Abstract
The vasoconstrictive effect due to the addition of epinephrine to local anesthetic has been clearly shown by measuring blood-flow volume or blood anesthetic concentration in oral mucosal tissue. However, there are no reports on the measurement of anesthetic concentration using samples directly taken from the jawbone and oral mucosal tissue. Consequently, in this study, the effect of lidocaine concentration in the jawbone and oral mucosal tissue by the addition of epinephrine to the local anesthetic lidocaine was considered by quantitatively measuring lidocaine concentration within the tissue. Japanese white male rabbits (n = 96) were used as test animals. General anesthesia was induced by sevoflurane and oxygen, and then cannulation to the femoral artery was performed while arterial pressure was constantly recorded. Infiltration anesthesia was achieved by 0.5 mL of 2% lidocaine containing 1 : 80,000 epinephrine in the upper jawbone (E+) and 0.5 mL of 2% of epinephrine additive–free lidocaine (E0) under the periosteum. At specified time increments (10, 20, 30, 40, 50, and 60 minutes), samples from the jawbone, oral mucosa, and blood were collected, and lidocaine concentration was directly measured by high-performance liquid chromatography. No significant differences in the change in blood pressure were observed either in E+ or E0. In both E+ and E0 groups, the serum lidocaine concentration peaked 10 minutes after local anesthesia and decreased thereafter. At all time increments, serum lidocaine concentration in E+ was significantly lower than that in E0. There were no significant differences in measured lidocaine concentration between jawbone and mucosa within either the E+ or the E0 groups at all time points, although the E0 group had significantly lower jawbone and mucosa concentrations than the E+ group at all time points when comparing the 2 groups to each other. Addition of epinephrine to the local anesthetic inhibited systemic absorption of local anesthetic into the blood such that a high concentration could be maintained in the tissue. Epinephrine-induced vasoconstrictive effect was observed not only in the oral mucosa but also in the jawbone.
Key Words: Lidocaine concentration, Jawbone, Epinephrine, Infiltration anesthesia, Rabbit
During dental and oral surgery, a significant local anesthetic effect is needed, as not only do the soft tissues require surgery, but also the hard tissue such as jawbones because of surgical interventions. In current clinical dentistry practice, vasoconstrictive agents such as epinephrine are commonly added to local anesthetics to inhibit bleeding from the surgical site and to enhance local anesthetic efficacy by delaying absorption of the local anesthetic into the blood and thus prolonging activity.1–5 Currently, the vasoconstrictor effect due to the addition of epinephrine to local anesthetic has been sufficiently confirmed. In most reports, however, anesthetic concentration in tissue was indirectly considered by measuring blood-flow volume or serum anesthetic concentration.1,6–11 In regard to the vasoconstrictive effect in bone due to the addition of epinephrine, only a few reports using methods such as electrodialytical hydrogen clearance and radioisotope measurement have been published,12–14 and no reported studies have directly measured lidocaine concentration using samples directly taken from the jawbone. Consequently, in this study, we studied the effect of lidocaine concentration in the jawbone and oral mucosal tissue by the addition of epinephrine to the local anesthetic lidocaine, by quantitatively determining lidocaine concentration directly in tissue.
METHODS
Animals
Ninety-six Japanese white rabbits (body weight: 2.65 ± 0.3 kg, 16 weeks of age, male) (Nippon Bio-Supp Center, Tokyo, Japan) were used. The animals were kept in a controlled animal room at 23°C and 60% humidity, and given free access to feed pellets (MF, Oriental Yeast, Tokyo, Japan) and drinking water (tap water) until the experimental day. This study was performed in accordance with the Animal Experiment Regulations of Ohu University (Permit No. 2013-49, 2014-29).
General Anesthesia and Experimental Model
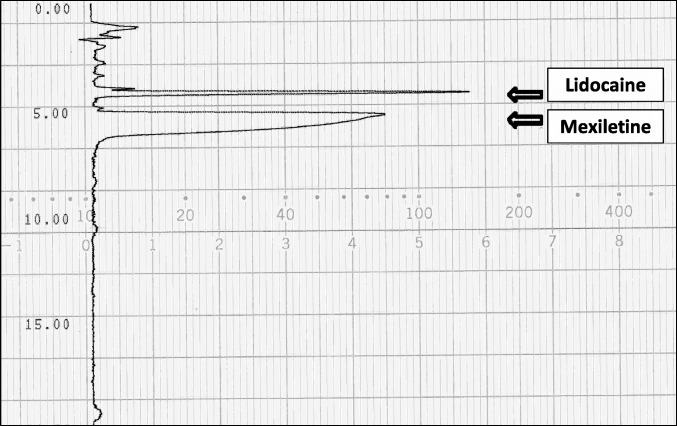
General anesthesia was induced with 5% sevoflurane and oxygen 5 L/min was administered using anesthesia equipment for small animals (Soft Lander, Shin-Ei Industries, Tokyo, Japan). A tracheotomy was performed while general anesthesia was maintained by 3% sevoflurane and oxygen 3 L/min. Cannulation of the femoral artery was performed, and arterial pressure was constantly recorded during the experiment using a polygraph (Sanei Sokki, Tokyo, Japan) and a pressure transducer (Nihon Kohden, Tokyo, Japan) (Figure 1).
