Abstract
Purpose
Identification of high-risk patients with pulmonary embolism is vital. The aim of the present study was to examine clinical scores, their single items, and anamnestic features in their ability to predict 30-day mortality.
Materials and Methods
A retrospective, single-center study from 06/2005 to 01/2010 was performed. Inclusion criteria were presence of pulmonary embolism, availability of patient records and 30-day follow-up. The following clinical scores were calculated: Acute Physiology and Chronic Health Evaluation II, original and simplified pulmonary embolism severity index, Glasgow Coma Scale, and euroSCORE II.
Results
In the study group of 365 patients 39 patients (10.7%) died within 30 days due to pulmonary embolism. From all examined scores and parameters the best predictor of 30-day mortality were the Glasgow Coma scale (≤ 10) and parameters of the circulatory system including presence of mechanical ventilation, arterial pH (< 7.335), and systolic blood pressure (< 99 mm Hg).
Conclusions
Easy to ascertain circulatory parameters have the same or higher prognostic value than the clinical scores that were applied in this study. From all clinical scores studied the Glasgow Coma Scale was the most time- and cost-efficient one.
Introduction
Acute pulmonary embolism (PE) is a common disease. It has a high mortality in some patient groups, e.g. in patients with hemodynamic instability or right ventricular dysfunction [1].
It is undisputed that identification of high-risk patients is vital. However, the tools of risk stratification are under continued research and improvement. The tools include clinical scores [2] and anamnestic features [3].
Imaging techniques [4] and biomarkers [5] also play a major role in risk stratification. However, these were not considered in the present study.
Clinical scores can be time consuming to ascertain. For example, the euroSCORE is calculated from about 24 items [6]. Furthemore, it can be impossible to gather anamnestic features in patients with a deteriorated state of consciousness.
Therefore, the aim of the present study was to examine a broad array of promising scores, their single items and anamnestic features to find the most time- and cost-efficient risk stratification tools in acute pulmonary embolism.
Materials and Methods
Study design
The study was approved by the institutional ethic commitee (Martin-Luther-University). All analyzed patient records were anonymized and de-identified prior to analysis. In a single-center, retrospective study at a hospital of maximum medical care (Halle University Hospital), all patients with acute symptomatic PE were reviewed from 06/2005 to 01/2010.
Patients were identified via analysis of patient records and using the radiological information system. Inclusion criteria were: performance of computed tomography pulmonary angiography positive for pulmonary embolism, availability of patient records and 30-day follow-up. The final study group included 365 patients (age median 65 years, age range 18–91, 178 male). Treatment methodology was same during the study period following the guidelines of the diagnosis and management of acute pulmonary embolism as defined by the European Society of Cardiology [7]. High risk patients underwent thrombolysis or embolectomy.
Survival was defined as surviving the following 30 days after the PE diagnosis. Patients, who died from acute respiratory failure, cardiopulmonary arrest or shock in the absence of other cardiopulmonary diseases were defined as non-survivors. Patients who died from other causes were excluded from the study group: one patient with intracranial hemorrhage, one patient with acute renal failure, and four patients with septic shock.
Computed tomography examination
The computed tomography scanners used during the study period were two 64-multidetector systems (Somatom Sensation 64, Siemens, Erlangen, Germany; Aquillon 64, Toshiba, Neuss, Germany). In the pulmonary computed tomography angiography examination 60 ml of an iodinated intravenous contrast medium (Solutrast 370 with 370 mg iodine / ml, Bracco Imaging Germany GmbH, Konstanz, Germany) was given at a rate of 2.0 ml / second. Typical imaging parameters were 120 kVp, 150–300 mAs, slice thickness 2 mm, and a pitch of 0.6–1.2 depending on body size. Automatic bolus timing was used with effective delays of 12–25 seconds.
Clinical scores
A clinical score that has been established for PE survival is the pulmonary embolism severity index (PESI) [2]. It estimates the risk of 30-day mortality in patients with acute PE. It will be referred to as ‘original PESI’ in this work.
