Abstract
Introduction
Plasmodium vivax malaria has a wide geographic distribution and poses challenges to malaria elimination that are likely to be greater than those of P. falciparum. Diagnostic tools for P. vivax infection in non-reference laboratory settings are limited to microscopy and rapid diagnostic tests but these are unreliable at low parasitemia. The development and validation of a high-throughput and sensitive assay for P. vivax is a priority.
Methods
A high-throughput LAMP assay targeting a P. vivax mitochondrial gene and deploying colorimetric detection in a 96-well plate format was developed and evaluated in the laboratory. Diagnostic accuracy was compared against microscopy, antigen detection tests and PCR and validated in samples from malaria patients and community controls in a district hospital setting in Sabah, Malaysia.
Results
The high throughput LAMP-P. vivax assay (HtLAMP-Pv) performed with an estimated limit of detection of 1.4 parasites/ μL. Assay primers demonstrated cross-reactivity with P. knowlesi but not with other Plasmodium spp. Field testing of HtLAMP-Pv was conducted using 149 samples from symptomatic malaria patients (64 P. vivax, 17 P. falciparum, 56 P. knowlesi, 7 P. malariae, 1 mixed P. knowlesi/P. vivax, with 4 excluded). When compared against multiplex PCR, HtLAMP-Pv demonstrated a sensitivity for P. vivax of 95% (95% CI 87–99%); 61/64), and specificity of 100% (95% CI 86–100%); 25/25) when P. knowlesi samples were excluded. HtLAMP-Pv testing of 112 samples from asymptomatic community controls, 7 of which had submicroscopic P. vivax infections by PCR, showed a sensitivity of 71% (95% CI 29–96%; 5/7) and specificity of 93% (95% CI87-97%; 98/105).
Conclusion
This novel HtLAMP-P. vivax assay has the potential to be a useful field applicable molecular diagnostic test for P. vivax infection in elimination settings.
Author Summary
Plasmodium vivax has a worldwide distribution and is the second most common causative agent of human malaria. The dormant liver stage of P. vivax allows the infection to recur unless diagnosed and treated appropriately, which poses a significant challenge to the goals of malaria elimination and eradication as outlined by the WHO. Although highly sensitive molecular diagnostic tools are available in reference laboratory settings, the currently available diagnostic tools outside referral settings for the detection of P. vivax are limited to microscopy and rapid diagnostic tests, which are insufficiently sensitive for the detection of low level parasitemia particularly in asymptomatic individuals. Based on a DNA amplification technology called loop-mediated isothermal amplification (LAMP), this study describes the development and validation of a colourimetric, high throughput assay (HtLAMP) suitable for the detection of P. vivax infection in non-referral settings. The sensitivity of the assay combined with its field applicability offers the potential for it to play an important role as a diagnostic tool for the purpose of malaria elimination.
Introduction
Plasmodium vivax is the most geographically widespread of the Plasmodium species that infect humans [1] and can cause severe and fatal disease [2]. In the 2014 World Malaria Report it was estimated that there were 15.8 million cases of P. vivax in 2013, accounting for 47% of malaria cases outside the African region [3]. Asymptomatic sub-microscopic P. vivax infection is commonly reported in endemic countries [4–6], accounting for on average 69.5% of P. vivax infection relative to those with patent parasitaemias from community surveys [7], compared with 50.8% for P. falciparum [8]. The parasite reservoir of P. vivax is also aided by the dormant liver stage which can cause relapsing infection, with fast gametocyte production allowing transmission earlier in the course of the disease, and the development of multidrug resistance [9] posing difficulties for both clinical management and malaria elimination goals.
In non-referral settings in elimination areas, the diagnostic tools currently available for detection of P. vivax infections for case management and surveillance are microscopy and immunochromatographic lateral-flow antigen detection in the form of “rapid diagnostic tests” (RDTs). Reference laboratories may also offer expert microscopy and PCR. The reliability of RDTs for diagnosing P. vivax infections, particularly at low level parasitemia, remains less than that for P. falciparum [4,10]. While the most recent WHO RDT testing report found the highest performing parasite lactate-dehyrogenase (pLDH) based P. vivax RDTs were equivalent to HRP2-based P. falciparum RDTs at parasitemias of 200/μL [11], they remain inadequately sensitive for the detection of lower level P. vivax and P. falciparum parasitemia in sub-patent asymptomatic individuals. While microscopy and RDT provide adequate diagnostic accuracy for case management of symptomatic patients in clinical settings, they have been shown to be inadequate in detecting a large proportion of low density P.falciparum infections in active community surveillance [12], and for mass screening and treatment programs [13]. Studies using RDTs specifically for detection of P. vivax in this context are yet to be performed, although similar results could be expected given the inherently lower parasitemias associated with P. vivax infection. Although molecular based assays such as conventional PCR are capable of detecting very low density infections, they are not suitable for large scale community surveillance due to complex procedures that do not allow provision of test results on the day of sample, expensive reagents and the requirement for specialised equipment.
Loop mediated isothermal amplification (LAMP) is a molecular diagnostic technology that has the potential to be a readily-applicable tool in settings such as malaria elimination. LAMP is an isothermal process that relies on the Bacillus stearothermophilus (Bst) enzyme and does not require cyclical temperature changes [14]. As such, unlike PCR, it offers an opportunity for field adaptation because of its low technology requirement. The output of a LAMP reaction can be visualised as a magnesium pyrophosphate precipitate detectable by turbidimetry [14], metal ion detectors such as calcein [15], hydroxynaphthol blue [16] and pico-green [17]. In addition to melting curve analysis [18], LAMP end products have also been visualised using a bioluminescent output in real time(BART) [19], a lateral flow dipstick [20], or a portable device with a fluorescence detecting unit (realAmp) [21]. LAMP has also recently been performed on non-instrumented nucleic acid amplification (NINA) platforms [22] improving its potential for field application.
LAMP has been shown to detect all Plasmodium species [23] including P. knowlesi [24,25], to be amenable to use with crudely extracted DNA from whole blood [26], and to have a limit of detection of 5 parasites/ μL for identifying Plasmodium genus and P. falciparum [27]. Commercially available Loopamp MALARIA detection kits (Eiken chemical co) using Plasmodium genus and P. falciparum have been found to perform well in regional health facilities, but were not capable of specifically detecting P. vivax [28,29]. Furthermore, for specific detection of P. vivax, the three LAMP assays published to date have had low analytic sensitivity, with reported detection limits of 100 plasmid copies/ μL for 18s rRNA target [23] (which was equivalent to 500 parasites/ μL when tested by Patel et.al [30]), 125 parasites/μL for Pvr64 target (highly conserved repeat region in P. vivax genome) [30] and 100 copies/ μL for alpha-tubulin target [31].
Here we describe the development and validation of a novel P. vivax specific LAMP assay targeting mitochondrial DNA in a high-throughput, colourimetric platform. Its performance was compared to PCR and microscopy in a district hospital, non reference laboratory setting.
