Abstract
The aim of this clinical report is to describe the complex treatment of an adult Class III malocclusion patient who was disappointed with the outcome of a previous oral rehabilitation. Interdisciplinary treatment planning was performed with a primary indication for implant removal because of marginal bone loss and gingival recession, followed by orthodontic and surgical procedures to correct the esthetics and skeletal malocclusion. The comprehensive treatment approach included: (1) implant removal in the area of the central incisors; (2) combined orthodontic decompensation with mesial displacement and forced extrusion of the lateral incisors; (3) extraction of the lateral incisors and placement of new implants corresponding to the central incisors, which received provisional crowns; (4) orthognathic surgery for maxillary advancement to improve occlusal and facial relationships; and finally, (5) orthodontic refinement followed by definitive prosthetic rehabilitation of the maxillary central incisors and reshaping of the adjacent teeth. At the three-year follow-up, clinical and radiographic examinations showed successful replacement of the central incisors and improved skeletal and esthetic appearances. Moreover, a Class II molar relationship was obtained with an ideal overbite, overjet, and intercuspation. In conclusion, we report the successful esthetic anterior rehabilitation of a complex case in which interdisciplinary treatment planning improved facial harmony, provided gingival architecture with sufficient width and thickness, and improved smile esthetics, resulting in enhanced patient comfort and satisfaction. This clinical case report might be useful to improve facial esthetics and occlusion in patients with dentoalveolar and skeletal defects.
Keywords: Esthetics, Dental implants, Orthodontics, Orthognathic surgery
INTRODUCTION
Implant-supported oral rehabilitation has provided predictable treatment outcomes and elevated the success rate of selected clinical cases in the anterior maxilla.1 However, implant rehabilitation is a complex, challenging, and meticulous procedure for oral surgeons in patients with an unfavorable periodontal biotype associated with extensive bone defects and skeletal anteroposterior discrepancies.2,3 In this context, facial profile, dental occlusion, esthetic arrangement of the teeth, systemic alterations, and qualitative and quantitative assessments of available soft and hard tissues are important aspects that must be evaluated to achieve successful implant rehabilitation.4,5,6,7
From an esthetic standpoint, interdisciplinary treatment planning plays an important role in the clinical success of dental implants.1,8,9 Under normal conditions, osseointegrated implants must be properly sized and correctly positioned by following the rules of restorative-driven three-dimensional (3D) placement into the receptor areas.10 This enables an optimal gingival contour, the presence of papillae, adequate gap dimensions, and decreased buccal bone resorption.1,8,9,10 Improper implant placement may result in an undesirable loss of bone tissue, leading to mucogingival, biological, and biomechanical problems.11,12,13,14,15
Slow orthodontic forces along both the mesiodistal and vertical teeth axes are viable alternatives to 3D reconstructive procedures instead using bone grafts.16,17,18,19 Orthodontic movement, especially forced orthodontic eruption (FOE), increases the amount of attached gingiva and buccal bone, improving the 3D topography of the periodontal apparatus.16,17,18,19,20,21 Moreover, in patients with an unfavorable facial pattern caused by anteroposterior involvement, orthodontic movement is limited by the lack of a natural anterior protrusion on the alveolar ridge. One alternative for the correction of such sagittal discrepancies is orthognathic surgery.22
When attempting to improve skeletal malocclusion, increase patient satisfaction, and enhance esthetic outcomes, an interdisciplinary approach is essential for a more stable, predictable, and successful result. Thus, the aim of this clinical report is to present a complex oral rehabilitation procedure designed to meet the patient's functional and esthetic expectations that involved orthodontic movement, FOE, implant placement, orthognathic surgery, and prosthetic rehabilitation.
DIAGNOSIS AND ETIOLOGY
A 25-year-old Caucasian woman was referred to the Department of Oral Implantology for treatment of her anterior maxillary region. When she was 12 years old, she suffered trauma leading to the avulsion of her central incisors with no possibility of replantation. Five years later, she underwent orthodontic compensation followed by implant replacement of her central incisors. Eight years after implant placement and prosthetic rehabilitation, the patient expressed dissatisfaction with the esthetic outcome of her previous rehabilitation because of gingival recession and marginal bone loss. She had no significant medical history, was a nonsmoker, and denied consuming alcohol.
