Abstract
There are over 100 clinical trials worldwide focused on developing an HIV cure. Research participants will assume substantial individual risks while receiving little or no individual benefit. Physicians will have important dual roles of leading HIV cure research studies and guiding patient expectations. Many low and middle-income nations have started HIV cure trials, including China. The goal of this study was to better understand physician attitudes, behaviors, and perceptions of HIV cure research within the context of China. We conducted a quantitative and qualitative evidence review of published literature on physician perceptions of HIV cure in China. Quantitative survey data revealed that physicians rarely believed HIV was curable, but this perception may be more common compared to other countries. Qualitative data showed that inconsistent terminology used among physicians may contribute to the perception of HIV as curable. The belief that HIV is curable among some physicians in China may be related to the influence of traditional Chinese medicine beliefs. Rather than seeking elimination of pathogens, traditional Chinese medicine aims to achieve harmony between organs and a vital life force. In this context, HIV infection can be seen as a temporary state of imbalance rather than an irreversible change. There is a wide range of physician perceptions about HIV cure in China. Conflicting information about HIV cure from physicians and other sources could thwart the progress of HIV cure research. Enhancing patient-physician communication about ongoing HIV cure research trials will be important for developing an HIV cure.
Keywords: HIV, Physician, Cure, China, Review
1. Introduction
Over the past three decades, HIV infection has changed from a death sentence to a manageable condition. Timothy Ray Brown’s possibly curative long-term remission[1] alongside other clinical HIV cure researches may slowly transit HIV from incurable to curable. As with other paradigm shifts, cure research will bring unintended consequences[2]. For example, early success in HIV cure research may change expectations for current HIV cure efforts[3]. Just as alternative and counterfeit HIV medications proliferated following the adoption of antiretroviral drugs[4,5], unproven curative treatments may similarly be spreading[6–8]. Already, prominent physicians in Iran[3] and Egypt[9] have promoted HIV cures that were ultimately ineffective, confusing patients and jeopardizing their antiretroviral drug compliance[6]. As HIV cure research continues, physicians are positioned to guide patients through the uncertainties and risks. Vital to the success of cure research, physicians will lead research studies focused on how to discuss HIV cure among other physicians and with patients[10,11]. Physicians’ perceptions of HIV cure may influence both the success and consequences of HIV cure research.
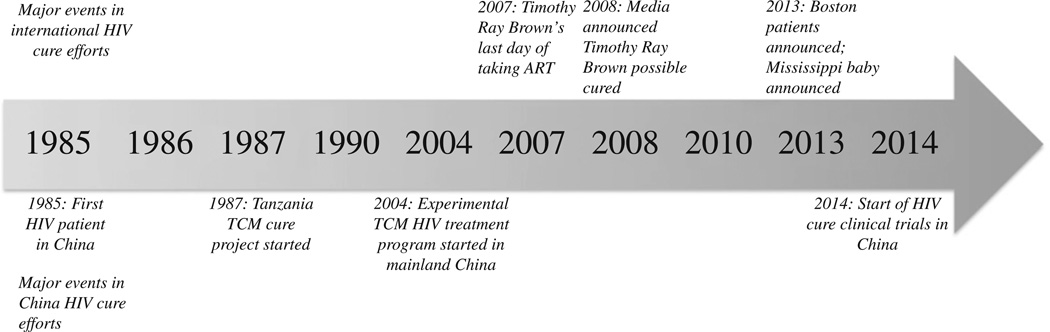
In China, physician perceptions of HIV cure are particularly important. First, China is expanding clinical HIV cure research[12] and is currently recruiting patients for a phase III study aimed at achieving virological remission[13]. Second, traditional Chinese medicine (TCM) treatments are believed by both providers and patients as being able to cure HIV early on in the epidemic[14–19]. TCM is commonly used in China[20] and has been a part of China’s cure effort (Figure 1). Third, HIV cure research has been identified as a priority according to both the National Institute of Health and the National Natural Science Foundation of China[21]. We conducted a mixed methods review to investigate physician perceptions of HIV cure and how these perceptions may influence HIV cure research. While there is some social science literature on HIV cure research in high-income settings[2,10,11,22] similar research is needed in low and middle-income settings.
Figure 1.
Timeline of major HIV cure events internationally and within China.
2. Quantitative research
We found five research articles that provided quantitative estimates of physician perceptions of HIV cure[23–27]. Physician belief in HIV cure ranged from 1.4%–75.0% (Table 1). While the percentages in Table 1 vary widely and are difficult to compare, overall they appear consistent with other low and middle-income countries such as Rwanda (16%) and Egypt (8.2%)[28,29]. Physicians in the two studies done after 2009 may be influenced by Timothy Ray Brown[1], the Mississippi Child[30], or other early cure research[31]. In the US among a sample of 132 physicians a reported 2% of doctors were judged as being without basic knowledge of HIV, a definition that included whether HIV is curable[32]. The limited literature on physician perceptions of HIV cure suggests the need for more researches.
