Abstract
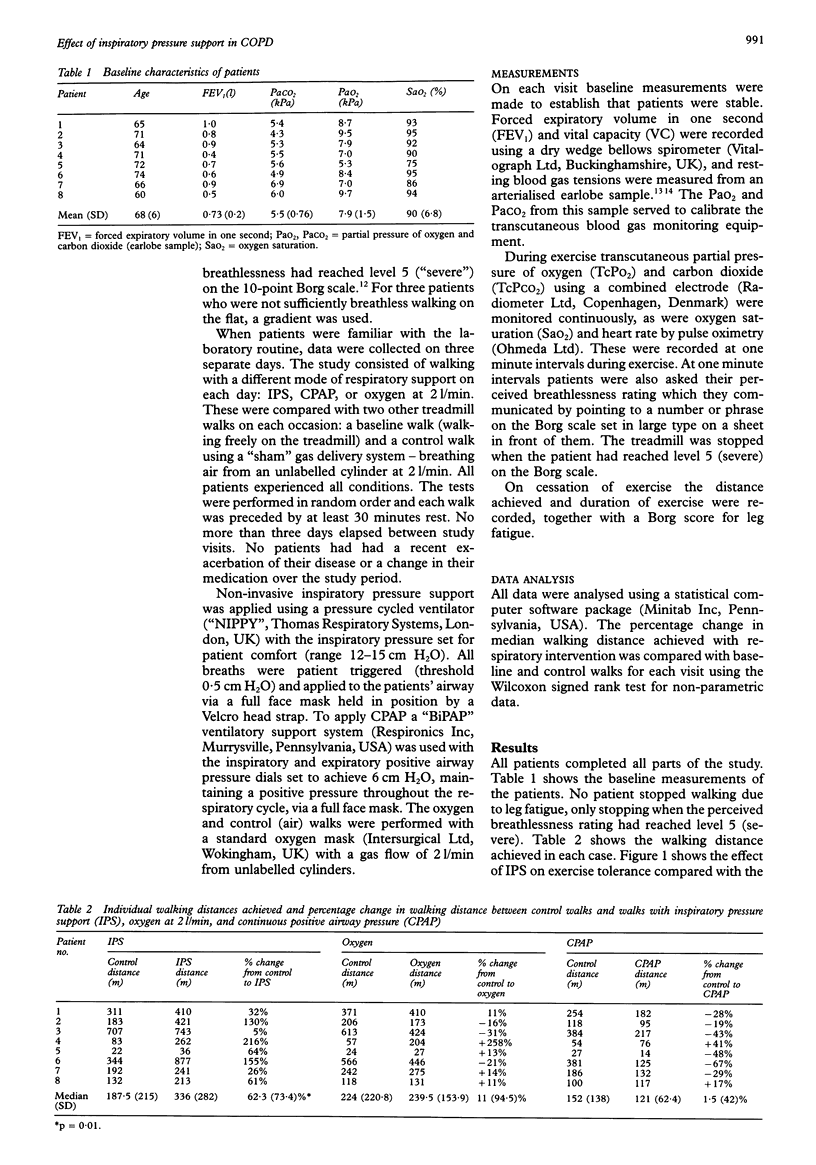
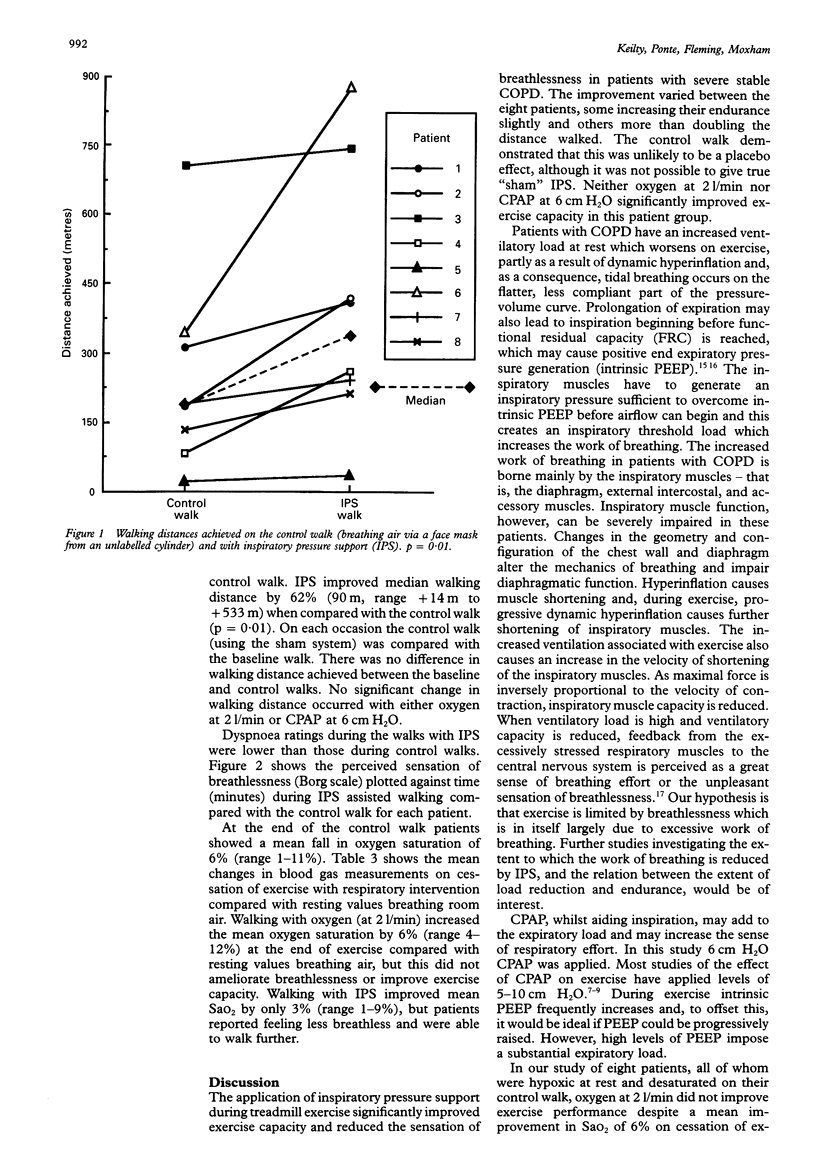
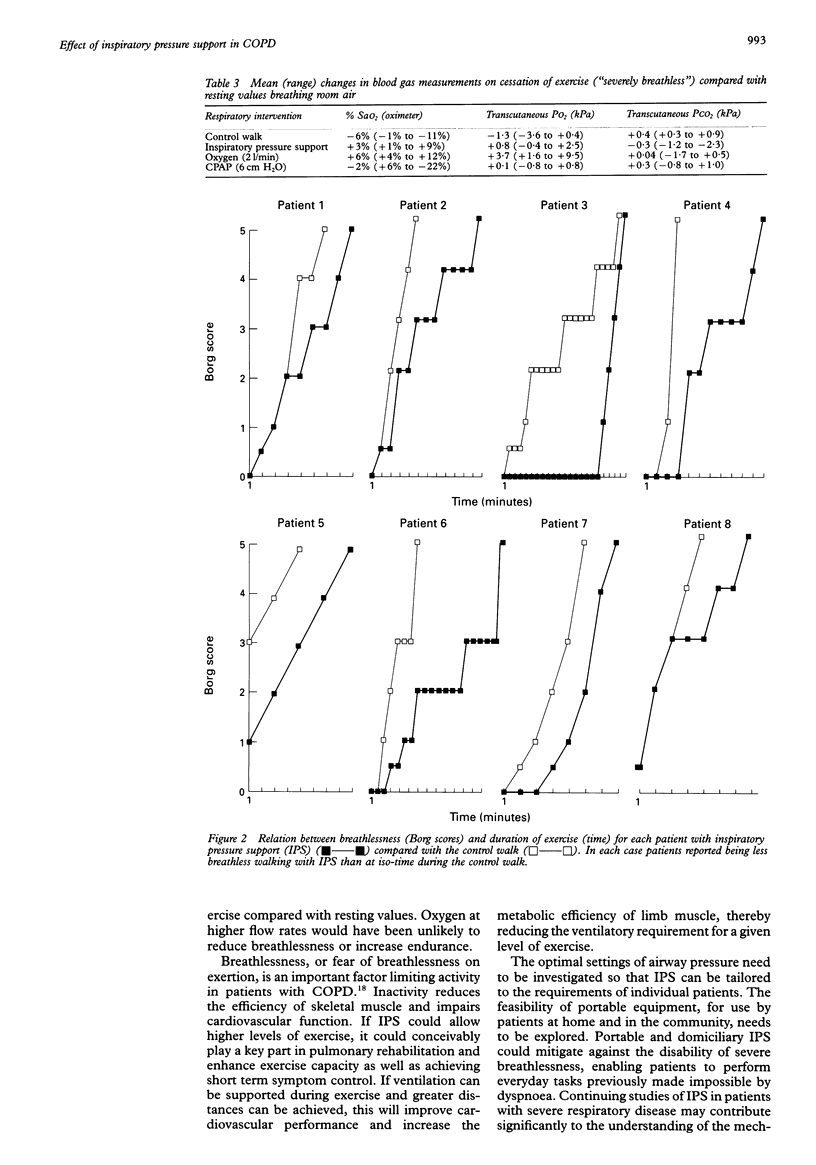
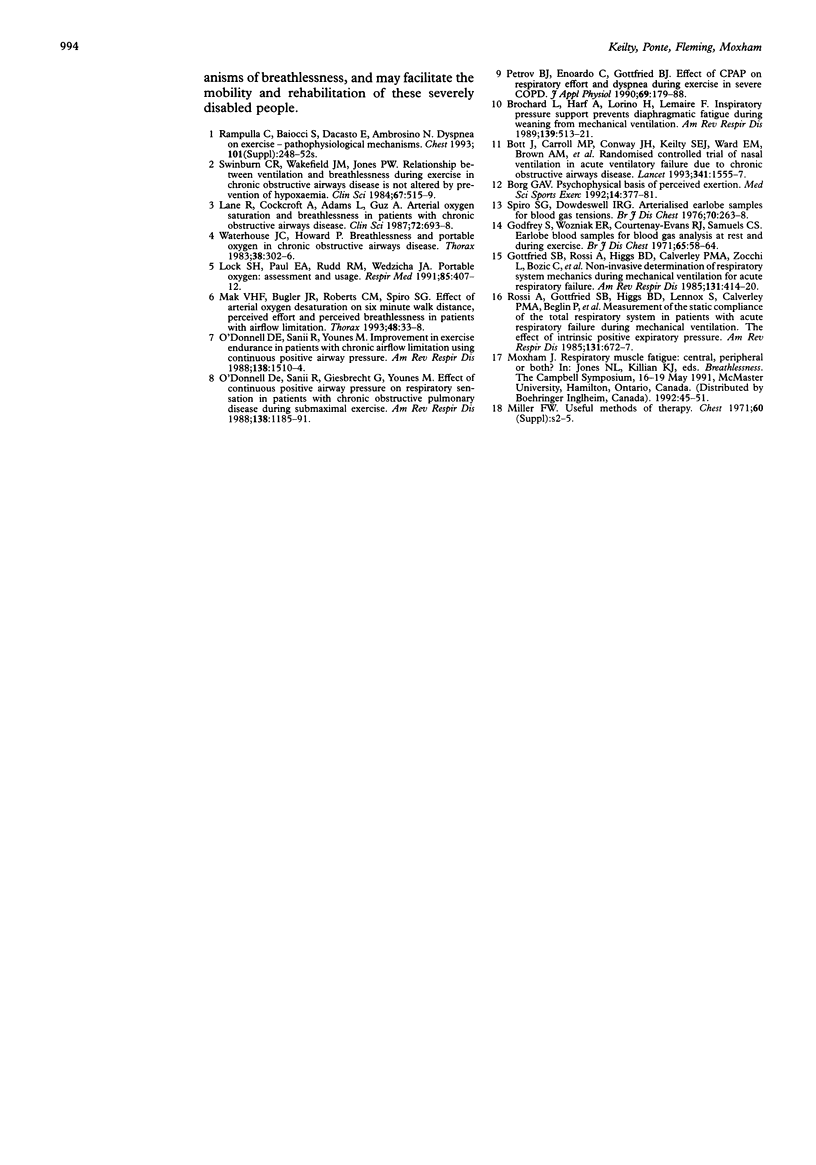
BACKGROUND--In patients with chronic obstructive pulmonary disease exercise tolerance is commonly limited by breathlessness. These patients have an increased ventilatory load at rest which is exacerbated during exercise. The purpose of this study was to investigate the effect of supporting ventilation by non-invasive inspiratory pressure support (IPS) during submaximal treadmill exercise in such patients to see if they would experience less breathlessness and improve their exercise capacity. METHODS--Eight men with disabling breathlessness due to chronic obstructive pulmonary disease (COPD) (mean (SD) FEV1 0.73 (0.2) 1) were studied. Patients walked on a treadmill until their sensation of breathlessness, scored at one minute intervals, reached level 5 ("severe") on the 10-point Borg scale. Studies were performed with IPS (mean airway pressure 12-15 cm H2O), continuous positive airway pressure (CPAP 6 cm H2O), and with oxygen (2 l/min via a mask) in random order on three separate days. Each of these walks was compared with a control walk using a sham circuit (breathing air via an oxygen mask at 2 l/min from an unlabelled cylinder), and with a baseline walk in which patients walked freely on the treadmill. On cessation of exercise, distance achieved and a leg fatigue score were