Methods
The clinical samples used retrospectively in this study to validate the P. vivax specific primers were obtained with ethics approval granted by the Malaysian Medical Research Ethics Committee, Menzies School of Health Research, Australia, and London School of Hygiene and Tropical Medicine, UK.
Parasite samples used for validating primers and limit of detection (LOD)
Primers were tested against parasite DNA from well characterised parasite lines and clinical samples of P. falciparum (3D7), P. vivax, P. malariae, P. ovale spp. and P. knowlesi for cross-reactivity and LOD.
In order to determine the analytical sensitivity of the HtLAMP-Pv, a two-fold dilution series of a P. vivax DNA sample beginning at a starting parasitemia of 90,000 parasites/ μL (as determined by quantitative PCR) was evaluated in duplicate. HtLAMP-Pv performance was compared with that of previously published P. vivax primers [23,30] in the HtLAMP platform. In addition, a sample of starting parasitemia of 2000 parasites/ μL (as determined by expert microscopy) was serially diluted in 50% haematocrit uninfected blood. DNA from each dilution was extracted using Qiagen blood kit and tested in duplicate using the HtLAMP-Pv assay.
Comparison between HtLAMP-Pv and RDT
The limit of detection of the HtLAMP-Pv assay was compared with the SD Bioline Pf/Pan RDT (Alere Standard Diagnostics). This RDT detects P. falciparum histidine-rich protein II (HRP-II) and Plasmodium lactate dehydrogenase (pLDH) with a reported sensitivity of 100% at 200 parasites/μL [11], microscopy and quantitative PCR on a blood sample obtained from a P. vivax blood stage clinical trial (ACTRN12614000930684) participant. Informed consent was obtained as per the approval of the QIMR Berghofer HREC. Briefly, a wild type P. vivax bank was produced using blood collected from a patient, who had returned to Australia from a malaria endemic country with PCR-proven P. vivax malaria infection, prior to treatment with artemether-lumefantrine. The clinical trial was performed as described [32] and a 2 ml EDTA-blood sample was collected from the clinical trial participant at peak parasitemia prior to commencement of antimalarial treatment. This sample was serially diluted in 50% haematocrit blood and each dilution was subjected to an LDH ELISA assay, thick film blood smear for expert microscopy, an SD Bioline Pf/Pan RDT (Alere Standard Diagnostics) and 4 x 5 μL filter paper (whatman) blood spots. The filter paper blood spots and the remaining whole blood, which had been stored at -20°C, was extracted in 10 μL and 50 μL volumes using modified chelex-saponin based DNA extraction protocols as described below. The extracted DNA was stored at -20°C until performance of the HtLAMP-Pv assay.
Diagnostic accuracy and field testing of HtLAMP-Pv
The sensitivity and specificity of the P. vivax HtLAMP was tested retrospectively on clinical samples from patients enrolled in a randomised controlled trial and case-control study performed in Sabah, Malaysia commencing in December 2012 as outlined by Grigg et al. [33]. Briefly, samples were collected from microscopy positive, symptomatic patients presenting as outpatients to Kota Marudu District Hospital and asymptomatic, microscopy negative, community controls as a result of reactive active case detection from within the village of a case patient from Kota Marudu district, Sabah. These were stored as 20 μL filter paper (Whatman) blood spots. A subset of 149 microscopy positive samples and 112 microscopy negative samples were used to compare the performance of the P. vivax HtLAMP (HtLAMP-Pv), with microscopy and PCR. DNA extraction of the filter paper samples from symptomatic patients and HtLAMP-Pv were performed in the Kota Marudu district hospital laboratory, with no standing molecular diagnostic capability, using a plastic bucket adapted into a water bath, a centrifuge and a portable spectrophotometer. Two local staff members were trained in the process of performing and interpreting the assay as part of its evaluation.
DNA extraction
The P.vivax DNA used for the analysis of sensitivity was extracted from whole blood samples as per Qiagen manufacturing protocol (QIAamp DNA mini kit) with some modifications. Briefly, 500 μL of packed red cell blood sample was mixed with 500 μL of PBS. To an aliquot of 500 μL of this mix, 400 μL of Qiagen AL Lysis buffer and 40 μL of Qiagen proteinase K were added. After incubation at 56°C for 10 minutes, 400 μL of 100% ethanol was added, mixed then loaded into a spin column for centrifugation at 8,000 rpm for 1 min. The spin column was then washed once with 650 μL of AW1 and then AW2 spinning each wash at 8,000 rpm for 1 min followed by a dry spin after the AW2 wash at 13,000 rpm for 1 minute. Nucleic acid extract were eluted in 100 μL of elution buffer and stored at -20°C until LAMP reactions were performed.
P. vivax DNA from the Kota Marudu clinical filter spot samples from symptomatic patients was extracted using an established chelex protocol [34] with incubations shortened to improve turnaround time. Briefly, 6 mm filter paper punch samples were incubated in PBS containing 0.5% saponin for 2 hours at 37°C, before being centrifuged, washed in PBS, heated at 98°C for 30 minutes in 150 μL 6% chelex and centrifuged at 4,000 rpm for 3 minutes. The resultant 100 μL DNA supernatant was then stored at -20°C until analysis by PCR and LAMP.
Red cell pellet samples from asymptomatic individuals were extracted using a different chelex protocol. Briefly, 1 ml of non-ionised water was incubated with 10 μL of whole blood for 15–30 minutes at room temperature, followed by centrifugation at 10,000–15,000 x g for 3 minutes. After discarding supernatant, 200 μL of 5% chelex was added, vortexed for 5–10 seconds, incubated at 55°C for 30–90 minutes and vortexed again for 5–10 seconds. The sample was then heated for 10 minutes at 100°C, vortexed for 5–10 seconds and centrifuged for 3 minutes at 10,000–15,000 x g. The DNA supernatant was placed in a sterile microfuge tube for storage at -20°C.
Whole blood samples, for the comparative study with RDTs, were extracted using a chelex-based DNA extraction methodology [35] modified by the addition of saponin. Briefly, 10 μL of whole blood was mixed with either 200 μL of 0.5% saponin and incubated at 37°C for 30 minutes. Samples were then centrifuged, supernatant discarded and pellet heated at 98°C in 150 μL of 6% chelex for 30 minutes. The resultant supernatant was stored at -20°C. The process was also performed on 50 μL of whole blood.
Positive control plasmid
In order to establish specificity of the P. vivax LAMP primers, a plasmid containing P. vivax cox1 gene was constructed. The target region of the gene was amplified using COX1 specific PCR primers. Reactions were performed in 20 μL total volume containing 1X NH4 buffer, 2 mM MgCl2, 200 μM dNTPs, 200 μM primer mix and 0.5 U Taq polymerase (Bioline). The ~500 bp PCR product was visualised following agarose gel electrophoresis. The PCR product was purified using a commercial kit (Roche) and TA cloned using pGEM-T easy as per manufacturer instructions. Recombinant E. coli were identified by blue-white colour selection. Presence of the P. vivax cox1 gene within the plasmid was confirmed by PCR and Sanger sequencing.
