Abstract
Objective
This study aimed to compare the effectiveness and complications between the retropubic and transobturator approaches for the treatment of female stress urinary incontinence (SUI) by conducting a systematic review.
Materials and Methods
We selected all randomized controlled trials (RCTs) that compared retropubic and transobturator sling placements for treatment of SUI. We estimated pooled odds ratios and 95% confidence intervals for intraoperative and postoperative outcomes and complications.
Results
Six hundred twelve studies that compared retropubic and transobturator approaches to midurethral sling placement were identified, of which 16 were included in our research. Our study was based on results from 2646 women. We performed a subgroup analysis to compare outcomes and complications between the two approaches. The evidence to support the superior approach that leads to better objective/subjective cure rate was insufficient. The transobturator approach was associated with lower risks of bladder perforation (odds ratio (OR) 0.17, 95% confidence interval (CI) 0.09-0.32), retropubic/vaginal hematoma (OR 0.32, 95% CI 0.16-0.63), and long-term voiding dysfunction (OR 0.32, 95% CI 0.17-0.61). However, the risk of thigh/groin pain seemed higher in the transobturator group (OR 2.53, 95% CI 1.72-3.72). We found no statistically significant differences in the risks of other complications between the two approaches.
Conclusions
This meta-analysis shows analogical objective and subjective cure rates between the retropubic and transobturator approaches to midurethral sling placement. The transobturator approach was associated with lower risks of several complications. However, good-quality studies with long-term follow-ups are warranted for further research.
Keywords: stress urinary incontinence, retropubic tape, transobturator tape, meta-analysis, systematic review
INTRODUCTION
Stress urinary incontinence (SUI) is a major health problem that affects millions of women throughout the world. It is estimated to affect 15% to 35% of women in the general population (1).
Since it was first described by Ulmsten et al. (2) in 1996, the tension-free vaginal tape (TVT) has been considered as the first-line approach for the treatment of SUI. Although the TVT procedure was shown to have a high and stable cure rate in the medium and long terms (3, 4), complications such as bladder perforation, retropubic hematoma related to the passage of the sling through the retropubic space (5), and voiding dysfunction (6) have been reported. To minimize these complications, in 2001, Delorme (7) described a new route of inserting the tape, which the author called transobturator taping (TOT), in which the tape was inserted through the obturator foramina.
In 2003, de Leval (8) introduced a modified technique called TVT-O, in which the tape is inserted in a reverse route, in through a vaginal incision and out through the obturator foramen (inside out).
Both the TOT and TVT-O procedures proved to have high success rates in short and medium term follow-ups and to be associated with few perioperative complications (9, 10). However, the use of transobturator slings is associated with specific complications such as thigh pain (11). Furthermore, whether the TOTs (both TOT and TVT-O) are equal to the TVT in effectiveness for the treatment of SUI is controversial. Some studies showed that the TOTs were as effective as the TVT (12, 13), but some trials proved that the TVT was superior than the TOT in terms of outcomes (14).
However, current researches were often driven by local norms and individual surgeon preferences instead of evidence-based medicine. Proper comparisons of effectiveness and associated complications between TVT and TOTs are currently limited.
The objectives of this systematic review were to determine and compare effectiveness between the TOTs and TVT in randomized controlled trials (RCTs) and to explore complication rates.
MATERIALS AND METHODS
A prospective protocol for this systematic review was developed. The study inclusion and exclusion criteria, statistical method, approach to estimating study quality, and outcomes are described in the sections that follow. This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of Cangzhou People Hospital. Written informed consent was obtained from all participants.
Sources
All RCTs that compared retropubic and transobturator midurethral sling placement in the treatment of SUI were collected. We searched literatures from 2001 to 2011 using the following online databases: PubMed, Springer, OVID, EBSCO, SAGE Journals, and Web of Science. We also found meeting abstracts from 2001 to 2011 on the Web sites of the International Continence Society, the American Urogynecologic Society, and Society for Urodynamics and Female Urology.
Our search strategy included the Medical Subject Heading term “urinary incontinence” and other “free” keywords such as “retropubic,” “transobturator,” “tension-free vaginal tape,” “TVT,” “TVT-O,” “TOT,” “Monarc,” “SPARC,” and “midurethral sling.” These search terms were used singly and in combination. There were no language restrictions on our searches. Two reviewers collaboratively performed our literature research. The corresponding author of each RCT included in the analysis was contacted.