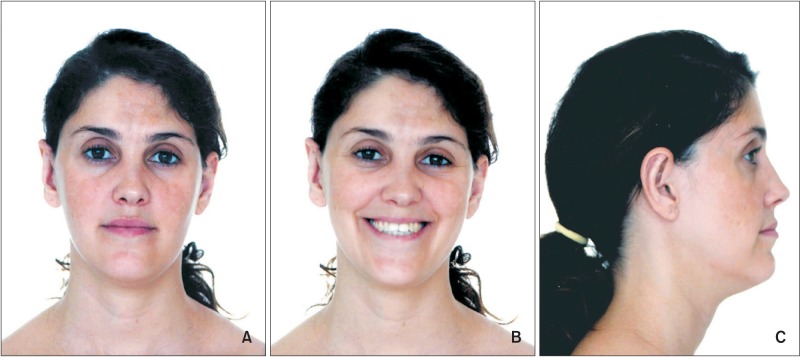
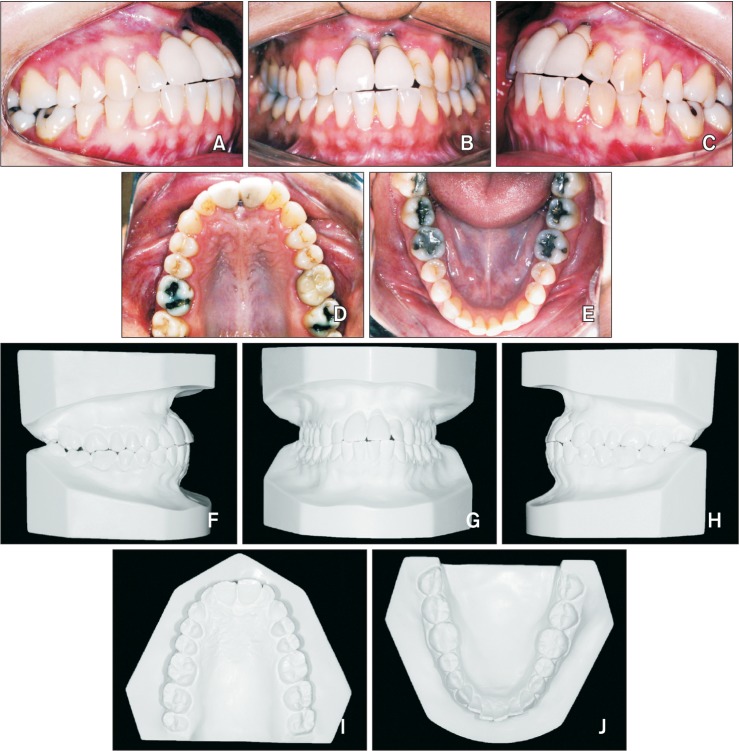
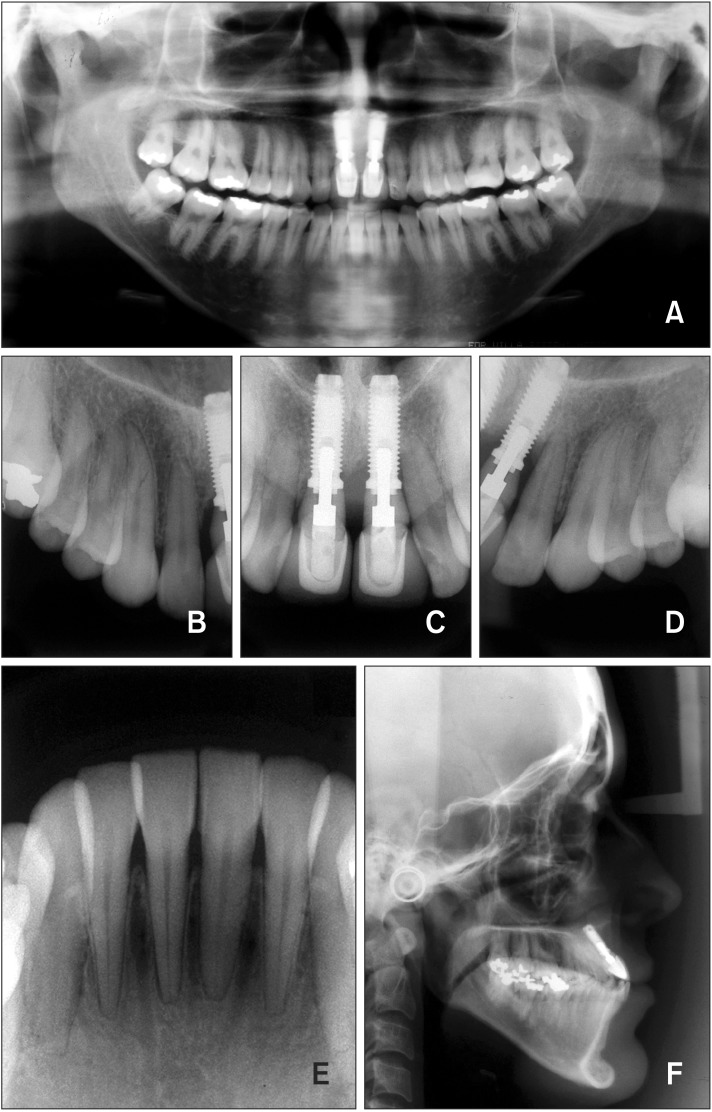
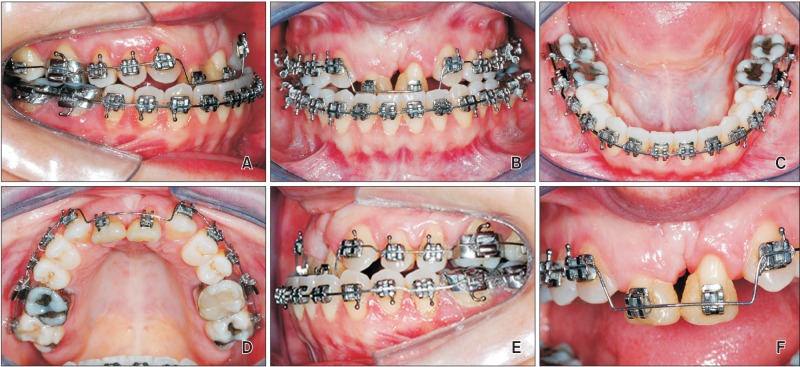
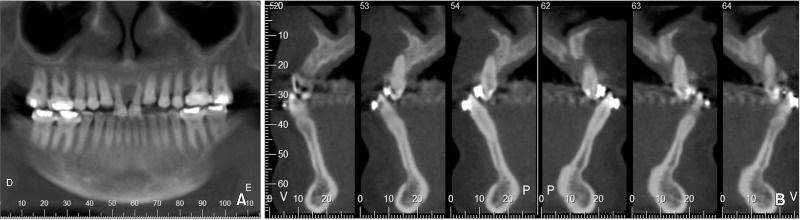
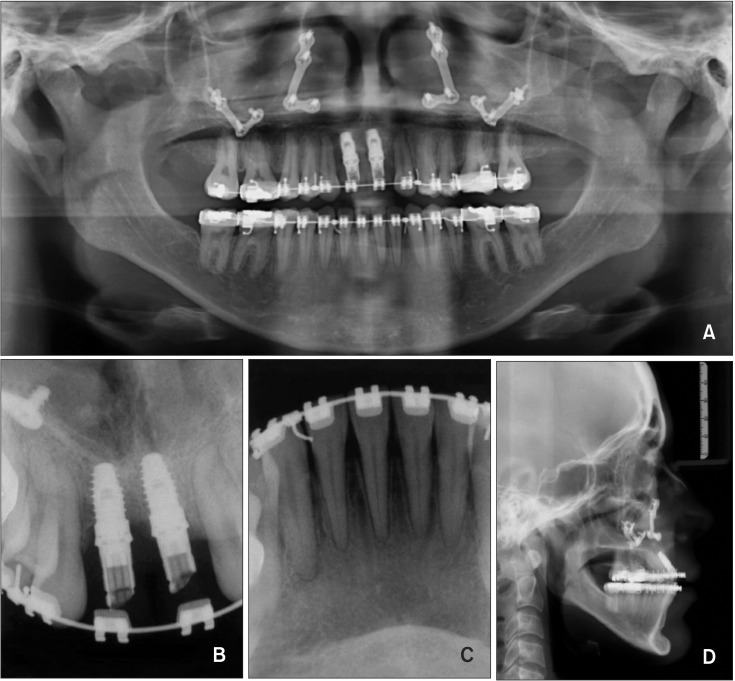
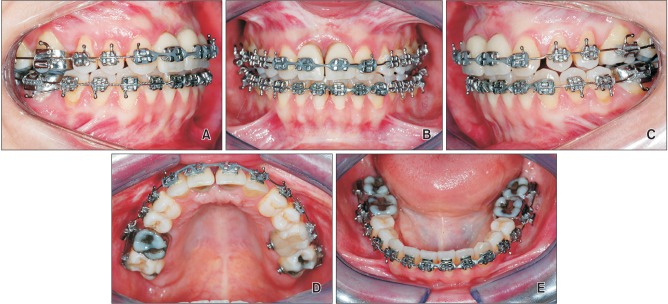
The initial facial examination revealed a Class III skeletal pattern with moderate maxillary deficiency (Figure 1). The occlusal relationship was Class I bilaterally, and markedly compensated with an end-to-end bite and reduced overjet and overbite. A clinical examination showed 2 osseointegrated implants in the central incisor region with a marked collapse of peri-implant tissues, extensive gingival recession, absence of keratinized gingiva, and 5 mm of probing depth. Moreover, prosthetic abutments and the cervical portions of the implants were exposed to the oral environment (Figure 2). Panoramic (Figure 3A) and periapical radiographs (Figure 3B-E) showed advanced vertical bone resorption in the implant region, with the first 3 threads exposed on the left implant. Furthermore, the left implant was in intimate contact with the left lateral incisor, violating the minimum distances established to optimize esthetics, and thus hindering the implant's maintenance. An analysis of lateral cephalometric radiography confirmed an increased maxillomandibular discrepancy with marked compensation of the anterior teeth and increased labial angulation of the implants (Figure 3F).
Figure 1. Facial photographs obtained before treatment.
Figure 2. Pretreatment photographs. A-E, Intraoral photographs obtained before treatment; F-J, pretreatment dental casts.
Figure 3. Pretreatment panoramic, periapical, and lateral cephalometric radiographs.
TREATMENT OBJECTIVES
The following objectives were established: removal of the dental implants from the central incisor area; orthodontic decompensation and FOE of the lateral incisors followed by implant placement; establishment of a Class II molar relationship on both sides where the mesiobuccal cusp of the upper first molar is anterior to the mesiobuccal groove of the lower first molar, with the mesiobuccal cusp resting between the first mandibular molars and second premolars; facial skeletal profile improvement with orthognathic surgery; and definitive prosthetic rehabilitation.
TREATMENT ALTERNATIVES
