Abstract
Background
Young adults display substantial weight gain. Preventing this age-related weight gain would reduce overweight and obesity.
Objective
We evaluated an internet based intervention using Internet-connected scales and graphic email feedback; the Caloric Titration Method (CTM), to reduce age-related weight gain over the course of 1 y among first-year college students.
Design
First-year college students (n=167) were randomized to (CTM) or control (C) group. Both groups were provided Internet-connected scales. CTM group was instructed to weigh daily, view a weight graph emailed to them after weighing, and try to maintain their weight as indicated in the graph. The C group could weigh at any time, but did not receive feedback. At six months and 1 year the C group were notified to provide weights. Intention to treat analysis, using a mixed model adjusted for baseline weight, BMI and gender was used to analyze the effect of the intervention.
Results
Baseline Body Mass Index was 22.9 ± 3.0 kg/m2. Frequency of self-weighing (median) was 5 times/week in the CTM group, compared to 1 time/week in C (p<0.001). Ninety-five percent of the CTM participants weighed ≥3 times/week, compared to 15% in C group (p<0.001). After 1 year the C group had gained 1.1 ± 4.4 kg whereas the CTM group lost 0.5 ± 3.7 kg, yielding a significant overall time*group interaction (F=3.39, p=0.035). The difference in weight change between the two groups at 1 year was significant (p=0.004). Weight change of the CTM group was not different from zero whereas weight gain in C group was significant. Retention was 81%.
Conclusions
The internet based frequent self-weighing CTM system was effective in preventing age-related weight gain in young adults over one year and thus offers promise to reduce overweight and obesity.
INTRODUCTION
Young American adults gain on average ~0.9 kg per year (1). For a marjority, this accumulates to overweight or obesity, increasing the risk of many chronic diseases and has proven very difficult to reverse (1–5). This postadolecent weight gain is labeled age-related weight gain. Data derived from the Behavioral Risk Factor Surveillance dataset demonstrate that body weight increases past adolescence until mid-life (2,6). A portion of this weight gain may be a part of the normal aging process (7,8), but a large part may be due to eating evoked by the environment causing imbalances in energy intake relative to energy expenditure (9,10).
The maximum rate of increase in body weight occurs between the ages about 18 to 25; a life-forming period labeled emerging adulthood (11). Although not specific to college-attending young adults, there is considerable evidence that rapid weight gain occurs the first year of college, and at a lower rate through the remainder of college (12–17). Reducing the rate of rise in body weight during this period of time would drastically reduce the overall prevalence of adult overweight and obesity (18), consistent with U.S. Healthy People 2020 national objectives (19). Unfortunately, preventive interventions aimed at young adults are few, evidence for efficacy is low, and strategies often rely on intensive time and resource demanding interventions (20,21).
Frequent self-weighing has been found to correlate significantly with weight control (22). However, experimental evidence demonstrating that self-weighing prevents weight gain is inconclusive. In 2006, Levitsky et al. published results from the first study to successfully block age-related weight gain in a sample of female first-semester university students using daily self-weighing and electronic graphic feedback in a program called the Caloric Titration Method (CTM) (23). Two other studies utilizing frequent self-weighing in first-year students did not observe frequent weighing to prevent weight gain (24,25). These latter studies may have been underpowered and/or not long enough to detect significant effects on weight, and also the participants were not motivated or instructed to maintain weight, nor provided with a target weight or electronic graphic feedback.
The purpose of the present study was to clarify the effectiveness of self-weighing to prevent weight gain and extend the findings of Levitsky et al.(23) by (a) using both males and females, (b) increase the time span for the study from 3 months to 12 months and (c) to test the effectiveness of internet based scales with the CTM to prevent age-related weight gain.
SUBJECTS AND METHODS
Study participants
In August through December 2012 eligible first-year students at Cornell University, Ithaca, NY, USA, were recruited through flyers, announcements in classes with a high proportion of first-year students, and e-mails via University list serves. Inclusion criteria were: first-year college student, age 18–25 years, and a self-reported body mass index (BMI) ≥18.5 kg/m2. Exclusion criteria were: diabetes, pregnancy or planning to become pregnant during study, an eating disorder or history thereof, and a score of >45 on the drive for objective thinness questionnaire (26). Procedures were approved by the Cornell University Institutional Review Board. All participants provided written informed consent.
Study design
Two online questionnaires were used to screen for eligibility (survey one) and further assess baseline characteristics (survey two) among interested individuals. The surveys were provided via an individual email with an internet link to an encrypted website (Qualtrics, 2009, v. 12,018, Provo, Utah, USA). Data on gender, age, weight and height, race/ethnicity, and other eligibility criteria were collected. Then, eligible participants were randomized to the CTM or C group. All participants were provided with an internet connected, commercial, digital scale (WiFi body scale, WiThings, Paris, France) and were asked to weigh themselves on three days during one week at baseline (i.e. direct after enrollment), six months, and 1 year.
The Caloric Titration Method: WiFi body scale and visual feedback system
The CTM is based on daily self-weighing and visual weight feedback. It consists of (a) daily self-weighing, and (b) an automated email containing a graph of the user’s weight plotted over time, sent immediately after each weighing. The graph also contains a horizontal reference line indicating the target, i.e. starting, weight (average of the first eight days weights). Additionally, (c) a computer program identifies and sends email reminders when 3 days of daily weights have not been transmitted from the scale to the database. The data from the scale is transmitted through local WiFi to the Withings website where it is relayed to servers at Cornell University and the CTM software. The CTM participants were disconnected from to the scale-manufacturer’s data or site, to avoid manipulation of settings or weight data that could compromise the research database.
