Abstract
Introduction
If nonoperative treatment for lumbar stenosis fails, surgery may be considered. This traditionally includes decompression often combined with fusion. Desire for less extensive surgery led to developing new techniques and implants, including an interlaminar device designed with the goal of providing segmental stability without fusion, following decompression. The purpose of this study was to investigate 5-year outcomes associated with an interlaminar device.
Methods
This prospective, randomized, controlled trial was conducted at 21 centers. Patients with moderate to severe lumbar stenosis at one or two contiguous levels and up to Grade I spondylolisthesis were randomized (2:1 ratio) to decompression and interlaminar stabilization (D+ILS; n=215) using the coflex® Interlaminar Stabilization® device (Paradigm Spine, LLC) or decompression and fusion with pedicle screws (D+PS; n=107). Clinical evaluations were made preoperatively and at 6 weeks and 3, 6, 12, 18, 24, 36, 48, and 60 months postoperatively. Overall Food and Drug Administration success criteria required that a patient meet 4 criteria: 1) >15 point improvement in Oswestry Disability Index (ODI) score; 2) no reoperation, revision, removal, or supplemental fixation; 3) no major device-related complication; and 4) no epidural steroid injection after surgery.
Results
At 5 years, 50.3% of D+ILS vs. 44% of D+PS patients (p>0.35) met the composite success criteria. Reoperation/revision rates were similar in the two groups (16.3% vs. 17.8%; p >0.90). Both groups had statistically significant improvement through 60 months in ODI scores with 80.6% of D+ILS patients and 73.2% of D+PS patients demonstrating >15 point improvement (p>0.30). VAS, SF-12, and ZCQ scores followed a similar pattern of maintained significant improvement throughout follow-up. On the SF-12 and ZCQ, D+ILS group scores were statistically significantly better during early follow-up compared to D+PS. In the D+ILS group, foraminal height, disc space height, and range of motion at the index level were maintained through 5 years.
Conclusion
Both treatment groups achieved and maintained statistically significant improvements on multiple outcome assessments throughout 5-year follow-up. On some clinical measures, there were statistically significant differences during early follow-up favoring D+ILS. At no point were there significant differences favoring D+PS. Results of this 5-year follow-up study demonstrate that decompression and interlaminar stabilization with coflex is a viable alternative to traditional decompression and fusion in the treatment of patients with moderate to severe stenosis at one or two lumbar levels.
Level of Evidence and Ethical Statements
This is a Level I study. Institutional approval was received at each of the sites participating in the trial. Each patient gave informed consent to participate in the trial.
Keywords: interlaminar device, spinal stenosis, lumbar spine, decompression, instrumented fusion, clinical outcome, randomized study
Introduction
With the steadily rising elderly population, the number of patients seeking care for lumbar spinal stenosis is likely to increase also. Traditional conservative care management including physical therapy, pain management, epidural steroid injections, and modification of activities of daily life often do not provide substantial improvement in symptoms. Results of the SPORT study found that surgical care is more effective than ongoing nonoperative care in patients with stenotic symptoms persisting more than 12 weeks.1 When surgical intervention is considered, the goal is to provide significant and sustainable pain relief with the least risk of complications and minimal amount of tissue disruption. The desire for minimally invasive treatment of stenosis led to the development of interspinous spacers with the goal of providing adequate indirect decompression of neural tissue to alleviate symptoms. These implants are primarily described for the treatment of intermittent neurogenic claudication related to stenosis with or without back pain. While good results were reported,2–5 other studies suggest that interspinous devices may not offer any benefit compared with traditional decompressive surgery and may be associated with a higher reoperation rate.6–9 However, it should be noted that patient selection is critical to gaining good outcomes, and in some studies this was not well described with respect to using the same indications applied in the prospective, randomized, large-scale clinical trials. In patients with lumbar stenosis and back pain of greater severity than leg pain, decompression was not as effective as desired in reducing back pain.10 An interlaminar device to be implanted after surgical decompression for stenosis has been developed. Results of a prospective nonrandomized study found decompression significantly reduced leg pain and back pain and that the implantation of the interlaminar device in addition to decompression resulted in significantly greater improvement in leg and back pain compared with decompression alone.11 Other investigators have suggested that interlaminar stabilization (ILS) may provide a benefit in the short-term, but, based on radiographic measures, suggested the results would not be sustainable over time.12 Davis, et al.13 reported significant improvements with ILS after decompression compared with posterior fusion with pedicle screws at 2-year follow-up in a prospective randomized study. The purpose of this study was to compare open microsurgical decompression and fusion using pedicle screws with autograft (D+PS) to open microsurgical decompression and interlaminar stabilization, using the coflex® (Paradigm Spine, LLC) (D+ILS) in patients with moderate to severe lumbar spinal stenosis at one or two contiguous levels, back pain, and up to Grade I spondylolisthesis, with five-year follow-up to determine the long-term outcomes.
