There are several indications for percutaneous tracheostomy and, although it is a common bedside procedure performed by a surgeon in intensive care units, gaps exist in follow-up after transfer to the ward. Given that deficiencies in specialized tracheostomy management may lead to serious complications – some of which may be life threatening – it is important to address these knowledge gaps in particular management strategies. Prompted, in part, by the lack of formalized processes at the author’s institution and the scarcity of high-quality literature evidence supporting the value of interprofessional tracheostomy teams, this article describes the implementation of such a team and its impact on several metrics.
Keywords: Decannulation, Intensive care, Interprofessional, Quality improvement, Respiratory therapy, Tracheostomy
Abstract
BACKGROUND:
Percutaneous tracheostomy is a common procedure in the intensive care unit and, on patient transfer to the wards, there is a gap in ongoing tracheostomy management. There is some evidence that tracheostomy teams can shorten weaning to decannulation times. In response to lengthy weaning to decannulation times at Trillium Health Partners – Credit Valley Hospital site (Mississauga, Ontario), an interprofessional tracheostomy team, led by respiratory therapists and consisting of speech-language pathologists and intensive care physicians, was implemented.
OBJECTIVE:
To evaluate the interprofessional tracheostomy team and its impact on time from weaning off mechanical ventilation to decannulation; and time from weaning to speech-language pathology referral.
METHODS:
Performance metrics were collected retrospectively through chart review pre- and post-team implementation. The primary metrics evaluated were the time from weaning off mechanical ventilation to decannulation, and time to referral to speech-language pathology.
RESULTS:
Following implementation of the interprofessional tracheostomy team, there was no improvement in decannulation times or time from weaning to speech-language pathology referral. A significant improvement was noted in the average time to first tracheostomy tube change (36.2 days to 22.9 days; P=0.01) and average time to speech-language pathology referral following initial tracheostomy insertion (51.8 days to 26.3 days; P=0.01).
CONCLUSION:
An interprofessional tracheostomy team can improve the quality of tracheostomy care through earlier tracheostomy tube changes and swallowing assessment referrals. The lack of improved weaning to decannulation time was potentially due to poor adherence with established protocols as well as a change in mechanical ventilation practices. To validate the findings from this particular institution, a more rigorous quality improvement methodology should be considered in addition to strategies to improve protocol compliance.
Abstract
HISTORIQUE :
La trachéostomie percutanée est une intervention fréquente dans l’unité de soins intensifs. Au transfert des patients au service d’hospitalisation, la continuité de la prise en charge de la trachéostomie pose un problème. Selon certaines données, les équipes de trachéostomie peuvent réduire le temps accordé au sevrage avant la décanulation. En réponse au long temps accordé sevrage avant la décanulation du Credit Valley Hospital des Trillium Health Partners (Mississauga, Ontario), une équipe interprofessionnelle de trachéostomie, dirigée par des inhalothérapeutes et composée d’orthophonistes et d’intensivistes, a été formée.
OBJECTIF:
Évaluer l’équipe interprofessionnelle de trachéostomie et ses effets lors du temps accordé entre le sevrage de la ventilation mécanique et la décanulation ainsi que sur le temps accordé entre le sevrage et l’orientation vers l’orthophonie.
MÉTHODOLOGIE :
Les chercheurs ont recueilli rétrospectivement les mesures de performance par une analyse des dossiers avant et après la formation de l’équipe. Les mesures primaires évaluées étaient le temps accordé entre le sevrage de la ventilation mécanique et la décanulation, et le temps accordé avant l’orientation vers un l’orthophonie.
RÉSULTATS :
Après la formation de l’équipe interprofessionnelle de trachéostomie, il n’y avait pas de réduction du temps accordé avant la décanulation ou l’orientation vers l’orthophonie. Le temps accordé, en moyenne, avant le premier changement de canule de trachéostomie a considérablement diminué (passant de 36,2 jours à 22,9 jours; P=0,01), de même que le temps accordé, en moyenne, avant l’orientation vers une orthophonie après l’insertion de la première trachéostomie (passant de 51,8 jours à 26,3 jours; P=0,01).