Table 1.
Five research studies examining physician belief in HIV cure (1999–2010) in several Chinese provinces.
| Study | Date collected | Province | Sample size | Question wording | Answer | Percentagea (%) |
|---|---|---|---|---|---|---|
| Jiang et al. 2006[26] | 2006 | Shandong | 1 310 | Is there a medicine or vaccine to cure AIDS? | Yes | 4.0 |
| Qu & Wu 2014[24] | Not reported | Liaoning | 285 | AIDS is incurable now | False | 15.0 |
| Chen et al. 2002[27] | Not reported | Hainan | 33 | Is AIDS curable now? | Yes | 75.0 |
| Li et al. 2000 [25] | 1999 | Multiple citiesb | 870 | HAART can cure HIV | Yes | 1.4 |
| Xiu 2013[23] | 2010 | Shandong | 153 | HARRT cannot cure AIDS | False | 4.5 |
: All percentages reflect belief that curing HIV is possible;
: Sample was a convenience sample of physicians in multiple cities; HAART: Highly active anti-retroviral therapy.
3. Qualitative research
We identified two qualitative research studies on physician perceptions of HIV cure[14,33]. The belief HIV is curable among health professionals in China may be related to philosophies and teachings of TCM. As one TCM practitioner explained early on in the AIDS epidemic (1990):
“Somebody asked me can you make a cure for AIDS? I can say yes, I can say no. No, because [we] never experienced [this] in China; yes, because traditional Chinese medicine helps the patient’s body get strong; the immune system rises. That means you can cure any disease. I don’t care about disease name.”[14].
Rather than seeking elimination of pathogens, TCM aims to achieve harmony between the bodies organs and vital life force[20]. HIV infection can be seen more as a temporary state of imbalance rather than an irreversible change. As described by one patient while describing his reasons for choosing a TCM practitioner:
“I believe in Chinese medicines more. The human body is not just a unit but also a correlated and balanced system. Therefore, I definitely would keep using traditional Chinese medicines to adjust my own balance. From the perspective of Qi, or for my own body’s good, I need to increase my body’s strengths. Everyone has viruses in his or her body, either this one or that one. When your immune system is strong, those viruses become weak, with no doubt. When your positive forces are enhanced, the negative forces must be weakened. So I will boost my own positive forces through Chinese medicine.”[34].
Similar to English[11], accurate terminology is necessary to ensure clarity in Chinese. The mandarin words “zhi yu” (treat heal) and “zhi hao” (treat good) can both be used to mean cure[33]. Although the term “zhi yu” is exclusively used with the physicians in the studies listed in Table 1, “zhi hao” is used by physicians[33] when discussing HIV cure with patients. More researches are needed into how physicians explain HIV cure to patients.
4. Discussion
Quantitative data suggest that belief of HIV as curable is not particularly common among Chinese physicians but maybe higher than that in low-income countries. Understanding physicians’ knowledge of HIV cure will be important for improving patients’ health. In Tanzania for example where physicians have relatively little knowledge of HIV cure[35,36], rumors about curing HIV have led to decreased medication adherence[6,36]. Encouragingly however, short intensive educational lectures on HIV have been effective in decreasing the percent of physicians that believe in a cure[37]. More researches are needed to more accurately gauge Chinese physicians’ knowledge of HIV, especially studies that can accurately account for recent developments in HIV cure research.
With ongoing HIV cure research, however, it will no longer be sufficient for physicians to merely say that HIV is incurable. News coverage of biomedical HIV cure efforts may have the unintended consequence of normalizing unproven HIV cures. Before reports of Timothy Ray Brown, physicians could simply tell patients HIV is incurable and any treatments marketed as otherwise are fraudulent. Conflicting information about HIV cure from physicians and the media should be investigated as a potential health risk. After learning about biomedical HIV cure efforts, patients may be more willing to pursue treatments advertised as being able to cure HIV. More researches are needed into how physicians should talk with patients about HIV cure and dissuade patients from using unproven therapies.
