Abstract
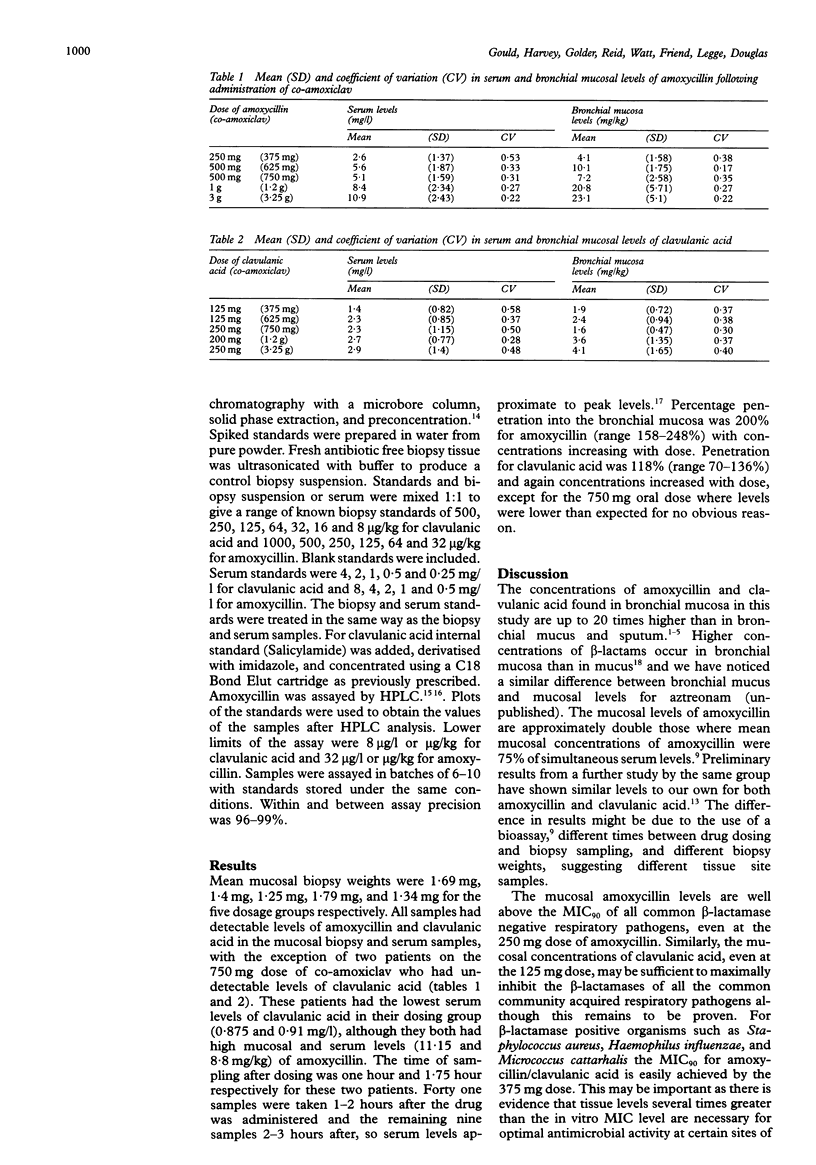
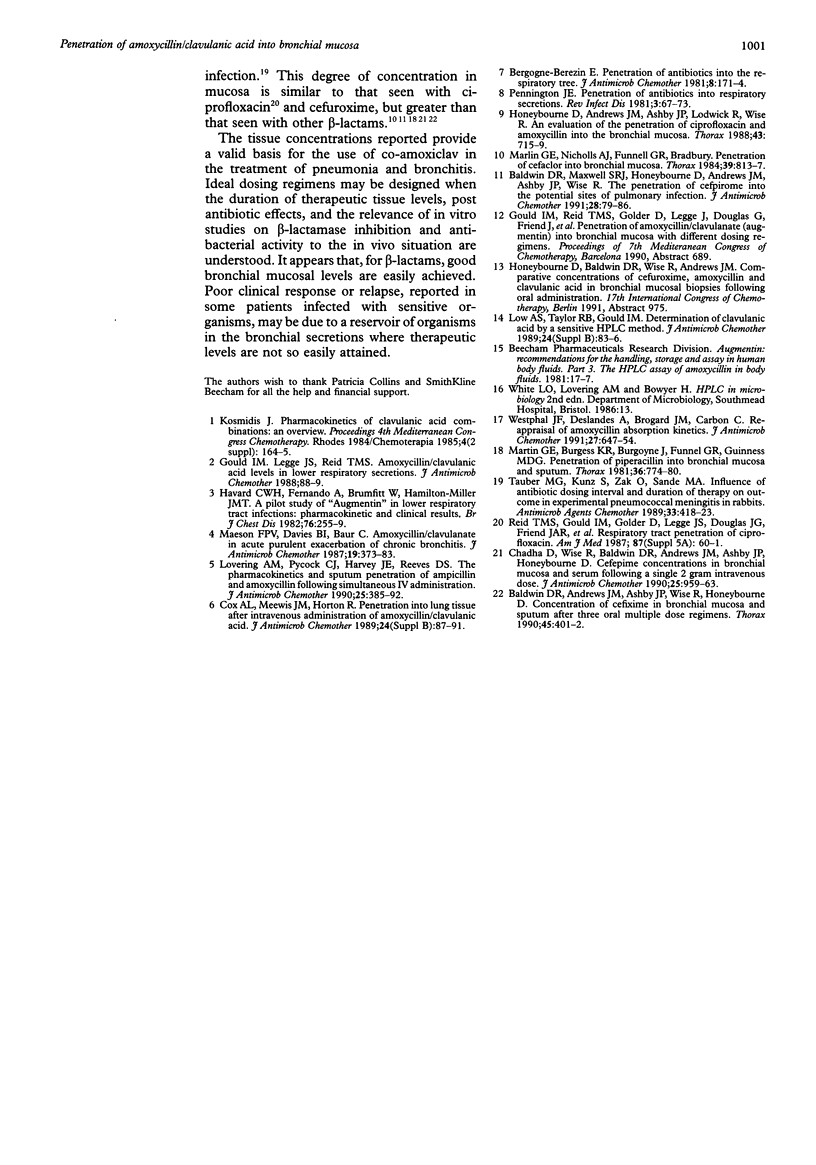
BACKGROUND--The efficacy of an antibiotic is related to its concentration at the site of infection. Previous studies of the concentrations of amoxycillin and clavulanic acid (co-amoxiclav) in respiratory secretions or whole lung tissue have suffered from methodological problems. The concentration of amoxycillin and clavulanic acid was determined in bronchial mucosal biopsy samples obtained at bronchoscopy following five different dosing regimens. METHODS--Bronchial biopsy and serum samples were obtained from 50 patients undergoing diagnostic bronchoscopy. Ten patients each received 375 mg, 625 mg, 750 mg, and 3.25 g oral, and 1.2 g intravenous co-amoxiclav 1-3 hours before bronchoscopy. The concentrations of clavulanic acid and amoxycillin were determined by high performance liquid chromatography using a microbore column, solid phase extraction, and preconcentration to improve sensitivity tenfold over previous methods. RESULTS--Concentrations of both clavulanic acid and amoxycillin in bronchial mucosa were dose related and were well above the MIC90 of co-amoxiclav for the common bacterial respiratory pathogens including Haemophilus influenzae, Micrococcus catarrhalis and Streptococcus pneumoniae for all dosing regimens. Mean mucosal levels were 200% and 118% of the corresponding serum levels for amoxycillin and clavulanic acid respectively. CONCLUSIONS--Amoxycillin and clavulanic acid are concentrated in bronchial mucosa and, even at the lowest dose of 375 mg orally, are likely to produce tissue levels in the lung sufficient to inhibit all the common community acquired respiratory pathogens.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baldwin D. R., Andrews J. M., Ashby J. P., Wise R., Honeybourne D. Concentrations of cefixime in bronchial mucosa and sputum after three oral multiple dose regimens. Thorax. 