Abstract
Patient: Male, 71
Final Diagnosis: Pulmonary nocardiosis
Symptoms: Cough • dyspnea • fever
Medication: Carfillzomib
Clinical Procedure: Bronchoscopy
Specialty: Infectious Diseases
Objective:
Rare co-existance of disease or pathology
Background:
The use of proteasome inhibitors like Bortezomib to treat multiple myeloma has been associated with increased rates of opportunistic infections, including Nocardia, especially when lymphopenia is present. The prevalence or association of such infections with newer agents like Carfilzomib is not known.
Case Report:
A 71-year-old man with multiple myeloma presented with a 6-week history of respiratory symptoms and cyclic fevers. He was undergoing chemotherapy with Carfilzomib. Work-up revealed severe lymphopenia and a CT chest showed multiple lung nodules and a mass-like consolidation. He underwent a bronchoscopy, and respiratory cultures grew Nocardia species. He responded well to intravenous antibiotics with resolution of symptoms and CT findings.
Conclusions:
With the introduction of newer agents like Carfilzomib for the treatment of multiple myeloma, clinicians must maintain a high degree of suspicion for opportunistic infections to achieve early diagnosis and treatment.
MeSH Keywords: Lymphopenia, Multiple Myeloma, Nocardia, Proteasome Inhibitors
Background
Proteasome inhibitors (PI) are being increasingly used to treat multiple myeloma (MM). They have been shown to reduce antigen processing and CD8 T cell function vital for cell-mediated immunity. PI bortezomib has been associated with increased rates of opportunistic infections when severe lymphopenia is present. Carfilzomib is a novel PI approved for the treatment of refractory MM for which the prevalence of opportunistic infections is not known. We report a case of pulmonary nocardiosis in a patient with refractory MM being treated with Carfilzomib chemotherapy.
Case Report
A 71-year-old man with MM presented with a 6-week history of fever and cough. He was diagnosed with MM 6 years before presentation and underwent autologous stem cell transplantation followed by lenalidomide maintenance. He relapsed and dexamethasone with bortezomib was added to his treatment. Due to breakthrough disease (8 weeks before admission), he was started on carfilzomib and received 13 cycles. Two weeks into therapy he developed transient low-grade post-chemotherapy fever and progressive dyspnea. He denied involvement in outdoor work or exposure to soil and had no weight loss, seizures, headache, focal weakness, skin abscesses, or ulcerations
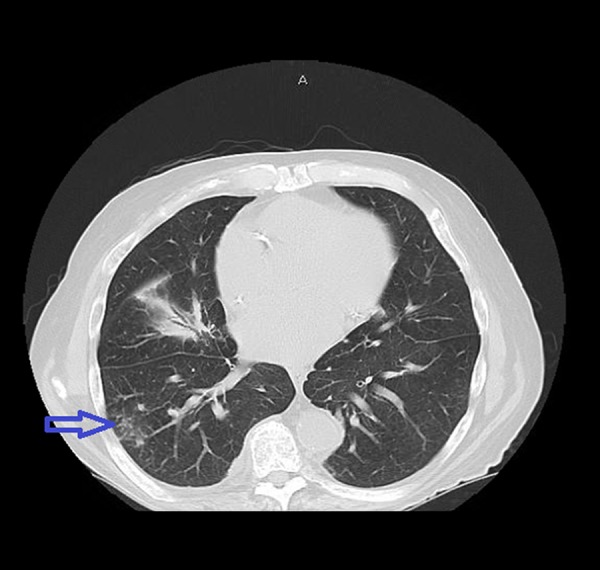
On admission, he was febrile and tachypneic. Examination was significant for diminished breath sounds over the right mid- and lower lung zones. WBC count was 6500/mcl with 90% neutrophils and 1% lymphocytes. CT angiography ruled out pulmonary embolism, but revealed a mass-like consolidation in the right lower lobe, with bilateral airspace consolidations (Figure 1). Bronchoscopy, bronchoalveolar lavage, and transbronchial biopsies were negative for malignancy; however, respiratory cultures grew Nocardia abscessus.
Figure 1.

Mass-like lesion at the right lower lobe with airspace consolidations.
He was treated with intravenous trimethoprim-sulfamethoxazole (TMP-SMX) and meropenem. Repeat CT showed a significant decrease in the mass-like lesion on the right, now with cavitation and resolution of the airspace consolidations (Figure 2) within a period of 3 weeks. He was discharged on trimethoprim-sulfamethoxazole and minocycline with close follow-up. Unfortunately, he returned with a fever and CT evidence of worsening right lower lobe consolidation. Treatment with intravenous meropenem and TMP-SMX were restarted. Malignancy was excluded by a CT-guided biopsy. Due to concerns that TMP-SMX were contributing to leukopenia, it was changed to tigecycline. He showed dramatic clinical improvement and was discharged to complete 42 days of intravenous tigecycline and meropenem while awaiting final Nocardia sensitivities. Close follow-up with the Infectious Diseases Department and Oncology was scheduled. He is currently on a chemotherapy regimen of Dexamethasone, Bortezomib, and Panobinostat for the treatment of MM.
Figure 2.
