Abstract
PURPOSE
This study examines the prevalence of depression in a sample of MSM who are at high risk for HIV. It examines the relationship between depressive symptomatology and involvement in HIV risk behaviors, and the factors associated with greater depressive symptomatology.
METHODS
The data come from a national random sample of 332 MSM who used any of 16 websites to identify men with whom they could engage in unprotected sex. Data were collected via telephone interviews.
RESULTS
Depression was more prevalent in this population (26.7%) than among men in the general population. Depression was not related directly to any of the HIV risk behaviors examined, but it was related to men’s attitudes toward condom use, which was the strongest predictor of their involvement in risky behaviors. Five factors were identified as being associated with greater depression: lower educational attainment, greater discrimination based on sexual orientation, greater eroticizing of ejaculatory fluids, experiencing more substance abuse problems, and greater childhood maltreatment.
CONCLUSIONS
Depression is a consequential problem in this population. Although depression does not appear to be related directly to HIV risk practices in this population, its influence cannot be discounted because of its effects on other key predictors of risk involvement.
Keywords: depression, gay men, bisexual men, men who have sex with men (MSM), HIV risk practices, Internet
INTRODUCTION
In recent years, increasing attention has been devoted to the subject of psychological and psychosocial functioning as it relates to HIV risk taking among men who have sex with other men (MSM). Research has shown that, in this population, greater rates of involvement in risky behaviors are associated with higher levels of impulsivity (Dudley et al., 2004; Semple et al., 2006), maladaptive or avoidant coping strategies (Kelly et al., 2009; Martin, Pryce, &Leeper, 2005;Yi, Sandfort, &Shidlo, 2010), and lower levels of self-esteem (Preston et al., 2007; Rosario, Schrimshaw, & Hunter, 2006; Stein et al., 2005).
Coinciding with these studies, learning more about the relationship between depression and HIV risk taking has been garnering scholars’ interest as well. There appear to be two competing “lines of thought” regarding how depression and risk involvement relate to one another. The first “line of thought,” which appears to be less favored and less well-supported by research findings, is that depression diminishes men’s libido, leading them to be less sexually active (Bancroft et al., 2003b; Phillips & Slaughter, 2000). Accordingly, during periods of active depression, men’s involvement in HIV risk behaviors will be lower than at other times when they are not depressed or when they are experiencing fewer depressive symptoms.
The second, seemingly more popular “line of thought” is that men who are depressed turn to various types of substance use/abuse and sexual risk practices as forms of cognitive escapism to help them cope with their negative emotional state (Parsons &Halkitis, 2002). Speaking about this very subject, DeSantis and Vasquez (2011: 159) wrote “MSM who are depressed and feel devalued related to lower levels of self-esteem may engage in high-risk behaviors in an effort to improve their mood and feelings of self-worth…. Mental health conditions such as depressive symptoms and altered self-esteem combined with high-risk sexual behaviors render MSM vulnerable to both STI and HIV infection.” Adam and colleagues (2005) suggested that when men feel depressed, they get into an “I don’t care” mood, which leads them to an increased likelihood of engaging in unsafe sex. On this subject, the authors wrote (p. 242): “If life does not seem worth living now and the future appears bleak as well, then self-preserving actions no longer make sense.” Speaking from a clinical psychology perspective, Shernoff (2005) noted that depression often leads gay men to be hyperactive sexually and to engage in unprotected sex.
Most, but not all (see Dudley et al., 2004; Paul et al., 2001; Safrenet al., 2010; and Reilly & Woo, 2001 for exceptions), of the published studies on this topic have shown that depression is linked with greater involvement in risk practices among MSM. For example, in their sample of African American MSM, Mimiaga and colleagues (2010) reported that experiencing more clinically-significant symptoms of depression was associated with more stimulant use during sex. Other work published by members of that same research team showed that depression was associated with a nearly tripled risk of having unprotected anal sex with a serodiscordant partner, as well as an eight-fold increase in the likelihood of recently having had a sexually transmitted infection (Reisner et al., 2009a). Additionally, MSM who were trying to reduce their risk for HIV by engaging in specific low-risk activities were less likely to experience depression than men who were not engaging in these specific risk-reduction practices (Reisner et al., 2009b). In a sample of HIV-positive MSM, Ross, Rosser, and Neumaier (2008) found that internalized homophobia was linked with greater depression, and that internalized homophobia was linked with greater involvement in unprotected anal intercourse with serodiscordant sex partners. One study of younger MSM (Salomon et al., 2009) found that these persons were more depressed than their older counterparts and more involved in risky practices. This led the authors to conclude that “depressive symptoms … may contribute to greater rates of substance use and other risk-taking behaviors among YMSM” (p. 817). Another study of younger MSM (23-29 year-olds) in the Seattle area reported that greater depression was associated with having three or more sex partners but none of the other risk measures examined (Perdue et al., 2003). In a study of MSM aged 40-70, men attributed their own HIV risk taking to feelings of depression as well as to other factors, such as inability to maintain erections when using condoms, impending mortality, and trading off safer sex (Murray & Adam, 2001). Other studies reporting on a link between greater depression and greater involvement in various types of HIV risk have included Mimiaga and colleagues’ (2009) multi-site study of MSM, Bousman and colleagues’ (2009) research on HIV-positive methamphetamine-using MSM, Bancroft and colleagues’ (2003) research with gay men, Semple, Patterson, and Grant’s (2000) work with HIV-positive gay men who had sex with seronegative or serostatus-unknown sex partners, Walch and Rudolph’s (2006) research on bisexual men, and Parsons and Halkitis’ (2002) examination of men frequenting commercial sex establishments, such as bathhouses and sex clubs.
Despite ongoing interest in the subject of how depression relates to HIV risk taking among MSM and the gradually-accumulating literature on this topic, more work needs to be done to understand the relationship of these factors to one another. Reading through the published literature reveals that the association between depression and HIV risk taking is a complex one, far more complex than a straightforward greater depression → greater risk approach (which usually has been the way that studies published to date on this subject have treated the topic) merits; and research has just begun to examine the myriad ways that depression has its effects on risk practices. In the present study, the main aims are to examine (1) whether or not depression is associated with HIV risk taking in one specific high risk population of MSM (namely, men who use the Internet to identify potential partners with whom they can engage in unprotected sex), and (2) the mechanisms by which depression may have an impact upon HIV-related risk taking in this population.
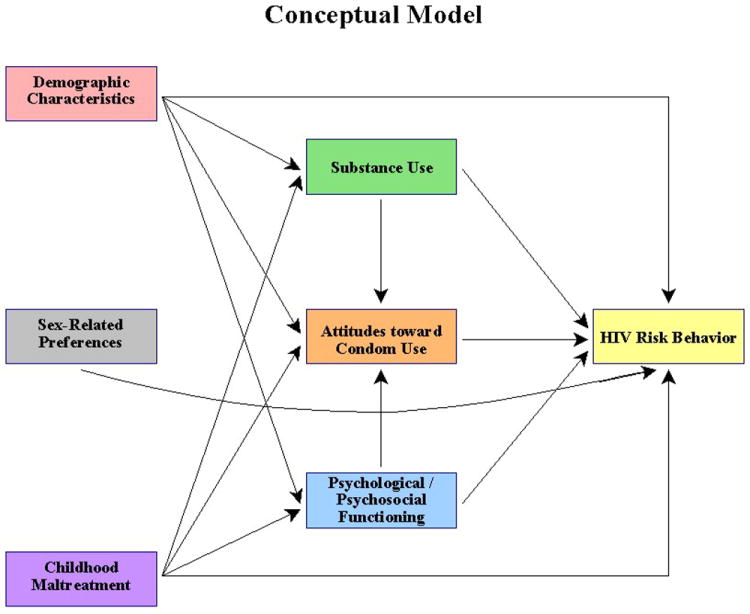
Conceptual Model
In the present paper, a structural approach is used to develop a better understanding of how depression affects HIV risk involvement in a sample of men who use the Internet specifically to find other men with whom they can engage in unprotected sex. Based on previously published studies, the following conceptual model was examined:
In this exploratory model, depression is hypothesized to have both direct and indirect effects on men’s involvement in risky practices. The indirect effects are hypothesized to operate both through the effects on substance use/abuse and on their attitudes toward condom use. As the conceptual model shows, depression is one of six types of influences hypothesized to affect men’s HIV risk practices. The others are demographic variables (e.g., race/ethnicity, age, HIV serostatus), sex-related behavioral preferences (e.g., self-identification as a sexual “top” versus a “bottom,” preferring to have sex that is “wild” or “uninhibited”), substance use/abuse, attitudes toward condom use, and childhood maltreatment experiences (e.g., sexual, physical, and emotional abuse, and physical and emotional neglect).