recorded. RESULTS--No patients stopped due to leg fatigue, all stopping only when their sensation of breathlessness had reached level 5 on the Borg scale. IPS improved median walking distance by 62% compared with the control walk (sham circuit). There was no change in walking distance with either CPAP or oxygen at 2 l/min. There was no difference between the control and the baseline walks. CONCLUSIONS--Inspiratory pressure support can reduce breathlessness and increase exercise tolerance to submaximal treadmill exercise in patients with COPD. This could have implications for the rehabilitation of these severely disabled patients.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Borg G. A. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377–381. [PubMed] [Google Scholar]
- Bott J., Carroll M. P., Conway J. H., Keilty S. E., Ward E. M., Brown A. M., Paul E. A., Elliott M. W., Godfrey R. C., Wedzicha J. A. Randomised controlled trial of nasal ventilation in acute ventilatory failure due to chronic obstructive airways disease. Lancet. 1993 Jun 19;341(8860):1555–1557. doi: 10.1016/0140-6736(93)90696-e. [DOI] [PubMed] [Google Scholar]
- Brochard L., Harf A., Lorino H., Lemaire F. Inspiratory pressure support prevents diaphragmatic fatigue during weaning from mechanical ventilation. Am Rev Respir Dis. 1989 Feb;139(2):513–521. doi: 10.1164/ajrccm/139.2.513. [DOI] [PubMed] [Google Scholar]