The original PESI was simplified in 2010 [8]. In the present work this score will be referred to as ‘simplified PESI’. Both scores were included in the present study.
The Acute Physiology and Chronic Health Evaluation II (APACHE II) is a very common severity-of-disease classification system [9]. It is calculated at admission to an intensive care unit and predicts risk of death. We decided to include the APACHE II because it is widely distributed.
Part of the APACHE II, yet a score of its own, is the revised Glasgow Coma Scale (GCS) [10]. As the APACHE II, it is a widely used score with a 15 point neurological scale that aims to record the conscious state of a patient.
A score that is promising and contains a lot of interesting single items is the euroSCORE II. It has been validated to assess risk factors for mortality in adult patients undergoing cardiac surgery [6]. Its latest definition can be found online (www.euroscore.org).
In addition, all single items of the abovementioned scores were tested on their own in their ability to predict 30-day mortality.
Single items of the original and simplified PESI, the euroSCORE II, and the APACHE II were taken from the patient records. The scores were calculated according to the description in the original reports [2,6,8–10].
Some items were contained in more than one score (e.g. age, gender, NYHA, heart rate, respiratory rate, blood pressure, history of cancer).
The three single items of the euroSCORE II that were not applicable to patients with PE were urgency (of surgery), risk of the intervention (of surgery), and surgery on thoracic aorta (yes / no). For calculation purposes, all three items were defined to be 0 (i.e. to have no influence on the score) in all study patients.
Anamnestic features
Anamnestic features that were promising to us are: presence of hemoptysis, acute onset of dyspnea, presence of chronic obstructive pulmonary disease, and presence of any form of anticoagulation prior to PE.
Furthermore, we examined whether admission at night or at weekend influenced prognosis. The information on the day and time of admission was taken from the time at which the patient’s insurance card was read. When the card was read between 8:00 a.m. and 4:00 p.m. the patient was considered as ‘admitted at day shift’. All anamnestic features were taken from patient records.
Statistical analysis
Collected data were evaluated by means of descriptive statistics: absolute and relative frequencies, median and 25%–75% interquartile range, sensitivity, specificity, negative predictive value, and positive predictive value.
The two-tailed Mann-Whitney-U test was used to estimate statistical differences between groups for metric variables. The chi-square-test was used to estimate statistical differences between groups for binary variables (SPSS Version 18, IBM, New York).
The suggested cut off points for measurements to predict 30-day mortality were selected so that the Youden index (sensitivity + specificity − 1) had a maximum value.
Results
In the study group of 365 patients 39 patients (10.7%) died within 30 days due to PE (14 patients respiratory failure due to PE; 25 patients cardiopulmonary arrest due to PE).
Clinical scores
The clinical scores were calculated for each patients. The median of the results for the group of survivors and non-survivors is shown in Table 1. The APACHE II, the GCS, and the original PESI were significantly different in survivors and non-survivors.
Table 1. Clinical scores in survivors and non-survivors (30-day mortality in patients with acute pulmonary embolism).
Scores are sorted in order of ascending p-value.