Methods and Materials
Study Design
A full description of the study design and inclusion/exclusion criteria was previously published by Davis et al.13 This multicenter, prospective, randomized, controlled trial was conducted at 21 sites in the United States under institutional review board approval. The study was initiated in 2006 and final follow-up was completed in January 2015. The 5-year follow-up rate was 91%.
Patients between the ages of 40 and 80 years were required to meet strict inclusion and exclusion criteria including: (1) minimum Oswestry Disability Index (ODI) score of at least 40%; and (2) visual analogue scale (VAS) back pain score of at least 50 of 100. Patients were enrolled using a 2:1 ratio of investigational to control groups. Study subjects were blinded to treatment group assignment until after surgery.
Clinical Outcomes Measures
Clinical outcomes assessments were made at baseline and at each of the following postoperative time points: 6 weeks, and 3, 6, 12, 18, 24, 36, 48, and 60 months. Outcomes measures evaluated included ODI, VAS separately assessing back and leg pain, the Zurich Claudication Questionnaire (ZCQ), and the Short Form-12 (SF-12). Neurological evaluation included motor, sensory, and reflex assessments. A patient was considered to have a successful neurological outcome if there was maintenance or improvement when comparing the postoperative assessment to the preoperative. Overall FDA success criteria or composite clinical success (CCS) required a patient to meet the following 4 end points: 1) improvement of at least 15 points in ODI (ODI-15) at 60 months compared with baseline; 2) no reoperations, revisions, removals, or supplemental fixation; 3) no major device-related complications, including but not limited to permanent new or increasing sensory or motor deficit at 60 months; and 4) no lumbar epidural steroid injection at any postoperative time point. Once a patient had either an injection or a secondary procedure, the patient was deemed a failure and no longer part of the analysis. All endpoints were evaluated for patients at each time point that had not had an epidural injection or secondary procedure. At Month 60, additional surgery and/or injections after the index surgery was performed in 67 of 215 (31.2%) of patients in the D+ILS group and 36 of 107 (33.6%) in the D+PS group.
In addition to the minimum 15 point improvement on ODI scores as a measure of favorable clinical outcome for a patient, the percentage of patients improving at least 20 points on the back and leg pain VAS scores was calculated and compared between the two groups.
Radiographic Outcomes Measures
In the D+ILS cohort, upright neutral lateral, flexion and extension radiographs were obtained at each time point. In the fusion control cohort, the same radiographical data was obtained, with the exception of flexion and extension radiographs, which were with-held at the 6-week and 3-month time points. All radiographic images were sent directly from the study sites to an independent core radiography laboratory (Medical Metrics Inc., Houston, TX) for evaluation.
Statistical Analysis
The primary efficacy endpoint for this study was Month 60. To achieve Month 60 CCS, a patient had to be a success in all 4 endpoints. Additionally, linear improvements were analyzed for each patient-derived questionnaire. Group comparisons included t-tests for comparing means, computation of standardized effect sizes (mean difference divided by pooled standard deviation), Chi-square and Fisher exact tests to compare categorical outcomes, graphical analyses, and correlational analyses. The analysis of patient accountability revealed a 60 month clinical and radiographic follow-up rate of 91%.
Results
Composite Clinical Success (CCS)
At 5-year follow-up, 50.3% of D+ILS patients met the success criteria compared with 44% of D+PS patients (p>0.35). Although the difference between the two groups was not significant, it is noteworthy that at all time points, the CCS percentage was higher in D+ILS group (Table 1). Moreover, within the 2-level cohort at Month 60, there was a trend for a greater percentage of D+ILS patients achieving success than D+PS patients (55.1% vs. 35.3%; 0.05<p<0.065)
Table 1.