Estimation of the number of mitochondrial cox1 genes in the P. vivax genome
Copy number of the pvcox1 gene in the P. vivax genome was estimated by quantitative real time PCR SYBR green PCR assay using the Light Cycler 96 (Roche). Two single copy genes coding for P. vivax mdr1 (GenBank Acc No. AY618622.1) and P. vivax aldolase (GenBank Acc No. AF247063) were used as reference genes to estimate the pvcox1 copy number. PCR reactions were set up in triplicates using the Roche Fast Start Essential DNA Green Master Mix (Cat. No. 06 402 712 001), 10 μM of each primer (Table 1) and 1 μl of each DNA (cox1 plasmid, mdr/aldolase plasmid, Pv gDNA) in a 12 μl reaction volume. Cycling conditions were: 950 C for 3 mins; 45 cycles of 950 C 30 secs and 600 C for 1 min. This was followed by melt curve analysis to confirm correct products were synthesised.
Table 1. Primers used to amplify Pv mdr, aldolase and cox 1 (*Source [36]).
| Gene | Primer name | Sequence |
|---|---|---|
| pv mdr* | Pvmdr F | 5’ CTGATACAAGTGAGG AAG AACTAC G 3’ |
| Pvmdr R | 5’ GTCCACCTGACAACTTAGATGC 3’ | |
| pv aldolase* | Pvaldo F | 5’ GACAGTGCCACCATCCTTACC 3’ |
| PvaldoR | 5’ CCTTCTCAACATTCTCCTTCTTTCC 3’ | |
| pv cox 1 | V1V2F3 | 5’ GGTACTGGATGGACTTTATAT 3’ |
| V1V2B3 | 5’ GGTAATGTTAATAATAGCATTACAG 3’ |
To assess PCR amplification efficiencies, standard curves containing five ten-fold dilutions of two plasmids containing either pvcox 1, or pvmdr1 and pvaldolase (1:1) Suwanarusk, 2007 [36] were prepared, starting from the same initial concentration of 7.2 x10-4 ng/μl. Differences in CT value between pvcox1 and pvmdr1/pvaldolase at each plasmid concentration was calculated and averaged to derive ΔCTcal. After confirming similar amplification efficiencies, genomic DNA extracted from 5 well characterised P. vivax isolates with varying DNA concentrations were used in the copy number assay. These samples were from patients enrolled in a clinical trial and surveillance study, with ethics approval granted by the Malaysian Medical Research Ethics Committee and Menzies School of Health Research, Australia, conducted in Kota Marudu district, Sabah, Malaysia[37,38]. Mean Ct values were calculated from triplicate and analysed using Graph Pad Prism (version 6). The pvcox1 copy number in each sample was calculated as N = 2 ΔΔ Ct +/- SD i.e. N = 2 (CTpvmdr1-CTpvcox1)-(CTpvmdr1cal-CTpvcox1cal) as reported in Suwanarusk, 2007 [36].
PCR
Nested PCR for P. vivax was performed as previously published [39]. Reactions were performed in 20 μL total volume containing 1X buffer, 2 mM MgCl2, 200 μM dNTPs, 200 μM primer mix (rPLU5new/rPLU6 for nest 1 and rVIV1/rVIV2 for nest 2) and 0.5 U Taq polymerase (Bioline). PCR products were visualised on a 2% agarose gel.
Multiplex PCR [40] for the detection of P. falciparum, P. vivax, P. malariae and P. ovale was performed on clinical samples from the 149 symptomatic case samples, with P. knowlesi confirmed using PCR as described by Imwong et al. [41]. Nested PCR, as described by Singh et al. [42], was performed on the 112 community control samples. Quantitative PCR on the P. vivax blood stage clinical trial sample was performed as previously described [32].
High-throughput LAMP
High throughput (HtLAMP) was performed on a 96-well standard u-bottom microtitre plate (Sterihealth) as previously described [43]. Briefly, reactions were performed in 25 μL total volume containing 5 μL DNA, 1X buffer (20 mM Tris HCL pH 8.8, 10 mM KCl, 8 mM MgSO4, 10 mM(NH4)SO4), 1.25 mM each dNTP, 1.78 μM each FIP/ BIP, 0.8 μM each LF/ LB, 0.2 μM each F3/ B3), 120 μM hydroxynaphthol-blue (Fluka, CAS number 63451-35-4)and 8 units Bst polymerase (New England Biolabs, Ipswich, MA). The microtitre plate was incubated in a waterbath at 65°C for 30 minutes before the colour change and precipitate in each well was recorded. A blue colour change with a visible precipitate was scored as a positive result, and purple colour without a precipitate was a negative result (Fig 1). The microtitre plate was then read in an ELISA plate reader at 600 nm wavelength to obtain an optical density (OD) reading of each well. The threshold value for a positive reaction was calculated using the mean plus two standard deviations of the no template control (NTC) wells. A positive or negative OD reading for each sample was then calculated using the threshold value and correlated with the visually detected colour change. Samples that were discordant in terms of colour change and OD threshold were deemed negative.
Fig 1. HtLAMP colour change associated with hydroxynaphtholblue (HNB).
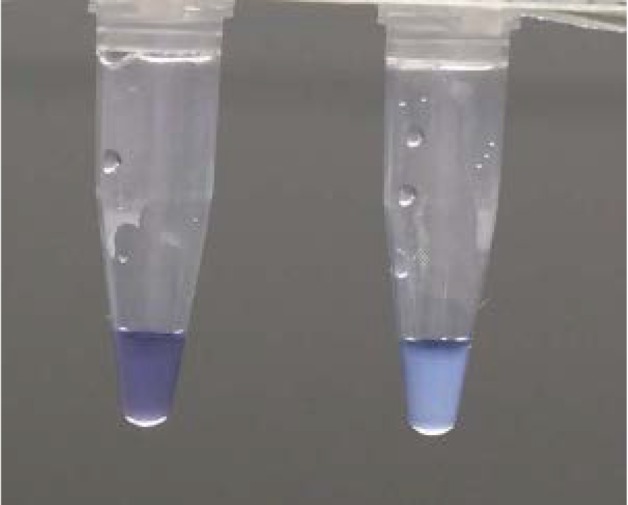
Left clear, purple colour = negative and right cloudy, blue colour = positive.
Statistical analysis
PCR, nested or multiplex, for the detection of P. vivax was used as the gold standard by which the sensitivity and specificity of HtLAMP-Pv was calculated. PCR is the best established molecular diagnostic tool available for the detection of Plasmodium parasites and therefore an appropriate choice for comparison of a new molecular diagnostic modality.
Sensitivity was estimated as the number of LAMP positives that were also PCR positive, divided by the number of PCR positives. Specificity was estimated as the number of LAMP negatives that were also PCR negative divided by the total number of PCR negatives.