Intervention conditions
Information to all participants
During the start-up session the C and CTM groups separately watched a short (22 min) video lecture in which the PI (DAL) informed them that the objective of the study was the evaluation of stability of body weight over the college experience, that the young adulthood time-period is important because evidence shows that weight change during this period may predispose them to medical risks later in life, and were provided with various evidence based techniques they could use if they found themselves gaining weight.4 They were informed on how to set up and connect the scale, and C and CTM groups were given group-specific information on how to use the scale.
Experimental condition: Frequent Self-Weighing using CTM
The CTM group was asked to view the e-mailed graph of their weight daily, and try not to gain weight above the target weight reference line indicated in the graph. The participants were asked to place their scale close to their bed so that they could weigh themselves as soon as they rose from bed each morning. They were not required to take their scales with them when traveling, except during summer vacation where they asked to take the scale with them and use it daily as before.
Control condition
Control participants were informed that they would be contacted via email when to provide weight measurements for the study by weighing themselves on three separate days within one week using their WiFi-scale. These measurements were requested every six months. They were free to weigh themselves whenever they wished, so that the normal frequency of self-weighing and its effect would not be underestimated. Though the weight data and frequency of weighing would be available to the research team, no data or graphic feedback was emailed to the control participants.
Study outcomes
The primary outcome was weight gain prevention, i.e. change in body weight from baseline, measured as a) different from zero, and b) difference between control and intervention groups. BMI was evaluated the same way. Measure of treatment was frequency of self-weighing. Gender differences were explored.
Primary outcome
Body weight change
Body weight was calculated as the average of the three first weight readings on different days during one week, using the WiFi-body scale with a precision of 0.05 kg. The participants were instructed to provide all weights under similar conditions, preferably first thing after rising from bed wearing only light underclothing. Change in body weight was calculated as the difference between baseline body weight and body weight at subsequent measurement points.
Body Mass Index
BMI was calculated using the measured body weight and self-reported height. Change was calculated as the difference between baseline BMI and BMI at subsequent measurement points.
Measure of treatment
Frequency of self-weighing
Frequency of self-weighing was measured by the number of weight measurements recorded by the WiFi-body scale, and calculated as the total number of measurements divided by the number of weeks of participation. Thus the frequency is expressed as number of weight measurements per week.
Indicator of adverse effects
Rapid weight change and/or negative experience
Rapid weight change could be a consequence of unhealthful weight control practices, or sign of other medical problem. It was registered as a potential adverse event, and defined as; if the participant lost or gained >5% of the prior week’s average weight in a one week period. All participants in CTM group were monitored for rapid changes in weight by a built in feature of the CTM software. If a rapid weight change was indicated the weight data was scrutinized and the participant contacted for a check-up. The participant was asked about their general health, specific symptoms associated with conditions that could be indicated by rapid weight change, lifestyle and whether they perceived their weight change problematic. Alternatively, if a participant felt negatively affected in any way by self-weighing or if any other issue emerged, they were advised to contact the study staff. The participant would be advised to withdraw from the study and receive counsel through health services at campus, if a) the weight change was suspected to be caused by a medical condition, or b) if the participant was found to be engaging in unhealthful weight control behaviors (practicing a nutritionally compromised diet, engaging in excessive exercise, and/or maintaining weight below BMI 18.5 kg/m2, as evaluated by a Registered Dietitian), or experience adverse psychological effects of the weight monitoring.
Statistical analysis
The sample size was calculated based on a predicted difference in body weight change between CTM and C group (0.0 ± 1.4 kg vs. 0.7 ± 1.4 kg), corresponding to blocked vs. expected 1 y weight gain. Assuming a dropout rate of 25%, 79 participants per group would be needed to detect a significant difference between these two groups with 80% power. Differences between groups at baseline were evaluated with t-test and Fisher’s exact test. Unadjusted analyses of observed trial outcomes were performed with independent and paired t-tests, including only participants providing baseline and six month and/or 12 month weight measurement, respectively. Intention to treat analyses included all participants with baseline and at least one additional weight measurement.
The data were analyzed with a Bonferroni adjusted repeated measures linear mixed model allowing a) adjustment for covariates; baseline weight, BMI, and gender, b) accounting for correlation between repeated measures within subjects, and c) handling missing data using restricted maximum likelihood estimations. The fixed effects in the model were group, time, and their interaction term. In analysis of gender the group, time and gender interaction was analyzed. A general linear model analysis using last value carried forward, i.e. last value recorded by the WiFi-body scale at any time between the baseline, and six month and 1 year follow-ups, was also used to corroborate the intent to treat analysis. Change in outcome variables was calculated as the value obtained at six months and 1 year minus the baseline value, or for last value carried forward the last data recorded by the WiFi-body scale. Statistical significance was indicated by p values < 0.05. All statistical analyses were performed using the SPSS software (version 20.0, IBM, Somers, NY).