Based on clinical and radiographic examinations, we suggested two treatment plans: The first included removal of the implants, autogenous block bone graft procedure to increase the buccal bone width, lateral incisors extraction and implant placement followed by orthognathic surgery. The second included a comprehensive treatment protocol with 5 operatory stages: (1) removal of the osseointegrated implants; (2) combined orthodontic decompensation with mesial displacement and FOE of the lateral incisors in an attempt to induce soft and hard tissue formation, thus reducing the edentulous space and favoring the placement of 2 new implants without the need for bone grafting; (3) extraction of the lateral incisors and placement of 2 new implants corresponding to the central incisors, which received provisional crowns; (4) orthognathic surgery for maxillary advancement to improve occlusal and facial relationships; and finally, (5) orthodontic refinement followed by definitive prosthetic rehabilitation and reshaping of the adjacent teeth. The first plan required an extensive surgical procedure to graft removal, which imposes heavy physical burdens on the patient, while second could facilitate achievement of treatment objectives with minimum interventions and post-operative discomfort. The second treatment plan was selected by the patient and written informed consent was obtained prior to initial treatment.
TREATMENT PROGRESS
The initial stage of treatment involved removal of the osseointegrated implants and immediate placement of an upper arch fixed appliance. Initial alignment and leveling of the upper arch was commenced using 0.4 mm nickel-titanium wires; brackets were bonded to prefabricated crowns and tied to the arch wire for acceptable esthetics. During the following month, a lower arch fixed appliance (Capelozza Prescription, Standard I, 0.022 × 0.028; Abzil 3M, São José do Rio Preto, Brazil) was set and a leveling wire placed to induce protrusion.
Orthodontic therapy involved decompensation as a bridge to orthognathic surgery. Within this context, the alveolar defect was partially solved by transposition of the lateral incisors and FOE for soft and hard tissue augmentation prior to implant placement. Progressive mesial displacement reduces the upper arch perimeter, which was the goal of orthodontic decompensation of the maxillary arch. Once this goal was achieved, the molars would be in a Class II relationship with the canines taking the places of the lateral incisors, thus requiring reshaping for anatomical acceptability. In the mandible, alignment and leveling were performed to increase the protrusion of the incisors and the perimeter of the arch, deliberately worsening existing occlusal relationships to make them more consistent with the patient's facial discrepancies.