To a great extent, this conceptual model owes its intellectual origins to the notion of syndemic and to Syndemics Theory. “Syndemic” refers to the tendency for multiple epidemics to co-occur and, for the various maladies to interact with one another, with each one worsening the effects of the others (Singer, 2009; Singer et al., 2006). Walkup et al. (2008) noted that health problems may be construed as syndemic when two or more conditions/afflictions are linked in such a manner that they interact synergistically, with each contributing to an excess burden of disease in a particular population. It is noteworthy that their work also addresses the syndemic of HIV, substance abuse, and mental illness. Stall and colleagues (2003) applied Syndemics Theory to urban MSM’s risk for acquiring HIV and focused on the intertwined epidemics of substance abuse, depression, childhood sexual abuse, and intimate partner violence. They found that the presence of the co-occurring epidemics increased the likelihood that MSM had engaged in unprotected sex and increased their likelihood of being HIV-positive. A number of authors, particularly during the past few years, have written about syndemics and Syndemics Theory as they apply to sexual risk taking and the HIV epidemic (Gielen et al., 2007; Mustanski et al., 2007; Romero-Daza, Weeks, & Singer, 2003; Senn, Carey, &Vanable, 2010; Singer et al., 2006), including specific mention of the applicability of the concept and theory to men who have sex with men (Klein, 2011b; Mustanski et al., 2007).
Based on this conceptual model and the theoretical paradigm described above, the present study examines several specific research questions. First, how prevalent is depression in this population of high-risk MSM? Second, how, if at all, is depression related to involvement in HIV-related risk practices among these men? Third, how, if at all, is depression interrelated with the other factors that are important in developing an overall model accounting for men’s risk practices? Fourth, what factors are associated with MSM experiencing greater/lower levels of depression?
METHODS
This paper draws from cross-sectional data that were collected between January 2008 and May 2009 for The Bareback Project, a study funded by the National Institute on Drug Abuse. The study sample consisted of men who use the Internet specifically to find other men with whom they can engage in unprotected sex. Men were recruited from 16 different websites. Some of the 16 websites catered exclusively to unprotected sex (e.g., Bareback.com, RawLoads.com). These sites accounted for 50.9% of the men subsequently recruited into the study. The other websites used did not cater to unprotected sex exclusively but did make it possible for site users to identify which individuals were looking for unprotected sex (e.g., Men4SexNow.com, Squirt.org). These sites supplied the remaining 49.1% of the men for the sample.
Recruitment
A nationwide sample of men was derived, with random selection of participants being based on a combination of the first letter of the person’s online username, his race/ethnicity (as listed in his profile), and the day of recruitment. Each day, members of the research staff working on recruitment had three letters or numerals assigned to them for their use that day. These letters and numerals were assigned randomly, using the software available at www.random.org (substituting the numbers 1 to 26 to represent, sequentially, the letters of the alphabet, and then using numbers after that to represent numerals). The first letter/numeral was restricted for use for recruiting Caucasian men only; the last two letters/numerals were to be used exclusively for recruiting men of color. (This oversampling technique for racial minority group men was adopted so as to compensate for the fact that men of color, especially African-American men, are more difficult to recruit into research studies than their Caucasian counterparts are.) In order for a particular person to be approached and asked to participate in the study, these letters/numerals had to correspond to the first letter/numeral of that individual’s profile and that person’s race/ethnicity, as stated in his profile, had to be a match for the Caucasian-versus-racial-minority-group-member designation on the daily randomization listing.
On recruitment sites where it was possible to know who was online at the time the recruiter was working, selection of potential study participants came from the pool of men who happened to be logged onto the site during the time block when the recruiter was working. All men who were online at the time the recruiter was working and whose profile name began with the appropriate letter/numeral were eligible to be approached. On recruitment sites where it was not possible to know who was online at the time the recruiter was working, ZIP codes were used to narrow down the pool of men who could be approached. To do this, in addition to the daily three letters/numerals that were assigned randomly to each recruiter throughout the study, each day, ten five-digit numbers were also assigned to each recruiter (five to be used for Caucasian men, five to be used for men of color). These five-digit numbers were random number combinations generated by the www.random.org software, and they were used in this study as proxies for ZIP codes. Recruiters entered the first five-digit number into the website’s ZIP code search field (which site users typically utilized to identify potential sex partners who resided within a specified radius from their residence), selected a five-mile radius, and then viewed the profile names of all men meeting those criteria who had logged onto that site within the previous 24 hours. Those men were eligible to be invited to participate, and their profiles were reviewed for the letter/numeral match described above for men who were online at the time that recruiters were working.
Recruitment efforts were undertaken seven days a week, during all hours of the day and nighttime, variable from week to week throughout the duration of the project. This was done to maximize the representativeness of the final research sample, in recognition of the fact that different people use the Internet at different times.
Participation
Initially, men were approached for participation either via instant message or email (much more commonly via email), depending upon the website used. Potential participants were provided with a brief overview of the study and informed consent-related information, and they were given the opportunity to ask questions about the study before deciding whether or not to participate. Potential participants were also provided with a website link to the project’s online home page, to offer additional information about the project and to help them feel secure in the legitimacy of the research endeavor. Interested men were scheduled for an interview soon after they expressed an interest in taking part in the study, typically within a few days. To maximize convenience for participants, interviews were conducted during all hours of the day and night, seven days a week, based on interviewer availability and participants’ preferences.
Participants in the study completed a one-time, confidential telephone interview addressing a wide array of topics. The decision to conduct the data collection via telephone interviews rather than via anonymous online surveys was made for a number of reasons. First, telephone interviews allowed the research team members to establish rapport with respondents, and this was deemed critical in light of the length of the questionnaire and the very personal nature of the questions being asked. Second, using telephone interviews enabled the research team to make sure that study participants understood all of the questions (something that cannot be achieved when online survey techniques are used), and helped people to “think through” some of the more complex questions asked during the interview. Third, The Bareback Project was a mixed-methods study, involving the collection of both quantitative and qualitative data. The latter would have been precluded had only an online survey been implemented.
The questionnaire that was used for the study’s quantitative component (which serves as the basis for the data reported in the present research) was developed specifically for The Bareback Project. Many parts of the survey instrument were derived from standardized scales previously used and validated by other researchers. The interview covered such subjects as: degree of “outness,” perceived discrimination based on sexual orientation, general health practices, HIV testing history and serostatus, sexual practices (protected and unprotected) with partners met online and offline, risk-related preferences, risk-related hypothetical situations, substance use, drug-related problems, Internet usage, psychological and psychosocial functioning, childhood maltreatment experiences, HIV/AIDS knowledge, and some basic demographic information.
The interviews lasted an average of 69 minutes (median = 63, s.d. = 20.1, range = 30–210). Participants who completed the interview were offered $35. Two payment options were available, one of which allowed men to maintain complete anonymity (PayPal) and one of which required them to provide a name and mailing address to receive payment (check). Approval of the research protocol was given by the institutional review boards at Morgan State University, where the principal investigator and one of the research assistants were affiliated, and George Mason University, where the other research assistant was located.
Measures Used
The main measure of depression was the Center for Epidemiologic Studies Depression (CES-D) scale (Radloff, 1977), which asks respondents to indicate the number of days they experienced each of 20 symptoms of depression. Reliability for this scale was excellent (Cronbach’s alpha = 0.93). Higher scores on the scale indicate greater levels of depressive symptomatology, with scores of 16 or greater usually considered to be indicative of the likely presence of clinical depression. Additionally, scores in the 8-15 range can be construed as being indicative of sub-clinical levels of depression–that is, noticeably affected by depressive symptoms but not reaching the higher, more-stringent threshold of clinical depression.
