Abstract
BACKGROUND
Older people with complex health issues and needs for functional support are increasingly living in nursing home alternatives, in various residential care environments as well as at home.
OBJECTIVE
This study aims to compare the demographics, cost, and healthcare utilization of Medicare beneficiaries by the setting in which they live: nursing homes, residential care settings, and at home.
DESIGN
This study uses the 2002 to 2010 Medicare Current Beneficiary Study (MCBS) Cost and Use files to provide a national, longitudinal analysis of health status and health care use among the elderly Medicare beneficiaries, making comparisons across different living arrangements.
PARTICIPANTS
All Medicare beneficiaries aged 65 years or older who participated in the fall MCBS interview (years 2002 to 2010) and were alive for the full year (n=83,507).
MAIN MEASURES
We focus on healthcare use and cost, but also on the differences among the populations living in these settings: demographics, medical, and functional status.
KEY RESULTS
There is a gradient in health status, physical and cognitive functioning and as health care use and spending across settings. Minority elderly groups are over-represented in facilities and under-represented in alternative living settings.
INTRODUCTION
As the elderly population continues to grow, there is considerable policy and clinical interest in the population of elders with cognitive impairment and physical disability. This tends to be a high-cost, high-utilization group, often with multiple chronic conditions that require careful clinical management. Although nursing homes have traditionally been the default setting for this population, they are widely disliked and expensive: for example, in 2012, a semiprivate room cost an average of $81,000 a year(1). Consequently, a variety of nursing home alternatives has become increasingly available over time (consistent with state and federal policies encouraging this trend), including services in the home as well as in “supportive housing” options such as adult foster care, board and care, and assisted living. Thus it is important for medical professionals to appreciate the range of populations living in these different residential settings, and differences in their service use and other characteristics.
Although the growth of residential alternatives to nursing homes as options for elderly people who are not able to live independently has been dramatic, our understanding of this shift and its consequences is incomplete (2). Some sense of this shift can be derived from looking at the Medicaid program, where states have sought to ‘rebalance’ their Medicaid programs away from nursing homes toward home- and community-based options, which grew from 2.1 million participants in 2000 to 3.2 million in 2010 (3). Our understanding of this population is good, due to readily available Medicaid data. However, data on non-Medicaid elderly people are scarce, resulting in a lack of nationally representative research on their health status and health use. In particular, there are indications that those who can afford it are increasingly living in assisted living settings in preference to nursing homes. Thus, it is important to understand more about the populations residing in such settings and the extent to which they overlap the populations living at home or in nursing homes. Most previous studies have examined only one or two settings (e.g., community dwelling, assisted living or facility only) (4–8) been focused on a single state (5), fail to distinguish among residential settings (9), or rely on relatively limited data (10, 11). Others have focused on residential settings that meet particular regulatory requirements (8). This study uses the Medicare Current Beneficiary Study to provide a national, longitudinal analysis of health status and health care use among the elderly, making comparisons across different living arrangements. The dataset enables us to provide information on healthcare utilization unavailable from other sources, combined with detailed information about health status and functional ability.
METHODS
The data for this pooled cross-sectional study are from the 2002 to 2010 Medicare Current Beneficiary Study (MCBS) Cost and Use files. The MCBS is a nationally representative rotating-panel survey of aged, disabled, and institutionalized Medicare beneficiaries sponsored by the Center for Medicare and Medicaid Services (CMS), which provides a detailed description of the data collection methodology (12). The stratified, three-stage area probability sample represents the Medicare population as a whole and within age groups and contains interview data that are linked to Medicare claims files. Each participant is followed for up to four years; however the cost and use files omit data from the first year of participation. Each fall, community-dwelling Medicare beneficiaries are interviewed in their homes about their health status and health care experiences (referred to as a “community” interview). Medicare beneficiaries living in institutional setting at the time of the fall interview, however, do not have an in-person interview: a separate ‘facility’ interview is conducted with a representative of their place of residence. Although the survey instrument parallels the in-person interview, responses are drawn from the beneficiary’s medical record and the representative’s assessment. Our analytic sample included all beneficiaries aged 65 years or older who participated in the fall interview and were alive for the full year (n=83,507). For analysis of medical expenditures, we excluded beneficiaries in Medicare Advantage plans because their Medicare claims data are not complete. Overall response rates range from 69.5% to 71.4%. This study was approved by the University of Pittsburgh Institutional Review Board.
