Abstract
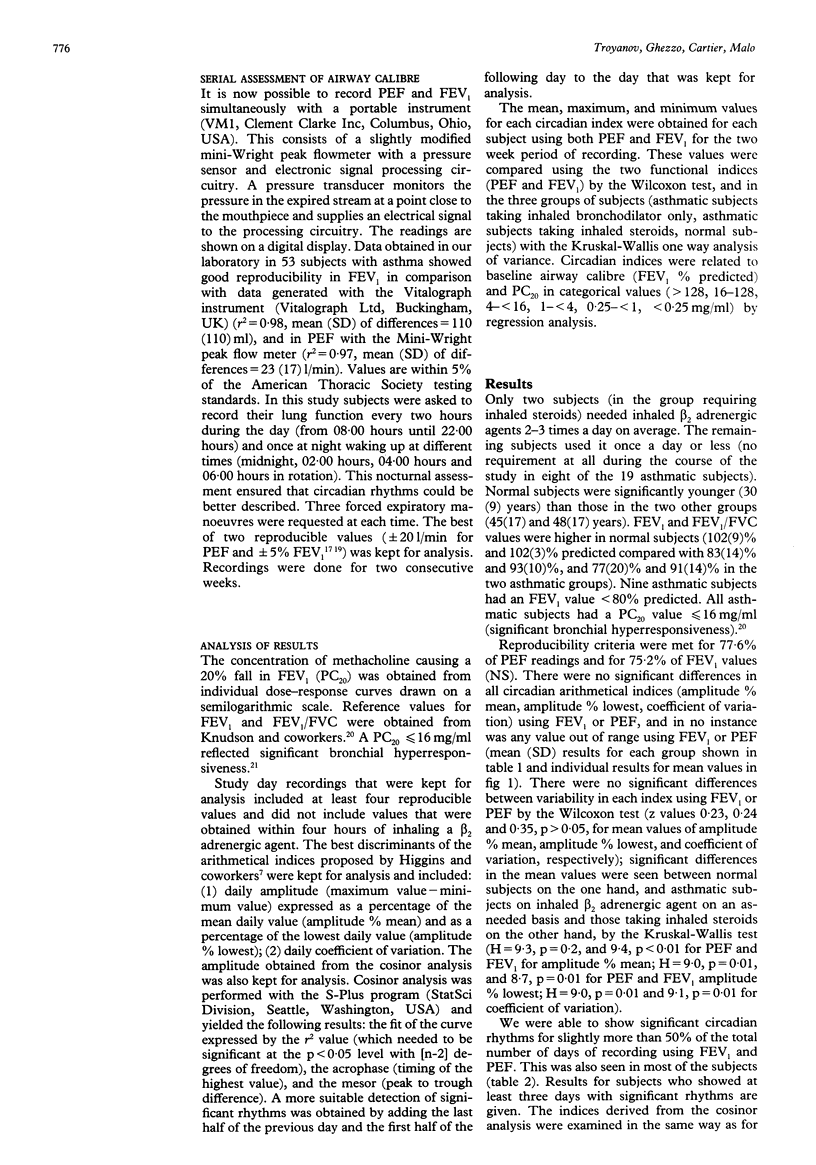
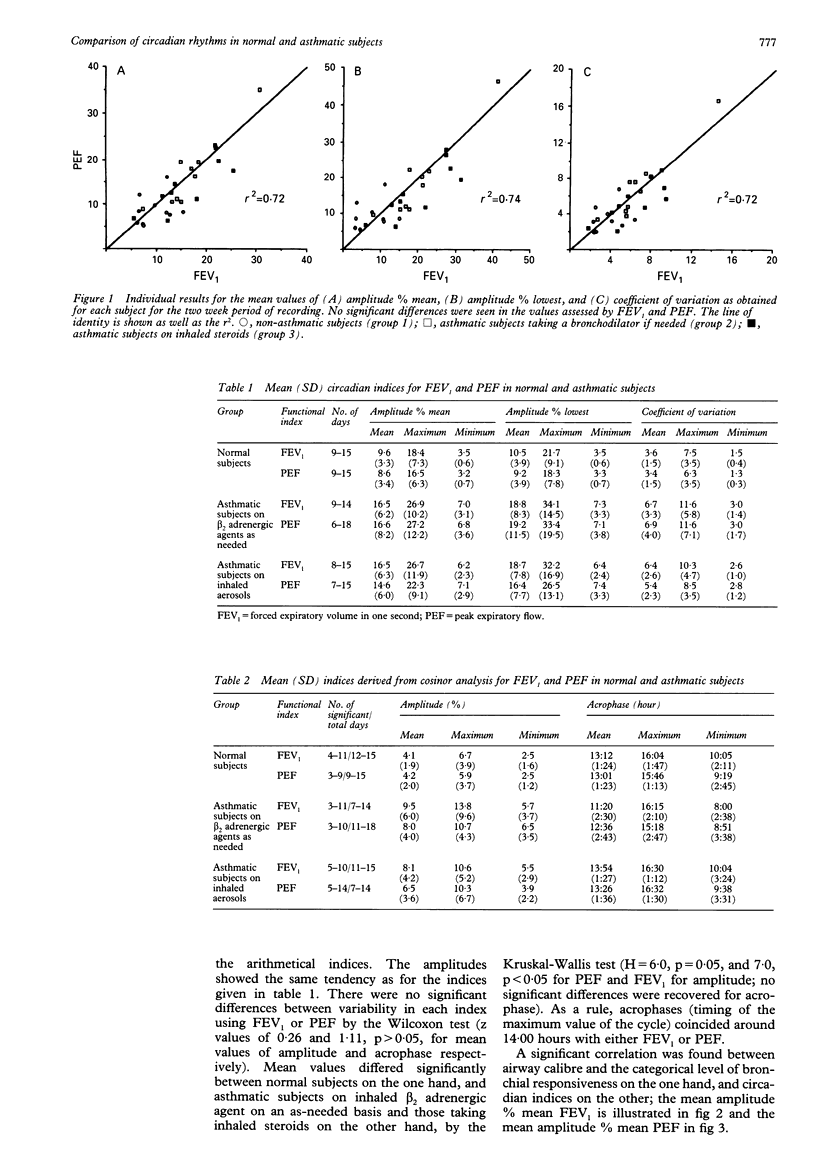
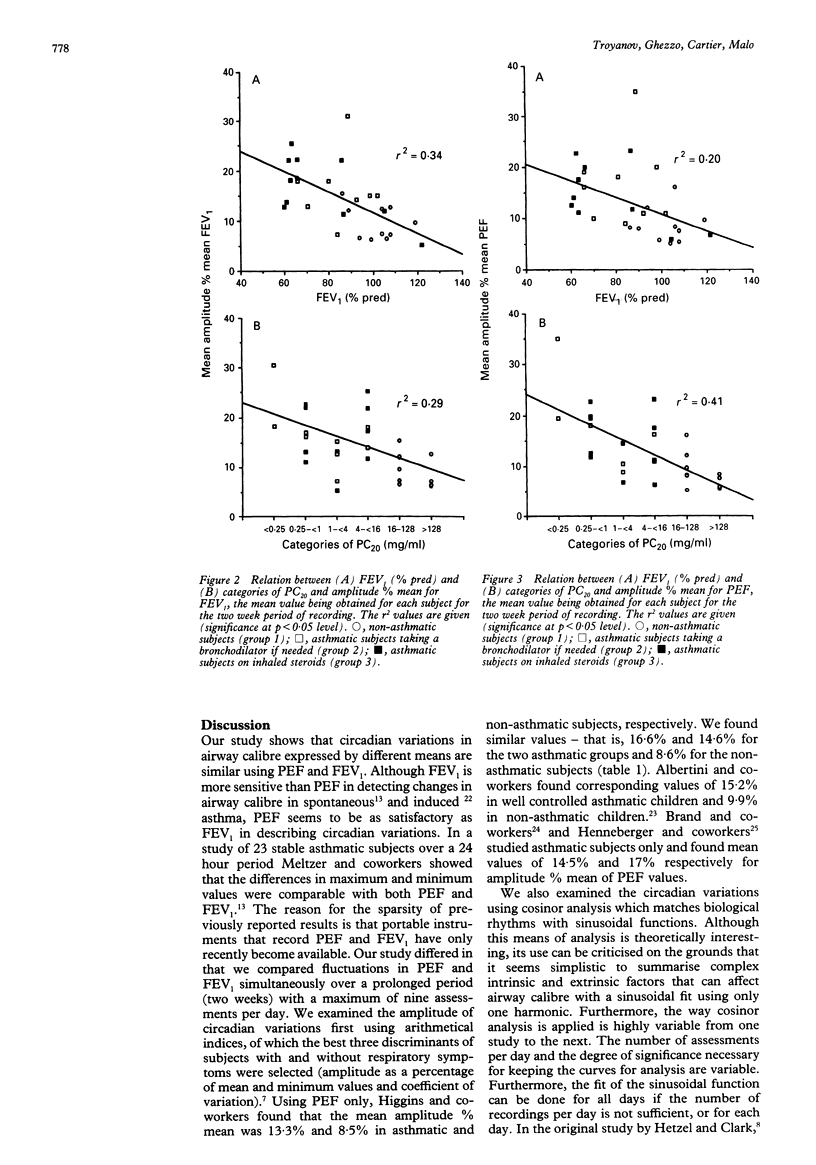
BACKGROUND--Most studies that describe circadian variations in asthma have used maximum rate of peak expiratory flow (PEF) rather than forced expiratory volume in one second (FEV1) to assess airway calibre. This study was designed to assess circadian variations in PEF and FEV1 measured simultaneously and to compare variations in these measurements in normal and asthmatic subjects in a stable clinical state. METHODS--Twenty nine subjects (nine asthmatic subjects on bronchodilators, 10 on inhaled steroids, and 10 normal controls) were asked to record their PEF and FEV1 with a new portable instrument every two hours during the day and once on waking at night for two weeks. Circadian variations were examined in different ways using arithmetical indices and cosinor analysis. RESULTS--78% of PEF values and 75% of FEV1 values were considered to be reproducible and were included in the analysis. Variations obtained using PEF did not differ from those obtained using FEV1. Significant cosinor variations were found in at least 50% of recording days for most of the subjects and showed the same features as for arithmetical indices. Daily variations in PEF and FEV1 were significantly correlated with airway calibre and PC20 methacholine (r approximately 0.5 to approximately 0.6). CONCLUSIONS--PEF is as satisfactory as FEV1 for describing circadian variations among normal subjects and stable asthmatic subjects.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Albertini M., Politano S., Berard E., Boutte P., Mariani R. Variation in peak expiratory flow of normal and asymptomatic asthmatic children. Pediatr Pulmonol. 1989;7(3):140–144. doi: 10.1002/ppul.1950070305. [DOI] [PubMed] [Google Scholar]