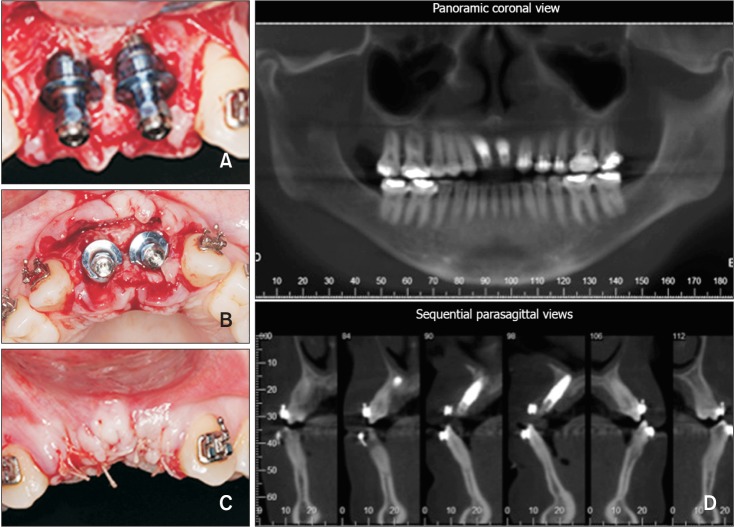
Orthodontic mesial movement of the lateral incisors was started with 0.45 mm stainless steel wire, with a consequent reduction in the upper arch perimeter. Upon completion of this process, FOE was initiated by placing step-down bends, which were gradually increased at each appointment (Figure 4). The patient was seen every 2 weeks to reduce the incisal surface of the teeth to prevent occlusal interference during extrusive movement. Endodontic treatment of both teeth was required because of extensive sensitivity during this process. Once orthodontic extrusion was complete after 12 weeks (Figure 5), a cone-beam computed tomography (CBCT) scan was acquired (Figure 6) and acceptable outcomes were achieved in the superior alveolar region with successful canine migration and appropriate prosthetic space, allowing adequate implant installation in a 3D position. At this time, the lateral incisors were extracted and 2 osseointegrated implants (3.25 × 11 mm; Biomet 3i NT, Palm Beach Gardens, FL, USA) were placed; they remained submerged during the osseointegration period (Figure 7A-C). FOE is considered a less invasive approach to restore vertical soft and hard tissues lost as a consequence of dental disease or trauma. In this case, FOE allowed immediate implant placement with sufficient implant length (11 mm); implant threads were sufficiently engaged in the remaining bone, favoring adequate primary implant stability. Because of advanced bone resorption in the buccal-palatal direction, we decided to install an implant with a narrow diameter (3.25 mm). A narrow diameter implant plays an important role in reducing the rate of vertical bone resorption at the buccal aspect of implants placed in fresh extraction sockets. After implant placement, a particulate anorganic bovine bone graft (Bio-Oss; Geistlich, Wolhusen, Switzerland) was applied to the buccal side of the alveolar crest and over the implant to increase buccal bone thickness and reduce the chances of vertical bone resorption postoperatively. CBCT showed correct positioning of the implants in relation to the remaining alveolar bone (Figure 7D).
Figure 4. A periapical radiograph obtained after mesial displacement and extrusion of the lateral incisors.
Figure 5. Intraoral photographs taken after extrusion of the lateral incisors.
Figure 6. A cone-beam computed tomography scan acquired prior to implant placement. A, Panoramic coronal view; B, sequential parasagittal views.
Figure 7. Implant installation. A-C, Intraoral photographs of implant placement; D, a cone-beam computed tomography scan acquired after implant installation.
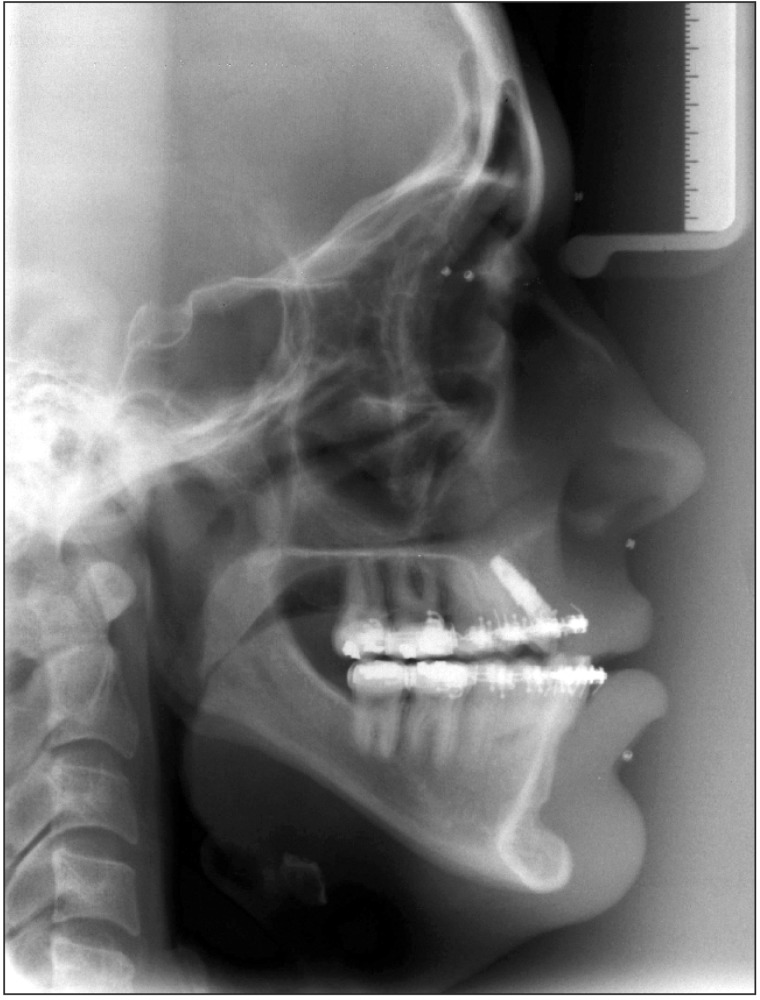
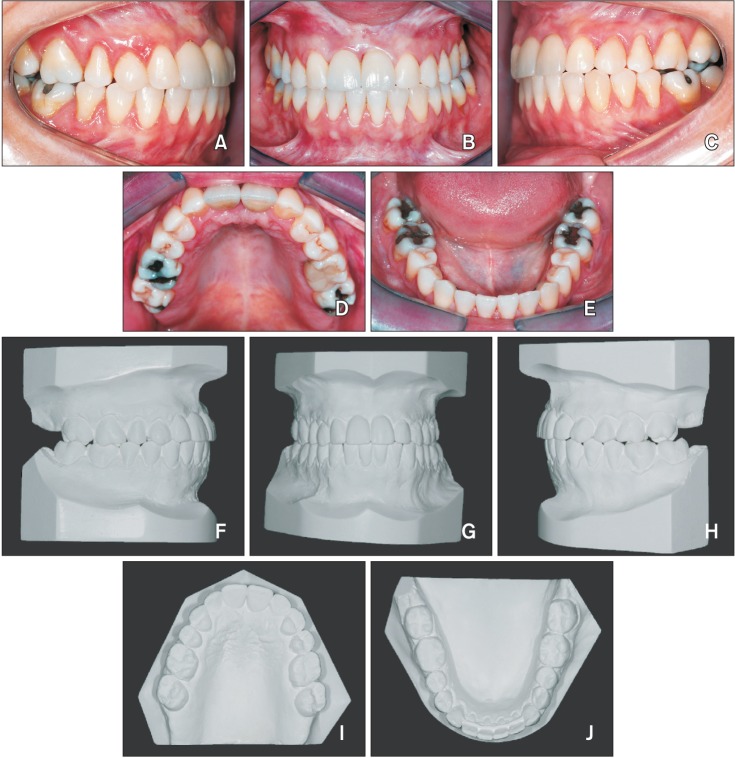
The upper and lower alignment and leveling stage was continued with up to 0.48 × 0.63 mm stainless steel wires. A dynamic analysis of diagnostic study models with the upper model in the predicted position after maxillary advancement confirmed that the patient was a candidate for orthognathic surgery (Figure 8). Preoperative lateral cephalometric radiography showed that the labial angulation of the implants was reduced, and the positions of the mandibular incisors were attenuated (Figure 9). Four months postoperatively, the implants received provisional prosthetic crowns fabricated in accordance with the arch morphology created during orthodontic decompensation until she underwent skeletal malocclusion surgery. Orthognathic