Abstract
Objective
The aims of our study were to verify the validity of the T-Scan III system (Tekscan) as an objective occlusal evaluation tool, and to assess the differences between two occlusal indexes-the peer assessment rating (PAR) index and the American Board of Orthodontics objective grading system (OGS)-by comparing the scores derived from the T-Scan III system with the two occlusal indexes and analyzing the correlations between them.
Methods
The final study sample included 48 adult volunteers (39 men and 9 women, mean age 24.14 ± 3.16 years), after excluding 29 volunteers whose occlusion could not be evaluated by the T-Scan III system due to severe skeletal or occlusal problems. PAR index and OGS scores were assessed using dental study models, and measurements of centric occlusion, protrusive movement, and lateral excursion movement were obtained via the T-Scan III system. The results were analyzed to determine correlations.
Results
Occlusal analysis by the T-Scan III system was clinically reliable (p < 0.05), and the PAR index and OGS scores were significantly correlated with several measurements obtained with the T-Scan III system (p < 0.05).
Conclusions
The T-Scan III system is a quantitative and reliable method for occlusal evaluation, and represents a potential substitute for occlusal indexes. Compared to the PAR index, the OGS scores of more variables were significantly correlated with the T-Scan measurements.
Keywords: Dental cast analysis, Orthodontic index, T-Scan, Occlusal evaluation
INTRODUCTION
From a recovery-of-function perspective, orthodontic treatment requires as much stability and precision as full-mouth rehabilitation does in the area of prosthodontics, when endeavoring to achieve satisfactory occlusion. However, occlusion formation in orthodontics has received comparatively less attention. Nevertheless, after orthodontic treatment, occlusal functional stability must be evaluated.
Methods for evaluating occlusal contact can be divided into qualitative and quantitative analyses. Qualitative analysis involves evaluating tooth contact and the positions of the teeth by means of occlusal film, shim stock, wax, and silicone. The disadvantages of this method include its lack of objectivity and reproducibility, as well as the difficulty of describing the various states of occlusion. Quantitative analysis involves the use of various occlusal indexes1,2 to evaluate the pretreatment occlusal state and the results of orthodontic treatment. However, some have argued that these indexes can vary depending on who takes the measurements, rendering them less reliable in terms of precision and objectivity.3
The peer assessment rating (PAR index)4 was first introduced in 1987. This occlusal index measures values based on dental casts taken before and after orthodontic treatment to quantitatively describe the status of the occlusion. While the PAR index is sufficient in terms of reproducibility and adequacy, it is not precise enough to distinguish minute differences in tooth position, and the weighting system can be problematic in that some indexes related to weighting can be overlooked.5
In 1999, the American Board of Orthodontics (ABO) introduced the objective grading system (OGS), which evaluates the results of orthodontic treatment via post-treatment dental casts and panoramic radiographs. In this method, a special ruler is used to measure seven indexes from the dental cast and one index from the panoramic radiograph, and these indexes are represented numerically.6
The traditional occlusal index has low objectivity and its results often differ owing to the perspective or proficiency of the measurer, rendering it insufficient in terms of reproducibility and validity.7 This index also uses dental casts and panoramic radiographs to analyze static occlusion, but occlusion is not static, rather it is a parameter of a structure with dynamic motion. Occlusion must therefore be evaluated not only based on dental casts, but also with consideration of factors relating to dynamic motion, such as intermaxillary maximum intercuspation, protrusion, and lateral excursion.
The T-Scan III system developed by Tekscan (Boston, MA, USA) uses computers to analyze dynamic occlusion, allowing both qualitative and quantitative occlusion analysis to be performed simultaneously and with great precision.8 Because occlusion involves the entire dentition, not just part of it, this method represents occlusal status in terms of quantitative values for various parameters such as the distribution of occlusive forces in the anterior area, between molars, and between the right and left dentition. In addition, it can measure the sequence of tooth contact and quantitative changes in relation to time, locate excessive occlusal forces, and register the amount of time from early contact to equilibrium of occlusal forces. Therefore, the T-Scan system provides information that cannot be obtained by traditional methods of occlusal measurement and evaluation. In addition, when repeated measurements in the same subjects were evaluated there was no statistically significant difference between the results, meaning that this method has sufficient validity and reproducibility.9
This study was designed to verify the validity of the T-Scan III system as an objective occlusal evaluation tool, and to assess the differences between it and the PAR index and the OGS by comparing the scores obtained using the T-Scan III system with those obtained via the latter two indexes and analyzing the resulting correlations.