RESULTS
Study participants
A total of 355 individuals completed the first screening survey during the Fall semester 2012, and among these, 310 were eligible to take the second survey. The second survey was completed by 221 individuals between January 2013 and March 2013. Among these 167 volunteered to participate, and were randomized to C (n=82) or CTM (n=85) group, see Figure 1 for baseline characteristics. Self-identified race and ethnicity was white; 64%, black/African American; 5%, Asian; 32%, American Indian/Alaska native; 4%, native Hawaiian/other Pacific islander; 2%, and other; 10% respectively, and 13% as Hispanic. Race and ethnicity were not different between CTM and C groups. Among those randomized that provided baseline measurements, 135 (84%) completed the 6 month follow-up, and 129 (81%) remained to complete the 1 year follow-up (Figure 1). Mean duration of participation was 377 ± 94 days, with no difference between groups (CTM 366 ± 95 days; C 388 ± 92 days, p=0.152). Nineteen participants (10 females, 9 males) discontinued the CTM over the course of the year. Ten discontinued the C group 10 (6 females, 4 males). Their BMIs were not significantly different from those who remained in the study (p=0.605 and 0.124 in CTM and C respectively). Reasons for discontinuing were: lost interest, travel, uncomfortable with weight monitoring, internet connection issues. One CTM participant was excluded from analysis after repeated episodes of indecisiveness about leaving the trial. Among participants remaining in the trial, baseline characteristics and anthropometric variables did not differ significantly between the two groups (Table 1).
Figure 1.
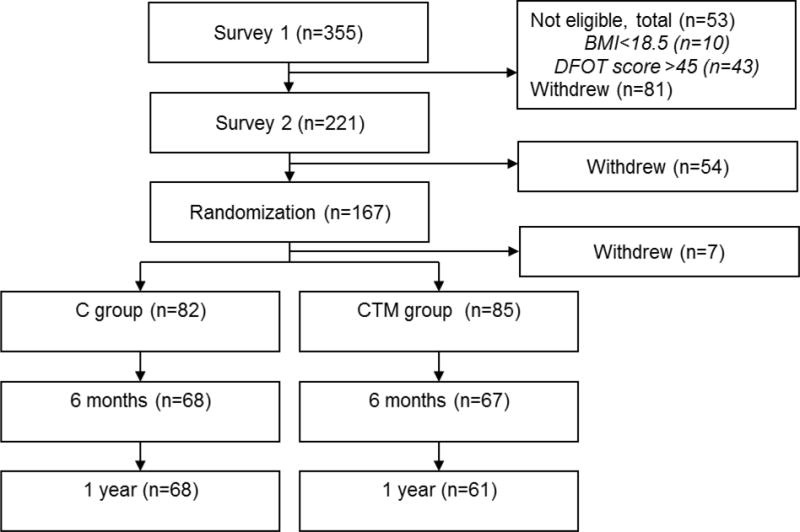
Screening, randomization, and follow-up of study participants in the frequent self-weighing and visual feedback to prevent age-related weight gain among young adults trial. DFOT denotes drive for objective thinness, C control, and CTM Caloric Titration Method.
Table 1.
Baseline characteristics of study participants.*
| Variable | Control Group | CTM Group | |
|---|---|---|---|
| n=781 | n=812 | p-value | |
| Age, y | 19 ± 0.4 | 19 ± 0.4 | 0.431 |
| Gender, female/male | 39/39 | 47/34 | 0.241 |
| Body Mass Index, kg/m2 | 22.7 ± 2.9 | 23.0 ± 3.1 | 0.494 |
| Body weight, kg | 66.6 ± 12.5 | 67.6 ± 12.5 | 0.621 |
| Body weight, kg, females | 59.2 ± 8.8 | 61.6 ± 8.4 | 0.394 |
| Body weight, kg, males | 74.1 ± 11.2 | 76.4 ± 12.3 | 0.208 |
| Body Mass Index categories | |||
| <24.9 kg/m2, % | 80 | 77 | 0.691 |
| 25-29.9 kg/m2, % | 17 | 19 | 0.832 |
| ≥30 kg/m2, % | 3 | 4 | 0.675 |
Values are means ±SD. Significant differences among groups were determined by t-test for continuous variables, and Fisher’s exact test for categorical variables.
Randomized n=82, of which 4 never initiated trial or provided data.
Randomized n=85, of which 3 never initiated trial or provided data, and 1 was excluded from analysis.
CTM denotes Caloric Titration Method.
Effects of the CTM self-weighing intervention
Treatment implementation indicators
The median (interquartile range) frequency of self-weighing in the CTM group was at six months and 1 year, respectively, 5.0 (2.1) and 5.8 (1.7) times/week, compared to 0.8 (1.1) and 1.0 (0.9) times/week in C group (all between group comparisons p<0.001). There were no differences between frequencies of weighing between the first six months of testing and the last six months, nor between females and males. Among CTM-participants 95% weighed themselves ≥3 times/week and 67% weighed themselves ≥5times/week, compared to 15% and 9% in C (both p<0.001).
Intervention outcomes
Body weight change trajectories, as analyzed with the adjusted mixed model (intention to treat), are displayed in Figure 2. Over the course of the year, the CTM group lost 0.5 ± 3.7 kg, whereas C group gained 1.1 ± 4.4 kg (Table 2), yielding a significant overall time*group interaction (F=3.39, p=0.035). The difference in weight change between the two groups at 1 year was significant (p=0.004). These findings were corroborated using an independent t-test (only participants completing the intervention measurements), as well as using the last value carried forward in a general linear model.