Month 60 overall efficacy of subjects achieving clinical success defined by the individual components of success.
| D+ILS | D+PS | ||||||
|---|---|---|---|---|---|---|---|
| Status pre-op compared with Month 60 | N assessed | N meeting criterium | % | N assessed | N meeting criterium | % | p-value |
| Improvement of≥15 points in ODI at Month 60 compared to baseline | 124 | 100 | 80.6 | 55 | 41 | 74.5 | >0.40 |
| No reoperation or epidural steroid injection | 215 | 148 | 68.8 | 107 | 71 | 66.4 | >0.70 |
| No reoperations, revisions, removals, or supplemental fixation | 215 | 179 | 83.3 | 107 | 89 | 83.2 | >0.90 |
| No epidural injection at any lumbar level | 215 | 173 | 80.5 | 107 | 82 | 76.6 | >0.40 |
| No persistent new or increasing sensory or motor deficit | 88 | 83 | 94.3 | 40 | 40 | 100.0 | >0.30 |
| No persistent new or increasing sensory deficit | 148 | 143 | 96.6 | 66 | 66 | 100.0 | >0.30 |
| No persistent new or increasing motor deficit | 146 | 144 | 98.6 | 74 | 72 | 97.3 | >0.60 |
| No major device-related complications | 215 | 212 | 98.6 | 107 | 102 | 95.3 | >0.10 |
| Composite Clinical Success (Month 60 CCS-FDA) | 191 | 96 | 50.3 | 91 | 40 | 44.0 | >0.30 |
Secondary Surgical Procedures (reoperations, revisions, removals, or supplemental fixation) or Epidural Steroid Injections
At 24 months, as previously reported, the reoperation rate for the D+ILS group was 23/215 (10.7%) and the D+PS was 8/107 (7.5%) and was not significant (p>0.40). At 60 months, there was also no significant difference in the cumulative total occurrences of reoperations/revisions between the D+ILS group 35/215 (16.3%) and D+PS group 19/107 (17.8%) (p>0.90). The reoperations/revisions were divided into 5 categories: (1) Wound-related; (2) Under-treatment; (3) Device-related; (4) Ineffective (a) less than 2 years or (b) between 2 and 5 years; or (5) Trauma (Table 2). Categories 1 and 2 were early postoperative revisions that can be considered surgery-related. In patients with wound-related reoperations, there were 7 D+ILS patients (3.3%) and 1 D+PS patient (0.09%). Among patients classified as under-treated, there were 5 D+ILS patients (2.3%) and 2 D+PS patients (1.9%) who underwent early revisions such as re-decompression or poor patient selection/surgical planning requiring additional surgery. Among device-related reoperations, the most common issue in the D+ILS group was a pars fracture in comparison to the D+PS group where the most common issue involved broken instrumentation. There were more than twice as many devicerelated reoperations in the D+PS group compared to the D+ILS group with 6 patients in the D+ILS (2.8%) and 7 patients in the D+PS group (6.5%). The reoperation group classified as ineffective treatment to manage the condition and was further stratified into early and late revisions. In the D+ILS group, there were 7 (3.3%) early and 9 (4.2%) late revisions. In comparison, the D+PS group reported a two-fold increase between the early and late phases where there was 3 (2.8%) early and 6 (5.6%) late revisions. There was one motor vehicle accident in the D+ILS group requiring revision and was classified as a trauma.
Table 2.
Classification of reoperations/revisions by category.
| Reoperation Category | D+ILS (N=215) n (%) |
D+PS (N=107) n (%) |
|---|---|---|
| (1) Wound/surgery related | 7 (3.3%) | 1 (1.0%) |
| (2) Under treatment | 5 (2.3%) | 2 (1.9%) |
| (3) Device related issue | 6 (2.8%) | 7 (6.5%) |
| (4) Device ineffective | ||
| A. Early (≤ 2 years post-op) | 7 (3.3%) | 3 (2.8%) |
| B. Late (> 2 years post-op) | 9 (4.2%) | 6 (5.6%) |
| (5) Trauma | 1 (0.5%) | 0 |
| Total | 35 (16.3%) | 19 (17.8%) |
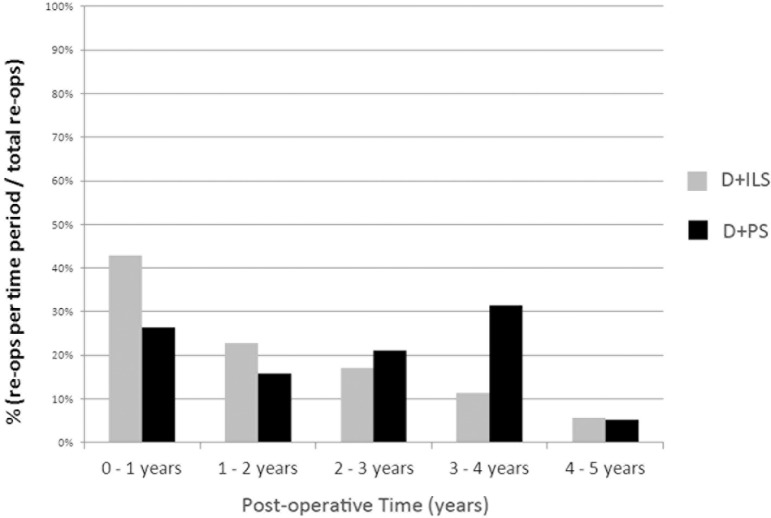
In addition to the reoperation/revision types, the timeframe for reoperation was also analyzed. In Figure 1, the reoperations/revisions were stratified by postoperative year as a percentage of the total reoperations/revisions for each treatment group. Many of the D+ILS reoperations/revisions occurred within the first year (42.9%; 15/35) with a decreasing trend over 5 years. In comparison, the majority of reoperations/revisions in the D+PS group occurred in years 2 through 4 accounting for 52.6% of the total reoperations/revisions in that group.