- Gottfried S. B., Rossi A., Higgs B. D., Calverley P. M., Zocchi L., Bozic C., Milic-Emili J. Noninvasive determination of respiratory system mechanics during mechanical ventilation for acute respiratory failure. Am Rev Respir Dis. 1985 Mar;131(3):414–420. doi: 10.1164/arrd.1985.131.3.414. [DOI] [PubMed] [Google Scholar]
- Lane R., Cockcroft A., Adams L., Guz A. Arterial oxygen saturation and breathlessness in patients with chronic obstructive airways disease. Clin Sci (Lond) 1987 Jun;72(6):693–698. doi: 10.1042/cs0720693. [DOI] [PubMed] [Google Scholar]
- Lock S. H., Paul E. A., Rudd R. M., Wedzicha J. A. Portable oxygen therapy: assessment and usage. Respir Med. 1991 Sep;85(5):407–412. doi: 10.1016/s0954-6111(06)80186-1. [DOI] [PubMed] [Google Scholar]
- Mak V. H., Bugler J. R., Roberts C. M., Spiro S. G. Effect of arterial oxygen desaturation on six minute walk distance, perceived effort, and perceived breathlessness in patients with airflow limitation. Thorax. 1993 Jan;48(1):33–38. doi: 10.1136/thx.48.1.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Donnell D. E., Sanii R., Giesbrecht G., Younes M. Effect of continuous positive airway pressure on respiratory sensation in patients with chronic obstructive pulmonary disease during submaximal exercise. Am Rev Respir Dis. 1988 Nov;138(5):1185–1191. doi: 10.1164/ajrccm/138.5.1185. [DOI] [PubMed] [Google Scholar]
- O'Donnell D. E., Sanii R., Younes M. Improvement in exercise endurance in patients with chronic airflow limitation using continuous positive airway pressure. Am Rev Respir Dis. 1988 Dec;138(6):1510–1514. doi: 10.1164/ajrccm/138.6.1510. [DOI] [PubMed] [Google Scholar]
