Abstract
Effective pain control during local anesthetic injection is the cornerstone of behavior guidance in pediatric dentistry. The aim of this study was to evaluate the practical efficacy of a 2-stage injection technique in reducing injection pain in children. This was a split-mouth, randomized controlled crossover trial. One hundred cooperative children aged 7 to 13 years in need of bilateral local anesthetic injections (inferior alveolar nerve block, posterior superior alveolar nerve block, or maxillary and mandibular buccal infiltrations) for restorative, endodontic, and extraction treatments were recruited for the study. Children were randomly allocated to receive either the 2-stage injection technique or conventional technique at the first appointment. The other technique was used at the successive visit after 1 week. Subjective and objective evaluation of pain was done using the Wong–Baker FACES Pain Rating Scale (FPS) and Sound Eye Motor (SEM) scale, respectively. The comparison of pain scores was done by Wilcoxon sign-rank test. Both FPS and SEM scores were significantly lower when the 2-stage injection technique of local anesthetic nerve block/infiltration was used compared with the conventional technique. The 2-stage injection technique is a simple and effective means of reducing injection pain in children.
Key Words: Local anesthesia, Injection pain, Inferior alveolar nerve block, Posterior superior alveolar nerve block, Buccal infiltration
Local anesthetic injection is the most anxiety-provoking factor for children in dentistry,1 as it is allied with pain and extreme discomfort.2 Pain is highly complex and multidimensional, the control of which is crucial to instill a positive dental attitude in children.3 Various techniques of reducing injection pain in children can be broadly categorized as psychological and physical. The psychological approach includes behavior management techniques such as distraction4 and hypnosis.5 Physical means include various strategies such as topical anesthesia application, warming injection solution, increased injection time, reducing the needle diameter, and other recent techniques such as WAND, electronic dental anesthesia, and so forth. However, none of these techniques have been successful in eliminating fear and anxiety in children.6
Walton,7 Torabinejad,7 and Levine8 have addressed a simple and practical approach called the 2-stage injection technique to reduce injection pain. This is done by initial submucosal deposition of local anesthetic solution for regional numbness and then targeting the nerve to be anesthetized after several minutes so that injection pain is reduced. Nusstein et al9 evaluated the practical outcome of this 2-stage injection technique for inferior alveolar nerve block (IANB) and reported a significant reduction in pain during needle placement. To the extent of our knowledge, no single study has evaluated the effectiveness of this technique in children. We feel that children are the target group for whom pain control should be adequately followed. Hence, the purpose of this study was to compare pain perception rates during local anesthetic nerve blocks using the conventional injection technique and the 2-stage injection technique in children.
METHODS
This study was conducted on outpatients attending the Department of Pediatric Dentistry, G Pulla Reddy Dental College and Hospital, between January 2013 and September 2013. A total of 100 children aged 7 to 13 years of both genders who met the criteria were recruited for the study. All parents were informed about the study protocol, and prior written consent was obtained. The study protocol was approved by the G Pulla Reddy Dental College and Hospital ethical committee for research activities. Inclusion criteria were children with good general health (ASA I–II) without any history of allergic reactions as determined by a written history and personal interview of the parent and children not taking any medication that would alter their pain perception. Children demonstrating definitely negative behavior (Frankl behavior rating scale) during their initial examination visit were excluded from the study.
This was a split-mouth, randomized controlled crossover trial in which each child served as his or her own control. Children indicated for bilateral dental extractions, pulpal treatments, or operative procedures, either in the maxillary or mandibular arch, who needed local anesthesia were recruited for the study. Only IANB, posterior superior alveolar nerve block (PSAN), and maxillary and mandibular buccal infiltrations were tested. At visit 1, the children were randomly assigned to either the conventional technique or the 2-stage injection technique based on their assigned participant number and corresponding randomization code. Only the random codes were entered in the datasheets to blind the experiment. After 1 week, the other technique was used to perform treatment on the contralateral side. All injections were delivered by a single trained dentist unaware of the study protocol, and he was instructed to choose similar sites bilaterally during injections. The sample distribution was as follows: total number of children = 100, PSAN = 25, IANB = 25, maxillary infiltrations = 25, mandibular infiltrations = 25.