Inclusion/Exclusion Criteria
All prospective RCTs that compared TOTs (TOT or TVT-O) and TVT in the treatment of urodynamically proven SUI were included. The following inclusion criteria were used: (i) prospective randomized studies that compared between the retropubic and transobturator approaches to tension-free midurethral polypropylene sling placement for SUI; (ii) clearly defined objective and/or subjective outcome measures; and (iii) clearly defined follow-up periods. Studies were excluded on the basis of the following criteria: (i) duplicate reports, in which case the report containing the most complete data was included; (ii) patients who had previously undergone anti-incontinence surgery; (iii) the rate of loss to follow-up was higher than 15% in general; (iv) fewer than 40 included cases; (v) the operation method included TVT-secure; and (vi) animal experiments.
Data Abstraction
The quality of the research studies and data abstraction were evaluated independently by two reviewers (Feng S and Qinglu S) according to Cochrane guidelines 4.2.2 and the quality-control standards set by Jada et al. (15). In case of any dissents between the two reviewers, a third member (Hongbo Z) participated in a discussion to reach a consensus. We collected the following information: (i) the quality of the trials (allocation concealment, randomization method, blinding, power calculation, and intention-to-treat analysis); (ii) the participants’ characteristics (number, type of sling used, and type of SUI, either isolated or mixed); (iii) follow-up duration and number of patients lost to follow-up; (iv) outcomes, namely subjective and/or objective cure; (v) intraoperative (bladder perforation and retropubic/vaginal hematoma) and postoperative complications (thigh/groin pain, de novo urgency or urge incontinence, transient voiding dysfunction, long-term voiding dysfunction, and tape erosion).
Statistical analysis
Statistical analysis was performed using the RevMan 5.0.24 software. For the dichotomous data in our review, we assessed statistical heterogeneity using the following criteria: “P≤0.05 or I2≥50%” was considered to represent statistically significant heterogeneity, and the Mantel-Haenszel random effects model was used to estimate odds ratios (ORs) and 95% confidence intervals (95% CIs). The Peto fixed effects model was used if “P>0.05 and I2<50%.”
We assessed publication bias using funnel plots. Subgroups were established prior to the analysis of the objective/subjective outcomes, according to two perspectives as follows: (i) women with isolated and mixed incontinence and women with isolated incontinence, and (ii) “TVT vs. TOT” and “TVT vs. TVT-O.” The subgroups established prior to the analysis of the complications included only “TVT vs. TOT” and “TVT vs. TVT-O.”
RESULTS
Characteristics of the studies
Our search identified 612 reports, of which 588 were excluded on the basis of their titles/abstracts because of several shortcomings, including the following: lack of a comparative study design, a retrospective design, midurethral slings made of autogenous materials, non-randomized study design, association with other pelvic operations, and fewer than 40 study subjects. The remaining trials were assessed in detail. Three were excluded because neither the objective nor subjective cure criteria were defined (16-18). One was excluded because of lack of a clear explanation of the randomization method (19). Another was excluded because of a high rate of loss to follow-up (20). Three were excluded because of duplicate reports (21-23). Sixteen prospective randomized studies (24-39) were included in the review. The included studies used different objective cure criteria, singly or in combination, such as negative cough stress test result in the urodynamic testing (24-27, 29-39), and 1-hour pad test <1 g (28,29,34), <2 g (32,38), and <3 g (30). Twelve trials reported subjective cure rates (24-30, 32-35, 39). Different subjective measures such as the visual analogue scale, Incontinence Impact Questionnaire, Urogenital Distress Inventory, and other validated questionnaires were also used. Patient satisfaction of the subjective cure was described as “satisfied,” “very satisfied,” or “dry.”
We randomized 2646 women to undergo midurethral sling placement for SUI using either TOTs (TOT/TVT-O) or TVT. Nine trials included women with either isolated or mixed SUI (25-27, 30-32, 34, 35, 39). Seven trials included women with isolated SUI only (24, 28, 29, 33, 36-38). Ten trials compared between TVT-O and TVT (24-26, 29, 34-39); 5 trials compared between TOT and TVT (27, 28, 31-33); and 1 trial included both TOT and TVT-O (30). Perioperative cystoscopy was performed for all the patients in 7 trials (25-28, 30, 31, 38); cystoscopy was used only for the TVT group in the remaining trials. Five of the trials reported allocation concealment (26, 28, 32, 33, 38). Thirteen trials had computer-generated randomization (24-28, 30-37), whereas the other trials used quasi-randomization. Only one trial had a single-blind design (24). Power calculation was performed in 10 trials (25-28, 31, 33, 34-36, 38); intention-to-treat (ITT) analysis was performed in only 1 trial (25). In all the trials, the general rates of loss to follow-up were not higher than 15%. The mean follow-up periods ranged from 6 to 36 months. The details of the included trials are shown in Table-1.