surgery was performed with advancement of the maxilla to create an appropriate facial profile and occlusal relationship. After the conclusion of orthodontic treatment, final panoramic, periapical, and lateral cephalometric radiographs were obtained (Figure 10) and the wires were bent to enable good occlusal contact (Figure 11). At this time, a black triangle was present between the central incisors from interproximal bone loss, which resulted in a papillary height defect. According to Tarnow et al.,23 when the distance from the base of the contact point to the bone crest was > 6 mm, interdental papillae were usually absent.
Figure 8. The photographs taken after orthodontic decompensation. A-C, Facial photographs; D-H, intraoral photographs.
Figure 9. A lateral cephalometric radiograph obtained after orthodontic decompensation.
Figure 10. Final panoramic, periapical, and lateral cephalometric radiographs obtained after orthognathic surgery.
Figure 11. Intraoral photographs taken after orthodontic movement and finalization of the surgical procedures.
RESULTS
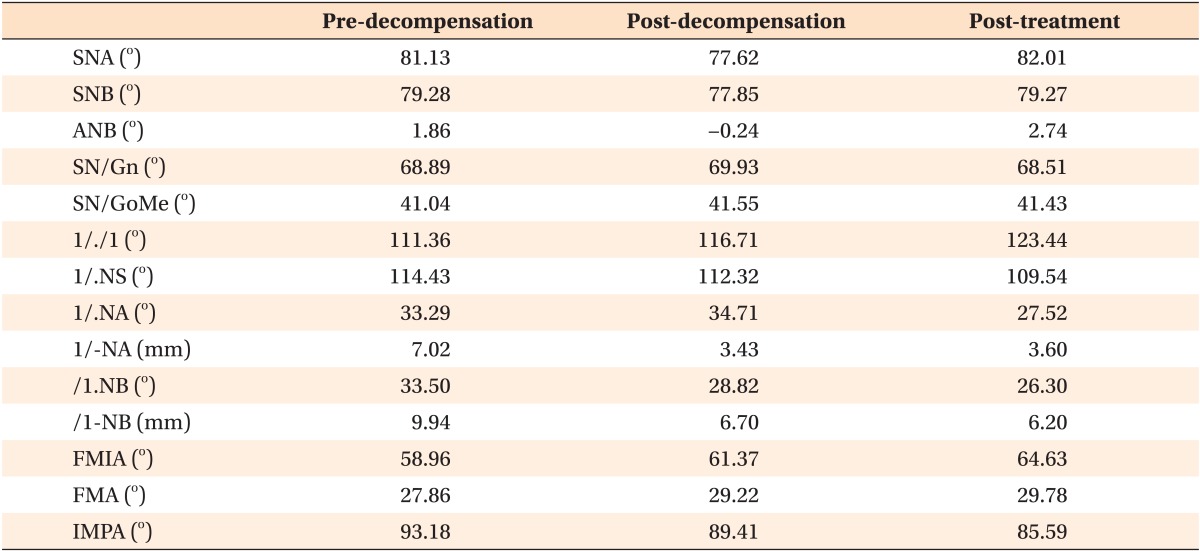
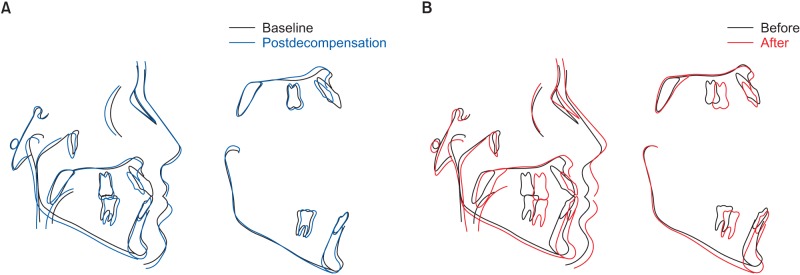
Both appliances were removed after 3 years and 8 months of treatment (the patient became pregnant, thus increasing the total treatment time). The patient underwent esthetic procedures to correct dental discrepancies i.e., reshaping of the canines into lateral incisors and the premolars into canines that occurred as a consequence of the tooth migration process (Figure 12). Another approach to improve esthetic outcomes in this case involved decreasing the distance from the prosthesis contact point close to the gingival margin to the bone crest, allowing the papilla to fill almost the entire space between the implants. At the three-year follow-up, facial and occlusal esthetic improvements were achieved with the proposed treatment and the results remained stable, meeting the functional and esthetic expectations of the patient (Figures 13 and 14). Cephalometric descriptions are shown in Table 1 for the pre-treatment phase (T1), after tooth decompensation (T2), and posttreatment (T3). In the proposed treatment, osteotomy was accomplished only in the maxilla with anterior movement and clockwise rotation without any surgical intervention in the mandible. However, rotation of the maxillary plane induced a rotation in the mandibular condyle axis, which resulted in a slight anterior movement of the mandible and concomitant alteration of the mandibular plane. Furthermore, occlusal plane alterations have much greater effects in the anteroposterior region (incisal region) than in the symphysis region, as shown in the post-treatment cephalometric tracing (Figure 15) only on the right side of the mandible. Pre- and post-treatment cephalometric tracings (Figure 15) show maxilla advancement and minimal changes in mandibular position.
Figure 12. Final photographs after orthodontic appliance removal. A-C, Facial photographs; D-H, intraoral photographs.
Figure 13. Facial photographs taken at the three-year follow-up.
Figure 14. The follow up after three years. A-E, Intraoral photographs taken three years post-treatment; F-J, final treatment dental casts.
Table 1. Cephalometric summary.