MATERIALS AND METHODS
To represent the general population, which exhibits a variety of occlusal patterns, we selected 48 study subjects (39 men and 9 women, mean age 24.14 ± 3.16 years) from 77 healthy adult volunteers. The exclusion criteria were as follows: (1) existence of orthodontic appliances, (2) edentulous areas, (3) severe periodontal disease, (4) severe skeletal deformities in the maxillofacial area, (5) a history of systemic disease, and (6) severe occlusal interference making it difficult to measure the T-Scan III system variables. This study was approved by the institutional review board of the Dankook University Dental Hospital (approval number H1110/008/003).
Occlusal index scoring
Based on dental models derived from the participants, two occlusal indexes were measured; the PAR index and the OGS. The PAR index is a quantitative occlusal index designed to evaluate pretreatment malocclusions and the effects of orthodontic treatments. The variables of the PAR index are displacement, buccal occlusion, overjet, overbite, and centerline, and a high score indicates an unsatisfactory occlusal condition. The OGS is designed to assess final occlusion via post-treatment dental casts and panoramic radiographs, as part of the ABO phase III examination. To achieve the most objective assessment of the dental casts possible, we used a specific ABO measuring gauge. Because the scores are subtracted from an initial total of 316, a high score indicates good occlusal condition. The OGS variables include tooth alignment, vertical positioning of marginal ridges, buccolingual inclination of posterior teeth, occlusal relationship, occlusal contacts, overjet, and interproximal contacts.
T-Scan III system methods
Before the examination, the subjects were taught the required mandibular movements and were asked to practice the required lateral mandibular excursions and protrusion in order to reduce measurement errors. At each step, the position of the occlusion and the condition of the sensor were inspected.
Centric occlusion, right lateral excursion, left lateral excursion, and protrusion were measured a total of four times each, then the maximum and minimum values were excluded and the average of the two intermediate values was calculated. As a precaution against weakening of occlusal forces over time due to fatigue, subjects were allowed to rest for 5 minutes after four trials of each type of movement. To maintain a regular sensor position during the four trials, the sensor was not removed from the oral cavity during the rest periods.
T-Scan III system variables
Table 1 shows the T-Scan III system variables measured in this study. Occlusion time (OT) describes the time from the first tooth contact to the point at which the entire dentition is contacted when evaluating maximum intercuspation. This evaluates how fast the entire dentition enters the occlusion status. When this period of time is long, there is occlusion interference, and when it is short, the occlusion is considered to be stable, especially when the span is less than 0.3 seconds. Disclusion time (DT) is the time from when anterior or canine guidance is formed to the point where molar contact is lost during lateral excursion (right [Rt]-DT, left [Lt]-DT) or protrusion (Pro-DT). The longer this period of time, the greater the interference of molars during lateral excursion or protrusion. A time of less than 0.5 seconds is considered normal.10
Table 1. Definitions of the T-Scan variables used in this study.
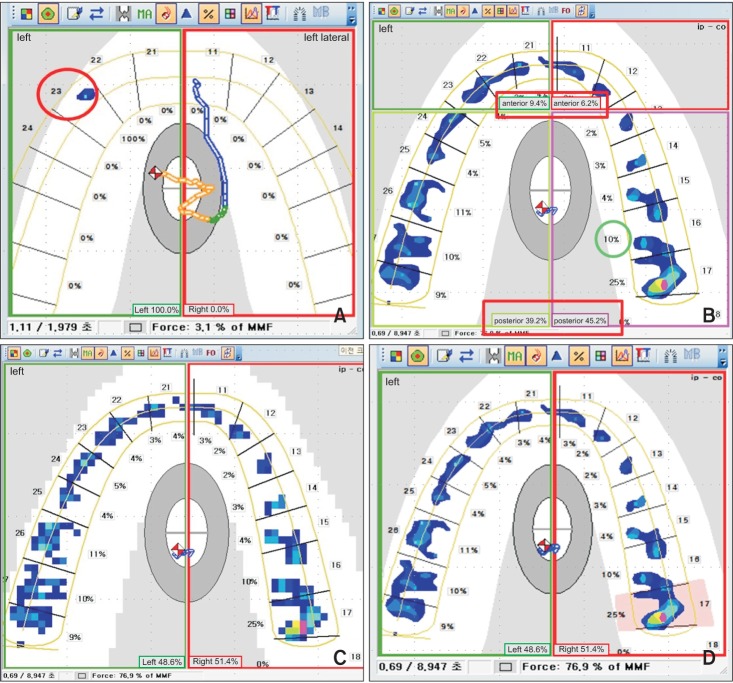
On the T-Scan, the occlusal force is presented as a relative value rather than an absolute one, making it difficult to compare a given value with that of another individual. As a result, in this study, we categorized and developed indexes that allowed comparisons between individuals, and thus could be analyzed statistically (Figure 1).