Figure 1. .
Method of general anesthesia. General anesthesia was induced by oxygen 5 L/min and 5% sevoflurane, and then a tracheotomy was performed, after which general anesthesia was maintained at oxygen 3 L/min and 3% sevoflurane. A cannula was inserted into the femoral artery, and arterial pressure was continuously recorded throughout the experiment using a polygraph and a pressure transducer.
Infiltration Anesthetic Injection and Excision of the Tissue
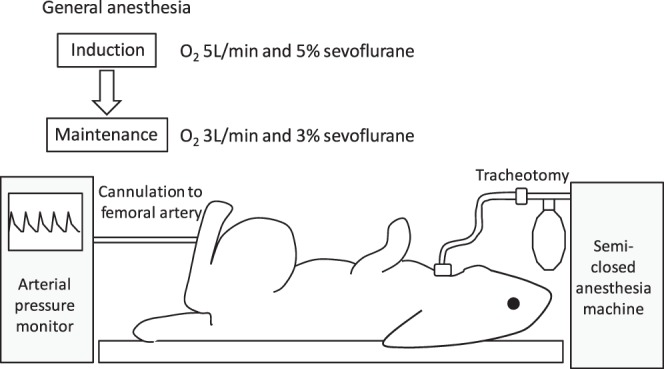
Under general anesthesia, a quantitative syringe (Cartri-Ace, Dentronics, Tokyo, Japan) with an injection needle (27 G, 0.40 × 19) (Terumo Needle, Terumo, Tokyo, Japan) was used to administer 0.5 mL of 2% of lidocaine containing 1 : 80,000 epinephrine (dental xylocaine cartridge containing 1 : 80,000 epinephrine, Dentsply Sankin, Tokyo, Japan) or 0.5 mL of 2% of epinephrine additive-free lidocaine (xylocaine injection polyamp 2%, Astra Zeneca, Tokyo, Japan) into the right maxillae for 40 seconds. The injection site was the right buccal side of the third molar (Figure 2). Subperiosteal infiltration anesthesia was performed by inserting the needle tip to the jawbone surface beneath the periosteum.
Figure 2. .
Location of infiltration anesthesia: 0.5 mL of 2% of lidocaine containing 1 : 80,000 epinephrine or 0.5 mL of 2% of epinephrine additive-free lidocaine was infused into the right maxillae for 20 seconds. Injection site was the buccal side of the third molar on both sides (white arrow). Subperiosteal infiltration anesthesia was performed by touching the needle tip to the jawbone surface under the periosteum.
Excision of the periosteum was carried out at specific time increments (10, 20, 30, 40, 50, and 60 minutes following local anesthetic injection). Excision of approximately 1 g of the injected site area of the maxilla and adjacent mucosa regions (from the apical area of third molar to the infrazygomatic crest) was carried out using rongeur forceps and the samples were stored at −80°C.
Measurement of the Mean Arterial Pressure Before and After Local Anesthesia Injection
Even under general anesthesia, pain stimuli will affect arterial pressure,15 and changes in pressure can be reflected by a polygraph. From polygraphic arterial pressure data, one-third pulse pressure + diastolic arterial pressure was calculated as the mean arterial pressure, and changes in arterial pressure were assessed 10 and 20 seconds after infiltration anesthesia of 2% lidocaine with or without 1 : 80,000 epinephrine to assess mean arterial pressure changes due to injection pain.