Injection Technique
The intraoral mucosal site was dried with 2 × 2 gauze and prepared with gauze dipped in povidine–iodine solution. Topical anesthetic gel (Benzocaine 20% w/w, Vishal care gel, India) was applied for 1 minute using a cotton applicator at the injection site. For all injections, a 24-gauge long needle (1½ inch) was selected and attached to a 3-mL hypodermic syringe (Dora, Kesava Medi Devices PVT LTD, Tirupati, India). For the local anesthetic solution, 2.5 mL of 2% lidocaine with 1:80,000 epinephrine was used (Lignox 2% A vial, Indico Remedies, Mumbai, India).
IANB 2-Stage Injection Technique
The initial needle penetration to a depth of 2 mm was done slowly; 0.5 mL of anesthetic solution was deposited over 60 seconds, and the needle was withdrawn. After 5 minutes, the needle was reinserted at the same location and advanced to the target site until bone was gently contacted. Aspiration to rule out any vascular entry was performed, and the rest of the anesthetic solution (2.0 mL) was deposited over 1 minute.
PSAN 2-Stage Technique
Initial needle penetration to a depth of 2 mm was done slowly at the height of the mucobuccal fold of the permanent maxillary first molar; 0.5 mL anesthetic solution was deposited over 60 seconds, and the needle was withdrawn. After 5 minutes, the needle was reinserted at the same location and advanced posteriorly, medially, and superiorly to the target site, where the rest of the solution (2.0 mL) was deposited over 1 minute.
Infiltration Anesthesia (Either Maxillary/Mandibular) 2-Stage Technique
The needle was inserted to a depth of 2 mm at the mucobuccal fold of the tooth, and submucosal deposition of 0.5 mL was done slowly for 20 seconds. After a gap of 5 minutes, the needle was reinserted into the mucosa at the same location and advanced to the target site over approximately 10 seconds, and another 2.0 mL was deposited for 10 seconds.
Conventional Block and Infiltration Anesthesia (Either Maxillary/Mandibular) Technique
The conventional block and infiltration injection techniques were identical to their respective 2-stage counterpart injections, except that they were accomplished with a single one-thrust placement to the endpoint target and then the local anesthetic was injected. The blinding of the injection methods was accomplished by adding an additional sham injection as suggested by Nusstein et al9 (5 minutes after the conventional injection, the needle was reinserted at the same site to a depth of 2–3 mm, and an injection was mimicked by lightly pushing on the syringe for 1 minute).
Subjective and Objective Evaluation of Pain
Immediately after the injections (sham injection for conventional technique, second insertion for 2-stage technique) and before treatment, children were asked to complete a Wong–Baker FACES Pain Rating Scale (FPS). Instructions were given to the child on how to use the FPS in the presence of parents. The scale ranges between 0 and 5, where 0 is no hurt and 5 is hurt very much. The pain perception of each child was evaluated objectively using the sound, eye, and motor (SEM) scale. The assessment criteria of the SEM scale are presented in Table 1. The sounds, eye symptoms, and movement of children were evaluated by a trained observer standing 60 cm away from the dental chair. The observer was previously trained in a pilot study done on a different sample. Intraexaminer variability was within the acceptable range (k value = 0.71). The SEM score was determined by summing the grade values.
Table 1. .
Sound Eye Motor (SEM) Scale

Descriptive analysis was done by calculating the mean and standard deviation of the scores. The Wilcoxon sign-rank test was used to compare scores between the 2 techniques. The significance level was set for ≤.05.