Several HIV risk behavior outcome measures were examined in conjunction with the third part of the analysis. The measure used for the main structural equation modeling indicated the proportion of all sex acts (insertive and receptive) that involved the use of condoms. It was a continuous measure based on sexual behaviors reported during the 30 days prior to interview.1 Other risk behaviors (all of which utilized a past-30-days time frame) assessed included the proportion of all anal sex acts that involved the use of condoms (continuous), the proportion of all sex acts involving internal ejaculation (continuous), the proportion of all anal sex acts involving internal ejaculation (continuous), the number of sex partners (continuous), the number of times engaging in anonymous sex (continuous), and the number of times having sex while under the influence of alcohol and/or other drugs (continuous).
Demographic data included age (continuous), race/ethnicity (categorical), educational attainment (continuous), sexual orientation (gay versus bisexual), HIV serostatus (HIV-positive versus HIV-negative or serostatus-unknown), sexual role identity (top, versatile top, versatile, versatile bottom, or bottom), and population density in one’s area of residence (continuous measure, computed based on the person’s ZIP code and Bureau of Census data for population density for that ZIP code; U.S. Census Bureau, 2000). Additional background information variables included knowing anyone who was living with AIDS (yes/no), knowing anyone who had died from AIDS (yes/no), and perceptions of discrimination experienced based on one’s sexual orientation (continuous scale measure derived from Pinel’s [1999] Stigma-Consciousness Questionnaire (SCQ) for Gay Men and Lesbians; Cronbach’s alpha = 0.75).
As the model depicted in Figure 1 shows, several substance abuse measures were examined as well. These included whether or not the person had used any illegal drugs during the month prior to interview (yes/no), total amount of illegal drug use during the previous 30 days (continuous measure, summing the quantity-frequency of use for nine different types of illegal drugs), and the number of symptoms of drug abuse and drug dependency experienced during one’s lifetime and during the past 30 days (both continuous scale measures, with items derived from the DSM-IV-TR [American Psychiatric Association, 2000]; Kuder-Richardson20 = 0.87 and 0.79, respectively).
Figure 1.
A few items assessing men’s sex-related preferences were also included in these analyses. These were: the extent to which men liked/preferred to have sex that was rough (continuous), the extent to which men liked/preferred to have sex that was “wild” or “uninhibited” (continuous), the extent to which men liked/preferred to have sex in public places (continuous), whether or not men liked to have anonymous sex (yes/no), and the extent to which men eroticized ejaculatory fluids (continuous scale measure; Cronbach’s alpha = 0.84).
In addition to depression, three other measures of psychosocial functioning were examined as well. These included men’s overall attitudes toward using condoms (continuous scale measure derived from applicable items in Brown [1984]; Cronbach’s alpha = 0.91), perceived accuracy of HIV serostatus information provided by prospective partners during discussions (five-level ordinal measure, ranging from “not at all” to “very”), and perceived accuracy of HIV serostatus information supplied in men’s online profiles (five-level ordinal measure, ranging from “not at all” to “very”).
Finally, childhood maltreatment experiences were assessed via the Childhood Trauma Questionnaire (Bernstein & Fink, 1998). These items enabled separate continuous scale measures to be developed to assess sexual abuse (Cronbach’s alpha = 0.93), physical abuse (Cronbach’s alpha = 0.85), emotional abuse (Cronbach’s alpha = 0.89), physical neglect (Cronbach’s alpha = 0.71), and emotional neglect (Cronbach’s alpha = 0.93) during men’s childhood and adolescent years, as well as an overall extent of maltreatment measure (Cronbach’s alpha = 0.94).
Analysis
Examination of the relationship between level of depression and involvement in HIV-related risk practices was undertaken by computing simple correlation coefficients (Pearson’s r), because all of the dependent and independent variables in question were continuous measures.
The next part of the analysis, focusing on the factors associated with engaging in unprotected sex, was undertaken in two steps. First, bivariate relationships were assessed for each of the independent variables outlined above and unprotected sex, using the latter as the dependent variable. Whenever the independent measure was dichotomous (e.g., sexual orientation, HIV-positive serostatus), Student’s t tests were used. Whenever the independent variable was continuous (e.g., educational attainment, age), simple regression was used. Then, all items found to be related either significantly (p<.05) or marginally (.10>p>.05) to the extent to which men used condoms were entered into a multivariate equation, and then removed in stepwise fashion until a best fit model containing only statistically-significant measures remained. A comparable approach was used to determine the multivariate measures that were associated with (i.e., predictive of) men’s attitudes toward condom use and men’s levels of depression.
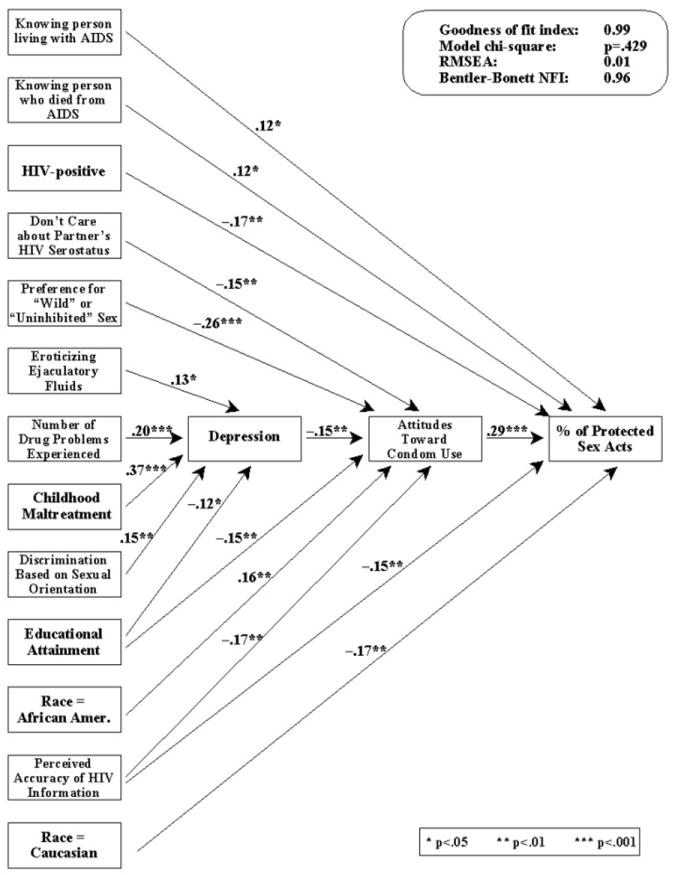
Subsequently, the relationships depicted in Figure 2 (which were the result of the bivariate and multivariate analyses described above) were subjected to a structural equation analysis to determine whether the way the relationships depicted there is an appropriate and effective representation of the study data. SAS’s PROC CALIS procedure was used to assess the overall fit of the model to the data. When we use this type of structural equation analysis, we look for several specific outcomes: (1) a goodness-of-fit index as close to 1.00 as possible, but no less than 0.90, (2) a Bentler-Bonett normed fit index value as close to 1.00 as possible, but no less than 0.90, (3) an overall chi-square value for the model that is statistically non significant, preferably as far from attaining statistical significance as possible, and (4) a root mean square error approximation value as close to 0.00 as possible, but no greater than 0.05. If these conditions are met, then the relationships depicted are considered to indicate a good fit with the data.
Figure 2.
Throughout all of the analyses, results are reported as statistically significant whenever p<.05.
RESULTS
Sample Characteristics
In total, 332 men participated in the study. They ranged in age from 18 to 72 (mean = 43.7, s.d. = 11.2, median = 43.2) (see Table 1). Racially, the sample was appropriately diverse, with 74.1% of the men being Caucasian, 9.0% each being African American and Latino, 5.1% self-identifying as biracial or multiracial, 2.4% being Asian, and 0.3% being Native American. These figures are a fairly close approximation of men in the general population-at-large (U.S. Census Bureau, 2001). The large majority of the men (89.5%) considered themselves to be gay and almost all of the rest (10.2%) said they were bisexual. On balance, men participating in The Bareback Project were fairly well-educated. About 1 man in 7 (14.5%) had completed no more than high school; 34.3% had some college experience without earning a college degree; 28.9% had a bachelor’s degree; and 22.3% were educated beyond the bachelor’s level. Consistent with the demography of the U.S. population (U.S. Census Bureau, 2000), 28.0% of the men lived in rural or low-density population areas (fewer than 500 persons per square mile), 23.5% lived in urban or higher-density population areas (more than 5,000 persons per square mile), with most of the latter group (17.2% of the sample) living in very high density population areas (more than 10,000 persons per square mile). Slightly more than one-half of the men (59.0%) reported being HIV-positive; most of the rest (38.6%) were HIV-negative.