CONCLUSION :
Une équipe interprofessionnelle de trachéostomie peut améliorer la qualité des soins de trachéostomie grâce au changement plus rapide de la canule de trachéostomie et à l’orientation vers une évaluation de la déglutition. L’absence de réduction du temps accordé entre le sevrage et la décanulation pouvait être causée par une mauvaise compliance aux protocoles établis et à un changement aux pratiques de ventilation mécanique. Pour valider les observations provenant de cet établissement, il faudrait envisager une méthodologie d’amélioration de la qualité plus rigoureuse en plus de stratégies pour améliorer la compliance au protocole.
Tracheostomy is a common bedside procedure in the intensive care unit (ICU) and is often performed percutaneously by a surgeon. The primary indications for tracheostomy are upper airway obstruction, to facilitate weaning from mechanical ventilation, airway protection and for secretion clearance (1). Patients may be transferred to the wards with a tracheostomy in situ but not followed-up or managed by a surgeon due to the procedure being performed at the bedside versus in the operating theatre (2,3). Without specialized knowledge and strategies to address tracheostomy care on the wards, serious complications may occur including respiratory failure and death due to tracheostomy tube occlusion (2,3). It has been reported that an intensivist-led multidisciplinary team was associated with shorter decannulation times and length of stays (3), and that standardized care provided by an interprofessional tracheostomy team was associated with fewer tracheostomy-related complications and increased the use of speaking valves (2). However, a systematic review and meta-analysis reported that there is only low-quality evidence that tracheostomy teams reduce total tracheostomy time and increase speaking valve use (4), which highlights that more evidence is needed to demonstrate the value of a tracheostomy team.
Respiratory therapists (RTs) at Credit Valley Hospital (Mississauga, Ontario) in conjunction with the ICU physicians identified that there was no formalized process for assessment and timing of decannulation, and patients were often not assessed by a physician for decannulation until their first tracheostomy change was due, according to the hospital policy for monthly tube changes. To improve the quality of care provided to patients with tracheostomies on the wards, an interprofessional tracheostomy team was implemented in 2011 at Trillium Health Partners – Credit Valley Hospital site. The interprofessional team was led by RTs who liaised with intensive care physicians, speech-language pathologists and nurses to advocate for quality patient care and timely decannulation.
The primary objective of the present quality improvement study was to evaluate the impact of an interprofessional tracheostomy team on time from weaning off mechanical ventilation to decannulation; and time from weaning to speech-language pathology (S-LP) referral. Secondary measures included time from tracheostomy insertion to first tracheostomy tube change, time from corking to decannulation and time from tracheostomy insertion to S-LP referral. Tertiary measures evaluated were time from tracheostomy insertion to weaning, time from weaning to corking and time from weaning to initial swallowing assessment.
METHODS
Design
The present study was a retrospective analysis in which performance metrics were collected through manual chart review pre- and postintervention.
Setting
The present quality improvement initiative was conducted in the ICU at the Credit Valley Hospital, a 19-bed medical surgical unit that provides continuous monitoring and invasive therapy including mechanical ventilation. Trillium Health Partners is an academic community hospital that consists of three main sites, Credit Valley Hospital, Mississauga Hospital and Queensway Health Centre. A full range of acute health care services, as well as specialized community-based programs, are offered. In 2014 to 2015, there were 1233 inpatient beds available, 61,844 inpatient admissions and 63,525 surgical procedures completed.
Interprofessional tracheostomy team
A working group consisting of respiratory therapy, S-LP and physician representatives came together to form a model for the interprofessional tracheostomy team and created documents to guide clinical practice. A low-risk decannulation pathway developed by Alberta Health Services (5) was referenced to create the team structure and processes. The interprofessional tracheostomy team started on October 18, 2011. The team, which remains in place, consisted of an intensive care physician, an RT and a speech-language pathologist who met weekly for rounds to discuss all patients with a tracheostomy on the wards. Preprinted orders were developed for tracheostomy tube cuff deflation, downsizing, corking and decannulation, which enabled the RT to perform orders according to an algorithm as opposed to requiring a physician order for each individual procedure. Corking was to be implemented for a maximum of 24 h, if tolerated, then the patient would be decannulated in consultation with the tracheostomy team physician. The preprinted orders were developed by the working group using the low-risk decannulation pathway (5) as a key reference. These orders were approved by several hospital committees before being put into practice. An interprofessional policy and procedure was created for all aspects of tracheostomy care and weaning to guide nursing and RT practice. The hospital policy that defined that the first tracheostomy tube must be changed by a physician after one month was modified to allow the RT to change the tube 10 days postinsertion according to preprinted orders and communication with the team. This change was accomplished in alignment with the respiratory therapy scope of practice legislated by the Regulated Health Professions Act (1991) in Ontario.