Figure 1. T-Scan overviews. A, Force distribution ratio of an maxillary left canine at D-point during left lateral excursion movement (canine guidance). B, The relative distribution of occlusal force is marked in each tooth as a green circle, and the arches are divided into four parts so that the relative distribution of the anterior-posterior occlusal forces on each side can be shown. C, The maximum area frame of the movie of maximum intercuspation was converted from contour lines to pixels, and the values were calculated. D, Representing the force outlier, the relative occlusal force for each tooth is the pink area.
The force distribution ratio of the maxillary canine at D-point (the point where the balancing side dentition loses contact) during the lateral excursion movement was evaluated to study the degree of canine guidance (Figure 1A). The force distribution ratio of the canines at D-point was measured from both the right (Rt-D-3) and the left (Lt-D-3). The force distribution ratio of the canines in Figure 1A is 100 percent (represented by 1.0), meaning that canine guidance is being performed.
The occlusal force ratio for right and left, centered on the midline, are described (100 percent is represented by 1.0). This is again divided into anterior and posterior, and as a result the occlusal force ratio of a total of four areas can be seen (Figure 1B). The relative distribution of occlusal force is marked in each tooth as a circle, and it also shows the ratio of occlusal forces of both sides. The arches are divided into four parts so that the relative distribution of the anterior-posterior occlusal forces on each side can be shown on the T-Scan. By subtracting the weaker side's occlusal force from the stronger side's occlusal force, the difference can be measured, i.e., the entire occlusal surface (DF-Total), anterior (DF-Ant), and posterior (DF-Post).
To measure the occlusal surface area when the teeth are in maximal contact (Occ-contact-Area), the maximum area frame (MA) of the movie of maximum intercuspation was converted from contour lines to pixels, and the values were calculated. After converting the occlusal window to pixels to measure the area of occlusal surface, the number of pixels was multiplied by 1.04 mm2 (the area of a pixel) to measure the occlusal surface area (Figure 1C).
The force outlier, which is the singular value for force, was also measured (sigma = maximum relative force). For representing the force outlier, the specimen showing the relative occlusal force for each tooth is the highest bar in T-Scan (pink area in Figure 1D). This is an index representing the degree of force when a tooth is under more occlusal force at a certain occlusal position than are the surrounding teeth. As the first value is more important than the largest value, this index was measured as both the first value (FO-First) and the largest value (FO-Max).
Statistical analysis
Statistical analysis was performed using SPSS version 12.0 for Windows (SPSS Inc., Chicago, IL, USA). Using descriptive statistics, we obtained the means (± standard deviation) of the values measured via the subjects' occlusal indexes (PAR index and OGS) and the T-Scan system. From the continuous variables, the occlusal indexes (PAR index and OGS) variables were categorized into interval scales. Therefore, these were analyzed by means of Spearman correlation analysis, a nonparametric method, and regression analysis was not performed for the same reason.
From the total of 48 subjects, 15 were selected at random for re-examination of the same indices by the same examiner after 1 week. The Wilcoxon signed-rank test was used to test the systematic error for reproducibility, and the random error was evaluated using Dahlberg's formula11:
where d is the difference between the two measured values and n is the number of subjects.
No systematic error was observed for the PAR index, the OGS, or the T-Scan based on the reliability test. The random error of the measured T-Scan values calculated using Dahlberg's formula is shown in Table 2. The random error range for the PAR index was 0.224-1.204, and the random error range for OGS was 0.68-1.20.
Table 2. Reliability test (Wilcoxon signed-rank test) and random error of T-Scan measurements.
Refer to Table 1 for the definitions of all variables.