Results
P.vivax LAMP primers
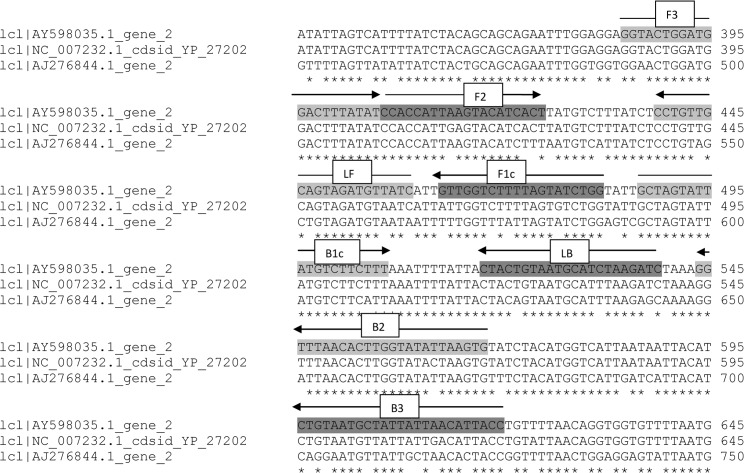
Two sets of LAMP primers (VIV1 and VIV2) targeting P. vivax mitochondrial sequences were designed manually. Each set of primers was tested for its ability to amplify P. vivax-specific DNA. However, only one set of primers (VIV2) targeting the P. vivax mitochondrial cox1 gene (Table 2 and Fig 2), was subject to further validation as the other set failed to amplify P. vivax DNA. The specificity of VIV2 primers was investigated by searching for nucleotide similarity using the BLAST algorithm at the NCBI nucleotide database (www.ncbi.nlm.nih.gov/Blast.cgi) and found to have limited sequence identity only to other Plasmodium species. Given the conserved nature of the mitochondrial genome and the sequence similarity across different P.vivax strains from around the world, no evaluation of VIV2 primers on different P.vivax strains was performed.
Table 2. P. vivax VIV2 HtLAMP primer sequences (5’ → 3’).
| Primer | Sequence |
|---|---|
| F3 | GGTACTGGATGGACTTTATAT |
| B3 | GGTAATGTTAATAATAGCATTACAG |
| LF | GATAACATCTACTGCAACAGG |
| LB | CTACTGTAATGCATCTAAGATC |
| FIP | CCAGATACTAAAAGACCAACCCACCATTAAGTACATCACT |
| BIP | GCTAGTATTATGTCTTCTTTCACTTAATATACCAAGTGTTAAACC |
Fig 2. P. vivax VIV2 HtLAMP primer set superimposed on alignments of P. vivax (AY598035), P. falciparum (AJ276844) and P. knowlesi (NC_007232) cox1 genes.
Species-specificity of VIV2 LAMP primers
The VIV2 primer set was tested in duplicate on DNA extracts from one PCR-confirmed sample of each of the following species: P. vivax, P. falciparum, P. knowlesi, P. malariae, P. ovale wallikeri and P. ovale curtisi. There was amplification of P. vivax and P. knowlesi DNA but no amplification product was detected for P. falciparum, P. malariae, P. ovale wallikeri or P. ovale curtisi.
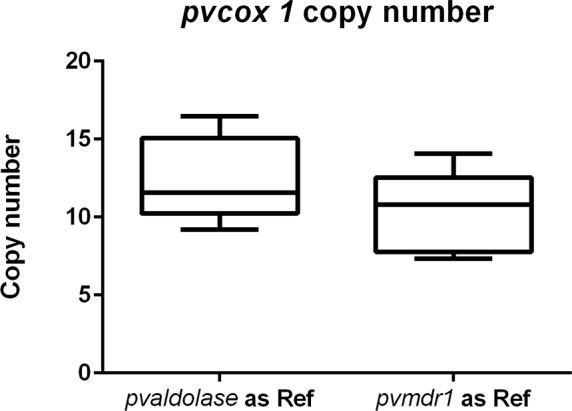
Quantification of mitochondrial cox1 gene copy numbers in the P. vivax genome
Using the single-copy P. vivax aldolase gene as reference, the estimated copy number of pvcox1 in five selected P. vivax samples ranged from 9.2–16.47 with a mean of 12.43 (± 1.233). Using the pvmdr1 gene as reference, the estimated copy number of pvcox1 ranged from 7.32–14.05 with a mean of 10.28 (± 1.182) (Fig 3).
Fig 3. Estimated Plasmodium vivax cox1 copy number based on comparison with two single copy genes, pv aldolase1 and pvmdr1.
Limit of detection of HtLAMP-Pv
Using a two-fold DNA dilution series of a clinical P. vivax sample, with a starting parasitemia of 90,000 parasites/ μL as determined by quantitative PCR, the LOD was 1.4 parasites/ μL (Table 3). Using the same dilutions, the LOD of P. vivax LAMP primers published by Han [23] and Patel [30], in the HtLAMP platform was determined to be706 parasites/ μL and 176 parasites/ μL respectively. HtLAMP-Pv performed on the microscopy-determined P. vivax dilution series in whole blood had an LOD of 2 parasites/ μL (Table 4).
Table 3. Analytical sensitivity of HtLAMP-Pv, compared with other published P. vivax LAMP primers, using a DNA dilution series of clinical sample with qPCR confirmed parasitemia.
Each sample was tested in duplicate in the HtLAMP platform using each of the three P. vivax LAMP primer sets. The dilution at which both duplicates were positive was the limit of detection for each of the primer sets in the HtLAMP platform (Pos* indicates dilutions at which only one of the duplicates was positive). HtLAMP-Pv was able to detect 1.4 parasites/ μL compared with previously published P. vivax LAMP primers.
| Sample | Quantitative PCR (parasites/μL calculated) | [23] 18s rRNA target | [30] Pvr64 target | HtLAMP-Pv cox1 target |
|---|---|---|---|---|
| 1 Original | 90,000 | Pos | Pos | Pos |
| 2 | 45,000 | Pos | Pos | Pos |
| 3 | 22,500 | Pos | Pos | Pos |
| 4 | 11,250 | Pos | Pos | Pos |
| 5 | 5625 | Pos | Pos | Pos |
| 6 | 2813 | Pos | Pos | Pos |
| 7 | 1406 | Pos | Pos | Pos |
| 8 | 703 | Pos | Pos | Pos |
| 9 | 352 | Pos* | Pos | Pos |
| 10 | 176 | Pos | Pos | |
| 11 | 88 | Pos | ||
| 12 | 44 | Pos | ||
| 13 | 22 | Pos | ||
| 14 | 11 | Pos | ||
| 15 | 5.5 | Pos | ||
| 16 | 2.7 | Pos* | Pos | |
| 17 | 1.4 | Pos | ||
| 18 | 0.7 | Pos* | ||
| 19 | 0.3 |
Table 4. Analytical sensitivity of HtLAMP-Pv on microscopy-determined whole blood P. vivax dilution series.