Data collection
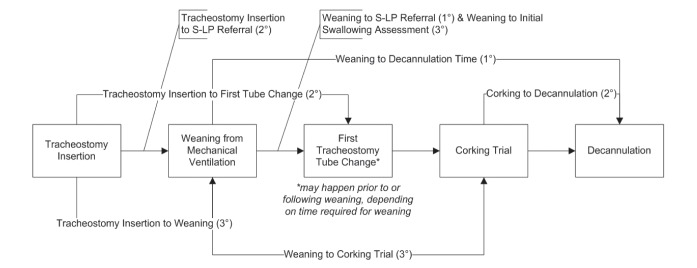
The primary performance metrics collected were the time from weaning from mechanical ventilation to decannulation, and time from weaning to referral to S-LP. Secondary metrics included time from tracheostomy insertion to first tracheostomy tube change, time from corking to decannulation and time from tracheostomy insertion to S-LP referral. Tertiary measures collected were time from tracheostomy insertion to weaning, time from weaning to corking and time from weaning to initial swallowing assessment. Primary, secondary and tertiary measures are graphically presented in Figure 1.
Figure 1).
Graphical timeline of tracheostomy insertion to decannulation pathway including primary (1°), secondary (2°) and tertiary (3°) performance metrics. S-LP Speech-language pathology
Pre-intervention data were collected retrospectively between October 1, 2009 and October 17, 2011. Tracking forms for patients with a tracheostomy were not routinely collected in the respiratory therapy department before 2009 and, therefore, were not available. Postintervention data were collected prospectively between October 18, 2011 and May 22, 2014. These data were collected by the RTs using patient-specific tracking forms for the postintervention group. Patients with a tracheostomy were identified through RT record keeping documents utilized for transfer of information between shift changes. Performance metrics were collected by reviewing progress notes, physician consult notes and flowsheets. In some cases, metrics were missing from the tracking forms for the postintervention group; therefore, retrospective chart reviews were performed to collect the missing data. In cases for which the metrics could not be easily located from chart reviews, the patient(s) were excluded. Performance metrics for each patient were tabulated on a computer spreadsheet (Excel, Microsoft Corporation, USA). Twenty patients were in the pre-intervention group and 24 patients were in the postintervention group. Inclusion criteria included patients who were successfully decannulated. Exclusion criteria included patients who had a permanent tracheostomy, were discharged home and/or patients who died with a tracheostomy in situ.
Data analysis
Calculations were performed using Excel to measure the number of days between performance metrics. Mean days were calculated and compared between the pre- and postintervention groups, in addition to SDs and P values. P values were calculated using a simple independent two-tailed Student’s t test. In addition to the dates of procedures and assessments, patient data were collected to compare patient age, sex and main indication for tracheostomy to determine whether there were any notable differences between the pre- and postintervention groups. Patient age was compared using a simple independent Student’s t test and sex was compared using a χ2 test. Differences were considered to be statistically significant at P<0.05. Statistical analysis was performed using StatPlus Professional version 5.8.4.3 (AnalystSoft, USA).
RESULTS
Patient characteristics
Table 1 summarizes the mean patient age and male sex percentage compared pre- and postintervention. There was no statistically significant difference between age and sex in the pre- and postintervention groups. The primary indication for tracheostomy differed across groups; although the majority of tracheostomies in both groups were performed to facilitate weaning from mechanical ventilation, this percentage was higher in the pre-intervention group. In the postintervention group, 37.5% (n=9) of patients had a tracheostomy inserted for airway protection, compared with only 20% (n=4) of patients in the pre-intervention group (Table 2).
TABLE 1.