Study Variables
Housing Type
We grouped individuals into three types of housing based on how they described their place of residence at the time of the fall interview: Community, Community Plus Services, or Facility. We defined the community plus services setting broadly to distinguish between people living in their own homes from those living in places that have formal arrangements in place to provide long-term services and supports. Data from both the ‘community’ and ‘facility’ interviews were used to group people into these categories, using two interview items: whether or not they received personal care (in the community interview) and facility description (in the facility interview). First, respondents in the community interview who described their housing as a retirement community, senior citizens housing, assisted living, continuing care community, stages living community, retirement apartment, church-provided housing, or a personal care home, were asked if the place where they lived had any of the following personal care services available: personal care, prepared meals, cleaning, laundry, medication assistance, transportation, or recreation. These individuals were considered to be living in ‘Community Plus Services.’ All other respondents living in the community were classified as “Community”. Second, respondents in the facility interview were asked to describe the facility where they lived. Respondents living in places described as assisted living, board and care, personal care home, domiciliary care, rest home, adult or group home or a retirement community, were considered ‘Community Plus Services.’ Finally, people living in a nursing home, rehabilitation facility, hospital, or mental health/mental retardation facility were considered to be living in a facility.
Physical and Cognitive Function
As a measure of physical function, we constructed a count of basic and instrumental activities of daily living (ADL, IADL) where the beneficiary received assistance or supervision. Measurement of ADL tasks was identical in the community and facility interviews, which used walking, dressing, toileting, eating and bathing. Respondents could have 0–5 ADL needs. However, the only IADL items collected in common across the two types of interviews were using the telephone, paying bills and making purchases; the range for this item was 0–3. Mobility difficulty was defined as difficulty stooping or kneeling, lifting, reaching, grasping or writing, or walking a quarter mile; respondents were ranked on a 0–5 scale for each item, where 1 represents no difficulty and 5 represents unable to perform the task. The variable used in the analysis was the average of these scores across all items. To address cognitive function, we summed three items that were measured for both samples: memory loss, trouble making decisions, or a diagnosis of Alzheimer’s disease or other dementia. Although this cognitive impairment score could theoretically range from 0–3, preliminary analysis found that there were no nursing home residents with both high levels of cognitive impairment and no IADL limitations. Thus, to avoid confounding the IADL and cognitive impairment variables, we restricted the range of the cognitive impairment score to 0–2.
Socio-Demographics
Respondent age is reported in years and converted to z-score for multivariate analysis. As measures of poverty and access to care, we include indicators for any Medicaid enrollment throughout the year and annual income lower than $25,000. Educational attainment was coded as a dichotomous variable where 1 = high school completion or greater. In addition, we include an indicator for living in a metropolitan statistical area (MSA). Race and ethnicity was coded as Non-Hispanic white, Non-Hispanic African American, Hispanic, Asian or Pacific Islander, and Other (including American Indian, multiple races).
Health Status
For ease of interpretation, we dichotomized the single item measure of health related quality of life (“How would you rate your health compared to others your age?”) as ‘excellent or very good’ versus ‘good, fair or poor.’ Each year of the MCBS survey, subjects are asked if they had been told by a physician that they had any chronic diseases using a list of options. We calculated the count of 13 diseases that were collected consistently for all study years in both the community and facility interviews: high blood pressure, myocardial infarction, coronary heart disease, stroke, skin cancer, other forms of cancer, diabetes, rheumatoid arthritis, osteoarthritis, osteoporosis, hip fracture, Parkinson disease, emphysema/chronic obstructive pulmonary disease. The existence of these disease conditions was assessed by single item question “ Have you ever told that you had (name of the condition)?” The count variable was top-coded at four chronic diseases since the frequency in each category gets sparse at higher levels.