Fig. 1.
Among patients who were reoperated, the percentage of those reoperations in each of the annual time periods. In the D+ILS group, reoperations occurred earlier than in the D+PS group.
By Month 60, 80.5% of the D+ILS group had not received an epidural injection (ESI) at any level in the lumbar spine compared with 76.6% of the D+PS group (p>0.45). The combination of the absence of ESI or secondary surgery defined the primary endpoint. At Month 60, there was not a significant difference between the two treatments with 68.8% D+ILS vs. 66.4% fusion group achieving the primary endpoint (p>0.70). However, within the 2-level cohort, there is a significant difference in the primary endpoint with 68.8% D+ILS vs. 48.7% D+PS (p<0.05) achieving success.
Major device-related complications
There were 3/215 major device related complications in the D+ILS group and 5/107 in the fusion group at Month 60 (1.4% vs. 4.7%; p>0.10).
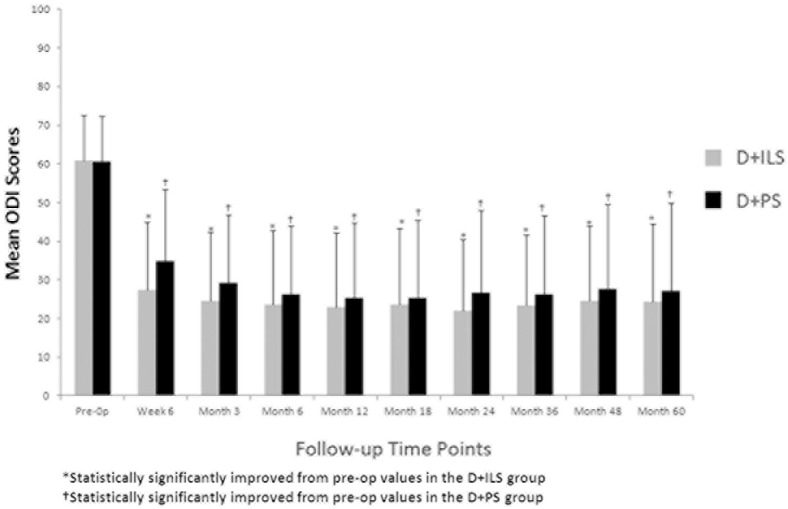
Oswestry Disability Index (ODI)
For the purposes of analyzing CCS, ODI data was censored to include into the analysis only patients that did not have a secondary surgical procedure or epidural injection. At Month 60, additional surgery and/or injections after the index surgery was performed in 67 of 215 (31.2%) of patients in the D+ILS group and 36 of 107 (33.6%) in the D+PS group. Patients in both treatment groups had significant sustained improvement from baseline to 60 months postoperative (Figure 2). The D+ILS group consistently had a larger percentage of patients achieving a 15 point improvement in each year of follow-up over 5 years. At 5 years, 80.6% for D+ILS and 73.2% for fusion (p>0.30) achieved a clinically significant ODI-15 (Figure 3). Interestingly, in the uncensored patient population, a significant difference for follow-up time points Week 6, Month 3, Month 24, Month 36, Month 48, and Month 60 with a higher percentage of D+ILS patients achieving 15 point improvement (p<0.05).
Fig. 2.
Mean ODI scores improved significantly in both groups and remained improved throughout follow-up. Error bars represent the standard deviation.
Fig. 3.
Percentage of patients achieving ≥15 point decrease in ODI scores compared to baseline at each follow-up time point.