Patient demographics pre- and post-interprofessional tracheostomy team implementation
| Demographic | Intervention | P | |
|---|---|---|---|
|
| |||
| Pre (n=20) | Post (n=24) | ||
| Age, years, mean | 61.6 | 61.0 | 0.90 |
| Male sex, % | 55.0 | 41.7 | 0.38 |
TABLE 2.
Primary indication for tracheostomy pre- and post interprofessional tracheostomy team implementation
| Tracheostomy indication | Intervention | |
|---|---|---|
|
| ||
| Pre (n=20) | Post (n=24) | |
| Airway obstruction | 1 (5.0) | 1 (4.2) |
| Airway protection | 4 (20.0) | 9 (37.5) |
| Facilitation of weaning | 15 (75.0) | 13 (54.2) |
| Secretion clearance | 0 (0) | 1 (4.2) |
Data presented n (%)
Primary performance metrics
As presented in Figure 2 and summarized in Table 3, there was an increase of 4.5 days from weaning to decannulation when comparing pre- and postintervention groups; however, this difference was not statistically significant (P=0.62).
Figure 2).
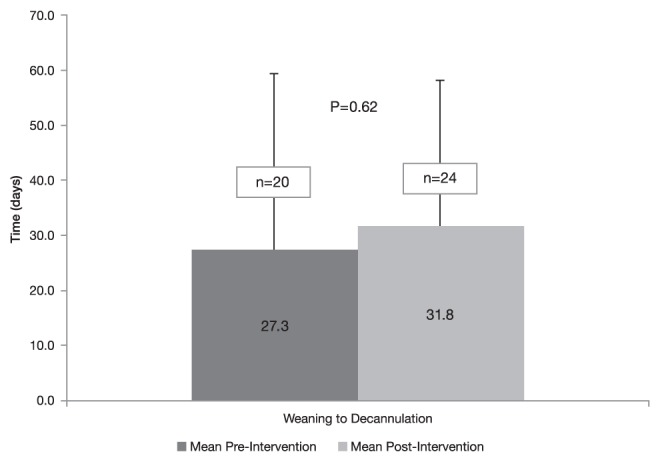
Comparison of weaning to decannulation times pre- and post-interprofessional tracheostomy team implementation
TABLE 3.
Summary of primary, secondary and tertiary results pre- and post-interprofessional tracheostomy team implementation
| Measure | Metric | Days, mean ± SD | Change, days | P | |
|---|---|---|---|---|---|
|
| |||||
| Pre | Post | ||||
| Primary | Weaning to decannulation | 27.3±32.1 (n=20) | 31.8±26.5 (n=24) | 4.5 | 0.62 |
| Weaning to speech-language pathology referral | 21.6± 29.0 (n=17) | 13.8±13.6 (n=20) | 7.8 | 0.27 | |
| Secondary | Tracheostomy insertion to first tube change | 36.2± 18.4 (n=13) | 22.9±11.8 (n=22) | 13.3 | 0.01 |
| Corking to decannulation | 4.8±3.9 (n=16) | 8.5±15.6 (n=22) | 3.7 | 0.35 | |
| Tracheostomy insertion to speech-language pathology referral | 51.8±37.2 (n=19) | 26.3±26.3 (n=21) | 25.5 | 0.01 | |
| Tertiary | Tracheostomy insertion to weaning | 28.8±33.2 (n=20) | 11.3±16.6 (n=24) | 17.5 | 0.03 |
| Weaning to corking | 25.2±35.1 (n=16) | 23.0±17.4 (n=22) | 2.2 | 0.80 | |
| Weaning to initial swallowing assessment | 25.4±31.2 (n=19) | 22.0±17.7 (n=21) | 3.4 | 0.68 | |
The mean number of days between weaning from mechanical ventilation and S-LP swallowing referral improved by 7.8 days; again, this difference was not statistically significant (P=0.27) (Figure 3, Table 3).
Figure 3).