Figure 2.
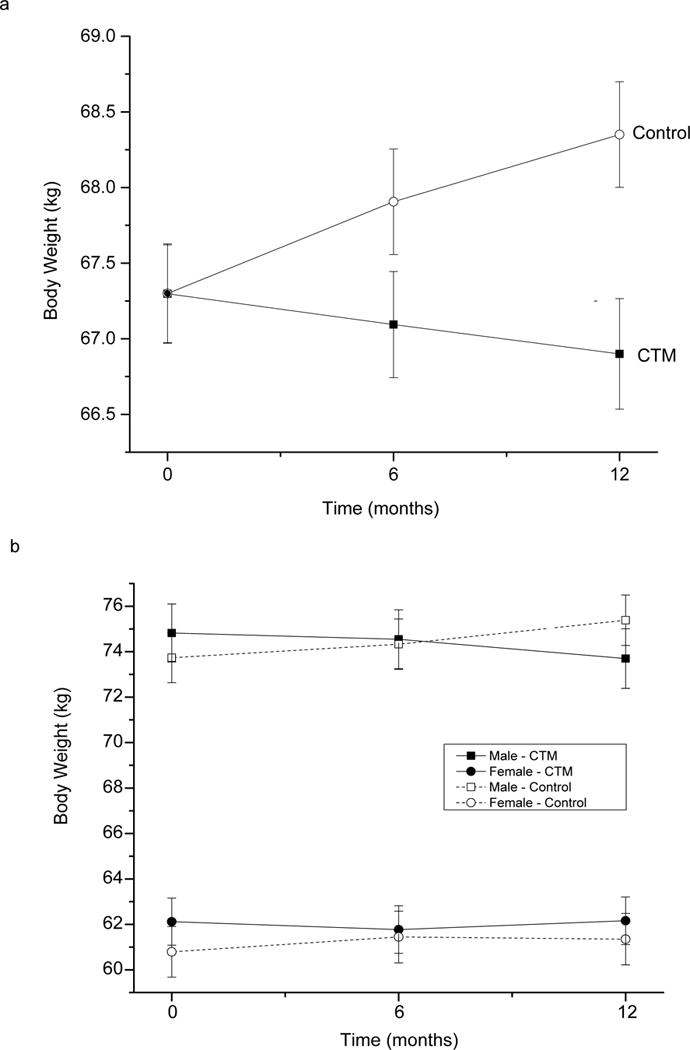
Body weight change in C and CTM groups over 1 year. Estimated means of 6 months and 1 year body weight change, as determined by mixed model, adjusted for baseline weight, BMI, and gender. In C n=78, and in CTM n=81. Error bars are 95% CI. CTM denotes Caloric Titration Method.
Table 2.
Effects of a frequent self-weighing intervention with electronic graphic feedback on weight change over 1 year among young adults.*
| Variable | Control Group | CTM Group | Between group
difference p-value |
||
|---|---|---|---|---|---|
| n=781 | n=812 |
t-test3 (Observed Data) |
Mixed model4 (Intent-to-Treat) |
||
| Treatment outcomes | Pairwise comparisons | Overall group*time interaction | |||
| Weight, kg | |||||
| Change at 6 months | 0.64 ± 3.57 | −0.19 ± 2.89 | 0.142 | 0.085 | |
| Change at 1 year | 1.08 ± 4.38 | −0.47 ± 3.66 | 0.032 | 0.004 | 0.035 |
| Body mass index, kg/m2 | |||||
| Change at 6 months | 0.22 ± 1.17 | −0.06 ± 0.98 | 0.142 | 0.061 | |
| Change at 1 year | 0.35 ± 1.40 | −0.15 ± 1.23 | 0.032 | 0.003 | 0.033 |
Values are observed values; means ± SD, for group outcomes. Significant differences between treatment outcomes were determined by t-test and repeated measures mixed model analysis.
Randomized n=82, of which 4 never initiated trial or provided data. At the 6 month and 1 year follow-ups, respectively, the number of participants was reduced to: n=68 and 68.
Randomized n=85, of which 3 never initiated trial or provided data, 1 excluded from analysis. At the 6 month and 1 year follow-ups, respectively, the number of participants was reduced to: n=67 and 61
Students t-test, including only participants who provided baseline, 6 month, and/or 12 month data (Observed Data), (Control n= 78, 68, 68, CTM n=81, 67, 61).
Covariates appearing in the adjusted model: baseline weight and BMI, and gender. All randomized participants initiating trial included in analysis (Intent-to-Treat), (n=78 and 81 in Control and CTM, respectively).
CTM denotes Caloric Titration Method.
The weight loss in CTM group was not different from zero; as analyzed by the adjusted mixed model; mean −0.5 kg, 95% CI −1.1 – 0.3. The weight gain in C group, on the other hand, was significantly different from zero; mean 1.1 kg, 95% CI 0.4 – 1.8, (p=0.033). Corresponding changes occurred in BMI (Table 2).