Measurement of the Serum Lidocaine Concentration
After local anesthesia injection, 3 mL of arterial blood was collected from the femoral artery at specific time intervals (10, 20, 30, 40, 50, and 60 minutes). The blood samples were centrifuged, and serum lidocaine concentration was measured by the enzyme multiplied immunoassay technique.16–18
Measurement of Tissue Lidocaine Level
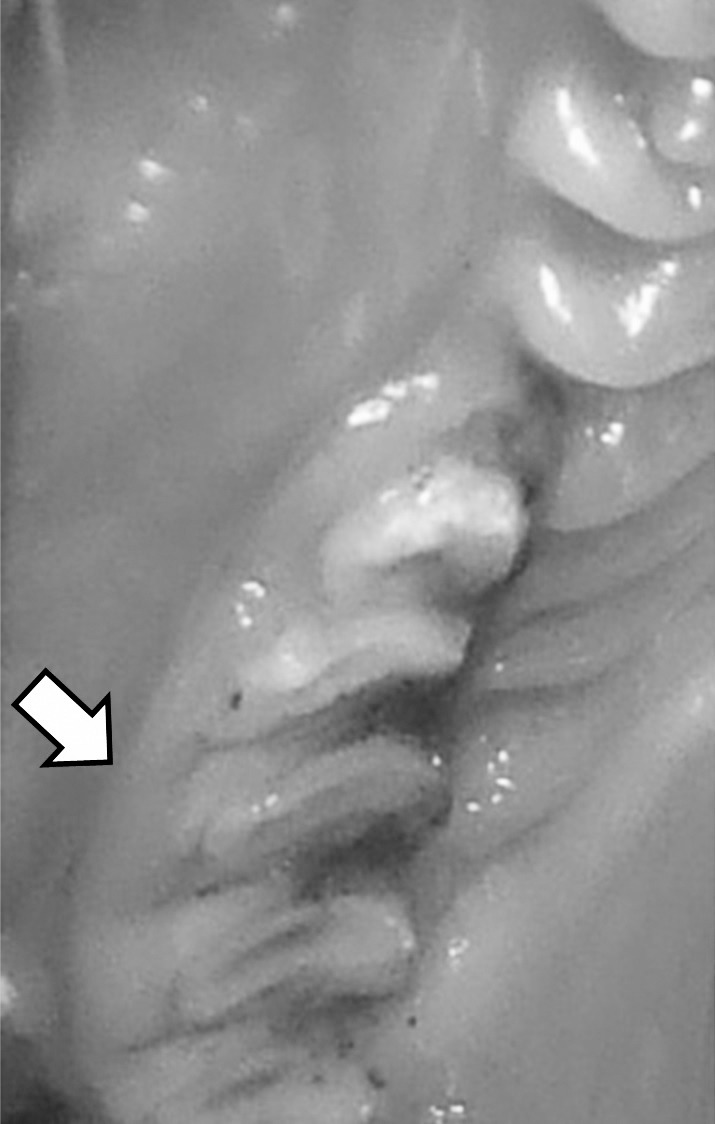
Frozen bone and mucosa samples were ground using a bone mill (TK-CM20S, Tokken, Tokyo, Japan), suspended with 0.01 M boric acid at pH 9.18, and homogenized for 2 minutes using a homogenizer (Polytron PT2100, Kinematica, Luzern, Switzerland). The supernatant (0.5 mL) was combined with 100 μL mexiletine (10 μg/mL) and then 5 mL of chloroform : methanol (8 : 2) was added. After mixing, the solution was centrifuged at 3000 rpm (1000g) for 10 minutes. Three milliliters of the organic layer was collected and dried under reduced pressure at 40°C for 60 minutes using a rotary evaporator (Eyela, Tokyo Rikakikai, Tokyo, Japan). The sample was then dissolved in 250 μL of the mobile phase (50 mM KH2PO4 : CH3CN = 4 : 1), mixed using a mixer, and then filtered. Lidocaine concentration levels were measured by high-performance liquid chromatography (HPLC) (Jasco PU-2080 Plus, JASCO, Tokyo, Japan), according to the method reported by Piwowarska et al.19 HPLC conditions detailed in the report of Morota et al20 are shown in the Table. Typical chromatograms of lidocaine from rabbit bone and mucosa samples are shown in Figure 3. Tissue lidocaine data were converted to lidocaine concentration level per gram tissue.
Conditions for HPLC Analysis of Lidocaine*
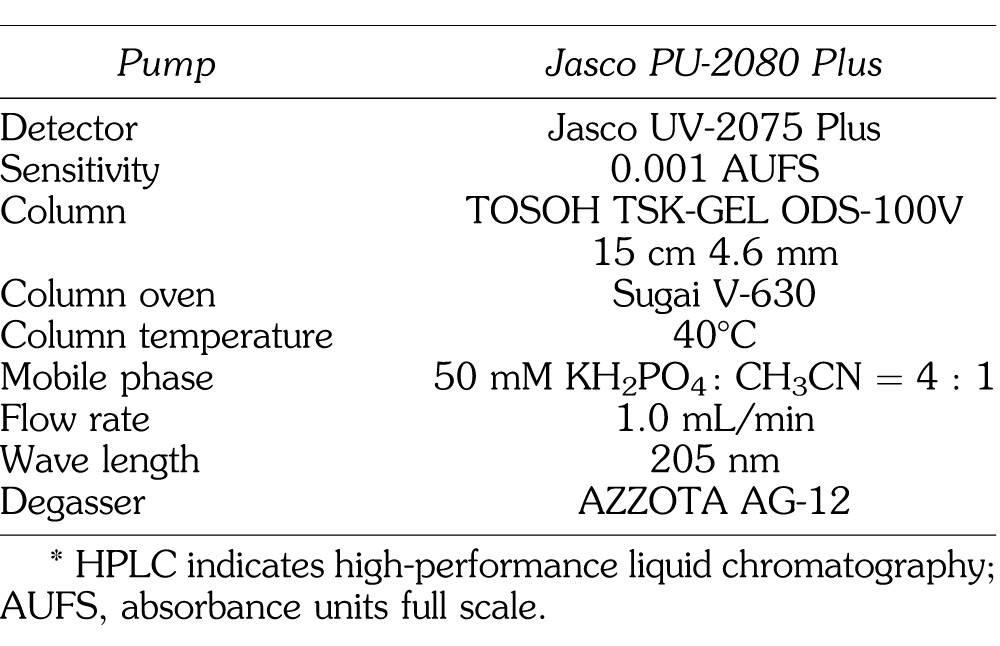
Figure 3. .
Chromatogram of lidocaine concentration from oral mucosa in rabbit in one case.
Statistical Comparison of Data
Mean arterial pressure, serum lidocaine concentration, and lidocaine concentration in tissue of the epinephrine addition group (E+) and the epinephrine additive–free group (E0) were compared. Lidocaine concentration in jawbone tissue and oral mucosa were also compared. For statistical analysis, comparison within a group was performed by Friedman's test and comparison between groups by Mann-Whitney U test. Statistical significance was set at P < .05. Most data in this study did not indicate normal distributions. Therefore, nonparametric statistical analysis was used in this study.