RESULTS
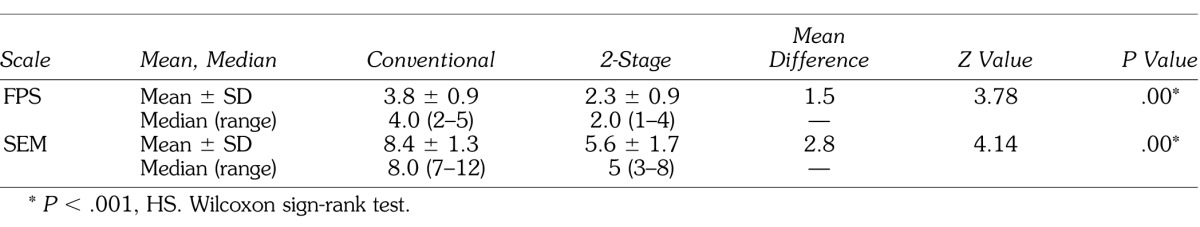
On comparison, the FPS and SEM scores were significantly lower in the sample tested when the 2-stage injection technique was used for all of the anesthetic blocks and infiltration techniques (Tables 2–5).
Table 2. .
Comparison of Wong–Baker FACES Pain Rating Scale (FPS) Scores and Sound Eye Motor (SEM) Scores Between Conventional and 2-Stage Posterior Superior Alveolar Nerve Block

Table 5. .
Comparison of Wong–Baker FACES Pain Rating Scale (FPS) Scores and Sound Eye Motor (SEM) Scores Between Conventional and 2-Stage Mandibular Infiltrations

Table 3. .
Comparison of Wong–Baker FACES Pain Rating Scale (FPS) Scores and Sound Eye Motor (SEM) Scores Between Conventional and 2-Stage Inferior Alveolar Nerve Block

Table 4. .
Comparison of Wong–Baker FACES Pain Rating Scale (FPS) Scores and Sound Eye Motor (SEM) Scores Between Conventional and 2-Stage Maxillary Infiltrations
DISCUSSION
Pain perception during local anesthetic nerve blocks can be differentiated as needle insertion pain, needle placement pain, and solution deposition pain. Different techniques employed to reduce this injection pain can be categorized as follows:
Techniques that reduce needle insertion pain: Topical anesthetic application (gel or spray or EMLA patches), ethyl chloride spray, reducing needle diameter
Techniques that reduce needle advancement pain: Counterstimulation, electronic dental anesthesia (transcutaneous electrical nerve stimulation)
Techniques that reduce solution deposition pain: Computer-controlled local anesthetic delivery (WAND), slow injection rate, warming injection solutions
Miscellaneous techniques that focus on overall pain control: Psychosocial interventions, such as distraction, hypnosis, jet injections, transcutaneous electrical nerve stimulation, and so forth
The 2-stage injection technique is one alternative to the conventional injections in which regional analgesia of the tissues ahead of the needle can reduce insertion, placement, and deposition pain. To our knowledge, only one study by Nusstein et al9 evaluated the efficacy of this technique in 51 young adults for IANB block. Subjective assessment using the Heft-Parker visual analog scale was done at 3 phases of the block, concluding that the 2-stage technique does not affect needle insertion pain or solution deposition pain but does affect needle placement pain in women. It was not clear from the methodological aspect whether the subjects were asked to rate their pain at each stage (such as insertion, placement, and deposition) by stopping the block at each level or whether they were asked to rate it after completion of the block. To rule out this bias, we have taken an overall assessment of pain after completing the block for the 2 techniques tested. The SEM scale was used in this study to record pain reactions since it is considered to be a sensitive scale, recording detailed levels of eye, sound, or motor reactions. The FPS was used as it is easy to understand and applicable to the age group selected.10 Results of the present study show that there was a significant reduction of both FPS and SEM scores in the sample when the 2-stage technique was used. Reduced pain scores in the sample can be explained below.