Secondary EndpointsVisual Analogue Scale (VAS)
VAS scores were collected for both back pain and for worse leg pain. At baseline, mean VAS back and worse leg pain were similar between groups. Both groups showed significant improvement from baseline in both back and leg pain at all time points out to 60 months (Figure 4). At Month 60, 99.2% of the D+ILS group reported ≥ 20 point improvement in VAS leg pain as did 96.2% of the D+PS group (p>0.20). Further, ≥ 20 point improvement in VAS back pain was achieved by Month 60 in 85.2% of D+ILS compared to 77.8% of D+PS patients (p>0.25).
Fig. 4.
Mean VAS back pain scores (A) and worse leg pain scores (B) improved significantly in both groups and remained improved throughout follow-up. Error bars represent the standard deviation.
Short-form 12 (SF-12)
At Month 60, 87.5% of the D+ILS group and 75.6% of the fusion group reported maintenance or improvement of the physical component score (PCS) of the SF-12. The SF-12 PCS scores were significantly different at Week 6 and Month 3 postoperative favoring D+ILS. From Month 6 to Month 60, scores were consistent with no deterioration but were not statistically different between treatments.
Zurich Claudication Questionnaire (ZCQ)
The ZCQ is separated into components of symptom severity, physical function, and patient satisfaction. With regards to the symptom severity, scores improved significantly in both groups from baseline by Week 6 and were significant favoring the D+ILS group (p<0.01). The improvement was maintained from Week 6 to Month 60 where mean values were consistently lower for the D+ILS group. The ZCQ symptom severity improvement of at least 0.5 was assessed per patient where 79.8% of D+ILS and 72.7% of D+PS (p>0.30) met that criteria (Figure 5A). The physical function improved from baseline to Month 3 and remained stable through Month 60 in both groups where the D+ILS mean values were consistently lower than D+PS at all time points and was significant favoring D+ILS at Week 6 (p<0.015), Month 3 (p< 0.01), and Month 24 (p<0.01). The ZCQ physical function improves at least 0.5 was assessed per patient where 78.2% of D+ILS and 70.9% of D+PS patients met the criteria but the difference between groups (p>0.30) was not significant (Figure 5B). The third component of patient satisfaction was consistent from Week 6 to Month 60 in both groups favoring D+ILS at all time points reaching statistical significance at Week 6 (p<0.01), Month 3 (p<0.01), Month 6 (p<0.01), Month 24 (p<0.01) and Month 36 (p<0.03; Figure 5C).
Fig. 5.
Zurich Claudication Questionnaire Scores on the symptom severity (A), physical function (B) and patient satisfaction (C) scales.
Narcotic Usage
Prior to surgery, more than 50% of patients were taking narcotics (52.6% D+ILS: 53.3% D+PS; p>0.90). There was a 35% improvement from pre-operative usage by Month 3 in the D+ILS and by Month 6 in the D+PS group. From Month 6 to Month 60, the percentage of patients using narcotics remained consistent in the D+ILS group and was sustained between 22-29% of the cohort. In comparison, the percentage of patients in the D+PS cohort using narcotics was less, with wider ranges from 20.8 to 38.3% between Month 6 and Month 60. There was no significant difference between the two groups at Month 60 but both groups were significantly improved from their preoperative status (Table 3).
Table 3.
Percentage of patients using narcotics to manage pain at each time point.
| Narcotics Usage | |||
|---|---|---|---|
| D+ILS (%) n=215 |
D+PS (%) n=107 |
p (Fisher's Exact) | |
| Pre-op | 52.6 | 53.3 | >0.90 |
| Week 6 | 46.0 | 54.2 | >0.10 |
| Month 3 | 34.4 | 44.9 | >0.08 |
| Month 6 | 29.8 | 34.6 | >0.40 |
| Month 12 | 28.0 | 38.3 | >0.40 |
| Month 18 | 22.3 | 29.0 | >0.20 |
| Month 24 | 23.3 | 33.6 | >0.06 |
| Month 36 | 23.3 | 22.4 | >0.90 |
| Month 48 | 23.7 | 20.6 | >0.50 |
| Month 60 | 23.7 | 24.3 | >0.90 |
Radiologic Assessment
The index level range of motion in the D+ILS group remained consistent from preoperative (4.56° ± 3.86°) to Month 60 (3.13° ± 3.43°). As intended, the fusion group's range of motion was significantly different (p<0.01) from preoperative (4.15° ± 3.33°) to Month 60 (0.98° ± 1.17°), radiographic fusion. Motion at the superior adjacent level to the D+ILS treatment was sustained and remained relatively unchanged from preoperative (4.16° ± 3.49°) to Month 60 (3.52° ± 3.16°). Interestingly, the adjacent level motion superior to the D+PS treatment increased from pre-operatively (3.68° ± 2.99°) to Month 24 (5.60° ± 4.62°), then decreased to Month 60 (3.59° ± 2.89°). The range of motion at the adjacent level was significantly different between the D+ILS and fusion treatments at Month 6, Month 24, Month 36, and Month 48.