Qualitative research revealed that Chinese physicians have multiple words when referencing HIV cure. The term “zhi yu” appears to be used among physicians and resembles a sterilizing cure. Alternatively, “zhi hao” is more familiar to patients and implies a temporary, symptoms based treatment possible analogous to remission. For self resolving illnesses such as the common cold it is easy to see how these terms could be interchangeable: a medication that left you symptom free until your body cleared the illness could seem synonymous with a cure. For chronic infections such as HIV the distinction between symptomatic and curative treatments becomes more pronounced. Medications that reduce HIV-infected individual’s symptoms could be described as “zhi hao” and mistakenly interpreted as a lasting cure. The differences between these two terms may have roots in the differences between biomedical and TCM based theories of HIV. Attributing HIV to a correctable imbalance rather than a concrete infection is consistent with the notion of HIV as curable and could contribute to the perception that HIV is curable.
This study has several limitations. Due to the novelty of the subject matter, relatively few relevant studies were found. Additionally this review does not specify the type of doctor included in each study. This is important for the implication these perceptions could have for patient care and future research. In China, the vast majority of HIV patients are treated by infectious disease specialists rather than primary care doctors. The perceptions discussed in this study may not be representative of doctors that have clinical interactions with HIV patients or are involved in cure research.
Future efforts should be take to use clear terminology and minimize misunderstandings between patients, biomedical, and TCM physicians. This is especially important with the growing role TCM has in HIV cure research. Over 20 000 known TCM substances have been catalogued for biomedical research, many of which have been shown to interact with HIV[38,39]. In particular, ingenols isolated from a TCM herb have shown promise in activating latent HIV reservoirs[40], an often cited barrier in cure research[39,41,42]. Although HIV cure may be many years away from entering mainstream clinical medicine, healthcare professionals should be prepared to guide patients through this exciting transition.
Acknowledgments
This research was supported by the National Institute of Health NIAID (1R01A108366-01) and by the Doris Duke Charitable Foundation through a grant supporting the Doris Duke International Clinical Research Fellows Program at The University of North Carolina at Chapel Hill. Zachary Clarke Rich is a Doris Duke International Clinical Research Fellow.
Footnotes
Conflict of interest statement
We declare that we have no conflict of interest.
References
- 1.Hütter G, Nowak D, Mossner M, Ganepola S, Müssig A, Allers K, et al. Long-term control of HIV by CCR5 Delta32/Delta32 stem-cell transplantation. N Engl J Med. 2009;360(7):692–698. doi: 10.1056/NEJMoa0802905. [DOI] [PubMed] [Google Scholar]
- 2.Tucker JD, Rennie S Social and Ethical Working Group on HIV Cure. Social and ethical implications of HIV cure research. AIDS. 2014;28(9):1247–1250. doi: 10.1097/QAD.0000000000000210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Amon JJ. Dangerous medicines: unproven AIDS cures and counterfeit antiretroviral drugs. Global Health. 2008;4:5. doi: 10.1186/1744-8603-4-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kelesidis T, Kelesidis I, Rafailidis PI, Falagas ME. Counterfeit or substandard antimicrobial drugs: a review of the scientific evidence. 2007;60(2):214–236. doi: 10.1093/jac/dkm109. [DOI] [PubMed] [Google Scholar]
- 5.Furin JJ. “You have to be your own doctor”: sociocultural influences on alternative therapy use among gay men with AIDS in west Hollywood. Med Anthropol Q. 1997;11(4):498–504. doi: 10.1525/maq.1997.11.4.498. [DOI] [PubMed] [Google Scholar]