Table 1. Basic data of research from literatures.
| Author | Year | Country | Follow-up duration (month) | Research quality | Retropubic group | Transobturator group |
|---|---|---|---|---|---|---|
| Zhu et al | 2008 | China | 14.5 | A | 35 (TVT) | 34 (TVT-O) |
| Karateke et al | 2009 | Turkey | 14 | A | 83 (TVT) | 84 (TVT-O) |
| Palva et al | 2010 | Finland | 36 | B | 136 (TVT) | 131 (TVT-O) |
| Deffieux et al | 2010 | France | 24 | B | 67 (TVT) | 67 (TVT-O) |
| Porena et al | 2007 | Italy | 31 | B | 70 (TVT) | 75 (TOT) |
| Ross et al | 2009 | Canada | 12 | B | 105 (TVT) | 94 (TVT-O) |
| Liapis et al | 2006 | Greece | 12 | B | 46 (TVT) | 43 (TVT-O) |
| Wang et al | 2011 | China | 12 | B | 32 (TVT) | 36 (TVT-O) |
| David et al | 2011 | Switzerland | 12 | B | 65 (TVT) | 70 (TVT-O/TOT) |
| Lee et al | 2006 | Republic of Korea | 13 | B | 60 (TVT) | 60 (TVT-O) |
| David-Montefiore et al | 2006 | France | 24 | B | 42 (TVT) | 46 (TOT) |
| Ahmed et al | 2010 | Egypt | 20 | B | 19 (TVT) | 21 (TVT-O) |
| de Tayrac et al | 2004 | France | 12 | B | 31 (TVT) | 30 (TVT-O) |
| Krofta et al | 2010 | Czech | 12 | B | 149 (TVT) | 151 (TVT-O) |
| Meschia et al | 2007 | Italy | 6 | B | 114 (TVT) | 117 (TVT-O) |
| Angelo et al | 2007 | Italy | 12 | B | 35 (TVT) | 37 (TVT-O) |
| Zhu et al | 2009 | China | 6 | B | 160 (TVT) | 155 (TVT-O) |
| Araco et al | 2008 | Britain, Italy | 12 | B | 120 (TVT) | 120 (TVT-O) |
| Total | 1369 | 1371 |
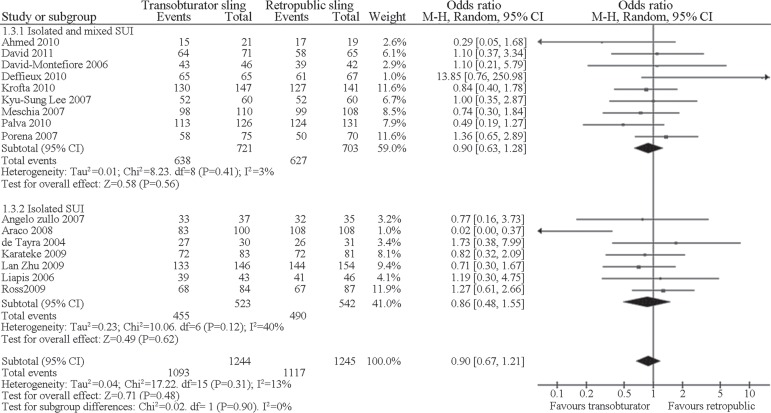
Effectiveness
We performed the first subgroup analysis according to different types of SUI (“isolated and mixed SUI” and “isolated SUI”). When compared with the TVT group, the objective cure rate in the transobturator group was equivalent to that of the “isolated and mixed SUI” subgroup (OR 0.90, 95% CI 0.63-1.28), as well as that of the “isolated SUI” subgroup (OR 0.86, 95% CI 0.48-1.55). The differences in combined objective cure rate were not statistically significant (OR 0.90, 95% CI 0.67-1.21). When the transobturator and TVT groups were compared in terms of subjective cure, the “isolated and mixed SUI” (OR 0.91, 95% CI 0.68-1.23) and “isolated SUI” subgroups had equivalent results (OR 1.17, 95% CI 0.71-1.93), while differences in combined subjective cure were not statistically significant (OR 0.97, 95% CI 0.76-1.26). Figure-1 provides the objective cure rates of the transobturator group (TVT-O and TOT) in comparison with those of the TVT group in the first subgroup analysis.
Figure 1. Meta-analysis of objective cure of SUI between transobturator and TVT approaches in the first subgroup analysis.