- Bahous J., Cartier A., Malo J. L. Monitoring of peak expiratory flow rates in subjects with mild airway hyperexcitability. Bull Eur Physiopathol Respir. 1985 Jan-Feb;21(1):25–30. [PubMed] [Google Scholar]
- Bonnet R., Jörres R., Heitmann U., Magnussen H. Circadian rhythm in airway responsiveness and airway tone in patients with mild asthma. J Appl Physiol (1985) 1991 Oct;71(4):1598–1605. doi: 10.1152/jappl.1991.71.4.1598. [DOI] [PubMed] [Google Scholar]
- Brand P. L., Postma D. S., Kerstjens H. A., Koëter G. H. Relationship of airway hyperresponsiveness to respiratory symptoms and diurnal peak flow variation in patients with obstructive lung disease. The Dutch CNSLD Study Group. Am Rev Respir Dis. 1991 May;143(5 Pt 1):916–921. doi: 10.1164/ajrccm/143.5_Pt_1.916. [DOI] [PubMed] [Google Scholar]
- Burge P. S., O'Brien I. M., Harries M. G. Peak flow rate records in the diagnosis of occupational asthma due to isocyanates. Thorax. 1979 Jun;34(3):317–323. doi: 10.1136/thx.34.3.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bérubé D., Cartier A., L'Archevêque J., Ghezzo H., Malo J. L. Comparison of peak expiratory flow rate and FEV1 in assessing bronchomotor tone after challenges with occupational sensitizers. Chest. 1991 Apr;99(4):831–836. doi: 10.1378/chest.99.4.831. [DOI] [PubMed] [Google Scholar]
- Carpentiere G., Marino S., Castello F. Effects of inhaled fenoterol on the circadian rhythm of expiratory flow in allergic bronchial asthma. Chest. 1983 Feb;83(2):211–214. doi: 10.1378/chest.83.2.211. [DOI] [PubMed] [Google Scholar]
- Cinkotai F. F., Sharpe T. C., Gibbs A. C. Circadian rhythms in peak expiratory flow rate in workers exposed to cotton dust. Thorax. 1984 Oct;39(10):759–765. doi: 10.1136/thx.39.10.759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cockcroft D. W., Killian D. N., Mellon J. J., Hargreave F. E. Bronchial reactivity to inhaled histamine: a method and clinical survey. Clin Allergy. 1977 May;7(3):235–243. doi: 10.1111/j.1365-2222.1977.tb01448.x. [DOI] [PubMed] [Google Scholar]