1990 May;45(5):401–402. doi: 10.1136/thx.45.5.401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldwin D. R., Maxwell S. R., Honeybourne D., Andrews J. M., Ashby J. P., Wise R. The penetration of cefpirome into the potential sites of pulmonary infection. J Antimicrob Chemother. 1991 Jul;28(1):79–86. doi: 10.1093/jac/28.1.79. [DOI] [PubMed] [Google Scholar]
- Bergogne-Berezin E. Penetration of antibiotics into the respiratory tree. J Antimicrob Chemother. 1981 Sep;8(3):171–174. doi: 10.1093/jac/8.3.171. [DOI] [PubMed] [Google Scholar]
- Chadha D., Wise R., Baldwin D. R., Andrews J. M., Ashby J. P., Honeybourne D. Cefepime concentrations in bronchial mucosa and serum following a single 2 gram intravenous dose. J Antimicrob Chemother. 1990 Jun;25(6):959–963. doi: 10.1093/jac/25.6.959. [DOI] [PubMed] [Google Scholar]
- Cox A. L., Meewis J. M., Horton R. Penetration into lung tissue after intravenous administration of amoxycillin/clavulanate. J Antimicrob Chemother. 1989 Nov;24 (Suppl B):87–91. doi: 10.1093/jac/24.suppl_b.87. [DOI] [PubMed] [Google Scholar]
- Havard C. W., Fernando A., Brumfitt W., Hamilton-Miller J. M. A pilot study of 'Augmentin' in lower respiratory tract infections: pharmacokinetic and clinical results. Br J Dis Chest. 1982 Jul;76(3):255–260. [PubMed] [Google Scholar]
- Honeybourne D., Andrews J. M., Ashby J. P., Lodwick R., Wise R. Evaluation of the penetration of ciprofloxacin and amoxycillin into the bronchial mucosa. Thorax. 1988 Sep;43(9):715–719. doi: 10.1136/thx.43.9.715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honeybourne D., Andrews J. M., Ashby J. P., Lodwick R., Wise R. Evaluation of the penetration of ciprofloxacin and amoxycillin into the bronchial mucosa. Thorax. 