We performed another subgroup analysis based on different anti-incontinence approaches (“TVT-O vs. TVT” and “TOT vs. TVT”). One study (30) was excluded in the meta-analysis because of the use of combined TVT-O and TOT in the transobturator group. When compared with TVT, the objective cure of SUI was equivalent between the TVT-O (OR 0.77, 95% CI 0.51-1.15) and TOT groups (OR 1.07, 95% CI 0.68-1.68), and the combined objective cure was not statistically significant (OR 0.86, 95% CI (0.63-1.16). The subjective cure in the transobturator group (TVT-O and TOT) in comparison with that in the TVT group was also not statistically significant (TVT-O vs. TVT: OR 0.97, 95% CI 0.71-1.33; TOT vs. TVT: OR 1.05, 95% CI 0.37-2.99, and total: OR 1.02, 95% CI 0.77-1.34). Figure-2 provides the objective cure rates of the two approaches (TVT-O and TOT) in comparison with that of the TVT in the subgroup analysis. The funnel plots indicated symmetrical distribution of the studies, indicating a low likelihood of publication or reporting bias (Figure-3).
Figure 2. Meta-analysis of the objective cure of the two approaches (TVT-O and TOT) in comparison with TVT.
Figure 3. A and B: Funnel plot of included trials to study the objective/subjective cure of SUI between transobturator and retropubic procedures in the first subgroup analysis C and D: Funnel plot of included trials to study the objective/subjective cure of SUI with procedures by TVT-O/TOT versus TVT.
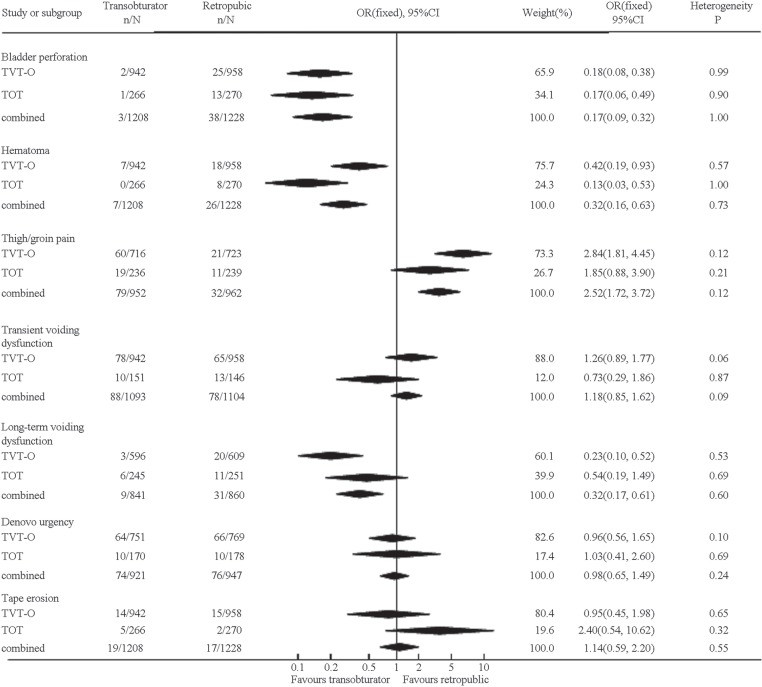
COMPLICATIONS
We excluded one study (30) in the analysis of complications because it used the combination of TVT-O and TOT in the transobturator group.
All the trials provided data on bladder perforation. In comparison with TVT, TVT-O and TOT were associated with statistically significantly lower risk of bladder perforation as follows: TVT-O group (OR 0.18, 95% CI 0.08-0.38), TOT group (OR 0.17, 95% CI 0.06-0.49), combined TVT-O and TOT (OR 0.17, 95% CI 0.09-0.32).
All trials reported data on retropubic/vaginal hematoma. In the subgroup analysis, the risk of hematoma was lower in both the TVT-O (OR 0.42, 95% CI 0.19-0.93) and TOT groups (OR 0.13, 95% CI 0.03-0.53) than in the TVT group.
Eleven trials (25-28, 31, 32, 34-37, 39) represented data on thigh/groin pain. The description and criteria of pain in each trial were not accordant. The TVT-O group seemed to be associated with a higher risk of pain than the TVT group (OR 2.8, 95% CI 1.81-4.45). However, no statistically significant difference was found between the TOT and TVT subgroups (OR 1.85, 95% CI 0.88-3.90). The risk of thigh/groin pain was higher for the combined TVT-O and TOT group (OR 2.53, 95% CI 1.72-3.72).
Thirteen trials (24-27, 29, 31, 33, 34-39) provided data on transient voiding dysfunction. The risks of transient voiding dysfunction were equivalent (TVT-O vs. TVT: OR 1.26, 95% CI 0.89-1.77 and TOT vs. TVT: OR 0.73, 95% CI 0.29-1.86).
Eleven studies (25-29, 31, 33, 34, 36, 38, 39) provided data on long-term voiding dysfunction. In the subgroup analysis, the risk of long-term voiding dysfunction was lower in the TVT-O group (OR 0.23, 95% CI 0.10-0.52) and equivalent between the TOT (OR 0.54, 95% CI 0.19-1.49) and TVT groups.