RESULTS
Variation in Mean Arterial Pressure by Local Anesthetic Injection
Mean arterial pressure of the E+ group was 78.0 ± 15.4 mm Hg prior to local anesthetic injection. The obtained value was 71.3 ± 15.4 mm Hg 10 seconds after injection and 81.1 ± 16.2 mm Hg at 20 seconds. No significant difference was observed. Mean arterial pressure of the E0 group was 77.1 ± 15.0 mm Hg prior to local anesthetic injection. The obtained value was 76.8 ± 14.7 mm Hg 10 seconds after injection and 75.2 ± 15.3 mm Hg at 20 seconds. No significant difference was observed (Figure 4).
Figure 4. .
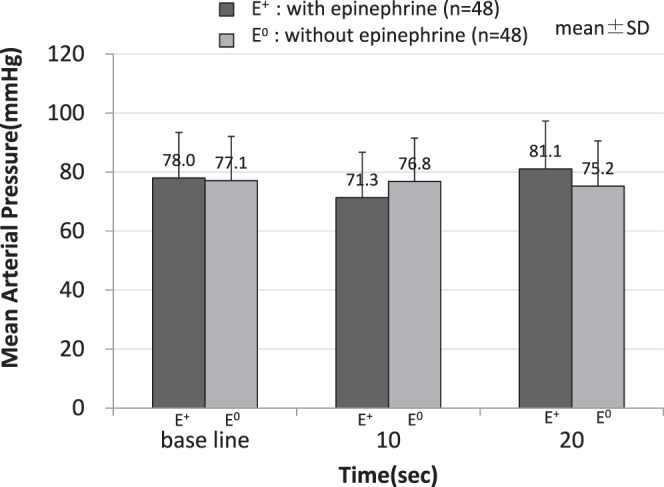
Change of mean arterial pressure before and after infiltration anesthesia. No significant difference was observed.
Serum Lidocaine Concentration
Peak serum lidocaine concentration obtained 10 minutes after local anesthetic injection of the E+ group was 0.96 ± 0.17 μg/mL. Concentration decreased over time at each time interval after injection as follows: 0.83 ± 0.14 μg/mL (20 minutes), 0.71 ± 0.13 μg/mL (30 minutes), 0.69 ± 0.13 μg/mL (40 minutes), 0.61 ± 0.12 μg/mL (50 minutes), and 0.48 ± 0.13 μg/mL (60 minutes). Peak serum lidocaine concentration obtained 10 minutes after local anesthetic injection of the E0 group was 1.97 ± 0.40 μg/mL. Concentration decreased over time at each time interval after injection as follows: 1.36 ± 0.16 μg/mL (20 minutes), 1.07 ± 0.20 μg/mL (30 minutes), 0.97 ± 0.15 μg/mL (40 minutes), 0.83 ± 0.17 μg/mL (50 minutes), and 0.66 ± 0.16 μg/mL (60 minutes). At all time intervals, serum lidocaine concentration of the E+ group was significantly lower than that for the E0 group.
Blood lidocaine concentration decreased gradually for the E+ group, whereas more rapid decrease was observed for the E0 group after the 10-minute interval. Differences between the 2 groups gradually decreased (Figure 5).
Figure 5. .
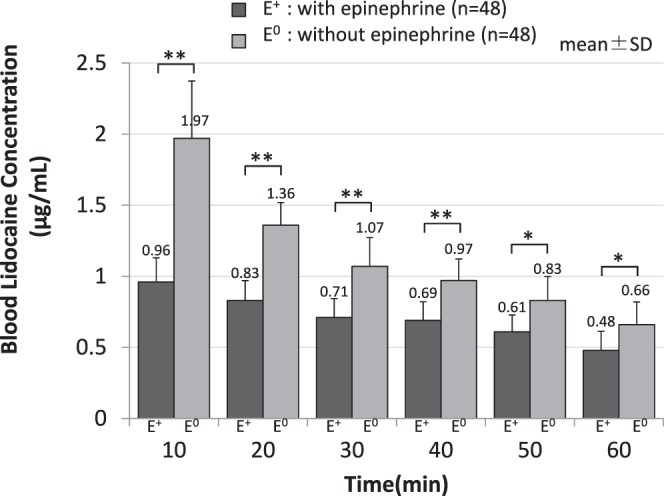
Change of blood lidocaine concentration after infiltration anesthesia. At all time points, blood lidocaine concentration in epinephrine addition group (E+) was significantly lower than that in epinephrine additive–free group (E0). ** P < .01 E+ versus E0. * P < .05 E+ versus E0.
Lidocaine Concentration in Tissue
Peak lidocaine concentration obtained 10 minutes after local anesthetic injection in the jawbone of the E+ group was 341.9 ± 154.5 μg/g. Concentration decreased over time at each time interval after injection as follows: 277.6 ± 121.4 μg/g (20 minutes), 235.6 ± 97.9 μg/g (30 minutes), 163.8 ± 72.2 μg/g (40 minutes), 142.4 ± 9.8 μg/g (50 minutes), and 71.5 ± 39.9 μg/g (60 minutes). Peak lidocaine concentration obtained 10 minutes after local anesthetic injection in jawbone of the E0 group was 114.5 ± 73.3 μg/g. Concentration decreased over time at each time interval after injection as follows: 83.5 ± 59.6 μg/g (20 minutes), 51.3 ± 26.2 μg/g (30 minutes), 26.6 ± 19.3 μg/g (40 minutes), 22.6 ± 18.6 μg/g (50 minutes), and 13.4 ± 14.6 μg/g (60 minutes). At all time intervals, lidocaine concentration in jawbone of the E+ group was significantly higher than that for the E0 group (Figure 6).