The limit of detection HtLAMP-Pv is 2 parasites/ μL, performed in duplicate and where both duplicates were positive.
| P. vivax Parasites /μL | HtLAMP-Pv |
|---|---|
| 2000 | Pos |
| 200 | Pos |
| 20 | Pos |
| 2 | Pos |
| 0.2 | Neg |
| 0 | Neg |
HtLAMP-Pv vs RDT
Quantitative PCR analysis of the P. vivax blood stage clinical trial sample confirmed a peak parasitemia of 12 parasites/ μL prior to commencement of antimalarial therapy. HtLAMP-Pv was positive and the RDT was negative at this level of parasitemia. The limit of detection (LOD) of the HtLAMP-Pv assay varied depending on the type and volume of sample from which DNA was extracted. The LOD for filter paper extracted using saponin and chelex was more than 12 parasites/ μL whereas the LOD for 10 μL and 50 μL of whole blood extracted using saponin and chelex was 3 parasites/ μL and 1.5 parasites/ μL respectively (Table 5).
Table 5. Comparing microscopy and RDT with the limit of detection of HtLAMP-Pv using filter paper and whole blood at 10 μL and 50 μL volumes.
| 0.75 parasites/ μL | 1.5 parasites/ μL | 3.0 parasites/ μL | 6.0 parasites/ μL | 12 parasites/ μL | |
|---|---|---|---|---|---|
| Microscopy | Neg | Neg | Pos | Pos | Pos |
| RDT | Neg | Neg | Neg | Neg | Neg |
| Filter paper (5 μL) | Neg | Neg | Neg | Neg | Pos |
| Whole blood 10 μL | Neg | Neg | Pos | Pos | Pos |
| Whole blood 50 μL | Neg | Pos | Pos | Pos | Pos |
The limit of detection (LOD) of the HtLAMP-Pv assay depends on the starting sample material and the volume of blood extracted. LOD threshold was determined by the presence of 2 positive duplicate tests (ie: 4 positive results) at a particular parasitemia. The LOD for a 5 μL filter paper blood spot extracted using a chelex-saponin protocol was more than 12 parasites/ μL. The LOD for 10 μL of whole blood extracted using a chelex-saponin protocol was 3 parasites/ μL compared with 50 μL of whole blood which was 1.5 parasites/ μL.
Sensitivity and specificity of HtLAMP-Pv in symptomatic patients
Of the 149 patients with microscopy-confirmed malaria from the district of Kota Marudu, Sabah, Malaysia, 145 were confirmed by PCR: 4 samples were excluded due to lack of microscopy and PCR data, 56 were identified as P. knowlesi (median parasitemia 2005 parasites/ μL, range 26–143,790), 64 as P. vivax (median parasitemia 4676 parasites/ μL, range 53–89,640), 7 as P. malariae, 17 as P. falciparum (median parasitemia 18,725 parasites/ μL, range 837–693,922) and 1 as a mixed P knowlesi/P. vivax infection. HtLAMP-Pv was compared with multiplex PCR in these clinical samples. The sensitivity of HtLAMP-Pv for P. vivax was 95% (62/65, 95% CI 87–99) and specificity was 55% (44/80, 95% CI 43–66) respectively compared with multiplex PCR and 94% (59/62, 95% CI 85–98) and 53% (44/83, 95% CI 42–64) respectively compared with expert microscopy (Table 2). The low specificity of the assay can be attributed to cross-reactivity of the VIV2 primers with P. knowlesi, with 97% sequence homology at the cox1 gene between P. vivax and P. knowlesi. When P. knowlesi samples were excluded from the analysis, the specificity was 100% compared with both multiplex PCR and microscopy (Table 6).
Table 6. Sensitivity and specificity of HtLAMP-Pv for P. vivax in symptomatic patients in Sabah with P. falciparum, P. vivax and P. knowlesi.
149 filter paper samples were tested by HtLAMP-Pv; 4 samples were excluded due to a lack of PCR and microscopy data. Among the 145 samples, PCR confirmation of species was as follows: n = 64 P. vivax n = 56 P. knowlesi, n = 17 P. falciparum, n = 7 P. malariae and n = 1 mixed P. vivax/P. knowlesi infection.
| Sensitivity | Specificity | |
|---|---|---|
| HtLAMP-Pv compared with multiplex PCR | 62/65(95%) | 44/80 (55%) |
| (95% CI 87–99) | (95% CI 43–66) | |
| HtLAMP-Pv compared with multiplex PCR excluding Pk samples | 62/65(95%) | 24/24 (100%) ( |
| (95% CI 87–99) | 95% CI 87–99) | |
| HtLAMP-Pv compared with microscopy | 59/62 (95%) | 44/83 (53%) |
| (95% CI 85–98) | (95% CI 42–64) | |
| HtLAMP-Pv compared with microscopy excluding Pk samples | 59/62 (95%) | 18/18 (100%) |
| (95% CI 85–98) | (95% CI 81–100) | |
| Multiplex PCR compared with microscopy | 60/65 (92%) | 78/80 (98%) |
| (95% CI 83–97) | (95% CI 91–99) |
Sensitivity and specificity of HtLAMP-Pv in asymptomatic, reactive active case detection community control patients
HtLAMP-Pv was compared with nested PCR for red cell pellet samples from asymptomatic, microscopy negative community controls from the malaria endemic district of Kota Marudu, Sabah, Malaysia. The sensitivity of HtLAMP-Pv was 71% (95% CI 29–96; 5/7) and specificity was 93% (95% CI 87–97; 98/105) compared with PCR.
Turnaround time of assay
The HtLAMP assay turnaround time was 1 hour after DNA extraction, 4 hours when combined with whole blood chelex saponin protocol and 6 hours when combined with filter paper rapid DNA extraction protocol.
Applicability of the assay in a non-reference laboratory in a resource limited setting
HtLAMP-Pv testing of a total of 149 filter paper samples was performed successfully in a regional hospital laboratory in Kota Marudu district, Sabah, Malaysia. Good workflow set up ensured that there was no contamination despite the lack of formal molecular diagnostic infrastructure. Locally trained staff was able to perform and interpret results of the HtLAMP-Pv assay using only a centrifuge, pipettes, water bath and a portable spectrophotometer.
Discussion
Field-applicable diagnostic tools for the detection of Plasmodium vivax are essential components for the malaria eradication agenda [44]. Given the widespread distribution and unique challenges P. vivax poses compared with P. falciparum, there is a pressing need for the development of species- specific molecular diagnostic tools. LAMP is a molecular diagnostic tool which holds much promise in terms of its ability to be deployed in non-referral laboratory settings, given its simplicity and rapid assay turnaround time, ability to be performed on crudely extracted DNA from both whole blood and filter paper and lack of expensive equipment. The colourimetric, 96 well microtitre plate-based platform for performing LAMP (HtLAMP) for the detection of Plasmodium parasites, as previously described [43], increases the throughput of the LAMP using minimal equipment. The objective of this paper was to develop and validate a P. vivax specific HtLAMP assay on this platform with good diagnostic accuracy.