SNA, Angle between anterior cranial base (SN) and point A; SNB, angle between anterior cranial base (SN) and point B; ANB, angle between lines NA and NB; SN/Gn, angle between anterior cranial base (SN) and gnathion; SN/GoMe, angle between SN and mandibular plane (GoMe); 1/./1, angle between long axis of upper and lower incisors; 1/.NS, angle between long axis of upper incisor (1/) and anterior cranial base (SN); 1/.NA, angle between long axis of upper incisor and NA line; 1/-NA, distance between upper incisor and NA line; /1.NB, angle between long axis of lower incisor and NB line; /1-NB, distance between lower incisor and NB line; FMIA, angle between FH plane and mandibular incisor; FMA, angle between FH plane and mandibular plane; IMPA, mandibular incisor angle to mandibular plane.
Figure 15. The cephalometric superimposition. A, Pre-treatment (black line) and post-decompensation (blue line). B, Pretreatment (black line) and post-treatment (red line).
DISCUSSION
Implant-based rehabilitation of the anterior region has always been a challenge in dental practice. The esthetic and functional maintenance of implants with adjacent natural teeth can be particularly difficult.3,4,24,25 In these cases, appropriate interdisciplinary treatment planning is essential.13 The manipulation of alveolar bone defects in the esthetic zone is another of the major difficulties in implant dentistry, especially when vertical defects are present, which is a particularly common finding in adult patients who have experienced periodontal tissue losses over time.26,27
Limitations inherent to complex oral rehabilitation include high morbidity associated with reconstructive procedures such as autogenous block bone grafts and osteopromotive techniques.28 These procedures involve major surgical manipulations (including donor site surgery), numerous invasive interventions, and the need for subsequent soft tissue enhancement. Furthermore, final volumes and esthetic outcomes are often unpredictable, despite satisfactory graft progress.29,30 In this case, a vertical bone defect was associated with extensive bone resorption in the neighboring teeth, hindering bone graft placement at the original cervical level. Another aspect related to defect etiology that must be taken into account is potentially limited mesiodistal space for implant placement.
In the present case, we decided to use mesial orthodontic displacement and FOE of the lateral incisors after implant removal to appropriately augment soft and hard tissue prior to implant placement. These procedures led to the activation of angiogenic growth factors stimulated by mechanical stresses exerted in the alveolar bone that contribute to the formation of new periodontal support tissue, i.e., gingiva, periodontal fibers, and new bone deposition via osteoblastic activity, favoring implant placement in an appropriate 3D position.16,18 The only prerequisite for the adequate application of these procedures is that the apical third of the root should provide an intact fiber apparatus.31 Therefore, in an attempt to reduce the edentulous area of the incisors, displacement of the lateral incisors toward the defect and migration of the canines to take the places of the lateral incisors were performed before FOE. Moreover, due to considerable periodontal attachment loss in the lateral incisal area, FOE alone would not have provided the necessary gain in bone height in the anterior region. For this reason, we opted to increase the amount of bone by placing particulate bone graft material over the buccal bone, decreasing the amount of vertical bone resorption that occurs after implant placement.