Figure 6. .
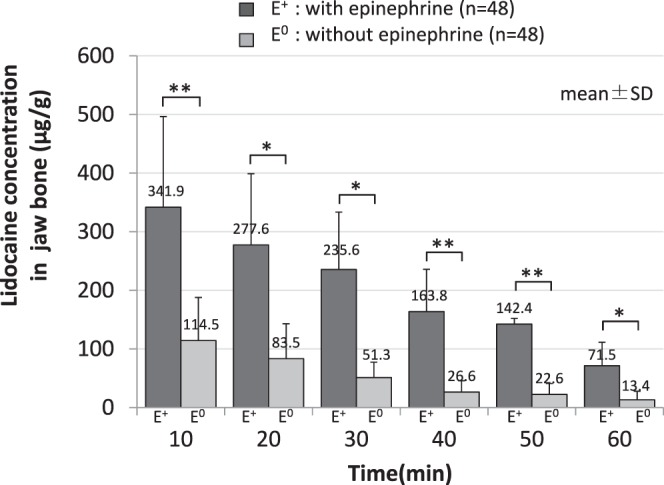
Change of lidocaine concentration in jawbone after infiltration anesthesia. At all time points, lidocaine concentration in jawbone in epinephrine addition group (E+) was significantly higher than that in epinephrine additive–free group (E0). ** P < .01 E+ versus E0. * P < .05 E+ versus E0.
Peak lidocaine concentration obtained 10 minutes after local anesthetic injection in oral mucosa of the E+ group was 358.3 ± 111.5 μg/g. Concentration decreased over time at each time interval after injection as follows: 303.5 ± 111.8 μg/g (20 minutes), 273.1 ± 124.8 μg/g (30 minutes), 194.1 ± 65.4 μg/g (40 minutes), 149.9 ± 28.1 μg/g (50 minutes), and 118.3 ± 46.0 μg/g (60 minutes). Peak lidocaine concentration obtained 10 minutes after local anesthetic injection in oral mucosa of the E0 group was 155.9 ± 128.0 μg/g. Concentration decreased over time at each time interval after injection as follows: 81.0 ± 75.5 μg/g (20 minutes), 31.9 ± 19.3 μg/g (30 minutes), 15.0 ± 13.3 μg/g (40 minutes), 15.9 ± 18.3 μg/g (50 minutes), and 4.6 ± 4.4 μg/g (60 minutes). At all time intervals, lidocaine concentration in oral mucosa of the E+ group was significantly higher than that for the E0 group (Figure 7).
Figure 7. .
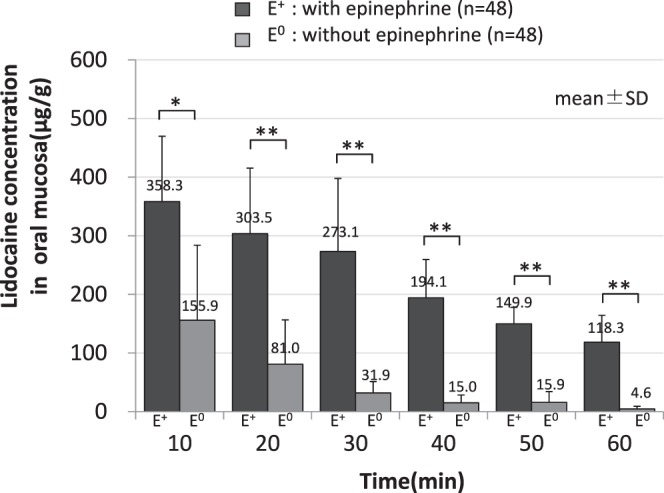
Change of lidocaine concentration in oral mucosa after infiltration anesthesia. At all time points, lidocaine concentration in oral mucosa in epinephrine addition group (E+) was significantly higher than that in epinephrine additive–free group (E0). ** P < .01 E+ versus E0. * P < .05 E+ versus E0.
Lidocaine concentration in jawbone of the E+ group was lower than that in oral mucosa at all time intervals, but no significant difference was observed between the concentration values of both groups (Figure 8). However, lidocaine concentration in jawbone of the E0 group was lower than that in oral mucosa only at the 10-minute time interval. Afterwards, values reversed, and no significant difference was observed between the concentration values in jawbone or oral mucosa for both groups (Figure 9).
Figure 8. .