Eleven studies (24, 25, 28, 29, 31, 33, 34, 36-39) described postoperative symptoms of de novo urgency/urge incontinence. The risks were equivalent between the transobturator and retropubic groups (TVT-O vs. TVT: OR 0.96, 95% CI 0.56-1.65 and TOT vs. TVT: OR 1.03, 95% CI 0.41-2.60).
All the trials reported data on tape erosion. The risks of tape erosion were equivalent (TVT-O vs. TVT: OR 0.95, 95% CI 0.45–1.98 and TOT vs. TVT: OR 2.40, 95% CI 0.54-10.62).
Figure-4 provides a summary of the complications associated with the two tapes (TVT-O and TOT) in comparison with the TVT.
Figure 4. Complications of the two procedures (TVTO and TOT) in comparison with TVT.
DISCUSSION
This systematic review has several superiorities. To ensure the accordance of baseline participant characteristics, we included only prospective and RCTs trials. To minimize the likelihood of publication or reporting bias, we set no language restrictions on our searches and sought both published and unpublished studies. Two reviewers independently estimated the quality of the studies according to Cochrane guidelines 4.2.2 and quality-control standards set by Jada et al. To obtain the most accurate results possible, we performed a subgroup analysis from two angles, namely (1) “isolated and mixed SUI” and “isolated SUI,” and (2) “TVT-O vs. TVT” and “TOT versus TVT.”
We found no statistically significant difference in either objective or subjective cure between the transobturator and retropubic approaches for the treatment of female SUI. The funnel plots of the outcomes in the two subgroup analyses were evenly distributed, indicating a less likelihood of publication bias and higher confidence in the results. These results are consistent with those of most of the included trials (24-31, 33-37, 39). However, these findings cannot demonstrate the equivalent effectiveness of the two approaches. Although we compared between the transobturator and retropubic approaches in the “isolated and mixed SUI” and “isolated SUI” subgroups, the comparison between the two approaches in women with intrinsic sphincter deficiency (ISD) was ignored because of the lack of sufficient relative trials. In fact, several studies (14, 40) proved that the transobturator approach was inferior to the retropubic approach in the treatment of ISD in women. Thus, further research in this field is warranted.
Both the TVT-O and TOT approaches are recognized as associated with lower risks of bladder perforation and retropubic hematoma than the TVT. This review confirms the above-mentioned standpoint. However, some RCTs avoided the systematic use of cystoscopy with transobturator procedures (24, 29, 32-37, 39), and all the 3 cases of bladder perforation during the transobturator procedure were reported by the trials in which perioperative cystoscopy was routinely used for all the patients (26, 27). Thus, the real bladder perforation rate during transobturator procedures may be a little higher. Although previous research (41) suggests that systematic use of cystoscopy was not necessary for transobturator approach, surgeons must be aware of the risk of bladder perforation, even with the transobturator procedure.
We found that the transobturator approach, especially the TVT-O procedure, was associated with a lower risk of long-term voiding dysfunction than the TVT. This result may be explained by the following, as reported by Juma (42) and Morey (43): the orientation of the transobturator tension-free midurethral sling was more similar to the natural hammock shape, as compared with the TVT procedure. As a result of lower shearing force to the urethra, the transobturator tape is more appropriate for women with slow urine flow rate.
Although we concluded that the risk of thigh/groin pain was higher in the transobturator group, the result was not persuasive owing to the lack of unified definition and description of the duration of pain. Some authors have reported that the hammock nature of the transobturator procedure decreases the risk of de novo urgency or urge incontinence (42). However, we found only insufficient evidence to support that claim, or that one approach leads to a lower risk of tape erosion.
Our study has potential limitations. First, the quality of the included trials was not good enough. For example, only one of the 16 trials had a single-blind design (24) and intention-to-treat analysis was performed only in one study (25). That may be a source of heterogeneity. Second, the criteria of objective and subjective cure, and complications such as pain were not consistent. These negative factors may cause bias and heterogeneity. Among our trials, the last one had the longest follow-up period of 36 months. The follow-up periods were too short to appropriately reflect long-term outcomes and complications.
In conclusion, the transobturator and retropubic approaches were equally effective for the treatment of SUI. In particular, the transobturator approach was associated with a decreased risk of complications. However, good-quality studies with long-term follow-up are warranted for further research.