Gender differences and weight trajectories
Although no difference in the frequency of weighing was observed between males and females at either six or 12 months in either the CTM or the C group, the pattern of weight change appeared to differ. Males in the CTM group maintained a consistent reduction in weight from six to 12 months. The C group males also maintained a consistent trend by continuing to gain weight from six to 12 months.
Unlike the males, females in the CTM group did not continue to lose weight. Between six and 12 months a non-significant regain of 0.5 ± 2.4 kg (p=0.186) was observed. Similarly, females in the C group did not continue to gain weight, like the males, but maintained their six month weight gain; the difference between six and 12 months was 0.1 ± 2.2 kg (p=0.984). Thus at 1 year the difference between the female CTM and C groups failed to reach statistical significance (p=0.442), whereas among males it was highly significant (p<0.001). The weight change over months 1–6 was negatively correlated with weight change over months and 7–12 among females in C group (r −0.64, p<0.001) but not in CTM group nor among males in either group. Although this pattern of weight change appears different between the genders the weight*time*gender interaction was only borderline significant (F=2.43, p=0.09).
Adverse events
The CTM administrative system generated five reports of rapid weight changes. When the participants were contacted no evidence of health problems were reported. Rather, the weight changes were caused by someone else trying the scale (n=2) or weighing another object (n=3). Two participants discontinued the intervention because the self-weighing was perceived to be associated with an undesirable focus on weight and diet. However, no alarmingly rapid weight gain or loss (1.3 kg over 3 months, −0.5 kg over six months), unhealthy low weight (both BMI 22 kg/m2), or disordered eating was found.
DISCUSSION
This study demonstrates, in a randomized controlled trial of 1 year, that frequent self-weighing with electronic graphic feedback produces a significant reduction of age-related weight and BMI gain among young adults. The diverging weight trajectories between CTM and C groups showed a significant difference in weight change from baseline over 1 year. The intervention prevented any significant weight gain over a period of 1 year, whereas the weight gain of the controls was significantly greater than zero.
Considering that ~95% of young adults are on weight gain trajectories (27), that young adults on average gain substantially (1,2,12–17,27), and that both the amount and rate of weight gain in this age group highly increases the risk of long-term excess weight gain and morbidity (3,4), the potential benefits of the CTM are substantial.
Higher frequency of self-weighing has been shown to be associated with weight control; mainly weight loss and maintenance of weight loss (28). Although early findings were conflicting, later experimental studies found frequent self-weighing, by itself, to produce a significant weight loss, and the correlation between the frequency of self-weighing and success at losing or maintain weight has been established (28).
The published evidence for effective preventive measures is poor for all strategies tested to-date, based on a recent systematic review in adults (20), and a systemic review evaluating college-based trials separately (21). Most trials focused on healthy eating, and/or exercise and some resulted in changes in measures of behavioral change, but effects on weight were limited (20,21). The one long term college-based intervention producing prevention of weight gain (29), built on 23 seminars lasting 45 min each to teach nutrition and exercise, over 24 months. Similar to our trial, after 1 year the intervention group had reduced mean weight by 0.2 kg, and weight had increased by 1.2 kg in controls. However, such programs depend on a consistent human interactions which increase costs.
In our trial the control group gained weight at an expected rate; a rate slightly lower than what has been documented on average for the first semester (range 0.6 – 1.9 kg) (12,13,16,30), which is reasonable as the intervention started the second semester. We were able to collect an objective measure of the frequency of weighing in the control group; the percentage of participants weighing ≥3 times/week (15%), was comparable to a large sample of young adults where 15% self-reported weighing “a few times per week or more” (31).
Our findings indicate that weight change across 1 year were different for females and males. The initial weight reduction in females in the CTM group, and increase in weight in females in the control group, was consistent with the previous trial by Levitsky et al. (23). However, following the six-month measurement in this longer trial females in C group did not continue to gain weight, but actually maintained their weight, and a negative correlation between weight changes the first six months compared to the latter was observed. A possible explanation is that those females in the C group who observed they had gained weight responded with a reduction in subsequent energy intake in order to lose the weight gained. A possible reason the same effect was not observed in males is that males have been found to be less concerned about the negative effects of weight gain than women (32–34). This may have been exacerbated by giving the controls scales they could put in their dorm room or apartments, allowing them to see the consequence of their eating behaviors during the first semester; similar to how the control condition in weight loss interventions may prevent expected weight gain (35), and how weight control is enhanced when people know they are being observed (36–39). It is interesting however, that those who observed themselves gaining weight during the first six months of the study did not increase the frequency of their weighing in the second six-month period.
As a consequence of the females in the C group not gaining more weight and CTM females regaining some weight, the weight difference between females in C and CTM groups diminished during second six months of the trial. The total weight change of the CTM females was a minimal loss, whereas the C group females gained about 0.6 kg. Neither were statistically different from zero. The intervention goal was weight gain prevention, not weight loss. A larger sample size would be needed to show a significant effect of the intervention among females if the C group gains at the rate observed here, possibly influenced by the study participation and measurements as discussed above.
Women are, from a young age, bombarded with stimuli to counter the environmental food stimuli; such as dieting ads, dieting books, and watching their weight. (40). Conversely, young men are less likely to have weight loss ambitions, but rather display weight gain ambitions (34), are less concerned about weight, and use fewer strategies to control weight gain compared to females (41). Therefore the motivational information about preventing weight gain, together with the continuous reinforcement of the self-weighing and feedback, may have caused and supported males to rethink and change their ambitions and behavior and thus produced a more powerful difference between controls and CTM-users compared to the females.