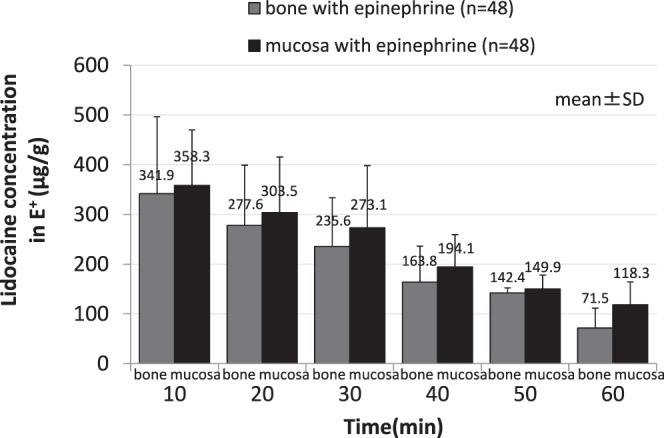
Change of lidocaine concentration in jawbone and oral mucosa in epinephrine addition group after infiltration anesthesia. Lidocaine concentration in jawbone was lower than that in oral mucosa at all time points, and no significant difference was observed between the concentration values of both groups.
Figure 9. .
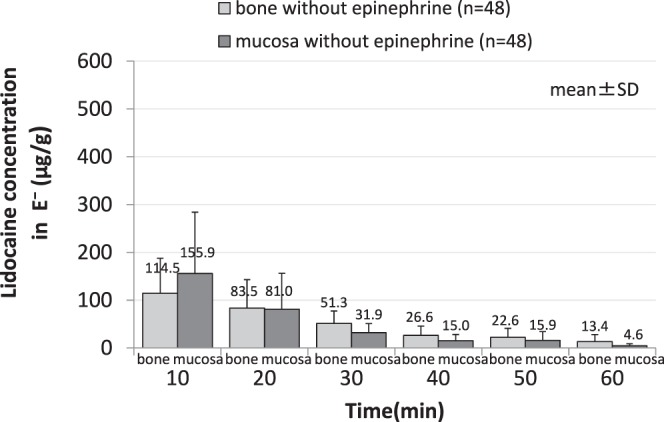
Change of lidocaine concentration in jawbone and oral mucosa in epinephrine additive–free group after infiltration anesthesia. Lidocaine concentration in jawbone was lower than that in oral mucosa only at the 10-minute time point. Values thereafter were reversed, and no significant difference was observed between the 2 concentration values of both groups.
DISCUSSION
Change in Mean Arterial Pressure by Local Anesthetic Injection
No significant difference in change in mean arterial pressure immediately after local anesthetic injection was observed in either the E+ group or the E0 group. Ichinohe et al21 reported that epinephrine increased cardiac output and decreased total peripheral vascular resistance. It has also been reported that 1 or 2 cartridges of 2% lidocaine with 1 : 80,000 epinephrine did not increase blood pressure in healthy adults.21 Troullos et al22 reported that local anesthesia with 8 cartridges of epinephrine-containing lidocaine in healthy adults increased heart rate and systolic blood pressure. Also, Yamatsuta et al23 reported on the influence of epinephrine on the peripheral circulation of rabbits administered 0.2 mL of 1 : 100,000 to 1 : 500,000 epinephrine showing no influence on respiration or circulation. Morota et al20 reported that intense pain or epinephrine overdose resulted in significant change in blood pressure. In this study, rabbits were injected with 0.5 mL of 1 : 80,000 epinephrine-containing lidocaine, and no significant change in mean arterial pressure was observed after injection. From this, the amount of epinephrine used in this study was considered clinically appropriate. However, although not significant, a temporary decrease in mean arterial pressure was observed in the E+ group after local anesthetic injection. As reported by Ichinohe et al,21 this is considered to occur because of β2-adrenergic action, which causes a temporary decrease in peripheral vascular resistance along with a decrease in mean arterial pressure, and α-adrenergic action, which is expressed in peripheral arteries immediately after the decrease with an increase in mean arterial pressure up to the value prior to injection.
Serum Lidocaine Concentration
At all time intervals, serum lidocaine concentration in the E+ group was significantly lower than that in the E0 group. Ito10 reported that a significantly higher serum lidocaine concentration was observed with injection of plain lidocaine compared to epinephrine-containing lidocaine. Moreover, time to reach maximum concentration was also found to be longer for epinephrine-containing lidocaine, and absorption tended to occur at almost the same rate in both groups after the 60-minute time interval. In this study, although maximum concentration was observed at the same time in both groups, serum lidocaine concentration in the E+ group was significantly lower than that in the E0 group at all time intervals, and the significant difference decreased only after the 50-minute time interval. From the above results, inhibition of lidocaine migration from tissue to blood vessel due to the vasoconstrictor effect of epinephrine was demonstrated.
Lidocaine Concentration in Tissue
Many studies on the vasoconstrictor effect due to the addition of epinephrine to local anesthetics have been reported. Most, however, consider concentration in tissue indirectly by measuring blood-flow volume or serum lidocaine concentration.10,11 In addition, there are no reports that directly measure local anesthetic concentration in tissue. Yasuda et al13 conducted quantitative analysis by autoradiography, using radioisotope 14C-labeled lidocaine. According to the report, lidocaine rapidly dissipated from tissue when administered alone, but with the addition of epinephrine, lidocaine concentration was better maintained in the injected areas. A high concentration was also observed in the adjacent tissue. However, depending on the radioisotope mixture, diffusion and dissipation rate varied from that of the original drug. In this study, lidocaine concentration in tissue could be measured directly by the amount of lidocaine extracted from tissue using the HPLC method. Vasoconstrictor effect by epinephrine could also be confirmed by measuring the actual concentration in tissue. Similar to the report by Yasuda et al,13 significantly lower lidocaine concentrations in both jawbone and oral mucosal tissue were observed in the E0 group in this study as well. This is reportedly due to the vasodilator effect of lidocaine,24 enhancing rapid absorption into blood vessels and the systemic circulation. This study also indicated such an occurrence. Local blood-flow volume decreases and lidocaine absorption is assumed to be inhibited because of the vasoconstrictor effects of epinephrine, and this results in a significantly higher lidocaine concentration in tissue.