Table 1. Sample Characteristics.
| Characteristic | N | % |
|---|---|---|
|
| ||
| Age | ||
| 18–29 | 44 | 13.3 |
| 30-39 | 69 | 20.8 |
| 40-49 | 109 | 32.9 |
| 50-59 | 81 | 24.5 |
| 60+ | 28 | 8.5 |
|
| ||
| Race/Ethnicity | ||
| Caucasian | 246 | 74.1 |
| African American | 30 | 9.0 |
| Latino | 30 | 9.0 |
| Asian / Pacific Islander | 8 | 2.4 |
| Native American / Native Alaskan | 1 | 0.3 |
| Biracial / multiracial | 17 | 5.1 |
|
| ||
| Educational Attainment | ||
| High school graduate or less | 48 | 14.5 |
| Some college | 114 | 34.3 |
| College graduate | 96 | 28.9 |
| Post-graduate | 74 | 22.3 |
|
| ||
| Population Density in Area of Residence | ||
| Rural (<250 persons per square mile) | 76 | 22.9 |
| Urban (1,000+ persons per square mile) | 198 | 59.6 |
| low density (1,000 to 2,500 persons) | (53) | (16.0) |
| medium density (2,501 persons to 5,000 persons) | (67) | (33.8) |
| high density (5,001+ persons) | (88) | (44.4) |
|
| ||
| Relationship Status | ||
| Married or “involved” | 87 | 26.2 |
| Single | 245 | 73.8 |
|
| ||
| HIV Serostatus | ||
| Negative | 128 | 38.6 |
| Positive | 196 | 59.0 |
| Don’t know | 8 | 2.4 |
|
| ||
| Sexual Orientation | ||
| Gay | 297 | 89.5 |
| Bisexual | 34 | 10.2 |
|
| ||
| Sexual Role Identity | ||
| Total top | 54 | 16.3 |
| Versatile top | 62 | 18.7 |
| Versatile | 60 | 18.1 |
| Versatile bottom | 92 | 27.7 |
| Total bottom | 64 | 19.3 |
Prevalence of Depression
Slightly more than half of the men in this study (52.3%) reported few enough symptoms of depression so as to be classified as “normal” or “not depressed.” Another 21.0% had experienced enough depression-related problems that they could be classified as sub-clinical but not unaffected by depression. The remaining men, 26.7% of the total sample, reported levels of depressive symptomatology so as to characterize them as probably being clinically depressed. In the latter group, more than one-quarter of the men (7.0% of the total sample) were experiencing high-impact levels of depression, reporting at least twice the minimum impact of depressive symptoms necessary to label them as being clinically depressed.
Factors Associated with Depression
Multivariate analysis revealed that five measures were associated with (i.e., predictive of) men’s levels of depression. First, the better educated a man was, the less affected he tended to be by depression (p=.015). Second, the more discrimination men perceived themselves to experience, particularly at the behest of other men, the more depressive symptoms they typically reported (p=.003). Third, the more they eroticized ejaculatory fluids, the more depressed men tended to be (p=.011). Fourth, the more drug abuse and drug dependency symptoms men reported having experienced during the preceding month, the greater their recent experiences with depression tended to be (p<.001). Fifth, the more they were maltreated during their childhood and/or adolescent years, the more depressed men tended to be in adulthood (p<.001). Together, these five items explained 30.2% of the total variance in men’s levels of depression.
Depression and Involvement in Risky Practices
In terms of direct effects, depression was not found to be related to any of the HIV risk-related outcome measures studied. This was true for the proportion of all sex acts involving the use of condoms (p=.246), the proportion of anal sex acts involving the use of condoms (p=.370), the proportion of all sex acts involving internal ejaculation (p=.148), the proportion of anal sex acts involving internal ejaculation (p=.218), the number of times having sex while under the influence of alcohol and/or other drugs (p=.516), the number of times engaging in anonymous sex (p=.370), or men’s recent number of sex partners (p=.356).
This is not to say that depression was irrelevant to understanding study participants’ risk practices, however. The multivariate analyses for men’s overall attitudes toward using condoms–which was the strongest predictor of their involvement in engaging in unprotected sex–revealed that depression was one of the main predictors of condom attitudes. This is depicted in Figure 2. Here, it is revealed that depression was one of six variables found to be associated with how men felt about using condoms, with the other relevant factors being educational attainment (more schooling = more negative attitudes toward using condoms; p=.006), race (African Americans had more conducive condom-related attitudes than members of all other races; p=.004), not caring about the HIV serostatus of potential sex partners (not caring = more negative attitudes toward using condoms; p=.005), liking sex that is “wild” or “uninhibited” (preference for this type of sex = more negative attitudes toward using condoms; p<.001), and perceived accuracy of HIV information provided by potential sex partners during discussion with them (greater perceived accuracy = more negative attitudes toward condom use; p=.001). Regarding depression, the findings showed that, the more depressed men were, the more negative their attitudes toward using condoms tended to be (p=.005).
Structural Equation Model
Figure 2 presents the findings for the overall structural equation model depicting the relationships amongst the types of measures hypothesized to relate to risk, as shown in the Figure 1 conceptual model. The coefficients presented on the figure are standardized coefficients (i.e., Beta values), so that effects sizes can be compared from predictor to predictor. As mentioned above, this figure shows that there was no direct association between depression and the outcome measure, unprotected sex. This can be seen by the absence of a relationship arrow connecting depression and unprotected sex in Figure 2. Depression was relevant to the overall equation/model, however, through its impact upon men’s attitudes toward using condoms (as evidenced by the arrow connecting depression and condom-related attitudes). As shown in Figure 2 (by the statistically-significant, negative coefficient linking these two measures), the more depressive symptoms men experienced, the more negatively they felt with regard to using condoms. The left side of Figure 2 also portrays the five variables that were found to contribute uniquely and significantly to study participants’ depression levels. The positive coefficients shown for eroticizing ejaculatory fluids, the number of drug problems experienced, childhood maltreatment experiences, and discrimination based on one’s sexual orientation all indicate a direct relationship between these measures and men’s levels of depression. Conversely, the negative coefficient shown for educational attainment indicates an inverse relationship with depression–that is, more depressive symptomatology experienced among people with lower levels of education.
The model depicted in Figure 2 is supported quite strongly by the data. The overall goodness-of-fit index is 0.99–well above the 0.90 value that is sought in structural equation modeling. The chi-square test for the overall equation was found to be statistically nonsignificant (p=.429) and, as desired in structural equation modeling, nowhere near attaining statistical significance. The root mean square error approximation was 0.01–well below the 0.05 maximum level considered to be acceptable. The Bentler-Bonett normed fit index value for this equation is 0.96–comfortably above the minimum 0.90 threshold established for a good-fitting structural equation model.
DISCUSSION
In this sample of unprotected sex-seeking MSM, depression was fairly commonplace and a large proportion of the men (26.7%) recently reported experiencing enough depressive symptoms so as to indicate the likely presence of clinical depression. This 26.7% figure is much greater than the 5.3% annual depression prevalence figure cited for adult men in the population-at-large (Substance Abuse Mental Health Services Administration, 2008). The present study’s 26.7% prevalence figure is also greater than the prevalence figures reported by Siconolfi and colleagues (2013) based on their research with HIV-infected MSM aged 50 or older (18.8%), Pantalone and colleagues (2012) based on their research with HIV-infected MSM attending university health clinics in the Seattle area (19.0%), Hirshfield and colleagues (2008) based on their research with HIV-positive MSM using gay-oriented websites for information or socializing with other gay men (18.0%), Mills and colleagues (2004) based on their research with HIV-positive MSM residing in four large American cities (20.1%), and Purcell and colleagues (2005) based on their research with HIV-positive men living in New York City or San Francisco (20.8%), but lower than the 40.4% prevalence figure reported by Becker and colleagues (2009) based on their research with HIV-infected MSM aged 40 or older, and comparable to the 30.0% prevalence figure reported by Houston and colleagues (2012) based on their research with HIV-infected MSM who intentionally seek unprotected sex via the Internet. Additional research is needed to understand the causes of depression among risk-taking, risk-seeking MSM, so that informed intervention efforts and courses of treatment can be developed and implemented. Moreover, additional research is needed to learn more about how depression affects these men’s health behaviors. In the present study, despite being highly prevalent, depression was not found to predict the extent to which men engaged in practices that could lead them to acquire or transmit HIV. This stands in contradiction to the large majority of published studies (cited earlier), which have shown a link between greater depression and greater involvement in risky behaviors.