| survivor* n = 326 | non-survivor* n = 39 | p-value | |
|---|---|---|---|
| APACHE II | 10 (6–15) | 25 (14–32) | <0.0001 |
| Glasgow Coma Scale | 15 (15–15) | 8 (3–15) | <0.0001 |
| original PESI | 109 (79–140) | 168 (138–203) | <0.0001 |
| simplified PESI | 2 (1–3) | 2 (2–3) | 0.0011 |
| euroSCORE II | 2.0 (1.0–6.7) | 6.5 (2.7–12.5) | 0.0026 |
*Median (25%–75% interquartile range)
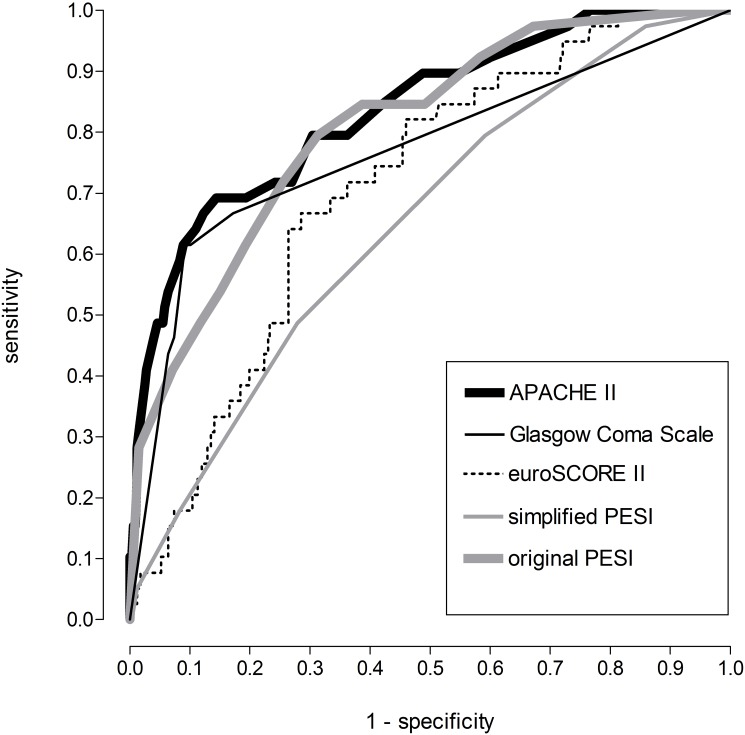
To compare the clinical scores in their ability to predict 30-day mortality a receiver operating characteristic curve was computed (Fig 1). The optimal cut off to predict 30-day mortality according to the Youden index, as well as sensitivity, specificity, positive and negative predictive value were calculated for each score. The results are shown in Table 2. The APACHE II performed best, the simplified PESI performed worst regarding their prognostic value on 30-day mortality in patients with PE.
Fig 1. Receiver operating characteristic curve of clinical scores and their ability to predict 30-day mortality on patients with acute pulmonary embolism.
Table 2. Prediction of 30-day mortality by clinical scores.
Scores are sorted in order of descending Youden index.
| cut off | sensitivity | specificity | PPV | NPV | Youden index | |
|---|---|---|---|---|---|---|
| APACHE II | ≥ 19 | 69% | 86% | 37% | 96% | 55% |
| Glasgow Coma scale | ≤ 10 | 62% | 91% | 44% | 95% | 52% |
| original PESI | ≥ 150 | 82% | 67% | 23% | 97% | 50% |
| euroSCORE II | ≥ 5.9 | 64% | 74% | 23% | 94% | 38% |
| simplified PESI | ≥ 3 | 49% | 72% | 17% | 92% | 21% |
Abbreviation: PPV positive predictive value; NPV negative predictive value
In addition, all single items of the scores were computed for each patient. The median of the results for the group of survivors and non-survivors is shown in Table 3. Eight single items (blood pressure, respiratory rate, pH arterial, post cardiac massage, mechanical ventilation, inotropes, acute renal failure) were significantly (p < 0.0001) different between survivors and non-survivors.
Table 3. Single items of scores in survivors and non-survivors (30-day mortality in patients with acute pulmonary embolism).
Items are sorted in order of ascending p-value.