Regarding cortical bone, Ogawa et al25 reported that more time is required for local anesthetics to reach into bone with infiltration injection. Local anesthetic injected beneath the periosteum infiltrates into jawbone through the cortical bone until reaching the bone marrow, and is then absorbed into capillaries over time.26 Because the insertion site in this study is beneath the periosteum and more lidocaine infiltrates into the mucosa than through the cortical bone, a significantly lower lidocaine concentration value in the jawbone was expected. Although no significant difference was observed, interesting results were obtained. Lidocaine concentration in the jawbone in the E+ group was lower than that in the oral mucosa for all time intervals. However, lidocaine concentration in the jawbone in the E0 group was lower than that in oral mucosa only at the 10-minute time interval. After that point in time, values reversed. It has been reported that a large amount of local anesthetic is rapidly absorbed into tissues with large blood flow.1 Therefore, lidocaine concentration was expected to rapidly decrease in mucosa rich in blood vessels, and the concentration in the jawbone would decrease more gradually. Although the vasoconstrictor effect of epinephrine was observed in both the jawbone and oral mucosa, it has been observed that the vasoconstrictor effect was slightly weaker in the jawbone than in the mucosa because blood flow in the jawbone is lower than in the mucosa.27 In Japan, 1 : 80,000 epinephrine is the most commonly used concentration in dental procedures. Therefore, we used 2% lidocaine with 1 : 80,000 epinephrine in this study. However, a concentration of 1 : 100,000 or 1 : 200,000 epinephrine with local anesthetics is often used in other countries. In addition, use of concentrations greater than 1 : 200,000 has been suggested for routine dentistry.28 Consequently, if a concentration of 1 : 100,000 or 1 : 200,000 epinephrine was used for this study, observation of a similar tendency as that shown in our results is presumed.
Future tasks include further clarification of evidence of the vasoconstrictor effect of epinephrine in jawbone by measuring epinephrine concentration in the jawbone, and confirmation of actual histology. If definitive vasoconstrictor effect in tissue can be confirmed with a minimal concentration of epinephrine, this will be a valuable study to decrease circulatory complications in patients with severe cardiovascular disease.
CONCLUSION
The effect on lidocaine concentration in jawbone and oral mucosal tissue by the addition of epinephrine to local anesthetic lidocaine was evaluated through direct quantitative determination of lidocaine concentration in tissue. As a result, high lidocaine concentration in tissue could be maintained by adding epinephrine to lidocaine. Epinephrine-induced vasoconstrictor effect was observed not only in the oral mucosa but also in the jawbone.
REFERENCES
- 1.Miller RD. Miller's Anesthesia. 6th ed. Tokyo, Japan: Medical Sciences International;; 2009. Local anesthesia; pp. 453–476. In. [Google Scholar]
- 2.Yamazaki T, Mamiya H, Ichinohe T, Kaneko Y. Distribution of lidocaine in alveolar tissues in rabbits. J Hard Tissue Biol. 2009;18:95–100. [Google Scholar]
- 3.Ohkado S, Ichinohe T, Kaneko Y. Comparative study on anesthetic potency depending on concentration of lidocaine and epinephrine: assessment of dental local anesthetics using the jaw-opening reflex in rabbits. Anesth Prog. 2001;48:16–20. [PMC free article] [PubMed] [Google Scholar]
- 4.Miyoshi T, Aida H, Kaneko Y. Comparative study on anesthetic potency of dental local anesthetics assessed by the jaw-opening reflex in rabbits. Anesth Prog. 2000;47:35–41. [PMC free article] [PubMed] [Google Scholar]
- 5.Goto K. Studies on mechanism of action of vasoconstrictors as potentiator in local anesthesia. Tohoku Univ Dent J. 1998;7:1–12. [Google Scholar]
- 6.Sasao M. In search for the ideal local anesthetic in dentistry—evaluation of the effect of infiltration anesthesia. J Jpn Dent Soc Anesthesiol. 2006;34:126–134. [Google Scholar]
- 7.Sasao M, Noguchi I, Ohyama N, Takano K, Amemiya Y. Effect on infiltration anesthesia induced by different concentrations of lidocaine and epinephrine: quantitative estimation by analysis of somatosensory evoked potentials in rats. J Jpn Dent Soc Anesthesiol. 1999;27:158–164. [Google Scholar]