This begs an important, and currently unanswerable, question: Why is it that depressed men in the present study were not more involved in risky behaviors than their non-depressed counterparts? It is possible that depression simply is not as salient or as immediate a factor in these men’s sex lives and drug-use behaviors as other situational factors, such as partner preferences for sexual safety (or the lack thereof), partner preferences for drug use in conjunction with sexual relations, general discomfort discussing safer sex or negotiating for lowered-risk practices, and so forth. These latter influences have been shown by other researchers to be highly relevant to men’s risk involvement (Horvath, Nygaard, & Rosser, 2010; Mansergh et al., 2010), and their influence may be superceding that of depression in terms of affecting men’s HIV-related decision-making. More research is needed to understand just how depression is and is not influential in this process, and the specific role that it plays in fostering risk behavior involvement among men who use the Internet to find partners for unprotected sex (as well as MSM more generally).
It is important to note, however, that despite the preceding findings of no direct association between depression and HIV risk taking in this population, depression was an important, relevant factor in the overall equation by virtue of its indirect effects on risk taking. Principally, depression seems to be operating “behind the scenes” by having an adverse impact upon men’s attitudes toward condom use. These attitudes, in turn, are the most consequential factor affecting their use or nonuse of sexual protection. Depression often causes people to lose interest in things that, in times of lesser or no depressive symptomatology, would be important to them (Romans et al., 2007). A prime example of this would be taking care of one’s health; and in numerous other studies, depression has been linked with poor health behaviors (Lyons et al., 2008; Masheb&Grilo, 2006; Zen et al., 2011). This appears to be applicable to the present study as well, in which persons experiencing the greatest level of depression were the same ones whose interest in engaging in health-promoting behaviors, such as using condoms and a willingness to consider using condoms, was the lowest.
Also well worth noting is the fact that depression does not operate in a vacuum. A variety of factors influenced the extent to which men in this study experienced depressive symptoms. These merit additional discussion.
The first influential factor here was educational attainment, with better-educated men reporting lower levels of depression than their less-well-educated counterparts. Other studies as well have reported on the inverse nature of the relationship between educational attainment and depression (Ladin, 2008; Ross &Mirowsky, 2006), and the present research is consistent with their findings. From a prevention and intervention standpoint, this finding suggests that gay and bisexual men with lower levels of education may be at particular risk of experiencing depression, thereby making these individuals a group in need of targeted intervention.
The second factor identified as being related to the extent to which study participants experienced depression was the amount of discrimination they perceived themselves to experience (particularly as perpetrated by males) as a result of their sexual orientation. This finding is consistent with other published studies, which have shown that experiences with discrimination are associated with greater levels of depression among men (Watkins et al., 2011), including some studies specifically focusing on this relationship among MSM (Chae& Yoshikawa, 2008; Diaz et al., 2001; Zakalik& Wei, 2006). The evidence from these studies as well as the present study suggests that perceiving oneself to be a victim of discrimination has an impact upon self-esteem and causes many men to feel frustrated and depressed. The remedy for this problem lies at two different levels. At the macro/societal level, it highlights the importance of fighting against homophobia and discrimination based on people’s sexual orientation, so that gay and bisexual men can live freely and happily without fear of reprisals for being who they are. At the micro/individual level, there may be some value in developing prevention materials and intervention program components that can help MSM to learn how to stand up to sexual orientation-based discrimination whenever they are confronted by it. This type of skills-based empowerment may help them to feel more capable of standing up for themselves and, in the process, diminish their likelihood of feeling hopelessness- and helplessness-based depression as a result of any instances of sexual orientation-related discrimination with which they are confronted.
The third factor found to be related to men’s levels of depression was the extent to which they eroticized ejaculatory fluids. Basically, the more they were turned on by the sight, smell, taste, and/or feel of ejaculatory fluids, the more likely men were to experience depressive symptoms. There is no easy way to explain this relationship, especially because very little has been written in the scientific literature pertaining to arousal from ejaculatory fluids–the so-called “cum freaks.” Notable exceptions include Gastaldo et al. (2009), Holmes and Warner (2005), and Ridge (2004), all of whom address the issue of some MSM being aroused by ejaculatory fluids but none of whom discuss this issue as it pertains to any aspect of psychological or psychosocial functioning. The finding obtained in the present study indicates a need for HIV prevention workers and interventionists to pay particular attention to the psychological and psychosexual needs of men who self-identify as “cum freaks” and those who are highly aroused sexually by ejaculatory fluid, as they appear to be at risk for depression.
In addition, the more symptoms of substance abuse and/or substance dependency that men experienced during the month prior to interview, the more depressive symptoms they also tended to report. Many authors have documented a link between substance use/abuse and depression (Cochran & Mays, 2009; Halkitis et al., 2008; Mimiaga et al., 2010), although the directionality of this relationship is very much a point of contention. (That is, does substance abuse cause people to experience symptoms of depression? Does depression lead people to self-medicate via the use of various substances? Is the relationship between the two phenomena ostensibly a recursive one? There is plenty of evidence available in the scientific literature to support all three of these positions.) Likewise, many authors have spoken about the need to address substance use/abuse issues among MSM (Carey, et al., 2009; Halkitis, Mukherjee, &Palamar, 2009; Semple et al., 2009), particularly because of the heightened risk that substance use/abuse causes with regard to HIV transmission. The present study’s finding is consistent with this body of literature and, once again, highlights the importance of working to diminish the prevalence of substance use/abuse among MSM. This issue has been addressed by the present author more comprehensively in another work, which interested readers are encouraged to consult (Klein, 2011a).
Finally, the more physical abuse, sexual abuse, emotional abuse, physical neglect, and/or emotional neglect that people experienced during their formative years, the more they were affected adversely by depression in adulthood. In previous studies, childhood maltreatment experiences among MSM have been linked with a wide variety of adverse outcomes in adulthood, including mental health problems (e.g., depression, anxiety, post-traumatic stress disorder, attempted suicide) (Balsam et al., 2010; Ratner et al., 2003), risky sexual behaviors (Gore-Felton et al., 2006; Mimiaga et al., 2009), and substance abuse (Kalichman et al., 2004; Rosario, Schrimshaw, & Hunter, 2006). These findings, as well as that obtained in the present research, indicate a need to work with MSM who experienced maltreatment during their childhood and/or adolescent years, to help them to recover from the long-term, damaging effects of their abuse or neglect. Interventionists wishing to assist this population should have strong linkages established with local-area mental health professionals, so that men who want to get counseling can do so “on demand” and with the support of the community-based programs that are trying to help them reduce their risk for HIV.
Potential Limitations
Before concluding, the author wishes to acknowledge a few potential limitations of this research. First, the data in this study are based on uncorroborated self-reports. Therefore, it is unknown whether participants underreported or over reported their involvement in risky behaviors. The self-reported data probably can be trusted, however, as noted by other authors of previous studies with similar populations (Schrimshaw et al., 2006). This is particularly relevant for self-reported measures that involve relatively small occurrences (e.g., number of times having a particular kind of sex during the previous 30 days), which characterize the substantial majority of the data collected in this study (Bogart et al., 2007). Other researchers have also commented favorably on the reliability of self-reported information in their studies regarding topics such as condom use (Morisky, Ang, & Sneed, 2002).
A second potential limitation is the possibility of recall bias. For most of the measures used, respondents were asked about their beliefs, attitudes, and behaviors during the past 7 or 30 days. These time frames were chosen specifically: (1) to incorporate a large enough time frame in order to facilitate meaningful variability from person to person, and (2) to minimize recall bias. Although the authors cannot determine the exact extent to which recall bias affected the data, other researchers who have used similar measures have reported that recall bias is sufficiently minimal that its impact upon study findings is likely to be negligible (Kauth, St. Lawrence, & Kelly, 1991). This seems to be especially true when the recall period is small (Fenton et al., 2001; Weir et al., 1999), as was the case for most of the main measures used in the present study.