| survivor* (n = 326) | non-survivor* (n = 39) | p-value | |
|---|---|---|---|
| mean arterial pressure [mm Hg] | 80 (73–91) | 66 (56–79) | <0.0001 |
| systolic blood pressure [mm Hg] | 111 (100–125) | 94 (78–111) | <0.0001 |
| respiratory rate [breaths per minute] | 23 (21–23) | 25 (23–31) | <0.0001 |
| pH arterial [] | 7.431 (7.400–7.475) | 7.334 (7.156–7.468) | <0.0001 |
| critical preoperative state [yes / no] † | |||
| » post cardiac massage [yes / no] | 6% (19) | 56% (22) | <0.0001 |
| » mechanical ventilation [yes / no] | 12% (38) | 77% (30) | <0.0001 |
| » inotropes or intra aortal balloon pump [yes / no] | 13% (42) | 67% (26) | <0.0001 |
| » acute renal failure (anuria or oliguria <10ml / hour) [yes / no] | 6% (19) | 28% (11) | <0.0001 |
| » ventricular tachycardia or ventricular fibrillation or aborted sudden death [yes / no] | 13% (44) | 28% (11) | 0.0152 |
| heart rate [beats per minute] | 106 (90–119) | 120 (100–130) | 0.0018 |
| potassium K+ (serum) [mmol/l] | 4.1 (3.8–4.6) | 4.3 (4.0–5.1) | 0.0034 |
| Chronic health points † | |||
| » organ insufficiency [yes / no] | 54% (175) | 77% (30) | 0.0057 |
| » post emergency surgery [yes / no] | 8% (25) | 18% (7) | 0.0319 |
| » no previous surgery [yes / no] | 77% (252) | 69% (27) | 0.2617 |
| » post elective surgery [yes / no] | 17% (57) | 18% (7) | 0.9425 |
| left ventricular ejection fraction (LVEF) † | |||
| » LVEF ≥ 50% | 69% (226) | 51% (20) | 0.0231 |
| » LVEF < 50% | 31% (100) | 49% (19) | 0.0231 |
| » LVEF < 30% | 6% (21) | 15% (6) | 0.0437 |
| » LVEF < 20% | 2% (7) | 5% (2) | 0.2566 |
| chronic lung disease [yes / no] | 17% (54) | 31% (12) | 0.0293 |
| creatinine [μmol/l] | 92 (76–111) | 120 (86–154) | 0.0915 |
| Saturation [%] | 92 (87–97) | 92 (85–98) | 0.0440 |
| extracardiac arteriopathy [yes / no] † | |||
| » claudication [yes / no] | 6% (20) | 13% (5) | 0.1182 |
| » previous or planned intervention on the abdominal aorta, limb arteries or carotids [yes / no] | 10% (31) | 13% (5) | 0.5121 |
| » carotid occlusion or >50% stenosis [yes / no] | 3% (10) | 3% (1) | 0.8620 |
| » amputation for arterial disease [yes / no] | 0% (0) | 0% (0) | N/A |
| angina at rest [yes / no] | 14% (46) | 5% (2) | 0.1167 |
| hematocrit [%] | 38 (32–41) | 35 (31–40) | 0.1491 |
| age [years] | 63 (53–75) | 67 (58–76) | 0.1533 |
| poor mobility [yes / no] | 17% (55) | 26% (10) | 0.1760 |
| active endocarditis [yes / no] | 1% (2) | 3% (1) | 0.2022 |
| History of cancer [yes / no] | 29% (96) | 38% (15) | 0.2475 |
| white blood cell count (x1000) | 10.0 (8.5–12.5) | 13.5 (10.0–18.6) | 0.3016 |
| NYHA † | |||
| » NYHA I | 16% (51) | 10% (4) | 0.3740 |
| » NYHA II to IV | 43% (140) | 44% (17) | 0.9387 |
| » NYHA III to IV | 27% (88) | 21% (8) | 0.3849 |
| » NYHA IV | 11% (35) | 13% (5) | 0.6937 |
| sodium Na+ (serum) [mmol/l] | 138 (136–140) | 138 (134–140) | 0.4056 |
| temperature (rectal) [°C] | 37.0 (36.9–37.5) | 37.0 (36.5–37.8) | 0.5034 |
| diabetes [yes / no] | 29% (93) | 33% (13) | 0.5320 |
| previous cardiac surgery [yes / no] | 8% (26) | 10% (4) | 0.6240 |
| recent myocardial infarction [yes / no] | 6% (21) | 8% (3) | 0.7658 |
| severe pulmonary hypertension (> 55 mm Hg) [yes / no] | 14% (47) | 13% (5) | 0.7874 |
| Male sex [yes / no] | 49% (159) | 49% (19) | 0.9948 |
*Median (25%–75% interquartile range) of metric variables and percent (number) of categorical variables.