Medical Use and Expenditures
This analysis is restricted to beneficiaries enrolled in fee-for-service Medicare for the full year, because medical care use and cost data available in the MCBS are incomplete for individuals covered by managed care plans (Medicare Advantage), which are not required to submit claims to CMS. For fee-for-service enrollees, we examined total annual medical care expenditures from all payment sources (e.g., Medicare, Medicaid, Veterans Affairs, and private plans), and separately for out of pocket spending. We constructed an indicator for having had no physician visits during the course of a year. Likewise, we constructed an indicator for having had one or more emergency room visits. To measure adequacy of preventive care, we constructed an indicator for whether the individual had a flu shot during the most recent flu season. Finally, we examined the number of inpatient stays and total inpatient days (per year).
Analysis
We report descriptive and bivariate statistics that are weighted to represent the population of aged Medicare beneficiaries alive for the entire year. Data from years 2002 to 2010 were combined to create a pooled cross-sectional analysis. As noted above, the same individuals can appear in up to 3 consecutive years of the MCBS Cost and Use files. This study treated each year of data as a separate cross-sectional analysis, weighted to represent the population of Medicare beneficiaries that year. Thus we did not need to adjust for correlations due to repeated observations.
Estimates of total health care expenditures, hospitalization and emergency room use were calculated using weighted regression and logistic regression models to adjust for age, gender, and year. To facilitate comparisons across settings, expenditures and use in each setting were computed at the means of the covariates for the entire population. All analyses were conducted using Stata SE 13.1. (13)
RESULTS
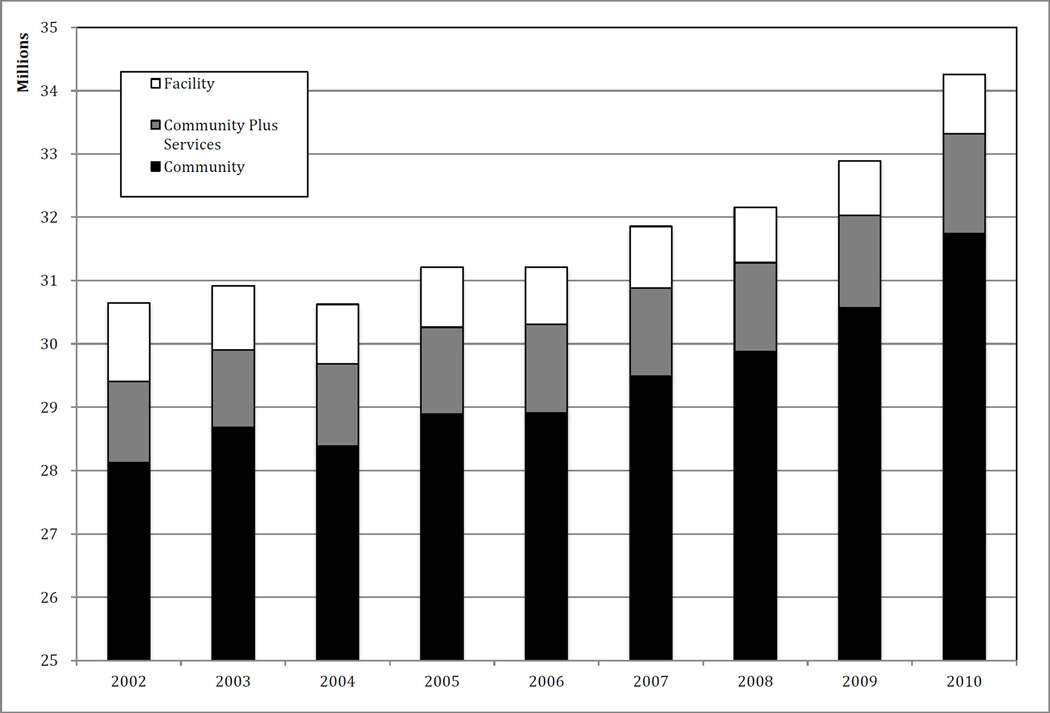
Figure 1 shows the growth in community-based alternatives to institutional care from 2002 through 2010, and illustrates the shift that has taken place over this time period. Although the overall proportion of older people living in community plus services settings increased modestly, from about 4.17% to 4.61%, the proportion living in nursing homes decreased considerably, from 4.06% to 2.74%. Overall, despite an increase of roughly 3.6 million in the elderly population over this time period, the number of nursing home residents declined by about 300,000. The community plus services group has expanded considerably.
Figure 1.
Population of Elderly Medicare Beneficiaries by Type of Housing (2002 to 2010).