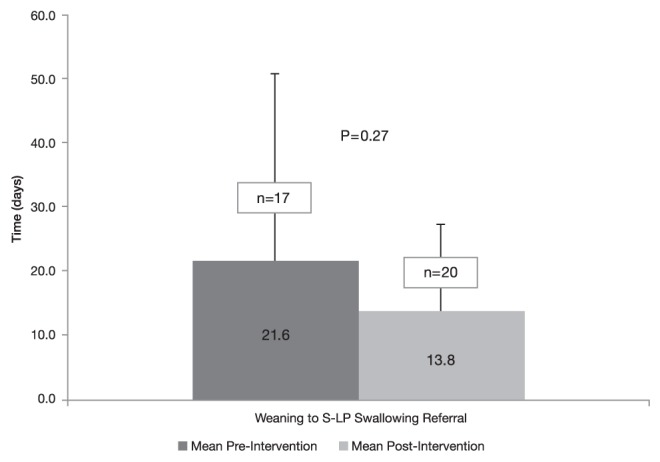
Comparison of weaning to speech-language pathology (S-LP) swallowing referral time pre- and post-interprofessional tracheostomy team implementation
Secondary performance metrics
The time between initial tracheostomy insertion and the first tube change was significantly different (13.3 days; P=0.01) when comparing pre- and postintervention groups, as shown in Figure 4. The time to S-LP referral following initial tracheostomy insertion also was significantly different (25.5 days; P=0.01) (Table 3). There was no significant difference in corking to decannulation times (Table 3).
Figure 4).
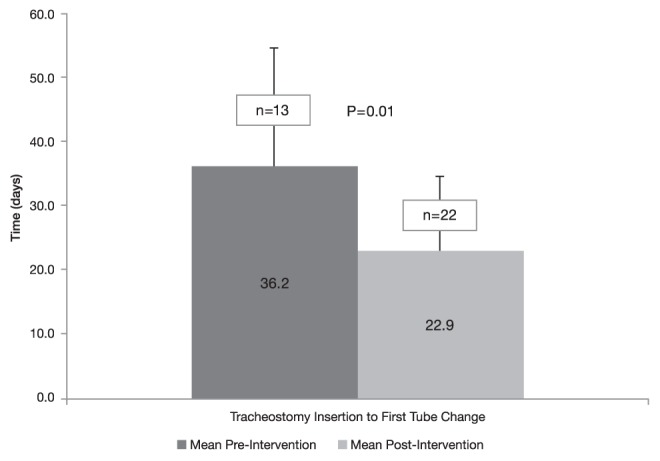
Comparison of time to first tracheostomy tube change pre- and post-interprofessional tracheostomy team implementation
Tertiary performance metrics
The time from tracheostomy insertion to weaning, or the duration of mechanical ventilation post-tracheostomy insertion, was noted to be significantly shorter in the postintervention group (11.3 days versus 28.8 days; P=0.03). Other tertiary metrics, including weaning to corking time and weaning to initial swallowing assessment, were not statistically significantly different (Table 3).
Survey results
The results of the survey completed by staff who used the tracheostomy team (n=10) revealed that 86% of staff believed that the team had improved patient care. Members of the team who completed a survey (n=12) reported that 100% found the team to be beneficial; 83% believed that the team had improved weaning to decannulation time; and 83% believed that communication between the interprofessional team had improved.
DISCUSSION
The interprofessional tracheostomy team was implemented at the Credit Valley Hospital site of Trillium Health Partners to improve the quality of care and experience for patients with a tracheostomy on the wards. The main findings after evaluation of this intervention were that there was no significant change in the primary measures of weaning to decannulation time or time to S-LP referral postweaning. It was noted, however, that there was a significant improvement in some secondary and tertiary metrics, including the time to first tracheostomy tube change and time to S-LP swallowing referral following initial tracheostomy.