We found no evidence of adverse effects of frequent self-weighing and graphical feedback. This is consistent with recent experimental findings indicating that frequent self-weighing leads to weight control and improvements in several psychological measures. Caution was warranted as correlational observations (31,42–44), and one 2 week experimental study (45), have indicated an association between self-weighing and adverse psychological effects. However, several other studies have examined the relationship between the frequency of weighing and body dissatisfaction found no such a relationship, or only among those overweight (46,47). Experimentally increasing the frequency self-weighing has been shown to cause a decrease in depression, (48,49), as well as an improvement in mood and body-image (50).
This trial had some limitations. First, the results are not generalizable to all young adults. The study population consisted of students attending university. Although weight gain may not differ between students and non-students, the acceptance and efficacy of the CTM outside the university remains to be tested. Second, the weight measurements among controls may have caused weight control behaviors among females gaining weight, introducing a bias that reduced the difference between CTM and C groups. Third, the study was not powered to fully evaluate gender differences. The strengths of this study include its randomized controlled design, which allows for causal inference; its long intervention period with high retention, which helped us to detect a meaningful effect of the CTM intervention; and the lack of adverse effects.
In conclusion, the internet based frequent self-weighing CTM system proved to be effective in preventing age-related weight gain in young adults over period of one year and thus provide a strategy for weight control at a time in life when marked weight gain otherwise occurs. Future trials may aim to include a more diverse population, further explore gender differences, identify predictors and correlates of successful weight control using the CTM, and examine the effectiveness of the CTM to prevent weight gain over a longer period of time.
Acknowledgments
Funding
Kenneth Horowitz, Alumni donation
Swedish Council for Working Life and Social Research (Post Doctoral grant: 2012-1951)
Footnotes
The suggested techniques included reduced portion sizes, reduced fat content, eat only when hungry, be vigilante that eating can be influenced by eating of others and that watching food ads on TV may influence one to eat.
Conflict of interest declaration:
None of the authors had a personal or financial conflict of interest.
Trial registration number:
References
- 1.Hill JO, Wyatt HR, Reed GW, Peters JC. Obesity and the environment: where do we go from here? Science. 2003 Feb 7;299(5608):853–855. doi: 10.1126/science.1079857. [DOI] [PubMed] [Google Scholar]
- 2.Levitsky DA, Pacanowski CR. Free will and the obesity epidemic. Public Health Nutr. 2012 Jan;15(1):126–141. doi: 10.1017/S1368980011002187. [DOI] [PubMed] [Google Scholar]
- 3.Adams KF, Leitzmann MF, Ballard-Barbash R, Albanes D, Harris TB, Hollenbeck A, et al. Body mass and weight change in adults in relation to mortality risk. Am J Epidemiol. 2014 Jan 15;179(2):135–144. doi: 10.1093/aje/kwt254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Mutsert R, Sun Q, Willett WC, Hu FB, van Dam RM. Overweight in early adulthood, adult weight change, and risk of type 2 diabetes, cardiovascular diseases, and certain cancers in men: a cohort study. Am J Epidemiol. 2014 Jun 1;179(11):1353–1365. doi: 10.1093/aje/kwu052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anderson JW, Konz EC, Frederich RC, Wood CL. Long-term weight-loss maintenance: a meta-analysis of US studies. Am J Clin Nutr. 2001 Nov;74(5):579–584. doi: 10.1093/ajcn/74.5.579. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC) BRFSS 2011 Survey Data and Documentation. 2012 Available at: http://www.cdc.gov/brfss/annual_data/annual_2011.htm#datafiles, 2012.
