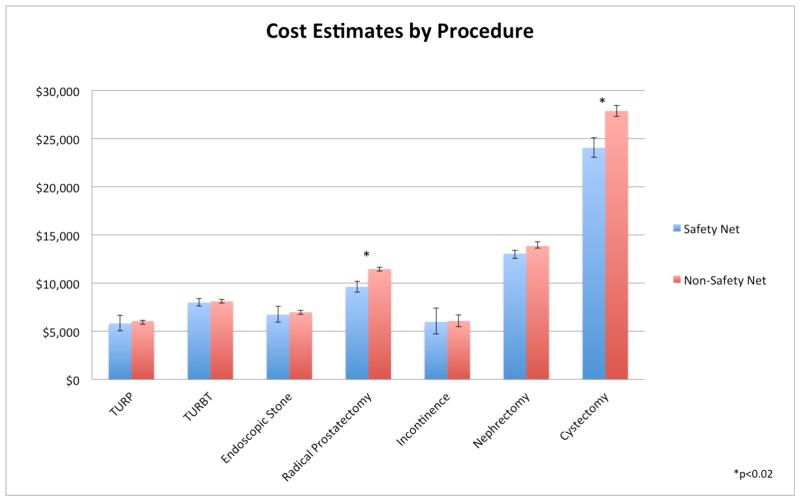
Finally, costs were similar at SNHs and non-SNHs for all procedures with the exception of radical prostatectomy and cystectomy (Figure 2). For these two procedures the average admission was significantly more expensive at non-safety-net facilities (prostatectomy $9,610 vs $11,457 and cystectomy $24,048 vs $27,875, p<0.001).
Figure 2.
Adjusted costs of common inpatient urological surgeries according to safety net status.
Discussion
The mix of inpatient urological surgeries differs for SNHs versus non-safety facilities. In particular, SNHs perform relatively more reconstructive surgery and fewer benign prostatectomies and major cancer surgeries, potentially related to caring for a younger patient population. Urological patients at SNHs are more frequently non-white, in the lower quartiles of household income and present with non-elective admissions. Perhaps driven by a more disadvantaged patient population, outcomes are less favorable for select urological procedures at SNHs with respect to both higher inpatient mortality and longer length of stay. While only statistically significant for TURP and nephrectomy, a similar trend of increased mortality at safety net facilities was noted across all procedures studied. In terms of cost comparisons, radical prostatectomy and radical cystectomy were less expensive at SNHs.
Our findings of higher in-hospital mortality, across all cases and for several procedures individually, contrasts with prior reports for patients with head and neck cancer11 and those undergoing vascular procedures5. Likewise, data on cost estimates for specialty care at safety net facilities have been mixed. Namely, while one analysis demonstrated higher costs for vascular procedures at SNHs5, others have shown—like us—that costs are lower for inpatient surgery performed at safety net facilities4. Adding to this arguably mixed picture of specialty care at safety net hospitals, our findings suggest that, for some procedures, urologic care delivered to the often-vulnerable populations served by SNHs is associated with less favorable outcomes often at a similar price.
Our study has several limitations. First, there is no uniform definition for SNH. Multiple methods for defining and identifying safety net hospitals exist, each with its own set of limitations16. Given this lack of a gold standard, there is potential for misclassification of our exposure variable. Nevertheless, the method we used is consistent with published literature in the field and has significant face validity. Second, our findings for mortality, LOS, and costs of care are susceptible to bias from residual confounding. In an effort to minimize this possibility, we accounted for several measurable patient characteristics in our multivariable models including race, comorbidities and admission type (e.g. emergent vs elective); however, the NIS does not allow measurement of other potential confounding variables including, for instance, severity of comorbidities, cancer stage, functional status and socioeconomic position. Furthermore, our analyses cannot take into account additional factors that may impact LOS at SNHs, including homelessness limited social support, and a lack of a usual source of care for other chronic conditions. It is also possible that SNHs have fewer resources devoted to detailed coding of claims and may not accurately capture disease severity. Finally, while we are able to estimate cost information from the charge data provided by the NIS, actual payment data are not available from the NIS. Future studies may utilize datasets containing more comprehensive patient and hospital characteristics or more detailed payment information to address these limitations.
Despite these limitations, our findings are relevant to several stakeholders including patients, urologists, and policymakers responsible for legislation that sets funding for safety net facilities. Given the observed differences in mortality and prolonged LOS at these SNH before implementation of the ACA, any realized reductions in funding from this legislation could exacerbate existing disparities for the vulnerable patients and populations served by these facilities. Because SNHs represent a significant source of care for urological patients, large shifts in funding that destabilize these facilities could reduce access or even eliminate an essential source of urological care. If access to urological care at SNHs is impeded, urologists at non-SNHs may see an increase in patients needing reconstructive care or patients presenting with more advanced disease due to delays in diagnosis and treatment.
At the same time, however, physicians working in SNHs will need to work with hospital leadership to improve outcomes for procedures where inpatient mortality is currently higher than for non-SNHs. Although admittedly challenging in resource-poor facilities that often treat disadvantaged patients, these efforts could involve implementation of existing programs aimed at improving the timely recognition and treatment of post-operative complications17. Furthermore, working to improve the balance in payer mix at SNHs by placing a focus on competitive provision of care (from both a quality and cost perspective) may offer an opportunity for more favorable reimbursement patterns at these facilities. For policymakers, these data underscore the need for careful monitoring of the balance between increased individual coverage with Medicaid expansion and reduced funding levels at safety net facilities. As coverage for vulnerable populations grows, as intended by the ACA, demand on the safety net system may increase beyond its capacity to care for these individuals in a timely fashion. This is particularly true if such rising demand occurs in synchronicity with other systemic funding cuts. To this point, two critical events for SNH will be the reductions in DSH payments scheduled for 2017, and the 10% decrease in federal support for Medicaid expansion scheduled for 2020.