Focusing on the D+ILS treatment group, the foraminal height was not different from preoperative (17.80 mm ± 2.66) through Month 60 (17.33mm ± 2.75). The disc height was not different from preoperative (7.73 mm ± 2.45) through Month 60 (6.67mm ± 2.25).
Discussion
This study analyzed the 5 year results of a prospective, randomized, controlled clinical trial evaluating visualized microsurgical decompression augmented with interlaminar stabilization as compared to decompression with instrumented posterolateral spinal fusion at one or two levels for the treatment of moderate to severe lumbar spinal stenosis. This patient population is somewhat controversial as these patients had to have substantial back pain; however, they may or may not have spondylolisthesis, and their care continuum is not well defined. While decompression alone may alleviate radicular symptoms in some patients, there is the possibility that the procedure may contribute to instability, which may generate symptoms later. Traditionally in such patients for whom decompression-related instability was a concern, as well as those with significant back pain, fusion was often performed to stabilize the spine with the hope of relieving pain and preventing future problems. The current study was designed to compare outcomes of using an interlaminar device, rather than fusion, in this population.
One recent study evaluated interlaminar stabilization following decompression for lumbar spinal stenosis in patients with low back pain scores of at least 5 on a 10 point scale.14 The data were collected from two European registries and patients carefully matched between those receiving coflex after decompression and those receiving decompression alone. The group receiving the interlaminar device had significantly better results based on several outcome assessments, with a high rate of satisfaction in both treatment groups. In the current study, one of the inclusion criteria was a minimum back pain score of 50/100. Our results support those published in the European study. The preoperative back pain scores were high and improved significantly by 6 weeks after surgery and remained stable and improved throughout the 5-year follow-up. The results demonstrate the sustainability and durability of decompression and interlaminar stabilization when utilizing the coflex device. One prospective, non-randomized study with 30 patients per treatment group reported no significant benefit of adding an interlaminar device after decompression for spinal stenosis.15 Of note, in that study, patients with instability were excluded and there was no consideration of back pain either as a selection criterion or on outcome measure.
One criticism of the current study may be not including a control group receiving decompression only. It is a classic question of whether decompression alone is indicated vs. fusion vs. instrumented fusion is the most effective treatment for various severities of lumbar spinal stenosis. Unfortunately to date there is no definitive answer for which procedure is best for which patients. Decompression alone is effective in some patients; however, if instability is a concern, fusion is often performed. The population included in the current study were patients with moderate to severe stenosis at one or two levels with up to Grade I spondylolisthesis and, very importantly, who had back pain with severity of at least 50 of 100. This tends to be the population where fusion is more likely to be performed rather than decompression alone. The study was designed to evaluate Coflex as a fusion alternative in such patients and not as a decompression add-on in patients for whom the surgeon thinks decompression alone can adequately address the patient's symptoms. Therefore a decompression only group was not included in the design and may not be the typical procedure for this specific subset of patients with stenosis.
Optimizing cost-effectiveness of healthcare is a rising priority. A recently published Milliman study16 found a significant reduction of per member per month patient costs of employer owned health plans when decompression and ILS was an alternative to traditional spinal fusion for stabilization in this patient group. One study compared the cost-effectiveness study of coflex to instrumented posterior fusion over the course of five years.17 The authors found that the interlaminar device provided higher utility and was significantly less costly. The favorable cost-effectiveness was even more pronounced in 2-level procedures.
One important factor in evaluating any spine surgical procedure is revision surgery. This is important to patient safety and well-being as well as having significant cost implications. As a cumulative total, the D+ILS group performed as well as the D+PS group on this measure. However, upon further examination, it appeared that some of the D+ILS revision surgeries could be explained as “learning curve” issues such as wound closure problems, poor surgical planning resulting in under treatment requiring additional surgery at the index and adjacent levels within days to a few months postoperatively, or poor patient selection resulting in ineffective treatment within 2 years. These three categories accounted for more than half of revisions in the D+ILS group. In comparison, these three categories resulted in only 32% of revisions in the D+PS group. Focusing on the categories of durability and sustainability, the D+PS group had a 6.5% rate of device-related failure requiring revision and 5.6% late-term ineffective treatment revisions thereby an effective 12.1% revision rate. In comparison, the D+ILS group had a 2.8% rate of device-related revisions and a 4.2% late-term ineffective treatment revisions resulting in an effective 7% revision rate with regard to durability and sustainability during 5-year follow-up. These results refute the supposition of an earlier author12 that the results achieved using an interlaminar device would not be sustainable in the long-term.