Tracheostomy weaning
To proceed with tracheostomy removal, a patient must be assessed to determine the likelihood that they will tolerate decannulation. This includes corking trials to assess whether the patient can breathe around the tracheostomy tube and through their upper airway. If corking trials are not initially tolerated, it is common practice at our institution to downsize the tracheostomy tube. As demonstrated in Figure 4, our results revealed that the time to first tracheostomy tube change was significantly improved following tracheostomy team implementation. This is an important step in the weaning to decannulation process. One of the main reasons for this finding was due to the updated hospital policy, which now allowed RTs to perform the first tracheostomy tube change after 10 days. Allowing RTs to work to their full scope of practice can improve the quality of care for this patient population. Preprinted orders that were developed indicated that corking trials should last for a minimum of 24 h if tolerated. We found, however, that corking trial duration did not significantly change but was actually trending upward after implementation of the tracheostomy team. One possible reason for this is that more patients in the postintervention group had a tracheostomy inserted for airway protection, which may indicate that team members were more cautious with respect to proceeding to decannulation. This would also explain the lack of improvement postintervention in our primary metric of weaning to decannulation time. At our institution, patients with a tracheostomy are located on various wards because there is no designated, specialized unit for these types of patients. This impacts the nursing comfort levels with regard to maintenance of tracheostomies, another possible contributing factor causing no significant change in corking and weaning to decannulation times. An additional explanation for these findings is poor compliance with the protocols and preprinted orders. Tracheostomy weaning is primarily driven by the RTs in consultation with the ICU physicians and speech-language pathologists on the team. If the RTs did not strongly advocate for decannulation, patients may have been corked for a longer duration than required. In some situations, it was the physician who ultimately ordered decannulation as opposed to the RT initiating this decision. RT comfort level with tracheostomy management, as well as team dynamics, may have been factors in this lack of compliance with the preprinted orders. An additional factor may have been RT workload: during times of high acuity, routine tracheostomy care is not prioritized as highly as emergency respiratory care. Practice patterns relating to weaning from mechanical ventilation have changed throughout the course of the tracheostomy team evaluation. Modes, such as proportional assist ventilation (PAV), are being used more often, resulting in earlier weaning and less tracheostomy insertions to facilitate weaning. This may explain why more patients in the postintervention group had a tracheostomy inserted for airway protection compared with the pre-intervention group. Although a comparison of performance metrics stratified into subgroups according to indication for tracheostomy would be beneficial, it was not warranted in the present study due to the small sample sizes. This is a potential area for future research.
Improved decannulation times were likely not evident due to poor adherence with established protocols. To improve compliance, regular audits and feedback should be undertaken to encourage the team to strive for continuous improvement. An electronic system that would enable immediate data entry is one possible solution to provide real-time data to staff to improve compliance. An additional reason decannulation times did not improve was potentially related to the indication for tracheostomy increasing for airway protection as opposed to weaning from mechanical ventilation. This would also explain the lack of improvement in weaning to corking times, in that staff may have been hesitant to initiate corking trials if there was a concern about protection of the airway. Patients requiring tracheostomies for airway protection are less likely to be successfully decannulated and the time to decannulation may be longer. At our institution, we find that we have a stable population with permanent tracheostomies and only a limited number of patients entering into and leaving the tracheostomy population.
The duration of mechanical ventilation post-tracheostomy insertion was significantly shorter in the postintervention group, likely due to two possible reasons. The PAV mode of mechanical ventilation is now used more frequently in our setting both before and following percutaneous tracheostomy. Improved weaning practices can explain the decrease of 17.5 days in time from tracheostomy insertion to weaning. The second possible explanation for this difference is that more patients had a tracheostomy inserted for airway protection in the postintervention group as opposed to a failure to wean from mechanical ventilation, indicating that the requirement for mechanical ventilation was lessened once a patient had their endotracheal tube replaced with a tracheostomy tube.
S-LP referral and assessment
The primary measure of time from weaning to S-LP referral did not reveal a statistically significant change with the implementation of the interprofessional tracheostomy team but did shorten it by 7.8 days, which has clinical implications on the quality of patient care. Our tertiary metric of time from weaning to initial swallowing assessment was also shortened (by 3.4 days); however, this was not statistically significant. Before implementation of the team, S-LP staff members were not informed of all patients who had a tracheostomy and some patients may have been started on oral nutrition without a formal swallowing assessment by a speech-language pathologist, thereby increasing the risk for aspiration and potential complications during the patient’s stay. For a speech-language pathologist to see a patient for swallowing or communication, a physician referral was necessary, putting the onus on the physician to initiate this referral for timely patient care. However, having preprinted orders as part of the process with the tracheostomy team for all tracheostomy patients ensured an automated notification process for S-LP. Also, as evident in the postimplementation survey, having an interprofessional tracheostomy team present meant better communication between S-LP and RTs, enabling the speech-language pathologist to determine candidacy for a swallowing assessment. With timely S-LP services, patients could be placed on the most appropriate diet textures and liquid consistencies to decrease aspiration risk and, ultimately, improve the quality of patient care. Apart from swallowing assessments and management, speech-language pathologists also had the opportunity to work closely with RTs to determine candidacy of speaking valves, which may have improved a patient’s quality of life.