RESULTS
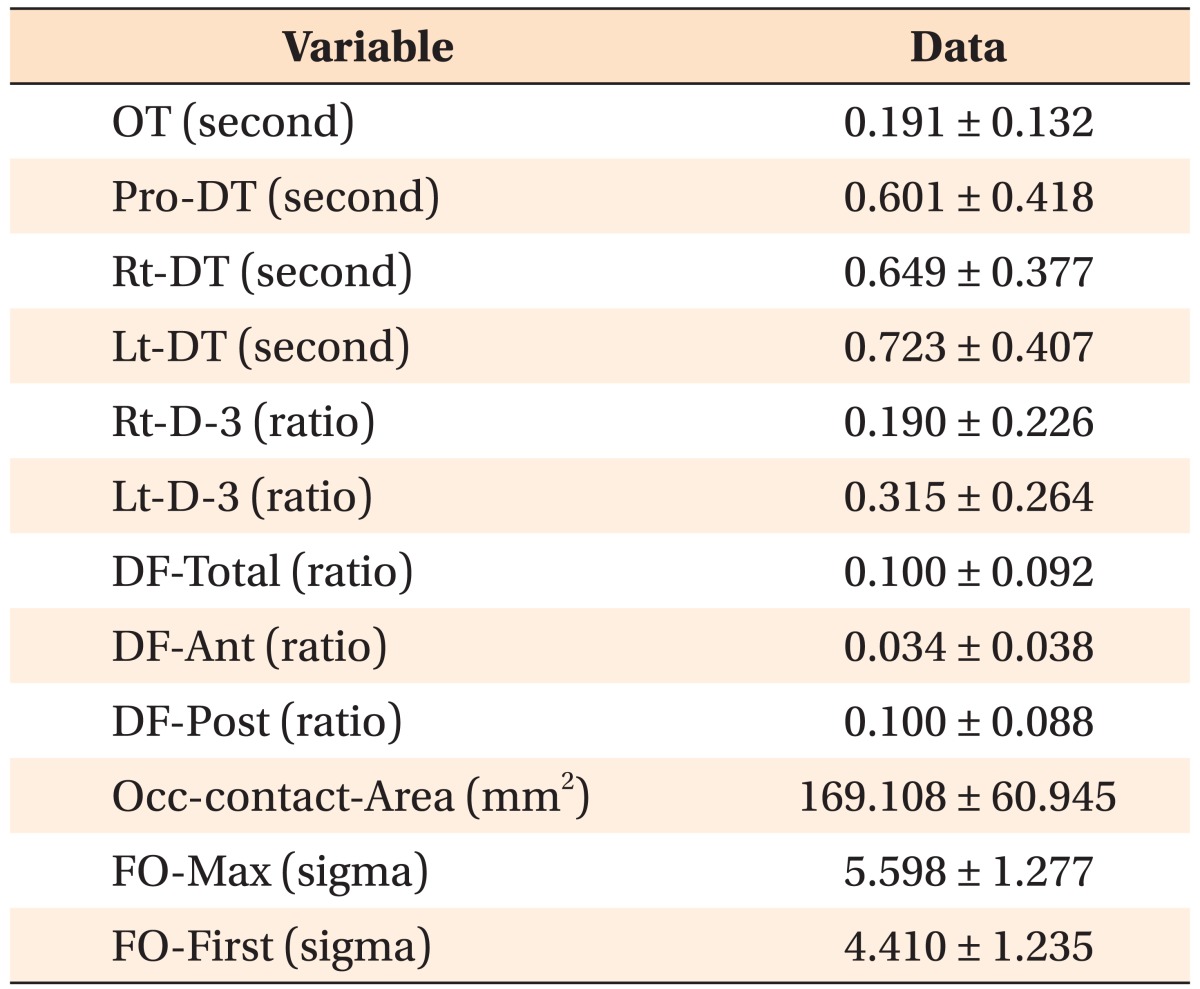
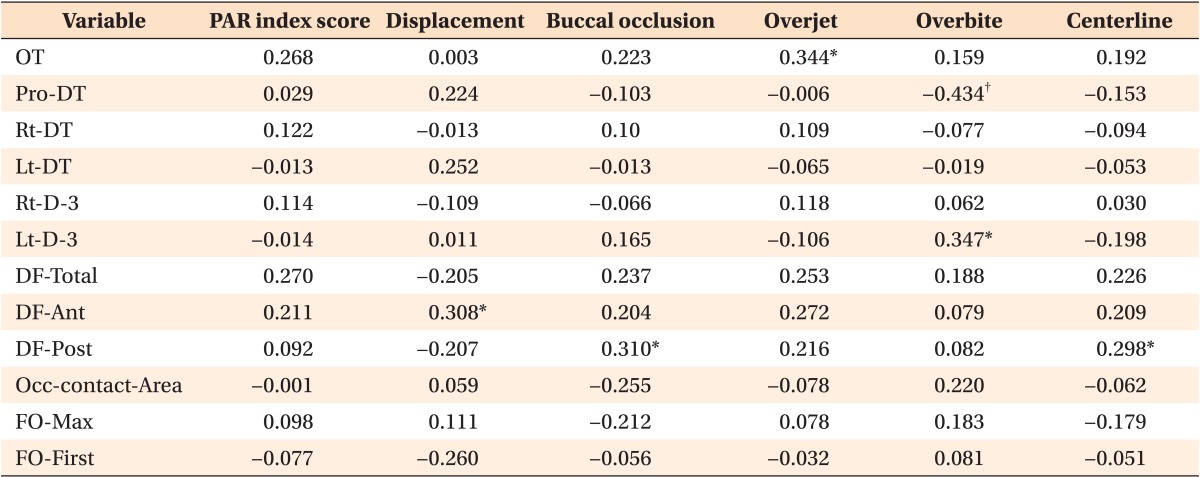
Descriptive statistics for the occlusal indexes (PAR index and OGS) and the T-Scan III system are shown in Tables 3 and 4. Tables 5 and 6 show the results of the Spearman correlation analysis comparing the occlusal indexes (PAR and OGS) and the T-Scan system. The OGS had nearly twice as many measuring items that correlated significantly with the T-Scan measurements, as compared with the PAR index. Moreover, there were more OGS variables than PAR variables that showed the large correlation coefficient with the T-Scan measurements (Tables 5 and 6). T-Scan variables that correlated significantly with the PAR index were OT, Pro-DT, Lt-D-3, DF-Ant, and DF-Post. On the other hand, T-Scan variables that correlated significantly with the OGS were OT, Pro-DT, Rt-DT, DF-Post, and Occ-contactrea.
Table 3. Descriptive statistics for the PAR index and OGS scores.
Values are presented as mean±standard deviation.
PAR index, Peer assessment rating index; OGS, American Board of Orthodontics objective grading system.
Table 4. Descriptive statistics for the T-Scan III system measurements.
Values are presented as mean±standard deviation.
T-Scan III: Tekscan, Boston, MA, USA.
Refer to Table 1 for the definitions of all variables.
Table 5. Spearman correlation analysis between the PAR index and the T-Scan III system.
The values presented are correlation coefficients.