The time to reoperation/revision surgery followed a different pattern in the two treatment groups. Within the reoperations/revisions that occurred, most of the D+ILS cases occurred within the first year after the index surgery. This is consistent with the categorization of the incidents and supports a “learning curve” scenario. In following years, the number of reoperations/revisions decreased suggesting that outcomes are sustainable in properly selected patients. However, the majority of fusion reoperations/revisions occurred between Month 24 and Month 48. These cases are not a consequence of learning a new technology but may represent a slow deterioration leading to subsequent surgery.
For all patient-derived parameters, there was statistically significant improvement maintained through 5 years for both groups. At 5 years, more than 99% of D+ILS patients achieved pain improvement of at least 20 mm in VAS leg pain and over 80% achieved at least 15 point improvement in ODI. By all patient-derived parameters, the treatments were found to produce similar results. Although not significantly different, a greater percentage of D+ILS patients at all follow-up time points achieved at least 15 point improvement in ODI, and at least 20 mm VAS leg pain and VAS back pain improvement compared to the D+PS group. Thus there was no suggestion that the interlaminar device produced outcomes inferior to fusion's. By the CCS, a patient was classified as a failure if that patient had an epidural injection or a reoperation. Reviewing the uncensored data for 15 point improvement in ODI, it highlighted an interesting finding showing a significant difference early and sustained late improvement favoring D+ILS. This finding is important because it shows that although a patient may hit a setback in their healing continuum, overall patients experienced less disability and greater success at activities of daily life after D+ILS procedure compared to fusion.
The study did have some limitations. The study was not blinded during follow-up. Clinically, this would be very difficult to achieve, but may have introduced a bias. There is always difficulty in determining how to address patients who undergo additional surgery or injections after the study surgery, as their outcome measures may then be reflecting the effect of the additional intervention rather that the index procedure. In the current protocol, these patients were classified outcome failures in the composite assessment of success, and excluded from the analyses of individual outcome assessments such as VAS and ZCQ.
Conclusion
The results of this study with 5-year follow-up support that decompression and ILS is an effective and sustainable treatment option for moderate to severe spinal stenosis and not an inevitable precursor to fusion. ILS after decompression produces outcomes similar or superior to fusion with pedicle screws. One and two levels yield equally good results compared to fusion. Two level D+ILS procedures had a significantly lower rate of revision than fusion procedures. Reductions in VAS back and leg pain were significant and sustainable in both groups.
Disclosures
Michael Musacchio has received consulting fees and honoraria from Paradigm Spine (the manufacturer of the device in this study), Medtronic, Centinel Spine, and RTI. Carl Lauryssen has received royalties from Medtronic and DePuy and has stock options in Paradigm Spine, Spinal Kinetics, and Spinal Elements. Reginald Davis is a consultant to Zimmer Biomet, LDR, Paradigm Spine, Zyga, and Medacta. Hyun Bae is a consultant for Paradigm Spine and owns stock in Paradigm Spine. John Peloza has acted as consultant to 4Web, K2M, Medtronic, Paradigm Spine, RTI, SpineView, and Expanding Orthopedics and received royalties from DePuy Synthes. Richard Guyer is a consultant to K2M, DePuy Synthes, Safe Orthopedics, and Paradigm Spine; has received royalties from Alphatel, and has stock options in Spinal Kinetics. Jack Zigler owns stock in Paradigm Spine. Donna Ohnmeiss is employed by an organization that has received institutional research support from the study sponsor. Scott Leary owns stock in and has been a paid consultant and speaker for Paradigm Spine.