REFERENCES
- 1.Maral I, Ozkardes H, Peskircioglu L, Bumin MA. Prevalence of stress urinary incontinence in both sexes at or after age 15 years: a cross-sectional study. J Urol. 2001;165:408–412. doi: 10.1097/00005392-200102000-00013. [DOI] [PubMed] [Google Scholar]
- 2.Ulmsten U, Henriksson L, Johnson P, Varhos G. An ambu-latory surgical procedure under local anesthesia for treat-ment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1996;7:81–85. doi: 10.1007/BF01902378. [DOI] [PubMed] [Google Scholar]
- 3.Celebi I, Gungorduk K, Ark C, Akyol A. Results of the tension-free vaginal tape procedure for treatment of female stress urinary A ncontinence: a 5-year follow-up study. Arch Gynecol Obstet. 2009;279:463–467. doi: 10.1007/s00404-008-0805-2. [DOI] [PubMed] [Google Scholar]
- 4.Olsson I, Abrahamsson AK, Kroon UB. Long-term efficacy of the tension-free vaginal tape procedure for the treatment of urinary incontinence. A retrospective follow-up 11.5 years post-operatively. Int Urogynecol J. 2010;21:679–683. doi: 10.1007/s00192-009-1083-7. [DOI] [PubMed] [Google Scholar]
- 5.Karram MM, Segal JL, Vassallo BJ, Kleeman SD. Complications and untoward effects of the tension-free vaginal tape procedure. Obstet Gynecol. 2003;101:929–932. doi: 10.1016/s0029-7844(03)00122-4. [DOI] [PubMed] [Google Scholar]
- 6.Sander P, Sørensen F, Lose G. Does the Tension-Free Vaginal Tape Procedure (TVT) Affect the Voiding Function Over Time? Pressure-Flow Studies 1 Year and 3½ Years after TVT. Neurourology and Urodynamics. 2007;26:995–997. doi: 10.1002/nau.20401. [DOI] [PubMed] [Google Scholar]
- 7.Delorme E. Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women. Prog Urol. 2001;11:1306–1313. [PubMed] [Google Scholar]
- 8.de Leval J. Novel surgical technique for the treatment of female stress urinary incontinence: transobturator vaginal tape inside-out. Eur Urol. 2003;44:724–730. doi: 10.1016/j.eururo.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 9.Shaker HS, Ban HM, Hegazy AS, Mansour MF. Functional and quality of life outcome of transobturator tape for treatment of female stress urinary. Int Urogynecol J. 2011;22:99–103. doi: 10.1007/s00192-010-1238-6. [DOI] [PubMed] [Google Scholar]
- 10.Rajendra M, Han HC, Lee LC, Tseng LA, Wong HF. Retrospective study on tension-free vaginal tape obturator (TVT-O) Int Urogynecol J. 2012;23:327–334. doi: 10.1007/s00192-011-1552-7. [DOI] [PubMed] [Google Scholar]
- 11.Hazewinkel MH, Hinoul P, Roovers JP. Persistent groin pain following a trans-obturator sling procedure for stress urinary incontinence: a diagnostic and therapeutic challenge. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20:363–365. doi: 10.1007/s00192-008-0714-8. [DOI] [PubMed] [Google Scholar]
- 12.Lier D, Ross S, Tang S, Robert M, Jacobs P. Trans-obturator tape compared with tension-free vaginal tape in the surgical treatment of stress urinary incontinence: a cost utility analysis. BJOG. 2011;118:550–556. doi: 10.1111/j.1471-0528.2010.02845.x. [DOI] [PubMed] [Google Scholar]
- 13.George S, Begum R, Thomas-Philip A, Thirumalakumar L, Sorinola O. Two-year comparison of tension-free vaginal tape and transobturator tape for female urinary stress incontinence. Obstet Gynecol. 2010;30:281–284. doi: 10.3109/01443610903551756. [DOI] [PubMed] [Google Scholar]
- 14.Chawla A. Transobturator tapes are preferable over transvaginal tapes for the management of female stress urinary incontinence: Against. Indian J Urol. 2009;25:554–557. doi: 10.4103/0970-1591.57903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jadad AR, Moore A, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 16.Dyrkorn OA, Kulseng-Hanssen S, Sandvik L. TVT compared with TVT-O and TOT: results from the Norwegian National Incontinence Registry. Int Urogynecol J. 2010;21:1321–1326. doi: 10.1007/s00192-010-1195-0. [DOI] [PubMed] [Google Scholar]