Application of topical anesthesia can anesthetize only 2- to 3-mm thickness of mucosa.11 When the 2-stage technique was used, the initial needle penetration was restricted to 2 mm, henceforth reducing insertion pain. The amount of solution deposited was only 0.5 mL at the initial stage, which results in minimal tissue distension, causing less pain. During the wait period of 5 minutes, the optimal diffusion of local anesthetic solution can be expected to block the peripheral nerves, which can reduce needle placement and deposition pain.12
Based on the present findings, it is obvious that the local anesthetic nerve block using the 2-stage injection technique causes less discomfort compared with the traditional technique. Another simple modification is advocated by the authors and called a multistage injection technique/successional technique. This is done by successive deposition of small amounts of local anesthetic solution ahead of needle placement during a nerve block. This is similar to the chasing technique, in which palatal injections were made acceptable by successive infiltration of the buccal mucosa, interdental papilla, and palatal gingiva.13 The possible disadvantage of these 2 techniques may be multiple injection trauma; however, it is negligible from a healing point of view. Hence, despite recent advances such as WAND and EDA, it is recommended that researchers evaluate simple and effective techniques such as the 2-stage injection and chasing techniques in vivo for painless treatment in children. The small sample size is this study's main limitation. However, the present study has proven the efficacy of the 2-stage injection technique as a practical alternative to conventional injections for reducing injection pain in children.
REFERENCES
- 1.Milgrom P, Coldwell SE, Getz T, Weinstein P, Ramsay DS. Four dimensions of fear of dental injections. J Am Dent Assoc. 1997;128:756–762. doi: 10.14219/jada.archive.1997.0301. [DOI] [PubMed] [Google Scholar]
- 2.Kuscu OO, Akyuz S. Is it the injection device or the anxiety experienced that causes pain during dental local anaesthesia? Int J Paediatr Dent. 2008;8:139–145. doi: 10.1111/j.1365-263X.2007.00875.x. [DOI] [PubMed] [Google Scholar]
- 3.McDonald RE, Avery DR, Dean JA, Jones JE. Local anesthesia and pain control for the child and adolescent. In: McDonald RE, DR Avery, Dean JA, editors. Dentistry for the Child and Adolescent. 9th ed. St Louis, Mo: CV Mosby Inc;; 2011. pp. 241–252. In. eds. [Google Scholar]
- 4.El-Sharkawi HF, El-Housseiny AA, Aly AM. Effectiveness of new distraction technique on pain associated with injection of local anesthesia for children. Pediatr Dent. 2012;34:35–38. [PubMed] [Google Scholar]
- 5.Accardi MC, Milling LS. The effectiveness of hypnosis for reducing procedure related pain in children and adolescents: a comprehensive methodological review. J Behav Med. 2009;32:328–339. doi: 10.1007/s10865-009-9207-6. [DOI] [PubMed] [Google Scholar]
- 6.Asarch T, Allen K, Petersen B, Beiraghi S. Efficacy of computerized local anesthesia device in pediatric dentistry. Pediatr Dent. 1999;21:421–429. [PubMed] [Google Scholar]
- 7.Walton RE, Reader A, Nusstein JM. Local anesthesia. In: Torabinejad M, Walton RE, editors. Endodontics Principles and Practice. 4th ed. St Louis, M: Saunders Elsevier;; 2008. pp. 129–147. In. eds. [Google Scholar]
- 8.Levine A. Preventing pain: the one-two injection. Tic. 1968;27:6. [PubMed] [Google Scholar]
- 9.Nusstein J, Steinkruger G, Reader A, Beck M, Weaver J. The effects of a 2-stage injection technique on inferior alveolar nerve block injection pain. Anesth Prog. 2006;53:126–130. doi: 10.2344/0003-3006(2006)53[126:TEOASI]2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.dos Santos Calderon P, Peixoto RF, Gomes VM et al. Concordance among different pain scales in patients with dental pain. J Orofac Pain. 2012;26:126–131. [PubMed] [Google Scholar]
- 11.Jeske AH, Blanton PL. Misconceptions involving dental local anesthesia. Part 2: pharmacology. Texas Dent J. 2002;119:310–314. [PubMed] [Google Scholar]
- 12.Malamed SF. Handbook of Local Anesthesia. St Louis, Mo: C.V. Mosby; 2004. pp. 189–226. 5th ed. [Google Scholar]
- 13.Meechan JG. Pain control in local analgesia. Eur Arch Paediatr Dent. 2009;10:71–76. doi: 10.1007/BF03321603. [DOI] [PubMed] [Google Scholar]