- Epstein S. W., Fletcher C. M., Oppenheimer E. A. Daily peak flow measurements in the assessment of steroid therapy for airway obstruction. Br Med J. 1969 Jan 25;1(5638):223–225. doi: 10.1136/bmj.1.5638.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henneberger P. K., Stanbury M. J., Trimbath L. S., Kipen H. M. The use of portable peak flowmeters in the surveillance of occupational asthma. Chest. 1991 Dec;100(6):1515–1521. doi: 10.1378/chest.100.6.1515. [DOI] [PubMed] [Google Scholar]
- Hetzel M. R., Clark T. J., Branthwaite M. A. Asthma: analysis of sudden deaths and ventilatory arrests in hospital. Br Med J. 1977 Mar 26;1(6064):808–811. doi: 10.1136/bmj.1.6064.808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hetzel M. R., Clark T. J. Comparison of normal and asthmatic circadian rhythms in peak expiratory flow rate. Thorax. 1980 Oct;35(10):732–738. doi: 10.1136/thx.35.10.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins B. G., Britton J. R., Chinn S., Jones T. D., Jenkinson D., Burney P. G., Tattersfield A. E. The distribution of peak expiratory flow variability in a population sample. Am Rev Respir Dis. 1989 Nov;140(5):1368–1372. doi: 10.1164/ajrccm/140.5.1368. [DOI] [PubMed] [Google Scholar]
- Knudson R. J., Lebowitz M. D., Holberg C. J., Burrows B. Changes in the normal maximal expiratory flow-volume curve with growth and aging. Am Rev Respir Dis. 1983 Jun;127(6):725–734. doi: 10.1164/arrd.1983.127.6.725. [DOI] [PubMed] [Google Scholar]
- Kondo S. The amplitude of circadian FEV1 variation suitable for phase determination by cosinor analysis in stable asthmatic children. Chest. 1992 Sep;102(3):771–774. doi: 10.1378/chest.102.3.771. [DOI] [PubMed] [Google Scholar]
- Malo J. L., Pineau L., Cartier A., Martin R. R. Reference values of the provocative concentrations of methacholine that cause 6% and 20% changes in forced expiratory volume in one second in a normal population. Am Rev Respir Dis. 1983 Jul;128(1):8–11. doi: 10.1164/arrd.1983.128.1.8. [DOI] [PubMed] [Google Scholar]