A third limitation of this research is the unknown extent to which findings may be generalized. As with many published studies focusing on risk practices among MSM, the present study had a larger-than-expected proportion of well-educated men. HIV-positive men were overrepresented as well, which is not surprising when one considers that the study population was comprised by men seeking unprotected sex online. Although study participants were selected at random from the various websites used for recruitment purposes, there is no way to know how well these individuals represent unprotected sex-seeking MSM more broadly. What the present study population does represent, however, is a sample of risk-seeking MSM who actively use the Internet to identify potential sex partners.
Finally, the CES-D, which was used to assess depression in the present study, is generally regarded as being more of a screening tool that provides indications of the likely presence of depression than it is an actual diagnostic instrument. Although numerous studies of depression among MSM have used this instrument (see, for example, Chae& Yoshikawa, 2008; Perdue et al., 2003; Reisneret al., 2009), future researchers might wish, instead, to employ depression inventories that can assess actual clinical depression diagnoses rather than provide the user with indications of the likely presence/absence of clinical depression.
Conclusion
Despite these limitations, the present study has much to offer with regard to understanding the role that depression may play in HIV risk taking among risk-seeking MSM. This study’s data suggest that the relationship between depression and HIV risk taking among unprotected sex-seeking MSM is a complicated one. It cannot be characterized simply or simplistically by assuming that depression → involvement in risk. Rather, it appears that depression → attitudes toward risk taking → involvement in risk. Moreover, as Figure 2 demonstrates, a number of factors were found to be related to the extent to which the men in this study experienced depression. Thus, the actual relationship that must be considered looks something like this: factors affecting/underlying depression → depression → attitudes toward risk taking → involvement in risk. As the conceptual model depicted in Figure 1 portrayed, a variety of factors are involved in the depression-and-HIV-risk-practices nexus. These factors interact with one another in a complex fashion that supports the notion of Syndemics Theory as being applicable to our understanding of how depression and HIV risk are interrelated among men who use the Internet in search of partners for unprotected sex.
Acknowledgments
This research (officially entitled Drug Use and HIV Risk Practices Sought by Men Who Have Sex with Other Men, and Who Use Internet Websites to Identify Potential Sexual Partners) was supported by a grant (5R24DA019805) from the National Institute on Drug Abuse. The author wishes to acknowledge, with gratitude, the contributions made by Thomas P. Lambing to this study’s data collection and data entry/cleaning efforts.
Footnotes
Although a measure assessing the total number of times a man reported having unprotected sex during a particular time period is a direct measure of risk, the author believes that the chosen measure, which assesses the proportion of sex acts that are unprotected, is a better measure because it indicates a person’s likelihood of having unprotected sex across time points. The latter indicates his “usual” practices and tendencies, whereas the former indicates his practices during a specific period that may or may not represent his “usual” sexual opportunities. The number of sexual encounters will increase or decrease during different time periods for the men in this study due to situational influences; thus, basing the risk assessment on the total number of unprotected sexual acts would miss this variation. Consequently, using the proportion of the sexual acts that were unprotected offers a better indication of this behavior when the men are engaging in their “typical” number of sexual encounters as well as for the times when their number of encounters increases or decreases.
References
- Adam BD, Husbands W, Murray J, Maxwell J. AIDS optimism, condom fatigue, or self-esteem? Explaining unsafe sex among gay and bisexual men. Journal of Sex Research. 2005;42:238–248. doi: 10.1080/00224490509552278. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-IV-TR) Arlington, VA: American Psychiatric Association; 2000. [Google Scholar]
- Balsam KF, Lehavot K, Beadnell B, Circo E. Childhood abuse and mental health indicators among ethnically diverse lesbian, gay, and bisexual adults. Journal of Consulting and Clinical Psychology. 2010;78:459–468. doi: 10.1037/a0018661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bancroft J, Janssen E, Strong D, Carnes L, Vukadinovic Z, Long JS. Sexual risk-taking in gay men: The relevance of sexual arousability, mood, and sensation seeking. Archives of Sexual Behavior. 2003a;32:555–572. doi: 10.1023/a:1026041628364. [DOI] [PubMed] [Google Scholar]
- Bancroft J, Janssen E, Strong D, Vukadinovic Z. The relation between mood and sexuality in gay men. Archives of Sexual Behavior. 2003b;32:231–242. doi: 10.1023/a:1023461500810. [DOI] [PubMed] [Google Scholar]
- Becker JT, Kingsley L, Mullen J, Cohen B, Visscher BR, et al. Vascular factors, HIV serostatus, and cognitive dysfunction in gay and bisexual men. Neurology. 2009;73:1292–1299. doi: 10.1212/WNL.0b013e3181bd10e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein DP, Fink L. Childhood Trauma Questionnaire: A retrospective self-report manual. San Antonio, TX: Psychological Corporation; 1998. [Google Scholar]
- Bogart LM, Walt LC, Pavlovic JD, Ober AJ, Brown N, Kalichman SC. Cognitive strategies affecting recall of sexual behavior among high-risk men and women. Health Psychology. 2007;26:787–793. doi: 10.1037/0278-6133.26.6.787. [DOI] [PubMed] [Google Scholar]
- Bousman CA, Cherner M, Ake C, Letendre S, Atkinson HH, Patterson TL, Grant I, Everall IP. Negative mood and sexual behavior among non-monogamous men who have sex with men in the context of methamphetamine and HIV. Journal of Affective Disorders. 2009;119:84–91. doi: 10.1016/j.jad.2009.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown IS. Development of a scale to measure attitude toward the condom as a method of birth control. Journal of Sex Research. 1984;20:255–263. [Google Scholar]
- Carey JW, Mejia R, Bingham T, Ciesielski C, Gelaude D, Herbst JH, Sinunu M, Sey E, Prachand N, Jenkins RA, Stall R. Drug use, high-risk sex behaviors, and increased risk for recent HIV infection among men who have sex with men in Chicago and Los Angeles. AIDS and Behavior. 2009;13:1084–1096. doi: 10.1007/s10461-008-9403-3. [DOI] [PubMed] [Google Scholar]
- Chae DH, Yoshikawa H. Perceived group devaluation, depression, and HIV-risk behavior among Asian gay men. Health Psychology. 2008;27:140–148. doi: 10.1037/0278-6133.27.2.140. [DOI] [PubMed] [Google Scholar]
- Cochran SD, Mays VM. Burden of psychiatric morbidity among lesbian, gay, and bisexual individuals in the California Quality of Life Survey. Journal of Abnormal Psychology. 2009;118:647–658. doi: 10.1037/a0016501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeSantis JP, Vasquez EP. A pilot study to evaluate ethnic/racial differences in depressive symptoms, self-esteem, and sexual behaviors among men who have sex with men. Journal of Gay and Lesbian Social Services. 2011;23:147–164. [Google Scholar]
- Diaz RM, Ayala G, Bein E, Henne J, Marin BV. The impact of homophobia, poverty, and racism on the mental health of gay and bisexual Latino men: Findings from 3 U.S. cities. American Journal of Public Health. 2001;91:927–932. doi: 10.2105/ajph.91.6.927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dudley MG, Rostosky SS, Korfhage BA, Zimmerman RS. Correlates of high-risk sexual behavior among young men who have sex with men. AIDS Education and Prevention. 2004;16:328–340. doi: 10.1521/aeap.16.4.328.40397. [DOI] [PubMed] [Google Scholar]
- Fenton KA, Johnson AM, McManus S, Erens B. Measuring sexual behaviour: Methodological challenges in survey research. Sexually Transmitted Infections. 2001;77:84–92. doi: 10.1136/sti.77.2.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gastaldo D, Holmes D, Lombardo A, O’Byrne P. Unprotected sex among men who have sex with men in Canada: Exploring rationales and expanding HIV prevention. Critical Public Health. 2009;19:399–416. [Google Scholar]