- 17.Aniuliene R. Tension-free vaginal tape versus tension-free vaginal tape obturator (inside-outside) in the surgical treatment of female stress urinary incontinence. Medicina (Kaunas) 2009;45:639–643. [PubMed] [Google Scholar]
- 18.Wang AC, Lin YH, Tseng LH, Chih SY, Lee CJ. Prospective randomized comparison of transobturator suburethral sling (Monarc) vs suprapubic arc (Sparc) sling procedures for female urodynamic stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17:439–443. doi: 10.1007/s00192-005-0035-0. [DOI] [PubMed] [Google Scholar]
- 19.Chen Z, Chen Y, Du GH, Yuan XY, Wu J, Zeng XY, et al. Comparison of three kinds of mid-urethral slings for surgical treatment of female stress urinary incontinence. Urologia. 2010;77:37–41. [PubMed] [Google Scholar]
- 20.Barry C, Lim YN, Muller R, Hitchins S, Corstiaans A, Foote A, et al. A multi-centre, randomised clinical control trial comparing the retropubic (RP) approach versus the transobturator approach (TO) for tension-free, suburethral sling treatment of urodynamic stress incontinence: the TORP study. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:171–178. doi: 10.1007/s00192-007-0412-y. [DOI] [PubMed] [Google Scholar]
- 21.Rinne K, Laurikainen E, Kivela A, Aukee P, Takala T, Valpas A, et al. A randomized trial comparing TVT with TVT-O: 12-month results. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:1049–1054. doi: 10.1007/s00192-008-0581-3. [DOI] [PubMed] [Google Scholar]
- 22.Laurikainen E, Valpas A, Kivela A, Kallioal T, Rinne K, Takala T, et al. Retropubic Compared With Transobturator Tape Placement in Treatment of Urinary Incontinence. A Randomized Controlled Trial. Obstet Gynecol. 2007;109:4–11. doi: 10.1097/01.AOG.0000249607.82768.a1. [DOI] [PubMed] [Google Scholar]
- 23.Angioli R, Plotti F, Muzii L, Montera R, Panici PB, Zullo MA. Tension-Free Vaginal Tape Versus Transobturator Suburethral Tape: Five-Year Follow-up Results of a Prospective. Randomised Trial. Eur Urol. 2010;58:671–677. doi: 10.1016/j.eururo.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 24.Karateke A, Haliloglu B, Cam C, Sakalli M. Comparison of TVT and TVT-O in patients with stress urinary incontinence: Short-term cure rates and factors influencing the outcome. A prospective randomised study. Aust N Z J Obstet Gynaecol. 2009;49:99–105. doi: 10.1111/j.1479-828X.2009.00957.x. [DOI] [PubMed] [Google Scholar]
- 25.Palva K, Rinne K, Aukee P, Kivela A, Laurikainen E, Takala T, et al. A randomized trial comparing tension-free vaginal tape with tension-free vaginal tape-obturator: 36-month results. Int Urogynecol J. 2010;21:1049–1055. doi: 10.1007/s00192-010-1160-y. [DOI] [PubMed] [Google Scholar]
- 26.Deffieux X, Daher N, Mansoor A, Debodinance P, Muhlstein J, Fernandez H. Transobturator TVT-O versus retropubic TVT results of a multicenter randomized controlled trial at 24 months follow-up. Int Urogynecol J. 2010;21:1337–1345. doi: 10.1007/s00192-010-1196-z. [DOI] [PubMed] [Google Scholar]
- 27.Porena M, Costantini E, Frea B, Giannantoni A, Ranzoni S, Mearini L, et al. Tension-Free Vaginal Tape versus Transobturator Tape as Surgery for Stress Urinary Incontinence: Results of a Multicentre Randomised Trial. Eur Urol. 2007;52:1481–1491. doi: 10.1016/j.eururo.2007.04.059. [DOI] [PubMed] [Google Scholar]
- 28.Ross S, Robert M, Swaby C, Dederer L, Lier D, Tang S, et al. Transobturator Tape Compared With Tension-Free Vaginal Tape for Stress Incontinence, A Randomized Controlled Trial. Obstet Gynecol. 2009;114:1287–1294. doi: 10.1097/AOG.0b013e3181c2a151. [DOI] [PubMed] [Google Scholar]
- 29.Liapis A, Bakas P, Giner M, Creatsas G. Tension-Free Vaginal Tape versus Tension-Free Vaginal Tape Obturator in Women with Stress Urinary Incontinence. Gynecol Obstet Invest. 2006;62:160–164. doi: 10.1159/000093320. [DOI] [PubMed] [Google Scholar]
- 30.Scheiner DA, Betschart C, Wiederkehr S, Seifert B, Fink D, Perucchini D. Twelve months effect on voiding function of retropubic compared with outside-in and inside-out transobturator midurethral slings. Int Urogynecol J. 2012;23:197–206. doi: 10.1007/s00192-011-1543-8. [DOI] [PubMed] [Google Scholar]