PAR index, Peer assessment rating index. T-Scan III: Tekscan, Boston, MA, USA.
Refer to Table 1 for the definitions of all variables.
*p < 0.05, †p < 0.01.
Table 6. Spearman correlation analysis between the OGS and the T-Scan III system.
The values presented are correlation coefficients.
OGS, American Board of Orthodontics objective grading system. T-Scan III: Tekscan, Boston, MA, USA.
Refer to Table 1 for the definitions of all variables.
*p < 0.05, †p < 0.01.
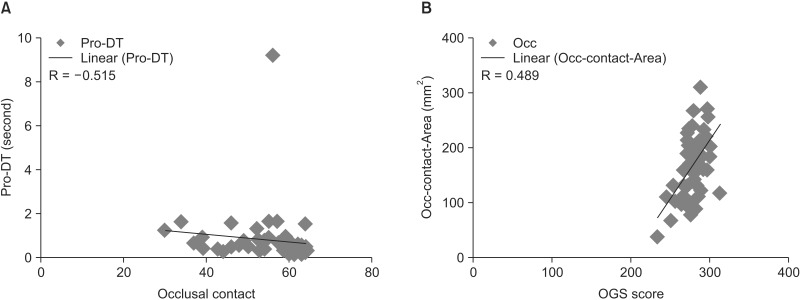
Scattergrams showing the correlations between the OGS and the T-Scan III system are shown in Figure 2.
Figure 2. Correlational analyses. A, Scattergram of the correlation between occlusal contact and Pro-DT. B, Scattergram of the correlation between OGS score and Occ-contact-Area. R, Correlation coefficient.
Refer to Tables 1, 3, and 4 for the definitions and units of all variables.
Correlations between the PAR index and the T-Scan III system
Overjet (PAR) was significantly positively correlated with OT. As overjet (PAR) increased (occlusion worsened), OT was increased (occlusion worsened). Overbite (PAR) was negatively correlated with DT. As overbite (PAR) increased (occlusion worsened), DT of protrusive movement was reduced (occlusion improved). This finding is contradictory.
As overbite (PAR) increased (occlusion worsened), Lt-D-3 increased (similar to canine guidance). This finding is also contradictory. As displacement (anterior crowding) increased (occlusion worsened), DF-Ant increased (occlusion worsened).