- Gielen AC, Ghandour RM, Burke JG, Mahoney P, McDonnell KA, O’Campo P. HIV/AIDS and intimate partner violence: Intersecting women’s health issues in the United States. Trauma, Violence, and Abuse. 2007;8:178–198. doi: 10.1177/1524838007301476. [DOI] [PubMed] [Google Scholar]
- Gore-Felton C, Kalichman SC, Brondino MJ, Benotsch EG, Cage M, DiFonzo K. Childhood sexual abuse and HIV risk among men who have sex with men: Initial test of a conceptual model. Journal of Family Violence. 2006;21:263–270. [Google Scholar]
- Halkitis PN, Moeller RW, Siconolfi DE, Jerome RC, Rogers M, Schillinger J. Methamphetamine and poly-substance use among gym-attending men who have sex with men in New York City. Annals of Behavioral Medicine. 2008;35:41–48. doi: 10.1007/s12160-007-9005-8. [DOI] [PubMed] [Google Scholar]
- Halkitis PN, Mukherjee PP, Palamar JJ. Longitudinal modeling of methamphetamine use and sexual risk behaviors in gay and bisexual men. AIDS and Behavior. 2009;13:783–791. doi: 10.1007/s10461-008-9432-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirshfield S, Wolitski RJ, Chiasson MA, Remien RH, Humberstone M, Wong T. Screening for depressive symptoms in an online sample of men who have sex with men. AIDS Care. 2008;20:904–910. doi: 10.1080/09540120701796892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes D, Warner D. The anatomy of a forbidden desire: Men, penetration, and semen exchange. Nursing Inquiry. 2005;12:10–20. doi: 10.1111/j.1440-1800.2005.00252.x. [DOI] [PubMed] [Google Scholar]
- Horvath KJ, Nygaard K, Rosser BRS. Ascertaining partner HIV status and its association with sexual risk behavior among internet-using men who have sex with men. AIDS and Behavior. 2010;14:1376–1383. doi: 10.1007/s10461-009-9633-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houston E, Sandfort T, Dolezal C, Carballo-Dieguez A. Depressive symptoms among MSM who engage in bareback sex: Does mood matter? AIDS and Behavior. 2012;16:2209–2215. doi: 10.1007/s10461-012-0156-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Gore-Felton C, Benotsch E, Cage M, Rompa D. Trauma symptoms, sexual behaviors, and substance abuse: Correlates of childhood sexual abuse and HIV risks among men who have sex with men. Journal of Child Sexual Abuse. 2004;13:1–15. doi: 10.1300/J070v13n01_01. [DOI] [PubMed] [Google Scholar]
- Kauth MR, St Lawrence JS, Kelly JA. Reliability of retrospective assessments of sexual HIV risk behavior: A comparison of biweekly, three-month, and twelve-month self-reports. AIDS Education and Prevention. 1991;3:207–214. [PubMed] [Google Scholar]
- Kelly BC, Bimbi DS, Izienicki H, Parsons JT. Stress and coping among HIV-positive barebackers. AIDS and Behavior. 2009;13:792–797. doi: 10.1007/s10461-009-9586-2. [DOI] [PubMed] [Google Scholar]
- Klein H. Substance use and abuse among men using the Internet specifically to find partners for unprotected sex. Journal of Psychoactive Drugs. 2011a;43:89–98. doi: 10.1080/02791072.2011.587391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein H. Using a syndemics theory approach to study HIV risk taking in a population of men who use the Internet to find partners for unprotected sex. American Journal of Men’s Health. 2011b;5:466–476. doi: 10.1177/1557988311398472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ladin K. Risk of late-life depression across 10 European Union countries: Deconstructing the education effect. Journal of Aging and Health. 2008;20:653–670. doi: 10.1177/0898264308321002. [DOI] [PubMed] [Google Scholar]
- Lyons M, Hitsman B, Xian H, Panizzon MS, Tsuang MT, et al. A twin study of smoking, nicotine dependence, and major depression in men. Nicotine and Tobacco Research. 2008;10:97–108. doi: 10.1080/14622200701705332. [DOI] [PubMed] [Google Scholar]
- Mansergh G, McKirnan DJ, Flores SA, Hudson SM, Koblin BA, Purcell DW, Colfax GN. HIV-related attitudes and intentions for high-risk, substance-using men who have sex with men: Associations and clinical implications for HIV-positive and HIV-negative MSM. Journal of Cognitive Psychotherapy. 2010;24:281–293. [Google Scholar]
- Martin JI, Pryce JG, Leeper JD. Avoidance coping and HIV risk behavior among gay men. Health and Social Work. 2005;30:193–201. doi: 10.1093/hsw/30.3.193. [DOI] [PubMed] [Google Scholar]
- Masheb RM, Grilo CM. Emotional overeating and its associations with eating disorder psychopathology among overweight patients with binge eating disorder. International Journal of Eating Disorders. 2006;39:141–146. doi: 10.1002/eat.20221. [DOI] [PubMed] [Google Scholar]
- Mills TC, Paul J, Stall R, Pollack L, Catania JA, et al. Distress and depression in men who have sex with men: The Urban Men’s Health Study. American Journal of Psychiatry. 2004;161:278–285. doi: 10.1176/appi.ajp.161.2.278. [DOI] [PubMed] [Google Scholar]
- Mimiaga MJ, Noonan E, Donnell D, Safren SA, Mayer KH, et al. Childhood sexual abuse is highly associated with HIV risk-taking behavior and infection among MSM in the EXPLORE study. Journal of Acquired Immune Deficiency Syndromes. 2009;51:340–348. doi: 10.1097/QAI.0b013e3181a24b38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mimiaga MJ, Reisner SL, Fontaine YM, Bland SE, Mayer KH, et al. Walking the line: Stimulant use during sex and HIV risk behavior among Black urban MSM. Drug and Alcohol Dependence. 2010;110:30–37. doi: 10.1016/j.drugalcdep.2010.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morisky DE, Ang A, Sneed CD. Validating the effects of social desirability on self-reported condom use behavior among commercial sex workers. AIDS Education and Prevention. 2002;14:351–360. doi: 10.1521/aeap.14.6.351.24078. [DOI] [PubMed] [Google Scholar]
- Murray J, Adam BD. Aging, sexuality, and HIV issues among older gay men. Canadian Journal of Human Sexuality. 2001;10:75–90. [Google Scholar]
- Mustanski B, Garofalo R, Herrick A, Donenberg G, et al. Psychosocial health problems increase risk for HIV among urban young men who have sex with men: Preliminary evidence of a syndemic in need of attention. Annals of Behavioral Medicine. 2007;34:37–45. doi: 10.1080/08836610701495268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pantalone DW, Hessler DM, Bankoff SM, Shah BJ. Psychosocial correlates of HIV-monoinfection and HIV/HCV-coinfection among men who have sex with men. Journal of Behavioral Medicine. 2012;35:520–528. doi: 10.1007/s10865-011-9381-1. [DOI] [PubMed] [Google Scholar]
- Parsons JT, Halkitis PN. Sexual and drug-using practices of HIV-positive men who frequent public and commercial sex environments. AIDS Care. 2002;14:815–826. doi: 10.1080/0954012021000031886. [DOI] [PubMed] [Google Scholar]
- Paul JP, Catania J, Pollack L, Stall R. Understanding childhood sexual abuse as a predictor of sexual risk-taking among men who have sex with men: The Urban Men’s health Study. Child Abuse and Neglect. 2001;25:557–584. doi: 10.1016/s0145-2134(01)00226-5. [DOI] [PubMed] [Google Scholar]
- Perdue T, Hagan H, Thiede H, Valleroy L. Depression and HIV risk behavior among Seattle-area injection drug users and young men who have sex with men. AIDS Education and Prevention. 2003;15:81–92. doi: 10.1521/aeap.15.1.81.23842. [DOI] [PubMed] [Google Scholar]
- Phillips RL, Jr, Slaughter JR. Depression and sexual desire. American Family Physician. 2000;62:782–786. [PubMed] [Google Scholar]
- Pinel EC. Stigma consciousness: The psychological legacy of social stereotypes. Journal of Personality and Social Psychology. 1999;76:114–128. doi: 10.1037//0022-3514.76.1.114. [DOI] [PubMed] [Google Scholar]
- Preston DB, D’Augelli AR, Kassab CD, Starks MT. The relationships of stigma to the sexual risk behavior of rural men who have sex with men. AIDS Education and Prevention. 2007;19:218–230. doi: 10.1521/aeap.2007.19.3.218. [DOI] [PubMed] [Google Scholar]
- Purcell DW, Wolitski RJ, Hoff CC, Parsons JT, Woods WJ, Halkitis PN. Predictors of the use of viagra, testosterone, and antidepressants among HIV-seropositive gay and bisexual men. AIDS. 2005;19:s57–s66. doi: 10.1097/01.aids.0000167352.08127.76. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Ratner PA, Johnson JL, Shoveller JA, Chan K, Hogg RS, et al. Non-consensual sex experienced by men who have sex with men: Prevalence and association with mental health. Patient Education and Counseling. 2003;49:67–74. doi: 10.1016/s0738-3991(02)00055-1. [DOI] [PubMed] [Google Scholar]