Significant improvement in the mass-like lesion, now with evidence of cavitation and resolution of airspace consolidations.
Discussion
Nocardia produces a life-threatening infection in patients with defective cell-mediated immunity, with a high propensity for delayed diagnosis because of the non-specific presentation and radiographic findings. In addition to the severe morbidity, including its predilection for the CNS, the diagnosis often involves prolonged courses of antibiotics and associated toxicities. There are multiple risk factors that predispose patients to infection with Nocardia, and conditions or medications that suppress cell-mediated immunity predominate. Multiple myeloma causes immune deficiency mainly through B-cell dysfunction.
Proteasomes are large protein complexes in nucleated cells that bind and degrade ubiquitinated proteins, thus helping, along with lysosomes, to maintain protein homeostasis. Malignant cells are highly dependent on this pathway. Proteasome inhibitors cause buildup of substrates, disrupt signaling pathways, and arrest cell cycle progression. Proteasome inhibitors like Bortezomib have been shown to have numerous effects on the immune system [1], which are all vital for cell-mediated immunity. They decrease proliferation and viability of T cells [2,3] and the number and function of NK and CD8 T cells [4].They impair antigen presentation, dendritic cell function [5,6], and alter cytokine secretion [7]. The use of bortezomib has been associated with increased incidence of opportunistic infections, including Nocardia, within the treatment period when severe lymphopenia is present [8,9]. Unlike bortezomib, whose effect is slowly reversible, carfilzomib exhibits irreversible inhibition of proteasome activity. The onset of action is similar but its effect is more sustained and specific [10]. In our patient, the lymphocyte count during admission was 1%, likely induced by carfilzomib and bortezomib, which may have contributed to Nocardia infection. In addition, the patient was also on dexamethasone, which contributed to the overall state of immunosuppression and perhaps the predisposition to nocardiosis.
Conclusions
Based on our case and recent reports of nocardiosis, there may be a role for close clinical monitoring in patients with severe lymphopenia who are treated with proteasome inhibitors for opportunistic nocardiosis.
With advancements in the treatments for multiple myeloma, clinicians must have a high degree of suspicion for the development of opportunistic infections, including Nocardia, in an effort to achieve early and effective diagnosis and treatment.
References:
- 1.Nucci M, Anaissie E. Infections in patients with multiple myeloma in the era of high-dose therapy and novel agents. Clin Infect Dis. 2009;49(8):1211–25. doi: 10.1086/605664. [DOI] [PubMed] [Google Scholar]
- 2.Blanco B, Pérez-Simón JA, Sánchez-Abarca LI, et al. Bortezomib induces selective depletion of alloreactive T lymphocytes and decreases the production of Th1 cytokines. Blood. 2006;107:3575–83. doi: 10.1182/blood-2005-05-2118. [DOI] [PubMed] [Google Scholar]
- 3.Sun K, Welniak LA, Panoskaltsis-Mortari A, et al. Inhibition of acute graft-versus-host disease with retention of graft-versus-tumor effects by the proteasome inhibitor bortezomib. Proc Natl Acad Sci USA. 2004;101(21):8120–25. doi: 10.1073/pnas.0401563101. (Published erratum appears in Proc Natl Acad Sci USA, 2004; 101(34):12777) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Uy GL, Peles S, Fisher NM, et al. Bortezomib prior to autologous transplant in multiple myeloma: Effects on mobilization, engraftment, and markers of immune function. Biol Blood Marrow Transplant. 2006;12(2):116. Suppl.1: [Google Scholar]
- 5.Miceli M, Atoui R, Thertulien R, et al. Deep septic thrombophlebitis: an unrecognized cause of relapsing bacteremia in patients with cancer. J Clin Oncol. 2004;22:1529–31. doi: 10.1200/JCO.2004.99.289. [DOI] [PubMed] [Google Scholar]
- 6.Tsukayama DT. Pathophysiology of posttraumatic osteomyelitis. Clin Orthop Relat Res. 1999;360:22–29. doi: 10.1097/00003086-199903000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Dispenzieri A. Complications of myeloma therapy. Hematol Oncol Clin North Am. 2007;21:1247–73. doi: 10.1016/j.hoc.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 8.Pamukçuoglu M, Emmez H, Tunçcan OG, et al. Brain abscess caused by Nocardia cyriacigeorgica in two patients with multiple myeloma: novel agents, new spectrum of infections. Hematology. 2014;19:158–62. doi: 10.1179/1607845413Y.0000000108. [DOI] [PubMed] [Google Scholar]
- 9.Jung SH, Bae SY, Ahn JS, et al. Lymphocytopenia is associated with an increased risk of severe infections in patients with multiple myeloma treated with bortezomib based regimens. Int J Hematol. 2013;97:382–87. doi: 10.1007/s12185-013-1270-7. [DOI] [PubMed] [Google Scholar]
- 10.Siegel D, Martin T, Wang M, et al. Results of PX-171-003-A1, an open label, single arm, phase 2 study of carfilzomib in patients with relapsed and refractory multiple myeloma. Blood. 2012;120(14):2817–25. doi: 10.1182/blood-2012-05-425934. [DOI] [PMC free article] [PubMed] [Google Scholar]