After accomplishing these procedures, a substantial reduction in upper arch perimeter was achieved, favoring implant rehabilitation following all the necessary steps for esthetic restoration, which conserved biologic width and supported implant maintenance. This change also improved the relationship between the upper and lower arch perimeters, facilitating orthognathic surgery treatment planning. At the end of this stage, there was a significant sagittal discrepancy, which is an unquestionable indication for surgical correction in patients with a Class III skeletal pattern for improved esthetics and quality of life.32
The maxillary advancement procedure created a divergence between the maxillary and mandibular occlusal planes with intrusion of the anterior segment, which helped alveolar ridge leveling. As the skeletal discrepancy created was insignificant in relation to the patient's expectations, there was no indication for bimaxillary surgery. Once the provisional crowns were placed, we identified a lack of exposure of the maxillary incisors, which enabled clockwise rotation of the maxilla with anterior extrusion rather than posterior intrusion to correct the lip-teeth relationship. Finally, multiple coronoplasty procedures (grinding and composite resin augmentation) were required to optimize the volume and intercuspation. Finally, definitive crowns were placed one year after surgery.
CONCLUSION
In conclusion, oral rehabilitation in adult patients requires well-planned, interdisciplinary treatment to ensure better esthetic and functional outcomes. In patients with missing teeth and alveolar bone loss in the anterior region, FOE of the teeth adjacent to the edentulous space may be considered a primary treatment option to induce soft tissue and bone formation and to create more favorable bone and periodontal conditions. Changes in arch perimeter as a result of such orthodontic displacement can cause skeletal discrepancies, which in turn may require surgical correction to improve facial esthetics and the occlusal profile.
Footnotes
The authors report no commercial, proprietary, or financial interest in the products or companies described in this article.
References
- 1.de Molon RS, Avila ED, Cirelli JA, Mollo-Jr FD, Andrade MF, Barros-Filho LA, et al. A combined approach for the treatment of resorbed fresh sockets allowing immediate implant restoration. A 2-year follow-up. J Oral Implantol. 2015;41:712–718. doi: 10.1563/AAID-JOI-D-13-00140. [DOI] [PubMed] [Google Scholar]
- 2.Choquet V, Hermans M, Adriaenssens P, Daelemans P, Tarnow DP, Malevez C. Clinical and radiographic evaluation of the papilla level adjacent to single-tooth dental implants. A retrospective study in the maxillary anterior region. J Periodontol. 2001;72:1364–1371. doi: 10.1902/jop.2001.72.10.1364. [DOI] [PubMed] [Google Scholar]
- 3.Kan JY, Rungcharassaeng K. Interimplant papilla preservation in the esthetic zone: a report of six consecutive cases. Int J Periodontics Restorative Dent. 2003;23:249–259. [PubMed] [Google Scholar]
- 4.Belser UC, Schmid B, Higginbottom F, Buser D. Outcome analysis of implant restorations located in the anterior maxilla: a review of the recent literature. Int J Oral Maxillofac Implants. 2004;19(Suppl):30–42. [PubMed] [Google Scholar]
- 5.Spear FM, Kokich VG, Mathews DP. Interdisciplinary management of anterior dental esthetics. J Am Dent Assoc. 2006;137:160–169. doi: 10.14219/jada.archive.2006.0140. [DOI] [PubMed] [Google Scholar]
- 6.de Molon RS, Morais-Camilo JA, Verzola MH, Faeda RS, Pepato MT, Marcantonio E., Jr Impact of diabetes mellitus and metabolic control on bone healing around osseointegrated implants: removal torque and histomorphometric analysis in rats. Clin Oral Implants Res. 2013;24:831–837. doi: 10.1111/j.1600-0501.2012.02467.x. [DOI] [PubMed] [Google Scholar]
- 7.de Molon RS, de Avila ED, Cirelli JA, Cardoso Mde A, Capelozza-Filho L, Borelli Barros LA. Optimizing maxillary aesthetics of a severe compromised tooth through orthodontic movement and dental implants. Case Rep Dent. 2014;2014:103808. doi: 10.1155/2014/103808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Avila ÉD, de Molon RS, de Assis Mollo F, Jr, de Barros LA, Capelozza Filho L, de Almeida Cardoso M, et al. Multidisciplinary approach for the aesthetic treatment of maxillary lateral incisors agenesis: thinking about implants? Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114:e22–e28. doi: 10.1016/j.oooo.2011.09.023. [DOI] [PubMed] [Google Scholar]
- 9.de Molon RS, de Avila ED, de Barros-Filho LA, Ricci WA, Tetradis S, Cirelli JA, et al. Reconstruction of the alveolar buccal bone plate in compromised fresh socket after immediate implant placement followed by immediate provisionalization. J Esthet Restor Dent. 2015;27:122–135. doi: 10.1111/jerd.12154. [DOI] [PubMed] [Google Scholar]
- 10.Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004;19(Suppl):43–61. [PubMed] [Google Scholar]
- 11.Fürhauser R, Florescu D, Benesch T, Haas R, Mailath G, Watzek G. Evaluation of soft tissue around single-tooth implant crowns: the pink esthetic score. Clin Oral Implants Res. 2005;16:639–644. doi: 10.1111/j.1600-0501.2005.01193.x. [DOI] [PubMed] [Google Scholar]
- 12.Jung RE, Pjetursson BE, Glauser R, Zembic A, Zwahlen M, Lang NP. A systematic review of the 5-year survival and complication rates of implant-supported single crowns. Clin Oral Implants Res. 2008;19:119–130. doi: 10.1111/j.1600-0501.2007.01453.x. [DOI] [PubMed] [Google Scholar]