Our secondary metric of tracheostomy insertion to S-LP referral time significantly improved following the tracheostomy team initiative. Duration of mechanical ventilation was noted to be shorter in the postintervention group, which may have confounded the metric of tracheostomy insertion to S-LP referral time. Based on our results, we would expect the time for this metric to decrease, on average, by 17.5 days; however, we witnessed a difference of 25.5 days. An explanation for the significant improvement in this measure was the use of the preprinted orders. Although the orders were designed to be implemented after weaning from mechanical ventilation, some patients were started on the orders sooner, which allowed for an earlier automated S-LP notification while the patient remained in the ICU.
Limitations and challenges
One of the main limitations of the tracheostomy team evaluation was difficulty with data collection. Data collection for the postintervention group was incomplete; therefore, retrospective chart reviews were undertaken. In our institution, the health record is mostly paper based and is scanned electronically postdischarge. Some performance metrics were only captured in narrative notes; therefore, it was challenging to review large volumes of notes to obtain the required information. In some cases, we were unable to find the data required; therefore, approximately seven patient records from the postintervention group were not included in the results. This further limited the sample size for the pre- and postintervention groups. Another limitation we identified in this study was the heterogeneity between pre- and postintervention indications for tracheostomy. The majority of patients in both groups had a primary indication for tracheostomy of facilitation of weaning; however, there was a higher percentage of airway protection as the primary indication in the postintervention group. This difference between groups can be explained by the aforementioned increased use of weaning modes, such as PAV, resulting in less need for percutaneous tracheostomy due to a failure to wean from mechanical ventilation.
CONCLUSION
Before the implementation of the tracheostomy team, patients on the wards with a tracheostomy often did not receive regular follow-up and management with respect to weaning and decannulation. Our evaluation indicates that an interprofessional tracheostomy team can improve the quality of patient care by earlier tracheostomy tube changes and facilitating swallowing referrals in a timelier manner. Our assessment did not demonstrate an improvement in weaning to decannulation times, unlike previous studies (3). Despite the lack of improved weaning to decannulation times, other key processes in the weaning continuum were evident including marked improvement in the initial S-LP referral times following tracheostomy insertion. To validate these findings in other institutions, a more rigorous quality improvement methodology should be used, along with ongoing protocol compliance measurement.
Acknowledgments
The authors thank the Institute for Better Health (IBH), Trillium Health Partner’s research institute, for their contribution to this work. They provided guidance on the data analysis and supported the drafting and critical appraisal of the manuscript. They also thank Gail Lang and Sharyn Gibbins from Trillium Health Partners for their support and guidance with the development of the interprofessional tracheostomy team at Credit Valley Hospital site. Finally, the authors thank Norm Tiffin for his assistance with the statistical analysis for this study.
Footnotes
DISCLOSURES: The authors have no financial disclosures or conflicts of interest to declare.
REFERENCES
- 1.Durbin CG. Indications for and timing of tracheostomy. Respir Care. 2005;50:483–7. [PubMed] [Google Scholar]
- 2.De Mestrel C, Iqbal M, Fong N, et al. Impact of a specialized multidisciplinary tracheostomy team on tracheostomy care in critically ill patients. Can J Surg. 2011;54:167–72. doi: 10.1503/cjs.043209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tobin AE, Santamaria JD. An intensivist-led tracheostomy review team is associated with shorter decannulation time and length of stay: A prospective cohort study. Crit Care. 2008;12:R48. doi: 10.1186/cc6864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Speed L, Harding KE. Tracheostomy teams reduce total tracheostomy time and increase speaking valve use: A systematic review and meta-analysis. J Crit Care. 2013;28:216.e1–216.e10. doi: 10.1016/j.jcrc.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 5.Smith KA, Matthews TW, Dubé M, Spence G, Dort JC. Changing practice and improving care using a low-risk tracheotomy clinical pathway. JAMA Otolaryngol Head Neck Surg. 2014;140:630–4. doi: 10.1001/jamaoto.2014.921. [DOI] [PubMed] [Google Scholar]