- 7.Beaufrere B, Morio B. Fat and protein redistribution with aging: metabolic considerations. Eur J Clin Nutr. 2000 Jun;54(Suppl 3):S48–53. doi: 10.1038/sj.ejcn.1601025. [DOI] [PubMed] [Google Scholar]
- 8.Zamboni M, Armellini F, Harris T, Turcato E, Micciolo R, Bergamo-Andreis IA, et al. Effects of age on body fat distribution and cardiovascular risk factors in women. Am J Clin Nutr. 1997 Jul;66(1):111–115. doi: 10.1093/ajcn/66.1.111. [DOI] [PubMed] [Google Scholar]
- 9.Swinburn B, Sacks G, Ravussin E. Increased food energy supply is more than sufficient to explain the US epidemic of obesity. Am J Clin Nutr. 2009 Dec;90(6):1453–1456. doi: 10.3945/ajcn.2009.28595. [DOI] [PubMed] [Google Scholar]
- 10.Swinburn BA, Sacks G, Lo SK, Westerterp KR, Rush EC, Rosenbaum M, et al. Estimating the changes in energy flux that characterize the rise in obesity prevalence. Am J Clin Nutr. 2009 Jun;89(6):1723–1728. doi: 10.3945/ajcn.2008.27061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arnett JJ. Emerging adulthood. A theory of development from the late teens through the twenties. Am Psychol. 2000 May;55(5):469–480. [PubMed] [Google Scholar]
- 12.Anderson DA, Shapiro JR, Lundgren JD. The freshman year of college as a critical period for weight gain: an initial evaluation. Eat Behav. 2003 Nov;4(4):363–367. doi: 10.1016/S1471-0153(03)00030-8. [DOI] [PubMed] [Google Scholar]
- 13.Levitsky DA, Halbmaier CA, Mrdjenovic G. The freshman weight gain: a model for the study of the epidemic of obesity. Int J Obes Relat Metab Disord. 2004 Nov;28(11):1435–1442. doi: 10.1038/sj.ijo.0802776. [DOI] [PubMed] [Google Scholar]
- 14.Lloyd-Richardson EE, Bailey S, Fava JL, Wing R, Tobacco Etiology Research Network (TERN) A prospective study of weight gain during the college freshman and sophomore years. Prev Med. 2009 Mar;48(3):256–261. doi: 10.1016/j.ypmed.2008.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Racette SB, Deusinger SS, Strube MJ, Highstein GR, Deusinger RH. Changes in weight and health behaviors from freshman through senior year of college. J Nutr Educ Behav. 2008 Jan-Feb;40(1):39–42. doi: 10.1016/j.jneb.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 16.Vella-Zarb RA, Elgar FJ. The ‘freshman 5’: a meta-analysis of weight gain in the freshman year of college. J Am Coll Health. 2009 Sep-Oct;58(2):161–166. doi: 10.1080/07448480903221392. [DOI] [PubMed] [Google Scholar]
- 17.Gropper SS, Simmons KP, Connell LJ, Ulrich PV. Changes in body weight, composition, and shape: a 4-year study of college students. Appl Physiol Nutr Metab. 2012 Dec;37(6):1118–1123. doi: 10.1139/h2012-139. [DOI] [PubMed] [Google Scholar]
- 18.Nelson MC, Story M, Larson NI, Neumark-Sztainer D, Lytle LA. Emerging adulthood and college-aged youth: an overlooked age for weight-related behavior change. Obesity (Silver Spring) 2008 Oct;16(10):2205–2211. doi: 10.1038/oby.2008.365. [DOI] [PubMed] [Google Scholar]
- 19.U.S. Department of Health and Human Services. HealthyPeople.gov Normal weight status. Available at: www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicid=29. Accessed 05/29, 2014.
- 20.Hutfless S, Gudzune KA, Maruthur N, Wilson RF, Bleich SN, Lau BD, et al. Strategies to prevent weight gain in adults: a systematic review. Am J Prev Med. 2013 Dec;45(6):e41–51. doi: 10.1016/j.amepre.2013.07.013. [DOI] [PubMed] [Google Scholar]
- 21.Gudzune K, Hutfless S, Maruthur N, Wilson R, Segal J. Strategies to prevent weight gain in workplace and college settings: a systematic review. Prev Med. 2013 Oct;57(4):268–277. doi: 10.1016/j.ypmed.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 22.Vanwormer JJ, French SA, Pereira MA, Welsh EM. The impact of regular self-weighing on weight management: a systematic literature review. Int J Behav Nutr Phys Act. 2008 Nov 4;5 doi: 10.1186/1479-5868-5-54. 54-5868-5-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Levitsky DA, Garay J, Nausbaum M, Neighbors L, Dellavalle DM. Monitoring weight daily blocks the freshman weight gain: a model for combating the epidemic of obesity. Int J Obes (Lond) 2006 Jun;30(6):1003–1010. doi: 10.1038/sj.ijo.0803221. [DOI] [PubMed] [Google Scholar]
- 24.Gow RW, Trace SE, Mazzeo SE. Preventing weight gain in first year college students: an online intervention to prevent the “freshman fifteen”. Eat Behav. 2010 Jan;11(1):33–39. doi: 10.1016/j.eatbeh.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Strimas RDM. Differential effects of self-weighing in restrained and unrestrained eaters. Personality and Individual Differences. 2010;49:1011–1014. [Google Scholar]
- 26.Chernyak Y, Lowe MR. Motivations for dieting: Drive for Thinness is different from Drive for Objective Thinness. J Abnorm Psychol. 2010 May;119(2):276–281. doi: 10.1037/a0018398. [DOI] [PubMed] [Google Scholar]
- 27.Malhotra R, Ostbye T, Riley CM, Finkelstein EA. Young adult weight trajectories through midlife by body mass category. Obesity (Silver Spring) 2013 Sep;21(9):1923–1934. doi: 10.1002/oby.20318. [DOI] [PubMed] [Google Scholar]