In Table 1, differences among populations in the different settings are shown. Facility residents are consistently found to be older, whiter, and poorer than those in other settings; they are also much more likely to be enrolled in Medicaid, with 73% of the nursing home residents enrolled, compared to 22% of the community plus services group and only 12% of the community only group. The community plus services group was the most likely to be white -- 89% of residents, compared to the 81% average in other settings. Indicators of health and functional status showed that nursing home residents are more impaired than those in other settings: they are also significantly more likely to have high levels of ADL and IADL needs, to not be cognitively intact, to have higher mobility needs, and are less likely to have excellent self-rated health: only 10% of institutional residents rated their health as excellent, while 38% of the community plus services group and nearly half (47%) of community residents did. However, nursing home residents were less likely to have multiple co-morbidities than those in other settings were. Those living in the community and the community plus services group had similar patterns of comorbidity, with over half having three or more chronic conditions, compared to about a third of the nursing home residents.
Table 1.
Demographics and Health Status of the Elderly Medicare Beneficiaries by Type of Housing (2002 to 2010)
| All | Community | Community Plus Services |
Facility | |
|---|---|---|---|---|
| (n = 78,542) | (n = 70,957) | (n = 3,946) | (n = 3,639) | |
| sAge | 76.4 | 75.9 | 82.0 | 84.1 |
| Gender (female) | 58% | 56% | 71% | 73% |
| Race | ||||
| non-Hispanic White | 81% | 80% | 89% | 82% |
| non-Hispanic Black | 8% | 8% | 6% | 11% |
| Hispanic | 7% | 8% | 3% | 5% |
| Asian/Pacific Islander | 2% | 2% | 1% | 1% |
| Other | 2% | 2% | 1% | 1% |
| Low Income (<=25,000) | 53% | 51% | 61% | 85% |
| Medicaid | 15% | 12% | 22% | 73% |
| ADL | ||||
| None | 87% | 90% | 74% | 12% |
| One | 5% | 4% | 10% | 9% |
| Two | 2% | 2% | 5% | 7% |
| Three | 2% | 2% | 5% | 15% |
| Four | 2% | 2% | 4% | 26% |
| Five | 2% | 1% | 3% | 32% |
| IADL | ||||
| None | 80% | 83% | 59% | 9% |
| One | 10% | 10% | 16% | 6% |
| Two | 5% | 4% | 12% | 21% |
| Three | 5% | 3% | 13% | 64% |
| Mobility Difficulty | 2.01 | 1.93 | 2.41 | 3.73 |
| Excellent Self-Rated Health | 8% | 7% | 19% | 45% |
| Cognitively Intact | 84% | 87% | 65% | 11% |
| Comorbidities (>=4) | ||||
| None | 7% | 7% | 9% | 16% |
| One | 16% | 16% | 16% | 25% |
| Two | 24% | 24% | 21% | 26% |
| Three | 23% | 23% | 22% | 18% |
| Four or More | 30% | 30% | 32% | 15% |
Notes: Sample n = 83,507; weighted sample represents a population of approximately 28.6 million elderly Medicare beneficiaries pa.
ADL = Activities of Daily Living (bathing, dressing, toileting, walking, eating). IADL = Instrumental Activities of Daily Living (telephoning, shopping, paying bills).
Cognitively intact means no problems with memory, decision making, and no diagnosis of Alzheimer's Disease or other dementia. Mobility difficulty measured from 0 to 5 where 0 is no difficulty and 5 is unable to perform bending, reaching, grasping, stooping, or walking.