The 6-kb mitochondrial genome of the genus Plasmodium encodes three mitochondrial proteins- cytochrome B (cytb) and subunit 1 and 3 of cytochrome c oxidase (cox1 and cox3), and is estimated to be present in relatively high copy number. The complete mitochondrial genome of P. vivax (Genbank AY598035) has been shown to be closely related to P. knowlesi [45]. Previously published standard PCR primers for P. vivax targeting cox1 have shown 100% sensitivity and specificity [46], but were not evaluated against P. knowlesi. LAMP primers targeting mitochondrial sequences for the detection of P. genus and P. falciparum demonstrated an analytical sensitivity of 5 parasites/ μL [27] suggesting that mitochondrial DNA offers an attractive target, presumably due to increased copy number of mitochondrial targets within cells. Recent estimates of genomic sequence coverage have shown that the P. falciparum genome contains ~20 copies/cell of the mitochondrial genome [47].
This HtLAMP-Pv assay targeting the conserved cox1 gene demonstrated excellent analytic sensitivity, being able to detect 1.4 parasites/ μL. This is the lowest LOD so far achieved for a published P. vivax–specific LAMP assay. The estimated copy number for cox1 in P. vivax is approximately 11 copies/ cell. Therefore, it is likely that the sensitivity of the HtLAMP-Pv assay is a reflection of the increased number of mitochondrial targets per cell. Previously published P. vivax LAMP primers, which targeted non-mitochondrial genes, when used in the HtLAMP platform had limits of detection of 706 parasites/ μL and 176 parasites/ μL which correlated well with published limits of detection of 125–500 parasites/ μL for these P. vivax primers sets [30].
The pkcox1 gene of P. knowlesi exhibits 97% sequence identity with pvcox1 at the nucleotide level, and thus the cross-reactivity of the VIV2 primers between these two species was expected. However, there was no cross-reactivity with P. falciparum (87% sequence identity), P. ovale wallikeri (92%), P. ovale curtisi (92%) or P. malariae (93%).
Validation of the HtLAMP-Pv in clinical samples of symptomatic patients with vivax, falciparum and knowlesi malaria demonstrated sensitivity for P. vivax of 94–95% and a specificity of 53–55% compared with microscopy and multiplex PCR respectively. The poor specificity however was a reflection of the cross-reactivity with P. knowlesi. When P. knowlesi samples were excluded from the analysis, the specificity of the HtLAMP-Pv assay improved to 100%, compared with both multiplex PCR and microscopy.
While this cross-reactivity appears to be a limitation of this HtLAMP-Pv assay, P. knowlesi malaria is uncommon or absent in most areas of P. vivax endemicity, so this would be an important consideration only in Malaysia, where P. knowlesi predominates [48] and in the other countries in south-east Asia where P. knowlesi human infection has been documented [49]. In terms of treatment, both P. vivax and P. knowlesi respond to artemisinin-based combination therapy (ACT) [50]. However, in elimination programmes utilising primaquine for radical cure of P. vivax malaria, there is a potential risk of inappropriate use of this potentially haemolytic drug in people with P. knowlesi infections. This is a problem localised to Southeast Asia, and would not pose a problem for LAMP-based detection and radical treatment of P. vivax for malaria elimination elsewhere.
The HtLAMP-Pv assay was also evaluated in a limited sample set of asymptomatic, microscopy negative, community control patients enrolled from the same village as a case patient, as a result of reactive active case detection. Although the LOD of HtLAMP-Pv appears to be 1.4 parasites/ μL, in this sample set its sensitivity was only 71%. This may be due to the very low parasitemias in these 7 PCR positive samples or variability due to stochastic effects at such low parasitemias. Therefore further validation in a larger sample set is required to confirm the sensitivity of HtLAMP-Pv in this population in order to evaluate the potential role for HtLAMP-Pv as a diagnostic tool in malaria elimination settings.
HtLAMP-Pv showed significantly better sensitivity than the SD Bioline Pf/Pan RDT at low parasitemia. RDTs were negative in the serially diluted samples at 12 parasites/ μL. HtLAMP-Pv was positive at this level. The analytical sensitivity of the assay varied depending on whether filter paper samples or whole blood was used irrespective of the chelex-saponin DNA extraction protocol used. This may have important implications for choosing the type of sample collected in addition to choosing the appropriate diagnostic tool for surveillance or screening policy and protocols for malaria elimination programs.
In this study we also demonstrated that HtLAMP-Pv performed well in the 96-well microtitre plate platform for increasing the throughput of the assay in a non-referral laboratory in a district hospital in Sabah, Malaysia. DNA extraction was performed in the non-referral laboratory using a chelex protocol on filter paper blood spots and the HtLAMP-Pv assay was able to process these samples in a simple water-bath within one hour from time of DNA extraction. Positive and negative results were readily identified by two locally trained staff by visual inspection of the colour change. Optical densitometry readings at 600 nm in portable photospectrometer were used to provide objective confirmation of the visually detected results. As such the validation of this HtLAMP-Pv assay in a rural district laboratory setting confirms the potential it has as a field-applicable molecular diagnostic tool. Furthermore, the process of assay validation using the combination of visual and optical densitometry values has previously shown that the visually detectable colour change was reliable for determining both positive and negative results [43]. Therefore while the photospectrometer offers objective confirmation, it is not an essential component of the assay.
Some of the limitations to this platform pertain to DNA extraction. Firstly, in order to maintain cost effectiveness of the assay, modified chelex-based protocols were used for whole blood and filter paper extractions. Although these multi-step DNA extraction processes, which relied on a centrifuge, were performed adequately in a resource limited setting, further simplification of DNA extraction would enhance the feasibility of the HtLAMP-Pv assay. It would also allow a greater number of samples to be processed, as might be required for mass surveillance for malaria elimination, thereby making full use of the high throughput aspect of the HtLAMP platform. Secondly, while equivalent small volumes of blood on filter paper and whole blood have shown whole blood to produce better analytical sensitivity in the HtLAMP platform [43], the limit of detection of HtLAMP-Pv using larger volumes of blood on filter paper is yet to be established.
In conclusion, this study outlines the development and validation of a novel P. vivax-specific LAMP assay which combines a low limit of detection with a high throughput, colourimetric, field applicable molecular diagnostic assay. As such, this HtLAMP assay holds much promise as a diagnostic tool to support malaria elimination efforts in resource-limited P. vivax endemic settings.
Acknowledgments
We thank Kim Piera (Menzies School of Health Research) for providing the P. vivax dilution series and sample shipments. We thank Marina Chavchich (Australian Army Malaria Institute) for providing the plasmid containing pvmdr1 and pvaldolase1 genes and for assay assistance.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by Malaysian Ministry of Health (Grant #BP00500420), AusAlD Asia-Pacific Malaria Elimination Network (Grant #108-07), Australian National Health and Medical Research Council (Program grant #1037304, Project Grant #1045156, Practitioner fellowship to NMA #1042072 and JSM #1041802, scholarship to SB #1055410 and MJG #1074795), and UK Medical Research Council (ESEI) (grant #1100796). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
References
- 1.Gething PW, Elyazar IR, Moyes CL, Smith DL, Battle KE, et al. (2012) A long neglected world malaria map: Plasmodium vivax endemicity in 2010. PLoS Negl Trop Dis 6: e1814 10.1371/journal.pntd.0001814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anstey NM, Douglas NM, Poespoprodjo JR, Price RN (2012) Plasmodium vivax: clinical spectrum, risk factors and pathogenesis. Adv Parasitol 80: 151–201. 10.1016/B978-0-12-397900-1.00003-7 [DOI] [PubMed] [Google Scholar]
- 3.WHO (2014) WHO Global Malaria Program—World Malaria Report 2014. Switzerland.