- 28.Pacanowski CR, Bertz F, Levitsky DA. Daily self-weighing to control body weight in adults: A critical review of the literature. Sage Open. 2014 doi: 10.1177/2158244014556992. Accepted Sep 25, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hivert MF, Langlois MF, Berard P, Cuerrier JP, Carpentier AC. Prevention of weight gain in young adults through a seminar-based intervention program. Int J Obes (Lond) 2007 Aug;31(8):1262–1269. doi: 10.1038/sj.ijo.0803572. [DOI] [PubMed] [Google Scholar]
- 30.Matvienko O, Lewis DS, Schafer E. A college nutrition science course as an intervention to prevent weight gain in female college freshmen. J Nutr Educ. 2001 Mar-Apr;33(2):95–101. doi: 10.1016/s1499-4046(06)60172-3. [DOI] [PubMed] [Google Scholar]
- 31.Quick V, Larson N, Eisenberg ME, Hannan PJ, Neumark-Sztainer D. Self-weighing behaviors in young adults: tipping the scale toward unhealthy eating behaviors? J Adolesc Health. 2012 Nov;51(5):468–474. doi: 10.1016/j.jadohealth.2012.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Provencher V, Polivy J, Wintre MG, Pratt MW, Pancer SM, Birnie-Lefcovitch S, et al. Who gains or who loses weight? Psychosocial factors among first-year university students. Physiol Behav. 2009 Jan 8;96(1):135–141. doi: 10.1016/j.physbeh.2008.09.011. [DOI] [PubMed] [Google Scholar]
- 33.Girz L, Polivy J, Provencher V, Wintre MG, Pratt MW, Mark Pancer S, et al. The four undergraduate years. Changes in weight, eating attitudes, and depression. Appetite. 2013 Oct;69:145–150. doi: 10.1016/j.appet.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 34.Grossbard JR, Neighbors C, Larimer ME. Perceived norms for thinness and muscularity among college students: what do men and women really want? Eat Behav. 2011 Aug;12(3):192–199. doi: 10.1016/j.eatbeh.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Waters L, George AS, Chey T, Bauman A. Weight change in control group participants in behavioural weight loss interventions: a systematic review and meta-regression study. BMC Med Res Methodol. 2012 Aug 8;12 doi: 10.1186/1471-2288-12-120. 120-2288-12-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Harvey-Berino J, Pintauro S, Buzzell P, DiGiulio M, Casey Gold B, Moldovan C, et al. Does using the Internet facilitate the maintenance of weight loss? Int J Obes Relat Metab Disord. 2002;26(9):1254–1260. doi: 10.1038/sj.ijo.0802051. [DOI] [PubMed] [Google Scholar]
- 37.Tate DF, Wing RR, Winett RA. Using Internet technology to deliver a behavioral weight loss program. JAMA. 2001;285(9):1172–1177. doi: 10.1001/jama.285.9.1172. [DOI] [PubMed] [Google Scholar]
- 38.Tate DF, Jackvony EH, Wing RR. Effects of Internet behavioral counseling on weight loss in adults at risk for type 2 diabetes: a randomized trial. JAMA. 2003;289(14):1833–1836. doi: 10.1001/jama.289.14.1833. [DOI] [PubMed] [Google Scholar]
- 39.Tate DF, Jackvony EH, Wing RR. A randomized trial comparing human e-mail counseling, computer-automated tailored counseling, and no counseling in an Internet weight loss program. Arch Intern Med. 2006;166(15):1620–1625. doi: 10.1001/archinte.166.15.1620. [DOI] [PubMed] [Google Scholar]
- 40.Pacanowski CR. PhD thesis. Cornell University; 2013. Effects of self-weighing and visual feedback on weight control in adults; p. 1. [Google Scholar]
- 41.Cluskey M, Grobe D. College weight gain and behavior transitions: male and female differences. J Am Diet Assoc. 2009 Feb;109(2):325–329. doi: 10.1016/j.jada.2008.10.045. [DOI] [PubMed] [Google Scholar]
- 42.Quick V, Loth K, MacLehose R, Linde JA, Neumark-Sztainer D. Prevalence of adolescents’ self-weighing behaviors and associations with weight-related behaviors and psychological well-being. J Adolesc Health. 2013 Jun;52(6):738–744. doi: 10.1016/j.jadohealth.2012.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR®. American Psychiatric Pub; 2000. [Google Scholar]
- 44.Mercurio A, Rima B. Watching my weight: Self-weighing, body surveillance, and body dissatisfaction. Sex Roles. 2011;65:47–55. [Google Scholar]
- 45.Ogden J, Whyman C. The effect of repeated weighing on psychological state. Eur Eating Dis Rev. 1997;5:121–130. [Google Scholar]
- 46.Ogden J, Evans C. The problem with weighing: effects on mood, self-esteem and body image. Int J Obes Relat Metab Disord. 1996 Mar;20(3):272–277. [PubMed] [Google Scholar]
- 47.Welsh EM, Sherwood NE, VanWormer JJ, Hotop AM, Jeffery RW. Is frequent self-weighing associated with poorer body satisfaction? Findings from a phone-based weight loss trial. J Nutr Educ Behav. 2009 Nov-Dec;41(6):425–428. doi: 10.1016/j.jneb.2009.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gokee LaRose J, Tate DF, Gorin AA, Wing RR. Preventing weight gain in young adults: a randomized controlled pilot study. Am J Prev Med. 2010 Jul;39(1):63–68. doi: 10.1016/j.amepre.2010.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wing RR, Tate DF, Gorin AA, Raynor HA, Fava JL, Machan J. STOP regain: are there negative effects of daily weighing? J Consult Clin Psychol. 2007 Aug;75(4):652–656. doi: 10.1037/0022-006X.75.4.652. [DOI] [PubMed] [Google Scholar]
- 50.Steinberg DM, Tate DF, Bennett GG, Ennett S, Samuel-Hodge C, Ward DS. Daily self-weighing and adverse psychological outcomes: a randomized controlled trial. Am J Prev Med. 2014 Jan;46(1):24–29. doi: 10.1016/j.amepre.2013.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]