- Reilly T, Woo G. Predictors of high-risk sexual behavior among people living with HIV/AIDS. AIDS and Behavior. 2001;5:205–217. [Google Scholar]
- Reisner SL, Mimiaga MJ, Skeer M, Mayer KH. Beyond anal sex: Sexual practices associated with HIV risk reduction among men who have sex with men in Boston, Massachusetts. AIDS Patient Care and STDs. 2009;23:545–550. doi: 10.1089/apc.2008.0249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, Mimiaga MJ, Skeer M, Bright D, Mayer KH, et al. Clinically significant depressive symptoms as a risk factor for HIV infection among Black MSM in Massachusetts. AIDS and Behavior. 2009;13:798–810. doi: 10.1007/s10461-009-9571-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridge DT. ‘It was an incredible thrill’: The social meanings and dynamics of younger gay men’s experiences of barebacking in Melbourne. Sexualities. 2004;7:259–279. [Google Scholar]
- Romans SE, Tyas J, Cohen MM, Silverstone T. Gender differences in the symptoms of major depression disorder. Journal of Nervous and Mental Disease. 2007;195:905–911. doi: 10.1097/NMD.0b013e3181594cb7. [DOI] [PubMed] [Google Scholar]
- Romero-Daza N, Weeks M, Singer M. “Nobody gives a damn if I live or die”: Violence, drugs, and street-level prostitution in inner-city Hartford, Connecticut. Medical Anthropology. 2003;22:233–259. doi: 10.1080/01459740306770. [DOI] [PubMed] [Google Scholar]
- Rosario M, Schrimshaw EW, Hunter J. A model of sexual risk behaviors among young gay and bisexual men: Longitudinal associations of mental health, substance abuse, sexual abuse, and the coming-out process. AIDS Education and Prevention. 2006;18:444–460. doi: 10.1521/aeap.2006.18.5.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross CE, Mirowsky J. Sex differences in the effect of education on depression: Resource multiplication or resource substitution? Social Science and Medicine. 2006;63:1400–1413. doi: 10.1016/j.socscimed.2006.03.013. [DOI] [PubMed] [Google Scholar]
- Ross MW, Rosser BRS, Neumaier ER. The relationship of internalized homonegativity to unsafe sexual behavior in HIV-seropositive men who have sex with men. AIDS Education and Prevention. 2008;20:547–557. doi: 10.1521/aeap.2008.20.6.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safren SA, Traeger L, Skeer MR, O’Cleirigh C, Meade CS, Covahey C, Mayer KH. Testing a social-cognitive model of HIV transmission risk behaviors in HIV-infected MSM with and without depression. Health Psychology. 2010;29:215–221. doi: 10.1037/a0017859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salomon EA, Mimiaga MJ, Husnik MJ, Welles SL, Mayer KH, et al. Depressive symptoms, utilization of mental health care, substance use and sexual risk among young men who have sex with men in EXPLORE: Implications for age-specific interventions. AIDS and Behavior. 2009;13:811–821. doi: 10.1007/s10461-008-9439-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schrimshaw EW, Rosario M, Meyer-Bahlburg HFL, Scharf-Matlick AA. Test-retest reliability of self-reported sexual behavior, sexual orientation, and psychosexual milestones among gay, lesbian, and bisexual youths. Archives of Sexual Behavior. 2006;35:225–234. doi: 10.1007/s10508-005-9006-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semple SJ, Patterson TL, Grant I. Psychosocial predictors of unprotected anal intercourse in a sample of HIV positive gay men who volunteer for sexual risk reduction intervention. AIDS Education and Prevention. 2000;12:416–430. [PubMed] [Google Scholar]
- Semple SJ, Strathdee SA, Zians J, Patterson TL. Sexual risk behavior associated with co-administration of methamphetamine and other drugs in a sample of HIV-positive men who have sex with men. American Journal on Addictions. 2009;18:65–72. doi: 10.1080/10550490802544466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semple SJ, Zians J, Grant I, Patterson TL. Sexual compulsivity in a sample of HIV-positive methamphetamine-using gay and bisexual men. AIDS and Behavior. 2006;10:587–598. doi: 10.1007/s10461-006-9127-1. [DOI] [PubMed] [Google Scholar]
- Senn TE, Carey MP, Vanable PA. The intersection of violence, substance use, depression, and STDs: Testing of a syndemic pattern among patients attending an urban STD clinic. Journal of the National Medical Association. 2010;102:614–620. doi: 10.1016/s0027-9684(15)30639-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shernoff M. Condomless sex: Considerations for psychotherapy with individual gay men and male couples having unsafe sex. Journal of Gay and Lesbian Mental Health. 2005;9:149–169. [Google Scholar]
- Siconolfi DE, Halkitis PN, Barton SC, Kingdom MJ, Brennan-Ing M, et al. Psychosocial and demographic correlates of drug use in a sample of HIV-positive adults aged 50 and older. Prevention Science. 2013 doi: 10.1007/s11121-012-0338-6. e-publication ahead of print. [DOI] [PubMed] [Google Scholar]
- Singer M. Introduction to syndemics: A systems approach to public and community health. San Francisco, CA: Jossey-Bass; 2009. [Google Scholar]
- Singer MC, Erickson PI, Badiane L, Diaz R, Ortiz D, Abraham T, Nicolaysen AM. Syndemics, sex and the city: Understanding sexually transmitted diseases in social and cultural context. Social Science and Medicine. 2006;63:2010–2021. doi: 10.1016/j.socscimed.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stall R, Mills T, Williamson J, Hart T. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. American Journal of Public Health. 2003;93:939–942. doi: 10.2105/ajph.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein JA, Rotheram-Borus MJ, Swendeman D, Milburn NG. Predictors of sexual transmission risk behaviors among HIV-positive young men. AIDS Care. 2005;17:433–442. doi: 10.1080/09540120412331291724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse Mental Health Services Administration. 2007 National Survey on Drug Use and Health: Detailed tables. Rockville, MD: Office of Applied Studies; 2008. [Google Scholar]
- U.S. Census Bureau. Profiles of general demographic characteristics 2000. Washington, DC: U.S. Government Printing Office; 2001. [Google Scholar]
- U.S. Census Bureau. GCT-PH1 Population, housing units, area, and density: 2000. Washington, DC: U.S. Government Printing Office; 2000. [Google Scholar]
- Walch SE, Rudolph SE. Negative affect and risk for Human Immunodeficiency Virus: One size may not fit all. American Journal of Health Promotion. 2006;20:324–333. doi: 10.4278/0890-1171-20.5.324. [DOI] [PubMed] [Google Scholar]
- Walkup J, Blank MB, Gonzales JS, Safren S, Schwartz R, Brown L, Wilson I, Knowlton A, Lombard F, Grossman C, Lyda K, Schumacher JE. The impact of mental health and substance abuse factors on HIV prevention and treatment. Journal of Acquired Immune Deficiency Syndromes. 2008;47:s15–s19. doi: 10.1097/QAI.0b013e3181605b26. [DOI] [PubMed] [Google Scholar]
- Watkins DG, Hudson DL, Howard C, Siefert K, Jackson JS. Discrimination, mastery, and depressive symptoms among African American men. Research on Social Work Practice. 2011;21:269–277. doi: 10.1177/1049731510385470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weir SS, Roddy RE, Zekeng L, Ryan KA. Association between condom use and HIV infection: A randomised study of self reported condom use measures. Journal of Epidemiology and Community Health. 1999;53:417–422. doi: 10.1136/jech.53.7.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yi H, Sandfort TGM, Shidlo A. Effects of disengagement coping with HIV risk on unprotected sex among HIV-negative gay men in New York City. Health Psychology. 2010;29:205–214. doi: 10.1037/a0017786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zakalik RA, Wei M. Adult attachment, perceived discrimination based on sexual orientation, and depression in gay males: Examining the mediation and moderation effects. Journal of Counseling Psychology. 2006;53:302–313. [Google Scholar]
- Zen AL, Whooley MA, Zhao S, Cohen BE. Post-traumatic stress disorder is associated with poor health behaviors: Findings from the Heart and Soul Study. Health Psychology. 2011 doi: 10.1037/a0025989. published online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]