† subitems (grey underground) were kept together and ranked according to the subitem with the lowest p-value.
For single items of the scores that showed a highly significant difference between groups (p < 0.0001) an optimal cut off to predict 30-day mortality according to the Youden index was calculated. The results are shown in Table 4.
Table 4. Prediction of 30-day mortality by single items of clinical scores.
Items are sorted in order of descending Youden index.
| cut off | sensitivity | specificity | PPV | NPV | Youden index | |
|---|---|---|---|---|---|---|
| » mechanical ventilation [yes / no] | yes | 77% | 88% | 44% | 97% | 65% |
| » inotropes or intra aortal balloon pump [yes / no] | yes | 67% | 87% | 38% | 96% | 54% |
| » post cardiac massage [yes / no] | yes | 56% | 94% | 54% | 95% | 51% |
| pH arterial [] | < 7.335 | 54% | 92% | 44% | 94% | 46% |
| mean arterial pressure [mm Hg] | < 67 | 56% | 84% | 30% | 94% | 41% |
| systolic blood pressure [mm Hg] | < 99 | 56% | 78% | 24% | 94% | 35% |
| respiratory rate [breaths per minute] | ≥ 25 | 51% | 83% | 26% | 93% | 34% |
| acute renal failure (anuria or oliguria <10ml / hour) [yes / no] | yes | 28% | 94% | 37% | 92% | 22% |
Abbreviation: PPV positive predictive value; NPV negative predictive value
Anamnestic features
Anamnestic features were computed for each patient. The median of the results for the group of survivors and non-survivors is shown in Table 5. Anamnestic feautures were not significantly different between survivors and non-survivors. Therefore, no cut off values were calculated.
Table 5. Anamnestic features in survivors and non-survivors (30-day mortality in patients with acute pulmonary embolism).
Features are sorted in order of ascending p-value.
| survivor* (n = 326) | non-survivor* (n = 39) | p-value | |
|---|---|---|---|
| acute Dyspnea [yes / no] | 53% (173) | 69% (27) | 0.0552 |
| chronic obstructive pulmonary disease [yes / no] | 11% (36) | 18% (7) | 0.2061 |
| Admitted at weekday [yes / no] | 79% (257) | 85% (33) | 0.3984 |
| hemoptysis [yes / no] | 6% (18) | 3% (1) | 0.4320 |
| Admitted at day shift [yes / no] | 57% (186) | 54% (21) | 0.7022 |
| Oral anticoagulation prior to PE [yes / no] | 36% (118) | 36% (14) | 0.9707 |
* percent (number)
Discussion
A recent meta-analysis [3] found an overall mortality of 6.5% in 2.288 patients. In some studies mortality rates of up to 18% [11] were described. Another meta-analysis with about 20.000 patients described a mortality of 10.7% [12]. Therefore, the mortality found in the present study confirms findings of the literature.
Clinical scores
The present results confirm the prognostic value of the original PESI. The optimal cut off found in the present study marks patients of the highest risk class in the original definition of the score [2]. Contrary to other studies [8], the simplified PESI did not performed equally well compared to the original PESI. Again, the optimal cut off found in the present study marks patients of high risk according to the original definition of the score [8].
The scores that were specifically developed to predict 30-day mortality in PE did not perform superior in our study group. We attribute this to the lack of specificity (see also Table 2). The PESI was derived from a patient population of 186 hospitals [2]. In contrast, the present results were derived from a hospital of maximum medical care which results in a higher fraction of patients with severe co-morbidities. However, co-morbidities result in a higher risk class in the PESI, making the score less specific in the present patient group.