- 4.Harris I, Sharrock WW, Bain LM, Gray KA, Bobogare A, et al. (2010) A large proportion of asymptomatic Plasmodium infections with low and sub-microscopic parasite densities in the low transmission setting of Temotu Province, Solomon Islands: challenges for malaria diagnostics in an elimination setting. Malar J 9: 254 10.1186/1475-2875-9-254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baum E, Sattabongkot J, Sirichaisinthop J, Kiattibutr K, Davies DH, et al. (2015) Submicroscopic and asymptomatic Plasmodium falciparum and Plasmodium vivax infections are common in western Thailand—molecular and serological evidence. Malar J 14: 611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thanh PV, Van Hong N, Van Van N, Van Malderen C, Obsomer V, et al. (2015) Epidemiology of forest malaria in Central Vietnam: the hidden parasite reservoir. Malar J 14: 601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cheng Q, Cunningham J, Gatton ML (2015) Systematic review of sub-microscopic P. vivax infections: prevalence and determining factors. PLoS Negl Trop Dis 9: e3413 10.1371/journal.pntd.0003413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Okell LC, Ghani AC, Lyons E, Drakeley CJ (2009) Submicroscopic infection in Plasmodium falciparum-endemic populations: a systematic review and meta-analysis. J Infect Dis 200: 1509–1517. 10.1086/644781 [DOI] [PubMed] [Google Scholar]
- 9.Price R, Tjira E, Guerra C, Yeung S, White N, et al. (2007) Vivax malaria: Neglected but not benign. American Journal of Tropical Medicine and Hygiene 77: 79–87. [PMC free article] [PubMed] [Google Scholar]
- 10.Mikhail AF, Leslie TJ, Mayan MI, Zekria R, Mohammad N, et al. (2011) Field trial of three different Plasmodium vivax-detecting rapid diagnostic tests with and without evaporative cool box storage in Afghanistan. Malar J 10: 169 10.1186/1475-2875-10-169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.WHO (2014) Malaria Rapid Diagnostic Test Performance- Summary results of WHO product testing of malaria RDTs: Round 1–5 (2008–2013). Italy: WHO. [Google Scholar]
- 12.Tiono AB, Ouedraogo A, Diarra A, Coulibaly S, Soulama I, et al. (2014) Lessons learned from the use of HRP-2 based rapid diagnostic test in community-wide screening and treatment of asymptomatic carriers of Plasmodium falciparum in Burkina Faso. Malar J 13: 30 10.1186/1475-2875-13-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cook J, Xu W, Msellem M, Vonk M, Bergstrom B, et al. (2015) Mass screening and treatment on the basis of results of a Plasmodium falciparum-specific rapid diagnostic test did not reduce malaria incidence in Zanzibar. J Infect Dis 211: 1476–1483. 10.1093/infdis/jiu655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mori Y, Nagamine K, Tomita N, Notomi T (2001) Detection of loop-mediated isothermal amplification reaction by turbidity derived from magnesium pyrophosphate formation. Biochem Biophys Res Commun 289: 150–154. [DOI] [PubMed] [Google Scholar]
- 15.Tomita N, Mori Y, Kanda H, Notomi T (2008) Loop-mediated isothermal amplification (LAMP) of gene sequences and simple visual detection of products. Nat Protoc 3: 877–882. 10.1038/nprot.2008.57 [DOI] [PubMed] [Google Scholar]
- 16.Goto M, Honda E, Ogura A, Nomoto A, Hanaki K (2009) Colorimetric detection of loop-mediated isothermal amplification reaction by using hydroxy naphthol blue. Bio Techniques 46: 1637–1172. [DOI] [PubMed] [Google Scholar]
- 17.Wastling SL, Picozzi K, Kakembo ASL, Welburn SC (2010) LAMP for Human African Trypanosomiasis: A Comparative study of detection formats. PLoS Negl Trop Dis 4: e865 10.1371/journal.pntd.0000865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yamamura M, Makimura K, Ota Y (2009) Evaluation of a new rapid molecular diagnostic system for Plasmodium falciparum combined with DNA filter paper, loop-mediated isothermal amplification, and melting curve analysis. Jpn J Infect Dis 62: 20–25. [PubMed] [Google Scholar]
- 19.Kiddle G, Hardinge P, Buttigieg N, Gandelman O, Pereira C, et al. (2012) GMO detection using a bioluminescent real time reporter (BART) of loop mediated isothermal amplification (LAMP) suitable for field use. BMC Biotechnol 12: 15 10.1186/1472-6750-12-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yongkiettrakul S, Jaroenram W, Arunrut N, Chareanchim W, Pannengpetch S, et al. (2014) Application of loop-mediated isothermal amplification assay combined with lateral flow dipstick for detection of Plasmodium falciparum and Plasmodium vivax. Parasitol Int 63: 777–784. 10.1016/j.parint.2014.06.004 [DOI] [PubMed] [Google Scholar]
- 21.Lucchi NW, Demas A, Narayanan J, Sumari D, Kabanywanyi A, et al. (2010) Real-time fluorescence loop mediated isothermal amplification for the diagnosis of malaria. PLoS One 5: e13733 10.1371/journal.pone.0013733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sema M, Alemu A, Bayih A, Getie S, Getnet G, et al. (2015) Evaluation of non-instrumented nucleic acid amplification by loop-mediated isothermal amplification (NINA-LAMP) for the diagnosis of malaria in Northwest Ethiopia. Malar J 14: 44 10.1186/s12936-015-0559-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Han E, Watanabe R, Sattabongkot J, Khuntirat B, Sirichaisinthop J, et al. (2007) Detection of four Plasmodium species by genus and species- specific loop mediated isothermal amplication for clinical diagnosis. Journal of Clinical Microbiology 45: 2521–2528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lau YL, Fong MY, Mahmud R, Chang PY, Palaeya V, et al. (2011) Specific, sensitive and rapid detection of human Plasmodium knowlesi infection by loop-mediated isothermal amplification (LAMP) in blood samples. Malar J 10: 197 10.1186/1475-2875-10-197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Iseki H, Kawai S, Takahashi N, Hirai M, Tanabe K, et al. (2010) Evaluation of a loop-mediated isothermal amplification method as a tool for diagnosis of infection by the zoonotic simian malaria parasite Plasmodium knowlesi. J Clin Microbiol 48: 2509–2514. 10.1128/JCM.00331-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Poon LL, Wong BW, Ma EH, Chan KH, Chow LM, et al. (2006) Sensitive and inexpensive molecular test for falciparum malaria: detecting Plasmodium falciparum DNA directly from heat-treated blood by loop-mediated isothermal amplification. Clin Chem 52: 303–306. [DOI] [PubMed] [Google Scholar]