As buccal occlusion increased (buccal occlusion worsened), DF-Post increased (occlusion worsened). As centerline increased (midline deviation increased), DF-Post increased (occlusion worsened).
Correlations between the OGS and the T-Scan III system
As OGS score increased (occlusion improved), OT was reduced (occlusion improved). As occlusal relation increased (sagittal part of occlusion improved), OT was reduced (occlusion improved).
As overjet (OGS) increased (occlusion improved), OT was reduced (occlusion improved). As occlusal contact increased (occlusion improved), protrusion DT was reduced (occlusion improved) (Figure 2A).
As OGS score increased (occlusion improved), DF-Post decreased (occlusion improved). As marginal ridges increased (difference between marginal ridges of adjacent teeth improved), DF-Post decreased (occlusion improved).
As buccolingual inclination increased (occlusion improved), DF-Post decreased (occlusion improved). As OGS score increased (occlusion improved), occlusal contact area increased (occlusal contact area at MA improved) (Figure 2B).
As occlusal contact increased (occlusion improved), occlusal contact area increased (occlusal contact area at MA improved).
DISCUSSION
The T-Scan III system cannot measure the absolute value of occlusal force, which can vary each time the subject bites down and according to the patient's position or the location of the occlusal contacts. Thus, measuring the absolute force of occlusion can be misleading, so the T-Scan, which can detect unequal distribution or relative occlusion, will indicate where excessive force is concentrated, and the changes in occlusion over time will be more useful clinically.
Wang et al.12 asserted that recordings made by the T-Scan II system are clinically useful in terms of precision and reproducibility when studying occlusal contact in lateral excursion. Saliva in the oral cavity does not affect the T-Scan system's recording process.4 Similarly, other clinical and laboratory research has confirmed the pressure sensitivity, accuracy, and stability of relative force loadings and the reproducibility of results obtained via the T-Scan system.13
To evaluate the reproducibility of our experiment, we measured the systematic error. The PAR index, OGS, and T-Scan system all resulted in no systematic errors and showed adequate reproducibility. Table 6 shows the reproducibility of the T-Scan system. In our study, we trained the subjects prior to obtaining measurements, in an effort to reproduce precise mandibular movements, increasing the precision of measurements. Sensor placement was as uniform as possible each time the measurements were made. A rest interval between measurements restored the stability of the occlusal force. To obtain accurate results for the indexes measured, location and time were strictly defined to decrease errors, resulting in acceptable reproducibility.
The pros of the T-scan system include not only its objectivity and reproducibility, but also the fact that it can detect occlusal changes over time. This system was able to measure the parameters that time-related factors, occlusal papers, and the occlusal indexes could not show. In addition, this method is currently the only one available for studying the dynamic characteristics of occlusion.10
To evaluate dynamic occlusion and the usefulness of occlusion evaluation, Kerstein and Wright10 reported an increase in DT in patients with chronic fascial pain disorder, and occlusal adjustment decreased DT, thus improving symptoms and confirming the effectiveness of the T-Scan system in occlusion analysis. Mizui et al.14 used the T-Scan system to study the difference in occlusion balance between patients with temporomandibular joint (TMJ) dysfunction and patients with normal TMJ function. The group with normal function showed balanced bilateral occlusion according to the T-Scan index, with the center of force appearing in the first molar region. On the other hand, the patients with TMJ dysfunction showed an asymmetrical, imbalanced occlusion.
In our study we found that the larger the PAR-overjet value (inadequate occlusion), the larger the OT value (inadequate occlusion), and this relationship was significant. Moreover, as the OGS-occlusal relation value became larger the OT value decreased, also indicating a relationship between the two values. The T-Scan system's effectiveness as an occlusion analysis tool was confirmed by the tendency for the OGS-overjet value to increase as the OT value decreased. In our study, the larger the imbalance in posterior occlusion as determined via the T-Scan, the larger the values of buccal occlusion and centerline according to the PAR index, indicating a relationship between these values. The larger the OGS value (the more ideal the occlusion), the lower the posterior imbalance value as determined via the T-Scan, thus confirming the effectiveness, objectivity, and quantitative characteristics of the T-Scan system as an occlusion evaluation tool.