- 6.Thielman NM, Ostermann J, Whetten K, Whetten R, Itemba D, Maro V, et al. Reduced adherence to antiretroviral therapy among HIV-infected Tanzanians seeking cure from the Loliondo healer. J Acquir Defic Syndr. 2014;65(3):e104–e109. doi: 10.1097/01.qai.0000437619.23031.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roura M, Nsigaye R, Nhandi B, Wamoyi J, Busza J, Urassa M, et al. “Driving the devil away”: qualitative insights into miraculous cures for AIDS in a rural Tanzanian ward. BMC Public Health. 2010;10:427. doi: 10.1186/1471-2458-10-427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peltzer K, Preez NF, Ramlagan S, Fomundam H, Anderson J, Chanetsa L. Antiretrovirals and the use of traditional, complementary and alternative medicine by HIV patients in Kwazulu-Natal, South Africa: a longitudinal study. Afr J Tradit Complement Altern Med. 2011;8(4):337–345. doi: 10.4314/ajtcam.v8i4.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hussein I, Bohannon J. Interview. A challenge to pseudoscience. Science. 2014;345(6192):16. doi: 10.1126/science.345.6192.16. [DOI] [PubMed] [Google Scholar]
- 10.Henderson GE. The ethics of HIV “cure” research: what can we learn from consent forms? AIDS Res Hum Retroviruses. 2015;31(1):56–63. doi: 10.1089/aid.2014.0219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tucker JD, Volberding PA, Margolis DM, Rennie S, Barré-Sinoussi F. Words matter: discussing research towards an HIV cure in research and clinical contexts. J Acquir Immune Defic Syndr. 2014;67(3):e110–e111. doi: 10.1097/QAI.0000000000000305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sun Y. HIV treatment: a new strategy for functional cure; 2014 National AIDS Conference; 2014 Oct 20; Beijing, China. [Google Scholar]
- 13.Sun Y. Bethesda: U.S. National Library of Medicine; 2014. [Accessed on 5th May, 2015]. Early cART and cART in combination with autologous HIV-1 specific cytotoxic T lymphocyte (CTL) infusion in the treatment of acute HIV-1 infected adults. [Online] Available from: https://clinicaltrials.gov/ct2/show/NCT02231281. [Google Scholar]
- 14.Hare ML. The emergence of an urban U.S. Chinese medicine. Med Anthropol Q. 1993;7(1):30–49. [Google Scholar]
- 15.Anderson W, O’Connor BB, MacGregor RR, Schwartz JS. Patient use and assessment of conventional and alternative therapies for HIV infection and AIDS. AIDS. 7(4):561–565. doi: 10.1097/00002030-199304000-00016. [DOI] [PubMed] [Google Scholar]
- 16.Erwin J, Peters B. Treatment issues for HIV+ Africans in London. Soc Sci Med. 49(11):1519–1528. doi: 10.1016/s0277-9536(99)00220-8. [DOI] [PubMed] [Google Scholar]
- 17.Duggan J, Peterson WS, Schutz M, Khuder S, Charkraborty J. Use of complementary and alternative therapies in HIV-infected patients. AIDS Patient Care STDs. 15(3):159–167. doi: 10.1089/108729101750123661. [DOI] [PubMed] [Google Scholar]
- 18.Standish LJ, Greene KB, Bain S, Reeves C, Sanders F, Wines RC, et al. Alternative medicine use in HIV-positive men and women: demographics, utilization patterns and health status. AIDS Care. 2001;13(2):197–208. doi: 10.1080/095401201300059759. [DOI] [PubMed] [Google Scholar]
- 19.Foote-Ardah CE. The meaning of complementary and alternative medicine practices among people with HIV in the United States: strategies for managing everyday life. Sociol Health Illn. 2003;25(5):481–500. doi: 10.1111/1467-9566.00355. [DOI] [PubMed] [Google Scholar]
- 20.Xu J, Yang Y. Traditional Chinese medicine in the Chinese health care system. Health Policy. 2009;90(2–3):133–139. doi: 10.1016/j.healthpol.2008.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Institute of Allergy and Infectious Diseases. Bethesda: National Institute of Allergy and Infectious Diseases; 2014. [Accessed on 25th March, 2015]. NIAID funding news-August 20, 2014. [Online] Available from: http://www.niaid.nih.gov/researchfunding/newsletter/2014/Pages/0820.aspx. [Google Scholar]
- 22.Johnston RE, Heitzeg MM. Sex, age, race and intervention type in clinical studies of HIV cure: a systematic review. AIDS Res Hum Retroviruses. 2015;31(1):85–97. doi: 10.1089/aid.2014.0205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xiu C. Survey on AIDS-related knowledge, attitude and the status of occupational exposure among 153 village doctors, Chengyang District, Qingdao City, 2010. Prev Med Tribune. 2013;(2) [Google Scholar]
- 24.Qu B, Wu Y. Health education of AIDS/HIV-related knowledge, attitude and behavior among rural doctors in Donggang City. J Prev Med Inf. 2014;30(4):251–253. Chinese. [Google Scholar]
- 25.Li JY, Bao ZY, Ma CG, Fan JL. Investigation on HIV/AIDS knowledge of military medical personnel. Chin J AIDS STD. 2000;6(2):92–93. Chinese. [Google Scholar]
- 26.Jiang XK, Zhou CG, Yu HR, Liang W, Liu SX, Zhang L. Investigation on HIV/AIDS knowledge and risk of occupational exposure of medical personnel in Liaocheng. Chin Prev Med. 2006;7(3):194–197. Chinese. [Google Scholar]