References
- 1.Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med. 2008;358:794–810. doi: 10.1056/NEJMoa0707136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zucherman JF, Hsu KY, Hartjen CA, et al. A multicenter, prospective, randomized trial evaluating the X STOP interspinous process decompression system for the treatment of neurogenic intermittent claudication: Two-year follow-up results. Spine. 2005;30:1351–8. doi: 10.1097/01.brs.0000166618.42749.d1. [DOI] [PubMed] [Google Scholar]
- 3.Patel VV, Whang PG, Haley TR, et al. Two-year clinical outcomes of a multicenter randomized controlled trial comparing two interspinous spacers for treatment of moderate lumbar spinal stenosis. BMC Musculoskelet Disord. 2014;15:221. doi: 10.1186/1471-2474-15-221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kuchta J, Sobottke R, Eysel P, et al. Two-year results of interspinous spacer (x-stop) implantation in 175 patients with neurologic intermittent claudication due to lumbar spinal stenosis. Eur Spine J. 2009;18:823–9. doi: 10.1007/s00586-009-0967-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buric J, Pulidori M. Long-term reduction in pain and disability after surgery with the interspinous device for intervertebral assisted motion (diam) spinal stabilization system in patients with low back pain: 4-year follow-up from a longitudinal prospective case series. Eur Spine J. 2011;20:1304–11. doi: 10.1007/s00586-011-1697-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moojen WA, Arts MP, Jacobs WC, et al. Interspinous process device versus standard conventional surgical decompression for lumbar spinal stenosis: Randomized controlled trial. BMJ. 2013;347:f6415. doi: 10.1136/bmj.f6415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stromqvist BH, Berg S, Gerdhem P, et al. X-stop versus decompressive surgery for lumbar neurogenic intermittent claudication: Randomized controlled trial with 2-year follow-up. Spine. 2013;38:1436–42. doi: 10.1097/BRS.0b013e31828ba413. [DOI] [PubMed] [Google Scholar]
- 8.Patil CG, Sarmiento JM, Ugiliweneza B, et al. Interspinous device versus laminectomy for lumbar spinal stenosis: A comparative effectiveness study. Spine J. 2014;14:1484–92. doi: 10.1016/j.spinee.2013.08.053. [DOI] [PubMed] [Google Scholar]
- 9.Wu AM, Zhou Y, Li QL, et al. Interspinous spacer versus traditional decompressive surgery for lumbar spinal stenosis: A systematic review and metaanalysis. PLoS One. 2014;9:e97142. doi: 10.1371/journal.pone.0097142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kleinstuck FS, Grob D, Lattig F, et al. The influence of preoperative back pain on the outcome of lumbar decompression surgery. Spine. 2009;34:1198–203. doi: 10.1097/BRS.0b013e31819fcf35. [DOI] [PubMed] [Google Scholar]
- 11.Kumar N, Shah SM, Ng YH, et al. Role of Coflex as an adjunct to decompression for symptomatic lumbar spinal stenosis. Asian Spine J. 2014;8:161–9. doi: 10.4184/asj.2014.8.2.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Park SC, Yoon SH, Hong YP, et al. Minimum 2-year follow-up result of degenerative spinal stenosis treated with interspinous u (coflex) J Korean Neurosurg Soc. 2009;46:292–9. doi: 10.3340/jkns.2009.46.4.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davis RJ, Errico TJ, Bae H, et al. Decompression and Coflex(r) interlaminar stabilization compared to decompression and instrumented spinal fusion for spinal stenosis and low-grade degenerative spondylolisthesis: Two-year results from the prospective, randomized, multicenter Food and Drug Administration Investigational Device Exemption trial. Spine. 2013;38:1529–39. doi: 10.1097/BRS.0b013e31829a6d0a. [DOI] [PubMed] [Google Scholar]
- 14.Roder C, Baumgartner B, Berlemann U, et al. Superior outcomes of decompression with an interlaminar dynamic device versus decompression alone in patients with lumbar spinal stenosis and back pain: A cross registry study. Eur Spine J. 2015;24:2228–35. doi: 10.1007/s00586-015-4124-6. [DOI] [PubMed] [Google Scholar]
- 15.Richter A, Halm HF, Hauck M, et al. Two-year follow-up after decompressive surgery with and without implantation of an interspinous device for lumbar spinal stenosis: A prospective controlled study. J Spinal Disord Tech. 2014;27:336–41. doi: 10.1097/BSD.0b013e31825f7203. [DOI] [PubMed] [Google Scholar]
- 16.Fitch K, Blumen H, Engel T. Milliman Client Report. 2015. Utilization and cost of surgery for lumbar spinal stenosis in a commercially insured population; pp. 1–18. [Google Scholar]
- 17.Schmier JK, Halevi M, Maislin G, et al. Comparative cost effectiveness of Coflex(r) interlaminar stabilization versus instrumented posterolateral lumbar fusion for the treatment of lumbar spinal stenosis and spondylolisthesis. Clinicoecon Outcomes Res. 2014;6:125–31. doi: 10.2147/CEOR.S59194. [DOI] [PMC free article] [PubMed] [Google Scholar]