The D-point was defined as the point where the molars diverge and the anterior teeth or canines make contact; however, in reality, various teeth guidelateral movement when lateral excursion occurs, and as a result, it is difficult to calculate DT precisely. In our study, we defined the D-point as the point where the entire balancing side dentition diverges, and the results obtained confirmed that this definition is valid. This finding will require complementary measurements in future studies. Our results showed that when the overbite value on the PAR index increased, the Lt-D-3 value on the T-Scan was higher—a contradictory result, possibly because even when actual occlusion is satisfactory, group function guides lateral excursion, or vice versa.
Based on the measured values, the increase in the overbite value on the PAR index and the decrease in DT on the T-Scan indexes were significantly related—another conflicting outcome. However, since the gradient of the line formed on the scattergram was not high, one can interpret this result as follows: the overbite value on the PAR index increases as the open bite and deep bite both worsen, and these factors combined to modify the result. This finding can be viewed as a limitation of the PAR index.
The PAR index has been used to evaluate treatment results by comparing normal tooth alignment and occlusion with those parameters in patients with malocclusion, to measure the degree of deviation.15 The limitations of the PAR index have also been reported.16 Hamdan and Rock5 pointed out that the overbite value was weighted as more important than the value of the overjet, and McGorray et al.17 noted that this conclusion depends on the orthodontist's personal opinion. Overall, the PAR index relies heavily on the proficiency of the clinicians and their subjective perspectives.
The OGS, first developed in 1999 by the ABO for evaluating the results of orthodontic treatment, tends to assess only the outcome of such treatment and does not consider the severity of pretreatment needs or the complex treatment procedures required.18 Murakami et al.19 pointed out that this scoring system varies depending on the proficiency of the dentist's measuring methods, and that caution is needed when one is scoring buccolingual inclination.
Traditionally, the OGS has been used as an index for evaluating the results of orthodontic treatment. We used the OGS in an experimental group who did not undergo orthodontic treatment, and occlusion status varied with this method. However, we had excluded those subjects who had severe skeletal deformities in the craniofacial region, and those with dentition loss, because in such individuals it was difficult to measure the required indices via the T-Scan system due to severe occlusal interference. Therefore, the validity of OGS measurements was not greatly affected (Table 3).
This study was conducted to evaluate the T-Scan III system and objectively apply it to address the aforementioned limitations of the occlusal indexes for evaluating occlusion. Our results were positive and confirmed that the T-Scan III system is a valid and objective method, and has the potential to be substituted for the conventional occlusal indexes. However, analysis using the T-Scan III system still has shortcomings that need to be remedied. Future studies in normal samples or well-treated samples should be undertaken, to improve occlusal evaluation using the T-Scan III system.
CONCLUSION
Overall, the OGS had nearly twice as many measuring items significantly correlated with the T-Scan III system measurements than the PAR index. Since the scores for both open bite and deep bite subjects on the overbite parameter of the PAR index increased as severity increased, it appears that the same points were scored in two opposite situations, resulting in statistical bias. The T-Scan III system has adequate reliability and is a quantitative, objective, and reliable method for "dynamic" occlusal evaluation, but it still requires further study and improvement before it can be substituted for the "static" occlusal indexes.
Footnotes
*The present research was conducted by the research fund of Dankook University in 2013.
The authors report no commercial, proprietary, or financial interest in the products or companies described in this article.
References
- 1.Eismann D. Reliable assessment of morphological changes resulting from orthodontic treatment. Eur J Orthod. 1980;2:19–25. [PubMed] [Google Scholar]