The euroSCORE II that is validated in assessing mortality risk in cardiac surgical adult patients [6] had an inferior prognostic value in patients with PE compared to the original PESI. In addition, the score is computed from a large number of single items. Therefore, we do not suggest using it in clinical routine for determining the prognosis in patients with PE. In retrospect, the score performed worse than expected in the present study. Nevertheless, the calculation of the score was useful because a number of single items of the score turned out as very good prognostic parameters.
The APACHE II predicts risk of death and is calculated at admission to an intensive care unit. It is remarkable, that the score performed slightly better than the original PESI in determining mortality in patients with PE. The optimal cut off found in the present study marks a mortality of 25% and higher according to the original definition of the score [9].
We assume that the good performance of the APACHE II is based on two facts. Firstly, the score is not devoted to a specific disease (e.g. contrary to the euroSCORE II that is devoted to cardiac surgical adult patients). Therefore, it can track risk factors that are independent of specific disease features. Secondly, the APACHE II was derived from intensive care unit patients. These patients usually have a high number of severe co-morbidities. Therefore, the patient group in the present study might have been similar to the patient group from which the APACHE II was derived.
The Glasgow Coma Scale (GCS) performed equally well in predicting mortality compared to the APACHE II and the original PESI. The scale has been established for predicting mortality after traumatic brain injury and it is an item in a considerable number of other scores devoted to prognosis [9,13]. However, no studies on the use of the Glasgow Coma Scale alone in predicting 30-day mortality in PE have been done before as far as we know.
Some single items of scores performed equally well or even better in predicting mortality compared to the best clinical scores. Contrary to clinical scores, single items are much faster to ascertain. The best three of them (mechanical ventilation, post cardiac massage, inotropes or intra aortal balloon pump) have a high specificity. However, they cannot be applied to less severely ill patients.
In this case, the other variables may be helpful: arterial pH, respiratory rate and blood pressure are fast, cheap and reliable to measure. The GCS and the abovementioned single items have in common that they are indicators of a threatening circulatory or conscious state. In addition, they are independent from specific disease feature. The advantage of these simple measurements is maybe, that they are “too dumb to fool”.
The high prognostic value of simple measurements has also previously been reported [14].
Anamnestic features
It is known that PE presents more significantly in patients with chronic obstructive pulmonary disease than in others [15]. However, in our study group it had no significant influence on prognosis.
The presence of acute dyspnea compared to slowly progressing dyspnea could be an indicator of more severe PE. The present data supported this thesis. Yet, differences were not significant.
It is to presume that on the one hand, the use of any form of anticoagulation prior to PE indicates a pre-existing morbidity resulting in a higher mortality. On the other hand, the anticoagulation should work against more severe PE. None of these speculations was proven by the present data.
It is a sign of quality that patients admitted at night at weekend had statistically a similar prognosis than patients admitted at day at the middle of the week.
Limitations
Due to the retrospective nature of our study comorbidities were defined solely by provider documentation in the patient chart review. Therefore, undescribed comorbidities could be missed. By excluding patient deaths that were not directly related to PE, complications of PE therapy and PE mortality might be underestimated.
Conclusion
In a patient group with severe co-morbidities the simplified PESI might be not specific enough. The results of the present study provide support for enhancing efforts toward identifying PE patients at risk of death. The original PESI, the APACHE II, and the Glasgow Coma Scale perform almost equally well in predicting mortality in patients with PE. However, the Glasgow Coma Scale is by far the score that is easiest to ascertain. Nevertheless, a number of circulatory parameters show equally or even better prognostic value. When implementing preventive strategies among patients with PE and severe co-morbidities the results of the present study support the selection of appropriate parameters.
Data Availability
All relevant data are within the paper.
Funding Statement
The authors have no support or funding to report.