- 27.Chen Y, Du JW, Xing W, Lin MH, Pan WL, Fu Y. Analysis of effectiveness on health education of AIDS and STD to village doctors in the Li minority village in Hainan Province. Re Dai Yi Xue Za Zhi. 2002;2(2):200–201. [Google Scholar]
- 28.Rahlenbeck SI. Knowledge, attitude, and practice about AIDS and condom utilization among health workers in Rwanda. J Assoc Nurses AIDS Care. 2004;15(3):56–61. doi: 10.1177/1055329003252057. [DOI] [PubMed] [Google Scholar]
- 29.Sallam SA, Mahfouz AA, Alakija W, al-Erian RA. Continuing medical education needs regarding AIDS among Egyptian physicians in Alexandria, Egypt and in the Asir Region, Saudi Arabia. AIDS Care. 1995;7(1):49–54. doi: 10.1080/09540129550126957. [DOI] [PubMed] [Google Scholar]
- 30.Persaud D, Gay H, Ziemniak C, Chen YH, Piatak M, Jr, Chun TW, et al. Absence of detectable HIV-1 viremia after treatment cessation in an infant. N Engl J Med. 2013;369(19):1828–1835. doi: 10.1056/NEJMoa1302976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Henrich TJ, Hu Z, Li JZ, Sciaranghella G, Busch MP, Keating SM, et al. Long-term reduction in peripheral blood HIV type 1 reservoirs following reduced-intensity conditioning allogeneic stem cell transplantation. J Infect Dis. 2013;207(11):1694–1702. doi: 10.1093/infdis/jit086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dworkin J, Albrecht G, Cooksey J. Concern about AIDS among hospital physicians, nurses and social workers. Soc Sci Med. 1991;33(3):239–248. doi: 10.1016/0277-9536(91)90357-i. [DOI] [PubMed] [Google Scholar]
- 33.Chu CE, Wu F, He X, Ma Q, Cheng Y, Cai W, et al. Exploring the social meaning of curing HIV: a qualitative study of people who inject drugs in Guangzhou, China. AIDS Res Hum Retroviruses. 2015;31(1):78–84. doi: 10.1089/aid.2014.0200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen WT, Shiu CS, Simoni J, Fredriksen-Goldsen K, Zhang F, Starks H, et al. Attitudes toward antiretroviral therapy and complementary and alternative medicine in Chinese patients infected with HIV. J Assoc Nurses AIDS Care. 2009;20(3):203–217. doi: 10.1016/j.jana.2008.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kohi TW, Horrocks MJ. The knowledge, attitudes and perceived support of Tanzanian nurses when caring for patients with AIDS. Int J Nurs Stud. 1994;31(1):77–86. doi: 10.1016/0020-7489(94)90009-4. [DOI] [PubMed] [Google Scholar]
- 36.Plummer ML, Mshana G, Wamoyi J, Shigongo ZS, Hayes RJ, Ross DA, et al. ‘The man who believed he had AIDS was cured’: AIDS and sexually-transmitted infection treatment-seeking behaviour in rural Mwanza, Tanzania. AIDS Care. 2006;18(5):460–466. doi: 10.1080/09540120500220367. [DOI] [PubMed] [Google Scholar]
- 37.Buskin SE, Li L, Yin H, Yu T, McGough JP. HIV/AIDS knowledge and attitudes in Chinese medical professionals and students before and after an informational lecture on HIV/AIDS. J Public Health Manag Pract. 2002;8(6):38–43. doi: 10.1097/00124784-200211000-00006. [DOI] [PubMed] [Google Scholar]
- 38.Chen CY. TCM Database@Taiwan: the world’s largest traditional Chinese medicine database for drug screening in silico. PloS One. 2011;6(1):e15939. doi: 10.1371/journal.pone.0015939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zou W, Liu Y, Wang J, Li H, Liao X. Traditional Chinese herbal medicines for treating HIV infections and AIDS. Evid Based Complement Alternat Med. 2012;2012:950757. doi: 10.1155/2012/950757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Abreu CM, Price SL, Shirk EN, Cunha RD, Pianowski LF, Clements JE, et al. Dual role of novel ingenol derivatives from Euphorbia tirucalli in HIV replication: inhibition of de novo infection and activation of viral LTR. PloS One. 2014;9(5):e97257. doi: 10.1371/journal.pone.0097257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Richman DD, Margolis DM, Delaney M, Greene WC, Hazuda D, Pomerantz RJ. The challenge of finding a cure for HIV infection. Science. 2009;323(5919):1304–1307. doi: 10.1126/science.1165706. [DOI] [PubMed] [Google Scholar]
- 42.Katlama C, Deeks SG, Autran B, Martinez-Picado J, van Lunzen J, Rouzioux C, et al. Barriers to a cure for HIV: new ways to target and eradicate HIV-1 reservoirs. Lancet. 2013;381(9883):2109–2117. doi: 10.1016/S0140-6736(13)60104-X. [DOI] [PMC free article] [PubMed] [Google Scholar]