- 8.Homma Y, Ichinohe T, Kaneko Y. Oral mucosal blood flow, plasma epinephrine and haemodynamic responses after injection of lidocaine with epinephrine during midazolam sedation and isoflurane anesthesia. Br J Anaesth. 1999;82:570–574. doi: 10.1093/bja/82.4.570. [DOI] [PubMed] [Google Scholar]
- 9.Oka S. Effect of concentration of vasoconstrictor in local anesthetic on local anesthesia and hemodynamic. J Jpn Dent Soc Anesthesiol. 1990;18:43–66. [Google Scholar]
- 10.Ito S. A study on changes of serum and plasma lidocaine concentrations in dentistry. J Jpn Dent Soc Anesthesiol. 1979;7:212–234. [Google Scholar]
- 11.Wildsmith JA, Tucker GT, Cooper S, Scott DB, Covino BG. Plasma concentrations of local anesthetics after interscalene brachial plexus block. Br J Anaesth. 1977;49:461–466. doi: 10.1093/bja/49.5.461. [DOI] [PubMed] [Google Scholar]
- 12.Nishizawa S, Ichinohe T, Kaneko Y. Tissue blood flow reductions induced by remifentanil in rabbits and the effect of naloxone and phentolamine on these changes. J Oral Maxillofac Surg. 2012;70:797–802. doi: 10.1016/j.joms.2011.10.012. [DOI] [PubMed] [Google Scholar]
- 13.Yasuda A, Yamashiro M, Hashimoto S, Sunada K. Effects of adrenaline on the pharmacokinetic of 14C-lidocaine after maxillary infiltration anesthesia in rats. J Jpn Dent Soc Anesthesiol. 2011;39:1–12. [Google Scholar]
- 14.Shinoda K. Determination of local blood flow in bone marrow by electrochemically generated hydrogen. J Juzen Med Soc. 1985;94:678–688. [Google Scholar]
- 15.Ma D, Chakrabarti MK, Whitwam JG. The combined effects of sevoflurane and remifentanil on central respiratory activity and nociceptive cardiovascular responses in anesthetized rabbits. Anesth Analg. 1999;89:453–461. [PubMed] [Google Scholar]
- 16.Beach CL, Ludden TM, Clementi WA, Allerheiligen SR. Measurement of lidocaine free concentration. Ther Drug Monit. 1986;8:326–330. doi: 10.1097/00007691-198609000-00015. [DOI] [PubMed] [Google Scholar]
- 17.Parish RC, Gotz VP, Lopez LM, Curry SH. Improved EMIT analysis for lidocaine. Clin Chem. 1985;31:1920–1921. [PubMed] [Google Scholar]
- 18.Oellerich M. Enzyme immunoassays in clinical chemistry: present status and trends. J Clin Chem Clin Biochem. 1980;18:197–208. doi: 10.1515/cclm.1980.18.4.197. [DOI] [PubMed] [Google Scholar]
- 19.Piwowarska J, Kuczynska J, Pachecka J. Liquid chromatographic method for the determination of lidocaine and monoethylglycine xylidide in human serum containing various concentrations of bilirubin for the assessment of liver function. J Chromatogr B Analyt Technol Biomed Life Sci. 2004;805:1–5. doi: 10.1016/j.jchromb.2004.01.030. [DOI] [PubMed] [Google Scholar]
- 20.Morota T, Kawaai H, Yamazaki S. Difference of injection point for local anesthesia in alveolar bone affects infiltration and action of anesthesia. Ohu Univ Dent J. 2014;41:29–38. [Google Scholar]
- 21.Ichinohe T, Kaneko Y, Nakakuki T. The Effect of epinephrine on circulation and respiration—investigation with epinephrine infusion technique. J Jpn Dent Soc Anesthesiol. 1990;18:477–497. [Google Scholar]
- 22.Troullos ES, Goldstein DS, Hargreaves KM, Dionne RA. Plasma epinephrine levels and cardiovascular response to high administered doses of epinephrine contained in local anesthesia. Anesth Prog. 1987;34:10–13. [PMC free article] [PubMed] [Google Scholar]
- 23.Yamatsuta Y, Kanri T, Sano K. Influence of epinephrine on peripheral blood flow. J Jpn Dent Soc Anesthesiol. 1989;17:479–489. [Google Scholar]
- 24.Suzuki T, Kitano T, Kanri T. The influence of various local anesthestic available on the market on peripheral blood flow in human gingiva. J Jpn Dent Soc Anesthesiol. 1990;18:627–641. [Google Scholar]
- 25.Ogawa S, Watanabe T, Kawaai H, Tada H, Yamazaki S. Lidocaine concentration in mandibular bone after subperiosteal infiltration anesthesia decreases with elevation of periosteal flap and irrigation with saline. Anesth Prog. 2014;61:53–62. doi: 10.2344/0003-3006-61.2.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ishikawa M, Momota Y, Kotani J. Effects of adrenalin and the sedative agent on the systemic vascular absorption of lidocaine after local infiltration anesthesia. J Jpn Dent Soc Anesthesiol. 2007;35:649–654. [Google Scholar]
- 27.Eger EI., II . Anesthetic Uptake and Action. Philadelphia, Pa: Williams & Wilkins;; 1974. Uptake of inhaled anesthetics, the alveolar to inspired anesthetic difference; pp. 77–96. In. [Google Scholar]
- 28.Becker DE, Reed KL. Essentials of local anesthetic pharmacology. Anesth Prog. 2006;53:98–108. doi: 10.2344/0003-3006(2006)53[98:EOLAP]2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]