- 2.Berg R. Post-retention analysis of treatment problems and failures in 264 consecutively treated cases. Eur J Orthod. 1979;1:55–68. doi: 10.1093/ejo/1.1.55. [DOI] [PubMed] [Google Scholar]
- 3.Casko JS, Vaden JL, Kokich VG, Damone J, James RD, Cangialosi TJ, et al. Objective grading system for dental casts and panoramic radiographs. American Board of Orthodontics. Am J Orthod Dentofacial Orthop. 1998;114:589–599. doi: 10.1016/s0889-5406(98)70179-9. [DOI] [PubMed] [Google Scholar]
- 4.Richmond S, Shaw WC, O'Brien KD, Buchanan IB, Jones R, Stephens CD, et al. The development of the PAR Index (Peer Assessment Rating): reliability and validity. Eur J Orthod. 1992;14:125–139. doi: 10.1093/ejo/14.2.125. [DOI] [PubMed] [Google Scholar]
- 5.Hamdan AM, Rock WP. An appraisal of the Peer Assessment Rating (PAR) Index and a suggested new weighting system. Eur J Orthod. 1999;21:181–192. doi: 10.1093/ejo/21.2.181. [DOI] [PubMed] [Google Scholar]
- 6.Deguchi T, Honjo T, Fukunaga T, Miyawaki S, Roberts WE, Takano-Yamamoto T. Clinical assessment of orthodontic outcomes with the peer assessment rating, discrepancy index, objective grading system, and comprehensive clinical assessment. Am J Orthod Dentofacial Orthop. 2005;127:434–443. doi: 10.1016/j.ajodo.2004.03.030. [DOI] [PubMed] [Google Scholar]
- 7.Throckmorton GS, Rasmussen J, Caloss R. Calibration of T-Scan sensors for recording bite forces in denture patients. J Oral Rehabil. 2009;36:636–643. doi: 10.1111/j.1365-2842.2009.01978.x. [DOI] [PubMed] [Google Scholar]
- 8.Maness WL, Benjamin M, Podoloff R, Bobick A, Golden RF. Computerized occlusal analysis: a new technology. Quintessence Int. 1987;18:287–292. [PubMed] [Google Scholar]
- 9.Koos B, Godt A, Schille C, Göz G. Precision of an instrumentation-based method of analyzing occlusion and its resulting distribution of forces in the dental arch. J Orofac Orthop. 2010;71:403–410. doi: 10.1007/s00056-010-1023-7. [DOI] [PubMed] [Google Scholar]
- 10.Kerstein RB, Wright NR. Electromyographic and computer analyses of patients suffering from chronic myofascial pain-dysfunction syndrome: before and after treatment with immediate complete anterior guidance development. J Prosthet Dent. 1991;66:677–686. doi: 10.1016/0022-3913(91)90453-4. [DOI] [PubMed] [Google Scholar]
- 11.Dahlberg G. Statistical methods for medical and biological students. London: G Allen & Unwin Ltd; 1940. pp. 1–140. [Google Scholar]
- 12.Wang YL, Cheng J, Chen YM, Yip KH, Smales RJ, Yin XM. Patterns and forces of occlusal contacts during lateral excursions recorded by the T-Scan II system in young Chinese adults with normal occlusions. J Oral Rehabil. 2011;38:571–578. doi: 10.1111/j.1365-2842.2010.02194.x. [DOI] [PubMed] [Google Scholar]
- 13.Garrido García VC, García Cartagena A, González Sequeros O. Evaluation of occlusal contacts in maximum intercuspation using the T-Scan system. J Oral Rehabil. 1997;24:899–903. doi: 10.1046/j.1365-2842.1997.00586.x. [DOI] [PubMed] [Google Scholar]
- 14.Mizui M, Nabeshima F, Tosa J, Tanaka M, Kawazoe T. Quantitative analysis of occlusal balance in intercuspal position using the T-Scan system. Int J Prosthodont. 1994;7:62–71. [PubMed] [Google Scholar]
- 15.Richmond S, Shaw WC, O'Brien KD, Buchanan IB, Jones R, Stephens CD, et al. The development of the PAR Index (Peer Assessment Rating): reliability and validity. Eur J Orthod. 1992;14:125–139. doi: 10.1093/ejo/14.2.125. [DOI] [PubMed] [Google Scholar]
- 16.Fox NA. The first 100 cases: a personal audit of orthodontic treatment assessed by the PAR (peer assessment rating) index. Br Dent J. 1993;174:290–297. doi: 10.1038/sj.bdj.4808157. [DOI] [PubMed] [Google Scholar]
- 17.McGorray SP, Wheeler TT, Keeling SD, Yurkiewicz L, Taylor MG, King GJ. Evaluation of orthodontists' perception of treatment need and the peer assessment rating (PAR) index. Angle Orthod. 1999;69:325–333. doi: 10.1043/0003-3219(1999)069<0325:EOOPOT>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 18.Onyeaso CO, Begole EA. Relationship between index of complexity, outcome and need, dental aesthetic index, peer assessment rating index, and American Board of Orthodontics objective grading system. Am J Orthod Dentofacial Orthop. 2007;131:248–252. doi: 10.1016/j.ajodo.2005.04.045. [DOI] [PubMed] [Google Scholar]
- 19.Murakami K, Deguchi T, Hashimoto T, Imai M, Miyawaki S, Takano-Yamamoto T. Need for training sessions for orthodontists in the use of the American Board of Orthodontics objective grading system. Am J Orthod Dentofacial Orthop. 2007;132:427.e1–427.e6. doi: 10.1016/j.ajodo.2007.02.050. [DOI] [PubMed] [Google Scholar]