References
- 1.Sanchez O, Trinquart L, Colombet I, Durieux P, Huisman MV, Chatellier G, et al. (2008) Prognostic value of right ventricular dysfunction in patients with haemodynamically stable pulmonary embolism: a systematic review. Eur Heart J 29: 1569–1577. 10.1093/eurheartj/ehn208 [DOI] [PubMed] [Google Scholar]
- 2.Aujesky D, Obrosky DS, Stone RA, Auble TE, Perrier A, Cornuz J, et al. (2005) Derivation and validation of a prognostic model for pulmonary embolism. Am J Respir Crit Care Med 172: 1041–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Masotti L, Righini M, Vuilleumier N, Antonelli F, Landini G, Cappelli R, et al. (2009) Prognostic stratification of acute pulmonary embolism: focus on clinical aspects, imaging, and biomarkers. Vasc Health Risk Manag 5: 567–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jimenez D, Lobo JL, Monreal M, Moores L, Oribe M, Barron M, et al. (2014) Prognostic significance of multidetector CT in normotensive patients with pulmonary embolism: results of the protect study. Thorax 69: 109–115. 10.1136/thoraxjnl-2012-202900 [DOI] [PubMed] [Google Scholar]
- 5.Henzler T, Roeger S, Meyer M, Schoepf UJ, Nance JW Jr., Haghi D, et al. (2012) Pulmonary embolism: CT signs and cardiac biomarkers for predicting right ventricular dysfunction. Eur Respir J 39: 919–926. 10.1183/09031936.00088711 [DOI] [PubMed] [Google Scholar]
- 6.Roques F, Michel P, Goldstone AR, Nashef SA (2003) The logistic EuroSCORE. Eur Heart J 24: 881–882. [DOI] [PubMed] [Google Scholar]
- 7.Torbicki A (2010) Pulmonary thromboembolic disease. Clinical management of acute and chronic disease. Rev Esp Cardiol 63: 832–849. [DOI] [PubMed] [Google Scholar]
- 8.Jimenez D, Aujesky D, Moores L, Gomez V, Lobo JL, Uresandi F, et al. (2010) Simplification of the pulmonary embolism severity index for prognostication in patients with acute symptomatic pulmonary embolism. Arch Intern Med 170: 1383–1389. 10.1001/archinternmed.2010.199 [DOI] [PubMed] [Google Scholar]
- 9.Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13: 818–829. [PubMed] [Google Scholar]
- 10.Teasdale G, Jennett B (1974) Assessment of coma and impaired consciousness. A practical scale. Lancet 2: 81–84. [DOI] [PubMed] [Google Scholar]
- 11.Vedovati MC, Germini F, Agnelli G, Becattini C (2013) Prognostic role of embolic burden assessed at computed tomography angiography in patients with acute pulmonary embolism: systematic review and meta-analysis. J Thromb Haemost 11: 2092–2102. 10.1111/jth.12429 [DOI] [PubMed] [Google Scholar]
- 12.Gong XW, Yuan YD (2013) [Meta-analysis of risk factors for all-cause mortality of pulmonary thromboembolism]. Zhonghua Yi Xue Za Zhi 93: 2534–2540. [PubMed] [Google Scholar]
- 13.Ahun E, Koksal O, Sigirli D, Torun G, Donmez SS, Armagan E (2014) Value of the Glasgow coma scale, age, and arterial blood pressure score for predicting the mortality of major trauma patients presenting to the emergency department. Ulus Travma Acil Cerrahi Derg 20: 241–247. 10.5505/tjtes.2014.76399 [DOI] [PubMed] [Google Scholar]
- 14.Castelli R, Bucciarelli P, Porro F, Depetri F, Cugno M (2014) Pulmonary embolism in elderly patients: Prognostic impact of the Cumulative Illness Rating Scale (CIRS) on short-term mortality. Thromb Res. [DOI] [PubMed] [Google Scholar]
- 15.Bertoletti L, Quenet S, Mismetti P, Hernandez L, Martin-Villasclaras JJ, Tolosa C, et al. (2012) Clinical presentation and outcome of venous thromboembolism in COPD. Eur Respir J 39: 862–868. 10.1183/09031936.00058811 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.