Moving forward, studies assessing outcomes before and after implementation of the ACA will definitively inform the impact of this legislation on the access, quality and cost of urologic care at safety net facilities. Such studies will be essential for development and implementation of evidence-based policies that preserve or improve access to high quality urological care for vulnerable patients.
Conclusions
Reductions in funding to safety net hospitals as a result of healthcare reform could adversely impact access to care for patients with a broad range of urological conditions, and potentially exacerbate existing disparities for vulnerable populations served by these facilities.
Acknowledgments
All authors had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Funding:
This project was supported by funding from the National Institute of Diabetes, Digestive and Kidney Diseases (T-32-F025681 to LAH) and the National Cancer Institute (1-R01-CA-174768-01-A1 to DCM).
Footnotes
Conflicts of Interest: Dr. Herrel is a paid consultant for ArborMetrix, Inc., a company that provides software and analytics for assessing hospital quality and efficiency. Dr. Miller previously served as a consultant to ArborMetrix. The company had no role in conducting this study.
References
- 1.Patient Protection and Affordable Care Act, HR 3590, 111th Cong (2009).
- 2.Neuhausen K, Davis AC, Needleman J, et al. Disproportionate-share hospital payment reductions may threaten the financial stability of safety-net hospitals. Health Aff (Millwood) 2014;33:988–96. doi: 10.1377/hlthaff.2013.1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dupree JM, Neimeyer J, McHugh M. An advanced look at surgical performance under Medicare’s hospital-inpatient value-based purchasing program: who is winning and who is losing? J Am Coll Surg. 2014;218:1–7. doi: 10.1016/j.jamcollsurg.2013.09.017. [DOI] [PubMed] [Google Scholar]
- 4.Gilman M, Adams EK, Hockenberry JM, et al. California Safety-Net Hospitals Likely To Be Penalized By ACA Value, Readmission, And Meaningful-Use Programs. Health Aff. 2014;33:1314–1322. doi: 10.1377/hlthaff.2014.0138. [DOI] [PubMed] [Google Scholar]
- 5.Eslami MH, Rybin D, Doros G, et al. Care of patients undergoing vascular surgery at safety net public hospitals is associated with higher cost but similar mortality to nonsafety net hospitals. J Vasc Surg. 2014;60:1627–34. doi: 10.1016/j.jvs.2014.08.055. [DOI] [PubMed] [Google Scholar]
- 6.Bradley CJ, Dahman B, Shickle LM, et al. Surgery wait times and specialty services for insured and uninsured breast cancer patients: Does hospital safety net status matter? Health Serv. Res. 2012;47:677–697. doi: 10.1111/j.1475-6773.2011.01328.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Healthcare Cost and Utilization Project, Agency for Healthcare Research and Quality. Overview of the Nationwide Inpatient Sample. http://www.hcup-us.ahrq.gov/nisoverview.jsp.
- 8.Healthcare Cost and Utilization Project, Agency for Healthcare Research and Quality. Clinical Classifications Software for ICD-9-CM. http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp.
- 9.American Hospital Association Annual Survey. 2011 Available at: http://www.ahadataviewer.com/book-cd-products/AHA-Survey/
- 10.Wakeam E, Hevelone ND, Maine R, et al. Failure to rescue in safety-net hospitals: availability of hospital resources and differences in performance. JAMA Surg. 2014;149:229–35. doi: 10.1001/jamasurg.2013.3566. [DOI] [PubMed] [Google Scholar]
- 11.Genther DJ, Gourin CG. The effect of hospital safety-net burden status on short-term outcomes and cost of care after head and neck cancer surgery. Arch Otolaryngol Head Neck Surg. 2012;138:1015–22. doi: 10.1001/jamaoto.2013.611. [DOI] [PubMed] [Google Scholar]
- 12.America’s Essential Hospitals. [Accessed August 13, 2014]; http://essentialhospitals.org.
- 13.3M Health Information Systems. Centers for Medicare and Medicaid Services DRG Definitions Manual, Version 24.0. Salt Lake City, UT: 2006. Effective October 1, 2006. [Google Scholar]
- 14.Anonymous. Cost-to-charge ratio files. Healthcare Cost and Utilization Project, Agency for Healthcare Research and Quality; http://www.hcup-us.ahrq.gov/db/state/costtocharge.jsp. [PubMed] [Google Scholar]
- 15.Sun Y, Friedman B. Tools for more accurate inpatient cost estimates with HCUP databases. 2009 http://www.hcup-us.ahrq.gov/reports/methods/methods.jsp.
- 16.Werner RM, Goldman LE, Dudley RA. Comparison of Change in Quality of Care Between Safety-Net and Non–Safety-Net Hospitals. JAMA. 2008;299:2180–2187. doi: 10.1001/jama.299.18.2180. [DOI] [PubMed] [Google Scholar]
- 17.Levy MM, Dellinger RP, Townsend SR, et al. The Surviving Sepsis Campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Intensive Care Med. 2010;36:222–31. doi: 10.1007/s00134-009-1738-3. [DOI] [PMC free article] [PubMed] [Google Scholar]