1988 Sep;43(9):715–719. doi: 10.1136/thx.43.9.715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovering A. M., Pycock C. J., Harvey J. E., Reeves D. S. The pharmacokinetics and sputum penetration of ampicillin and amoxycillin following simultaneous i.v. administration. J Antimicrob Chemother. 1990 Mar;25(3):385–392. doi: 10.1093/jac/25.3.385. [DOI] [PubMed] [Google Scholar]
- Low A. S., Taylor R. B., Gould I. M. Determination of clavulanic acid by a sensitive HPLC method. J Antimicrob Chemother. 1989 Nov;24 (Suppl B):83–86. doi: 10.1093/jac/24.suppl_b.83. [DOI] [PubMed] [Google Scholar]
- Maesen F. P., Davies B. I., Baur C. Amoxycillin/clavulanate in acute purulent exacerbations of chronic bronchitis. J Antimicrob Chemother. 1987 Mar;19(3):373–383. doi: 10.1093/jac/19.3.373. [DOI] [PubMed] [Google Scholar]
- Marlin G. E., Burgess K. R., Burgoyne J., Funnell G. R., Guinness M. D. Penetration of piperacillin into bronchial mucosa and sputum. Thorax. 1981 Oct;36(10):774–780. doi: 10.1136/thx.36.10.774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlin G. E., Nicholls A. J., Funnell G. R., Bradbury R. Penetration of cefaclor into bronchial mucosa. Thorax. 1984 Nov;39(11):813–817. doi: 10.1136/thx.39.11.813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Täuber M. G., Kunz S., Zak O., Sande M. A. Influence of antibiotic dose, dosing interval, and duration of therapy on outcome in experimental pneumococcal meningitis in rabbits. Antimicrob Agents Chemother. 1989 Apr;33(4):418–423. doi: 10.1128/aac.33.4.418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westphal J. F., Deslandes A., Brogard J. M., Carbon C. Reappraisal of amoxycillin absorption kinetics. J Antimicrob Chemother. 1991 May;27(5):647–654. doi: 10.1093/jac/27.5.647. [DOI] [PubMed] [Google Scholar]