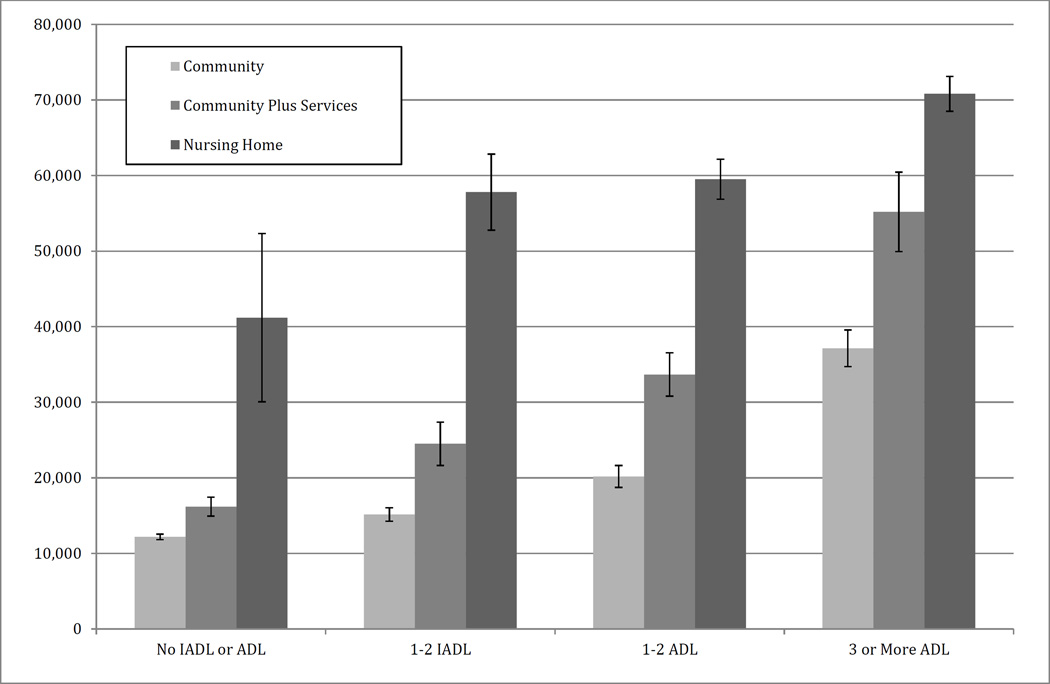
Health care utilization and costs also differed significantly among the three settings. Those in the community plus services group had nearly twice the medical expenditures that the community residents had – $24,075, compared to $12,646 – while the nursing home residents had vastly higher expenditures at $64,722. These cost figures are consistent with the more intensive pattern of utilization seen among the nursing home residents compared to the community plus services group, and the community plus services group relative to the community group: nursing home residents had 603 hospitalizations per thousand, while the CPS group had 464 per thousand, and the community group had 319. Hospital days and emergency room visits followed a similar pattern.
DISCUSSION
Over the period from 2002 to 2010, the elderly Medicare population grew by an estimated 11.8%. During this time, the number and percentage living in facilities declined while the population living in community settings that provide personal care services increased. As would be expected, there is a gradient in health status and function across the three settings, with facilities serving those in the poorest health and the most disabled and community plus services being intermediate. It is noteworthy that there is also a socio-economic gradient, with facilities serving the most poor, as well as the highest proportion of non-Hispanic African Americans. However, there is a dramatic racial and ethnic disparity in use of community plus services, with only 11% from minority groups compared to 18% - 20% in community and facility settings. These findings may be reflective of economic injustice and of health disparities: Greater proportion of minority older adults, especially non-Hispanic African Americans and Hispanic older adults, are poor and unable to “age in place” due to the greater clinical and functional disabilities.
There are substantial differences in health care expenditures across housing type, adjusting for age and gender. People living in community plus services type settings have 1.9 times higher average expenditures than people living in the community, while those in facilities generate 5.1 times as much spending. It should be noted, however, that health care expenditures for nursing home residents covered by Medicaid (73% of all facility residents in this study) include the cost of the accommodations as well as medical care, whereas such expenses are not included for people living in other settings. Notwithstanding this issue, the gradient exists with regard to hospitalization rate, hospital days and emergency room use.
Our findings are consistent with recent reports by the US Census and others (65+ in the United States: 2010). The Census found that from 2000 to 2010, the number and proportion of elderly living in facilities declined while the overall population of elderly grew. Feng et al. found comparable rates of emergency department use in community dwelling elderly and nursing home residents with dementia from 2000 to 2008; however they did not separately analyze people living in assisted living or other community plus services settings (14). Caffrey (8) reported similar rates of Medicaid use among people living in community plus services settings. Their estimate of the number of people living in state licensed residential care facilities (RCF) is lower than ours, likely due to our use of a broader definition of such settings. Similarly, we used a more inclusive definition of community plus services than Spillman et al. (15) and Mollica (16), leading to a higher estimate of the proportion of elderly living in these settings.