- Petrof B. J., Calderini E., Gottfried S. B. Effect of CPAP on respiratory effort and dyspnea during exercise in severe COPD. J Appl Physiol (1985) 1990 Jul;69(1):179–188. doi: 10.1152/jappl.1990.69.1.179. [DOI] [PubMed] [Google Scholar]
- Rossi A., Gottfried S. B., Zocchi L., Higgs B. D., Lennox S., Calverley P. M., Begin P., Grassino A., Milic-Emili J. Measurement of static compliance of the total respiratory system in patients with acute respiratory failure during mechanical ventilation. The effect of intrinsic positive end-expiratory pressure. Am Rev Respir Dis. 1985 May;131(5):672–677. doi: 10.1164/arrd.1985.131.5.672. [DOI] [PubMed] [Google Scholar]
- Spiro S. G., Dowdeswell I. R. Arterialized ear lobe blood samples for blood gas tensions. Br J Dis Chest. 1976 Oct;70(4):263–268. doi: 10.1016/0007-0971(76)90042-5. [DOI] [PubMed] [Google Scholar]
- Swinburn C. R., Wakefield J. M., Jones P. W. Relationship between ventilation and breathlessness during exercise in chronic obstructive airways disease is not altered by prevention of hypoxaemia. Clin Sci (Lond) 1984 Nov;67(5):515–519. doi: 10.1042/cs0670515. [DOI] [PubMed] [Google Scholar]
- Waterhouse J. C., Howard P. Breathlessness and portable oxygen in chronic obstructive airways disease. Thorax. 1983 Apr;38(4):302–306. doi: 10.1136/thx.38.4.302. [DOI] [PMC free article] [PubMed] [Google Scholar]