- Martin R. J., Cicutto L. C., Ballard R. D. Factors related to the nocturnal worsening of asthma. Am Rev Respir Dis. 1990 Jan;141(1):33–38. doi: 10.1164/ajrccm/141.1.33. [DOI] [PubMed] [Google Scholar]
- McFadden E. R., Jr Circadian rhythms. Am J Med. 1988 Jul 29;85(1B):2–5. doi: 10.1016/0002-9343(88)90230-6. [DOI] [PubMed] [Google Scholar]
- Meltzer A. A., Smolensky M. H., D'Alonzo G. E., Harrist R. B., Scott P. H. An assessment of peak expiratory flow as a surrogate measurement of FEV1 in stable asthmatic children. Chest. 1989 Aug;96(2):329–333. doi: 10.1378/chest.96.2.329. [DOI] [PubMed] [Google Scholar]
- Reinberg A., Gervais P., Chaussade M., Fraboulet G., Duburque B. Circadian changes in effectiveness of corticosteroids in eight patients with allergic asthma. J Allergy Clin Immunol. 1983 Apr;71(4):425–433. doi: 10.1016/0091-6749(83)90073-8. [DOI] [PubMed] [Google Scholar]
- Ryan G., Latimer K. M., Dolovich J., Hargreave F. E. Bronchial responsiveness to histamine: relationship to diurnal variation of peak flow rate, improvement after bronchodilator, and airway calibre. Thorax. 1982 Jun;37(6):423–429. doi: 10.1136/thx.37.6.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakula A. Sir John Floyer's A Treatise of the Asthma (1698). Thorax. 1984 Apr;39(4):248–254. doi: 10.1136/thx.39.4.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smolensky M. H., Barnes P. J., Reinberg A., McGovern J. P. Chronobiology and asthma. I. Day-night differences in bronchial patency and dyspnea and circadian rhythm dependencies. J Asthma. 1986;23(6):321–343. doi: 10.3109/02770908609073179. [DOI] [PubMed] [Google Scholar]
- Turner-Warwick M. On observing patterns of airflow obstruction in chronic asthma. Br J Dis Chest. 1977 Apr;71(2):73–86. doi: 10.1016/0007-0971(77)90086-9. [DOI] [PubMed] [Google Scholar]