- 13.Kan JY, Rungcharassaeng K, Fillman M, Caruso J. Tissue architecture modification for anterior implant esthetics: an interdisciplinary approach. Eur J Esthet Dent. 2009;4:104–117. [PubMed] [Google Scholar]
- 14.Nisapakultorn K, Suphanantachat S, Silkosessak O, Rattanamongkolgul S. Factors affecting soft tissue level around anterior maxillary single-tooth implants. Clin Oral Implants Res. 2010;21:662–670. doi: 10.1111/j.1600-0501.2009.01887.x. [DOI] [PubMed] [Google Scholar]
- 15.Papalexiou V, Novaes AB, Jr, Ribeiro RF, Muglia V, Oliveira RR. Influence of the interimplant distance on crestal bone resorption and bone density: a histomorphometric study in dogs. J Periodontol. 2006;77:614–621. doi: 10.1902/jop.2006.050172. [DOI] [PubMed] [Google Scholar]
- 16.de Barros LA, de Almeida Cardoso M, de Avila ED, de Molon RS, Siqueira DF, Mollo-Junior Fde A, et al. Six-year follow-up of maxillary anterior rehabilitation with forced orthodontic extrusion: achieving esthetic excellence with a multidisciplinary approach. Am J Orthod Dentofacial Orthop. 2013;144:607–615. doi: 10.1016/j.ajodo.2012.10.027. [DOI] [PubMed] [Google Scholar]
- 17.de Molon RS, de Avila ÉD, de Souza JA, Nogueira AV, Cirelli CC, Cirelli JA. Combination of orthodontic movement and periodontal therapy for full root coverage in a Miller class III recession: a case report with 12 years of follow-up. Braz Dent J. 2012;23:758–763. doi: 10.1590/s0103-64402012000600022. [DOI] [PubMed] [Google Scholar]
- 18.de Molon RS, de Avila ED, de Souza JA, Nogueira AV, Cirelli CC, Margonar R, et al. Forced orthodontic eruption for augmentation of soft and hard tissue prior to implant placement. Contemp Clin Dent. 2013;4:243–247. doi: 10.4103/0976-237X.114876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de Molon RS, Kim YJ, Dos Santos-Pinto A, Cirelli JA. Improvement of an anterior infrabone defect using combined periodontal and orthodontic therapy: A 6-year follow-up case report. Eur J Dent. 2014;8:407–411. doi: 10.4103/1305-7456.137657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Corrente G, Abundo R, Re S, Cardaropoli D, Cardaropoli G. Orthodontic movement into infrabony defects in patients with advanced periodontal disease: a clinical and radiological study. J Periodontol. 2003;74:1104–1109. doi: 10.1902/jop.2003.74.8.1104. [DOI] [PubMed] [Google Scholar]
- 21.Korayem M, Flores-Mir C, Nassar U, Olfert K. Implant site development by orthodontic extrusion. A systematic review. Angle Orthod. 2008;78:752–760. doi: 10.2319/0003-3219(2008)078[0752:ISDBOE]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 22.Sonego CL, Bobrowski ÂN, Chagas OL, Jr, Torriani MA. Aesthetic and functional implications following rotation of the maxillomandibular complex in orthognathic surgery: a systematic review. Int J Oral Maxillofac Surg. 2014;43:40–45. doi: 10.1016/j.ijom.2013.07.738. [DOI] [PubMed] [Google Scholar]
- 23.Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992;63:995–996. doi: 10.1902/jop.1992.63.12.995. [DOI] [PubMed] [Google Scholar]
- 24.Funato A, Salama MA, Ishikawa T, Garber DA, Salama H. Timing, positioning, and sequential staging in esthetic implant therapy: a four-dimensional perspective. Int J Periodontics Restorative Dent. 2007;27:313–323. [PubMed] [Google Scholar]
- 25.Garber DA, Belser UC. Restoration-driven implant placement with restoration-generated site development. Compend Contin Educ Dent. 1995;16:796, 798–802, 804. [PubMed] [Google Scholar]
- 26.Palacci P. Aesthetic treatment of the anterior maxilla: soft and hard tissue considerations. Oral Maxillofac Surg Clin North Am. 2004;16:127–137. doi: 10.1016/j.coms.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 27.Seibert JS, Salama H. Alveolar ridge preservation and reconstruction. Periodontol 2000. 1996;11:69–84. doi: 10.1111/j.1600-0757.1996.tb00185.x. [DOI] [PubMed] [Google Scholar]
- 28.Margonar R, Queiroz TP, Marcantonio É, Luvizuto ER, Faloni AP, Betoni W, Jr, et al. Rehabilitation of the maxillary arch after bone graft using immediate loading with implant-supported fixed restoration. J Craniofac Surg. 2014;25:e44–e48. doi: 10.1097/SCS.0b013e3182a2ee9a. [DOI] [PubMed] [Google Scholar]
- 29.Milinkovic I, Cordaro L. Are there specific indications for the different alveolar bone augmentation procedures for implant placement? A systematic review. Int J Oral Maxillofac Surg. 2014;43:606–625. doi: 10.1016/j.ijom.2013.12.004. [DOI] [PubMed] [Google Scholar]
- 30.Margonar R, Queiroz TP, Luvizuto ER, Santos PL, Wady AF, Paleari AG. Anterior tooth rehabilitation with frozen homogenous bone graft and immediately loaded titanium implant using computer-guided surgery. J Craniofac Surg. 2012;23:e470–e472. doi: 10.1097/SCS.0b013e3182587516. [DOI] [PubMed] [Google Scholar]
- 31.Shiu YT, Weiss JA, Hoying JB, Iwamoto MN, Joung IS, Quam CT. The role of mechanical stresses in angiogenesis. Crit Rev Biomed Eng. 2005;33:431–510. doi: 10.1615/critrevbiomedeng.v33.i5.10. [DOI] [PubMed] [Google Scholar]
- 32.de Ávila ED, de Molon RS, Loffredo LC, Massucato EM, Hochuli-Vieira E. Health-related quality of life and depression in patients with dentofacial deformity. Oral Maxillofac Surg. 2013;17:187–191. doi: 10.1007/s10006-012-0338-5. [DOI] [PubMed] [Google Scholar]