This study has several important implications. First, policy makers and health care providers should be alert to the high level of health care utilization among elderly living in community plus services settings. This is a growing segment of the elderly population with substantial levels of physical and cognitive disability, as well as acute needs. Further research is needed to examine the factors associated with hospitalization and other medical care in this population, and whether appropriate care – in particular, sufficient preventive care, post-acute care, and chronic disease management -- is being provided in these comparatively unregulated settings. These settings, which range from senior apartment buildings to continuing care retirement communities, staffed in varying degrees of the medical sophistication. High levels of cognitive impairment among residents raise particular concerns regarding the ability of providers to adequately care for this challenging population.
Several limitations should be noted. First, our estimate of the size of the elderly population is slightly lower than the 2010 US Census. This is likely due to the exclusion of people who die during each year. The MCBS collects health status data during the fall interview. Thus people who were not alive throughout the entire year were not included in this component of the data collection. In addition, the MCBS sample does not represent people who are not eligible for Medicare. People who become eligible during a calendar may be included in the MCBS, but are not interviewed during the year of partial eligibility and hence were not included in this study. This may also underestimate the overall proportion of older adults living in non-community settings. Second, the lower comorbidity rate among facility residents is likely due to the way nursing facilities are paid under state Medicaid and Medicare case-mix adjustment programs, which are based on physical function and rehabilitation potential, rather than on residents’ medical conditions (17). This payment method reduces incentives to thoroughly document diagnoses, compared to hospital settings. In addition, Alzheimer’s Disease and other dementias are highly prevalent but not included among the conditions counted in the comorbidity variable (these parameters were included in the “cognitively intact” item). Finally, the MCBS does not consistently capture use of or spending on supportive services, such as personal care, that are not covered by Medicare. Thus, we were unable to identify whether individuals in the community or community plus services settings receive, such as personal care, receive such services (e.g., through Medicaid home and community based services waivers, state financed programs or out of pocket).
CONCLUSION
Over the last decade or so, changes in policy and individual preference have resulted in a shift away from nursing homes among older people with a need for supportive services. This study shows the extent of this shift in the elderly Medicare population, and highlights the range of alternative residential settings that have evolved to serve them, as well the health and functional status of those who live in these settings. The well-establish status of the nursing home within our medical system means that medical professionals are well aware of the population that lives there and their medical needs. However, the nursing home population has changed: it has become smaller (both in number and proportion), sicker, and poorer, compared to other elderly people with support needs. Moreover, individuals who previously received care in a nursing home may now be living in an alternative residential setting. Ensuring the ongoing, quality care for these at-risk populations is becoming ever more complex yet essential.
Figure 2.
Adjusted Annual Expenditures by Type of Housing and Physical Function
Table 2.
Average Annual Health Care Use and Expenditures by Housing Type (2002 to 2010)
| Community | Community Plus Services | Facility | ||||
|---|---|---|---|---|---|---|
| Adj. Mean |
CI | Adj. Mean |
95% CI | Adj. Mean |
95% CI | |
| Total Expenditures | 12645.90 | (12352.38, 12352.38) | 24074.77 | (22366.71, 22366.71) | 64722.03 | (62916.99, 62916.99) |
| Hospitalizations (per 1000) | 319.18 | (308.43, 308.43) | 464.2466 | (418.26, 418.26) | 603.3525 | (545.57, 545.57) |
| Hospital Days | 1.66 | (1.58, 1.58) | 2.56 | (2.24, 2.24) | 3.94 | (3.48, 3.48) |
| Percent with Any Emergency Room Visit | 0.27 | (0.26, 0.26) | 0.40 | (0.38, 0.38) | 0.46 | (0.44, 0.44) |
| Number of Emergency Room Visits | 1.17 | (1.1, 1.1) | 1.79 | (1.56, 1.56) | 2.70 | (2.39, 2.39) |
Notes: Estimates are population means, adjusted for age, gender and year. Total Expenditures includes inpatient, outpatient, skilled nursing facility, home health care, hospice, durable medical equipment, professional services (i.e., physician visits), and medication.