- 27.Polley SD, Mori Y, Watson J, Perkins MD, Gonzalez IJ, et al. (2010) Mitochondrial DNA targets increase sensitivity of malaria detection using loop-mediated isothermal amplification. J Clin Microbiol 48: 2866–2871. 10.1128/JCM.00355-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cook J, Aydin-Schmidt B, Gonzalez IJ, Bell D, Edlund E, et al. (2015) Loop-mediated isothermal amplification (LAMP) for point-of-care detection of asymptomatic low-density malaria parasite carriers in Zanzibar. Malar J 14: 43 10.1186/s12936-015-0573-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vallejo AF, Martinez NL, Gonzalez IJ, Arevalo-Herrera M, Herrera S (2015) Evaluation of the loop mediated isothermal DNA amplification (LAMP) kit for malaria diagnosis in P. vivax endemic settings of Colombia. PLoS Negl Trop Dis 9: e3453 10.1371/journal.pntd.0003453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Patel JC, Oberstaller J, Xayavong M, Narayanan J, Debarry JD, et al. (2013) Real-Time Loop-Mediated Isothermal Amplification (RealAmp) for the Species-Specific Identification of Plasmodium vivax. PLoS One 8: e54986 10.1371/journal.pone.0054986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dinzouna-Boutamba SD, Yang HW, Joo SY, Jeong S, Na BK, et al. (2014) The development of loop-mediated isothermal amplification targeting alpha-tubulin DNA for the rapid detection of Plasmodium vivax. Malar J 13: 248 10.1186/1475-2875-13-248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McCarthy JS, Griffin PM, Sekuloski S, Bright AT, Rockett R, et al. (2013) Experimentally induced blood-stage Plasmodium vivax infection in healthy volunteers. J Infect Dis 208: 1688–1694. 10.1093/infdis/jit394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Grigg MJ, William T, Drakeley CJ, Jelip J, von Seidlein L, et al. (2014) Factors that are associated with the risk of acquiring Plasmodium knowlesi malaria in Sabah, Malaysia: a case-control study protocol. BMJ Open 4: e006004 10.1136/bmjopen-2014-006004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Plowe CV, Djimde A, Bouare M, Doumbo O, Wellems TE (1995) Pyrimethamine and proguanil resistance-conferring mutations in Plasmodium falciparum dihydrofolate reductase: polymerase chain reaction methods for surveillance in Africa. Am J Trop Med Hyg 52: 565–568. [DOI] [PubMed] [Google Scholar]
- 35.Walsh PS, Metzger DA, Higuchi R (1991) Chelex 100 as a medium for simple extraction of DNA for PCR-based typing from forensic material. Biotechniques 10: 506–513. [PubMed] [Google Scholar]
- 36.Suwanarusk R, Russell B, Chavchich M, Chalfein F, Kenangalem E, et al. (2007) Chloroquine resistant Plasmodium vivax: in vitro characterisation and association with molecular polymorphisms. PLoS One 2: e1089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grigg MJ, William T, Dhanaraj P, Menon J, Barber BE, et al. (2014) A study protocol for a randomised open-label clinical trial of artesunate-mefloquine versus chloroquine in patients with non-severe Plasmodium knowlesi malaria in Sabah, Malaysia (ACT KNOW trial). BMJ Open 4: e006005 10.1136/bmjopen-2014-006005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barber BE, William T, Grigg MJ, Menon J, Auburn S, et al. (2013) A prospective comparative study of knowlesi, falciparum, and vivax malaria in Sabah, Malaysia: high proportion with severe disease from Plasmodium knowlesi and Plasmodium vivax but no mortality with early referral and artesunate therapy. Clin Infect Dis 56: 383–397. 10.1093/cid/cis902 [DOI] [PubMed] [Google Scholar]
- 39.Snounou G, Viriyakosol S, Zhu XP, Jarra W, Pinheiro L, et al. (1993) High sensitivity of detection of human malaria parasites by the use of nested polymerase chain reaction. Mol Biochem Parasitol 61: 315–320. [DOI] [PubMed] [Google Scholar]
- 40.Padley D, Moody AH, Chiodini PL, Saldanha J (2003) Use of a rapid, single-round, multiplex PCR to detect malarial parasites and identify the species present. Ann Trop Med Parasitol 97: 131–137. [DOI] [PubMed] [Google Scholar]
- 41.Imwong M, Tanomsing N, Pukrittayakamee S, Day NP, White NJ, et al. (2009) Spurious amplification of a Plasmodium vivax small-subunit RNA gene by use of primers currently used to detect P. knowlesi. J Clin Microbiol 47: 4173–4175. 10.1128/JCM.00811-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Singh B, Bobogare A, Cox-Singh J, Snounou G, Abdullah MS, et al. (1999) A genus- and species-specific nested polymerase chain reaction malaria detection assay for epidemiologic studies. Am J Trop Med Hyg 60: 687–692. [DOI] [PubMed] [Google Scholar]
- 43.Britton S, Cheng Q, Sutherland CJ, McCarthy JS (2015) A simple, high-throughput, colourimetric, field applicable loop-mediated isothermal amplification (HtLAMP) assay for malaria elimination. Malar J 14: 335 10.1186/s12936-015-0848-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.MalERA (2011) A research agenda for malaria eradication: diagnoses and diagnostics. PLoS Med 8: e1000396 10.1371/journal.pmed.1000396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jongwutiwes S, Putaporntip C, Iwasaki T, Ferreira MU, Kanbara H, et al. (2005) Mitochondrial genome sequences support ancient population expansion in Plasmodium vivax. Mol Biol Evol 22: 1733–1739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cunha MG, Medina TS, Oliveira SG, Marinho AN, Povoa MM, et al. (2009) Development of a Polymerase Chain Reaction (PCR) method based on amplification of mitochondrial DNA to detect Plasmodium falciparum and Plasmodium vivax. Acta Trop 111: 35–38. 10.1016/j.actatropica.2009.02.003 [DOI] [PubMed] [Google Scholar]
- 47.Preston MD, Campino S, Assefa SA, Echeverry DF, Ocholla H, et al. (2014) A barcode of organellar genome polymorphisms identifies the geographic origin of Plasmodium falciparum strains. Nat Commun 5: 4052 10.1038/ncomms5052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.William T, Jelip J, Menon J, Anderios F, Mohammad R, et al. (2014) Changing epidemiology of malaria in Sabah, Malaysia: increasing incidence of Plasmodium knowlesi. Malar J 13: 390 10.1186/1475-2875-13-390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Moyes CL, Henry AJ, Golding N, Huang Z, Singh B, et al. (2014) Defining the geographical range of the Plasmodium knowlesi reservoir. PLoS Negl Trop Dis 8: e2780 10.1371/journal.pntd.0002780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Grigg MJ, William T, Menon J, Dhanaraj P, Barber BE, et al. (2015) Artesunate-mefloquine versus chloroquine for treatment of uncomplicated Plasmodium knowlesi malaria in Malaysia (ACT KNOW): an open-label, randomised controlled trial. Lancet Infect Dis. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.