- 31.David-Montefiore E, Frobert JL, Grisard-Anaf M, Lienhart J, Bonnet K, Poncelet C, et al. Peri-Operative Complications and Pain After the Suburethral Sling Procedure for Urinary Stress Incontinence: A French Prospective Randomised Multicentre Study Comparing the Retropubic and Transobturator Routes. Eur Urol. 2006;49:133–138. doi: 10.1016/j.eururo.2005.09.019. [DOI] [PubMed] [Google Scholar]
- 32.Ahmed S, Hefnawy EL, Bassem S, Nabeeh A. TOT for treatment of stress urinary incontinence: how should we assess its equivalence with TVT? Int Urogynecol J. 2010;21:947–953. doi: 10.1007/s00192-010-1138-9. [DOI] [PubMed] [Google Scholar]
- 33.de Tayrac R, Deffieux X, Droupy S, Chauveaud-Lambling A, Calvanese-Benamour L, Fernandez H. A prospective randomized trial comparing tension-free vaginal tape and transobturator suburethral tape for surgical treatment of stress urinary incontinence. Am J Obstet Gynecol. 2004;190:602–608. doi: 10.1016/j.ajog.2003.09.070. [DOI] [PubMed] [Google Scholar]
- 34.Krofta L, Feyereisl J, Otcenasek M, Velebil P, Kasikova E, Krcmar M. TVT and TVT-O for surgical treatment of primary stress urinary incontinence: prospective randomized trial. Int Urogynecol J. 2010;21:141–148. doi: 10.1007/s00192-009-1027-2. [DOI] [PubMed] [Google Scholar]
- 35.Meschia M, Bertozzi R, Pifarotti P, Baccichet R, Bernasconi F, Guercio E, et al. Peri-operative morbidity and early results of a randomised trial comparing TVT and TVT-O. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18:1257–1261. doi: 10.1007/s00192-007-0334-8. [DOI] [PubMed] [Google Scholar]
- 36.Zullo MA, Plotti F, Calcagno M, Marullo E, Palaia I, Bellati F. One-Year Follow-up of Tension-free Vaginal Tape (TVT) and Trans-obturator Suburethral Tape from Inside to Outside (TVT-O) for Surgical Treatment of Female Stress Urinary Incontinence: A Prospective Randomised Trial. Eur Urol. 2007;51:1376–1382. doi: 10.1016/j.eururo.2006.10.066. [DOI] [PubMed] [Google Scholar]
- 37.Wang W, Zhu L, Lang J. Transobturator tape procedure versus tension-free vaginal tape for treatment of stress urinary incontinence. Int J Gynaecol Obstet. 2009;104:113–116. doi: 10.1016/j.ijgo.2008.09.013. [DOI] [PubMed] [Google Scholar]
- 38.Araco F, Gravante G, Sorge R, Overton J, De Vita D, Sesti F, et al. TVT-O vs TVT: a randomized trial in patients with different degrees of urinary stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:917–926. doi: 10.1007/s00192-007-0554-y. [DOI] [PubMed] [Google Scholar]
- 39.Lee KS, Han DH, Choi YS, Yum SH, Song SH, Doo CK, et al. A Prospective Trial Comparing Tension-Free Vaginal Tape and Transobturator Vaginal Tape Inside-Out for the Surgical Treatment of Female Stress Urinary Incontinence: 1-Year Followup. J Urol. 2007;177:214–218. doi: 10.1016/j.juro.2006.08.063. [DOI] [PubMed] [Google Scholar]
- 40.Long CY, Hsu CS, Wu MP, Liu CN, Wang TN, Tsai EM. Comparison of tension-free vaginal tape and transobturator tape procedure for the treatment of stress urinary incontinence. Curr Opin Obstet Gynecol. 2009;21:342–347. doi: 10.1097/GCO.0b013e32832e07bf. [DOI] [PubMed] [Google Scholar]
- 41.Bonnet P, Waltregny D, Reul O, de Leval J. Transobturator vaginal tape inside out for the surgical treatment of female stress urinary incontinence: anatomical considerations. J Urol. 2005;173:1223–1228. doi: 10.1097/01.ju.0000148364.13525.7b. [DOI] [PubMed] [Google Scholar]
- 42.Juma S, Brito CG. Transobturator tape (TOT): Two years follow-up. Neurourol Urodyn. 2007;26:37–41. doi: 10.1002/nau.20353. [DOI] [PubMed] [Google Scholar]
- 43.Morey AF, Medendorp AR, Noller MW, Mora RV, Shandera KC, Foley JP, et al. Transobturator versus transabdominal mid urethral slings: a multi-institutional comparison of obstructive voiding complications. J Urol. 2006;175:1014–1017. doi: 10.1016/S0022-5347(05)00412-X. [DOI] [PubMed] [Google Scholar]