REFERENCES
- 1.Mature Market Institute. The 2012 MetLife Market Survey of Nursing Home, Assisted Living, Adult Day Services, and Home Care Costs. New York: 2012. [Google Scholar]
- 2.Wysocki A, Butler M, Kane R, Kane R, Shippee T, Sainfort F. Long-Term Care for Older Adults: A Review of Home and Community-Based Services versus Institutional Care. Rockville, MD: Agency for Healthcare Research and Quality; 2012. Contract No.: Report No.: 12(13)-EHC134-EF. [PubMed] [Google Scholar]
- 3.Ng T, Harrington C, Musumeci M, Reaves E. Medicaid Home and Community-Based Service Programs: 2010 Data Update. Washington, DC: Kaiser Family Foundation; 2014. [March 27, 2014]. Report No. [Google Scholar]
- 4.Zimmerman S, Sloane PD, Reed D. Dementia prevalence and care in assisted living. Health Aff (Millwood) 2014 Apr;33(4):658–666. doi: 10.1377/hlthaff.2013.1255. [DOI] [PubMed] [Google Scholar]
- 5.Frytak JR, Kane RA, Finch MD, Kane RL, Maude-Griffin R. Outcome trajectories for assisted living and nursing facility residents in Oregon. Health Serv Res. 2001 Apr;36(1 Pt 1):91–111. [PMC free article] [PubMed] [Google Scholar]
- 6.Amaral MM. Does substituting home care for institutional care lead to a reduction in Medicaid expenditures? Health care management science. 2010;13(4):319–333. doi: 10.1007/s10729-010-9132-9. [DOI] [PubMed] [Google Scholar]
- 7.Kane RL, Homyak P, Bershadsky B, Flood S, Zhang H. Patterns of utilization for the Minnesota senior health options program. J Am Geriatr Soc. 2004 Dec;52(12):2039–2044. doi: 10.1111/j.1532-5415.2004.52558.x. [DOI] [PubMed] [Google Scholar]
- 8.Caffrey C, Sengupta M, Park-Lee E, Moss A, Rosenoff E, Harris-Kojetin L. Residents Living in Residential Care Facilities: United States, 2010. Washington, DC: 2012. [April 2012]. Report No.: Contract No.: 91. [PubMed] [Google Scholar]
- 9.Jacobson G, Neuman T, D'amico A. Medicare Spending and Use of Medical Services for Beneficiaries in Nursing Homes and Other Long-Term Care Facilities. Washington, DC: Kaiser Family Foundation; 2010. [September 30, 2010]. Report No. [Google Scholar]
- 10.Harris-Kojetin L, Sengupta M, Park-Lee E, Valverde R. Long-term care services in the United States: 2013 Overview. Hyattsville, MD: National Center for Health Statistics; 2013. [PubMed] [Google Scholar]
- 11.The SCAN Foundation. Trends in the Residential Care Industry. Long Beach, CA: 2012. [October, 2012]. Report No.: Contract No.: 32. [Google Scholar]
- 12.Centers for Medicare and Medicaid Services. [cited 2014 July 21, 2014];Medicare Current Beneficiary Survey (MCBS) 2014 Available from: http://www.cms.gov/Research-Statistics-Data-and-Systems/Files-for-Order/LimitedDataSets/MCBS.html.
- 13.Stata. Stata [Computer Program] 13.1 ed. College Station: Stata Corp; 2013. [Google Scholar]
- 14.Feng Z, Coots LA, Kaganova Y, Wiener JM. Hospital and ED use among medicare beneficiaries with dementia varies by setting and proximity to death. Health Aff (Millwood) 2014 Apr;33(4):683–690. doi: 10.1377/hlthaff.2013.1179. [DOI] [PubMed] [Google Scholar]
- 15.Spillman B, Black K. The Size and Characteristics of the Residential Care Population: Evidence from Three National Surveys. Washington, DC: Department of Health and Human Services; 2006. [Google Scholar]
- 16.Mollica R, Houser A, Ujvari K. Assisted Living and Residential Care in the States in 2010. Washington, DC: AARP Public Policy Institute; [Google Scholar]
- 17.Feng Z, Grabowski DC, Intrator O, Mor V. The effect of state medicaid case-mix payment on nursing home resident acuity. Health Serv Res. 2006 Aug;41(4 Pt 1):1317–1336. doi: 10.1111/j.1475-6773.2006.00545.x. [DOI] [PMC free article] [PubMed] [Google Scholar]