Abstract
Why do some hamstring and quadriceps strains take much longer to repair than others? Which injuries are more prone to recurrence? Intramuscular tendon injuries have received little attention as an element in ‘muscle strain’. In thigh muscles, such as rectus femoris and biceps femoris, the attached tendon extends for a significant distance within the muscle belly. While the pathology of most muscle injures occurs at a musculotendinous junction, at first glance the athlete appears to report pain within a muscle belly. In addition to the musculotendinous injury being a site of pathology, the intramuscular tendon itself is occasionally injured. These injuries have a variety of appearances on MRIs. There is some evidence that these injuries require a prolonged rehabilitation time and may have higher recurrence rates. Therefore, it is important to recognise the tendon component of a thigh ‘muscle strain’.
Keywords: Muscle, Hamstring, Injuries, Quadriceps
Introduction
The traditional view of the muscle tendon unit involved a distinct delineation between the muscle belly and the tendon(s) at one or both ends of the muscle leading to its bony attachment. The musculotendinous junction has been described as the most common site of muscle injury,1 yet both clinically and radiologically, it is clear that the majority of muscle injuries occur within the muscle belly.
Improved resolution via MRI and excellent anatomical dissection studies provide evidence that in many muscles, the tendon extends within the muscle belly, and these muscle belly injuries occur at an intramuscular myotendinous or myoaponeurotic junction. The intramuscular tendon (rachis or aponeurosis) acts as a central supporting strut to which the muscle fibres attach.
Failure of the myofibrillar attachments may occur along the intramuscular tendon (or aponeurosis). This is analogous to the failure of struts along a suspension bridge.
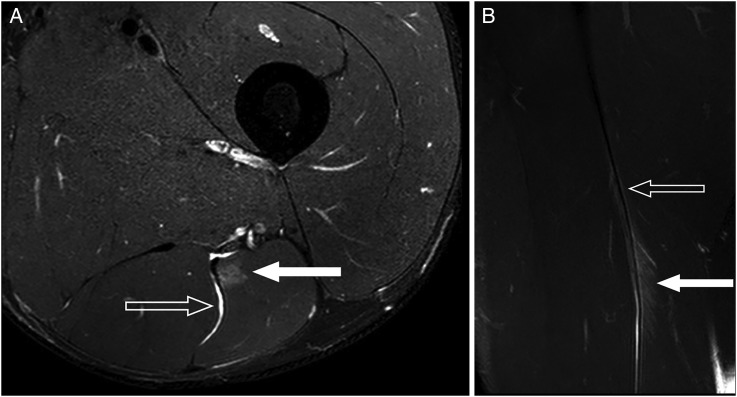
This failure often occurs in a zipper-like fashion with oedema and blood products tracking alongside the torn muscle fibres. The effect is a characteristic feather-like appearance on MRI (figure 1A,B) and ultrasound scans. Recently, injuries to the intramuscular tendon itself, often in association with a musculotendinous injury, have been identified.
Figure 1.
MRI appearance of injury at muscle-tendon junction of the intramuscular tendon showing characteristic feather-like appearance. (A) Axial fat suppressed image demonstrates intact intramuscular tendon rachis but myofibrillar tearing at the interface with the tendon (solid arrow). Blood products track along the medial margin of biceps coming in contact with the sciatic nerve and separating semitendinosis (open arrow). (B) Coronal fat suppressed images demonstrate classic feather-shaped appearance caused by myofibril disruption with oedema and blood fluid products tracking between the torn muscle fibres (solid arrow). Note that the intramuscular tendon has preserved its linear low signal appearance (open arrow).
The aim of this narrative review is to examine the evidence to support our clinical experience that muscle injuries involving damage to the tendon itself are more serious than those affecting the myotendinous junction only.
Imaging appearance
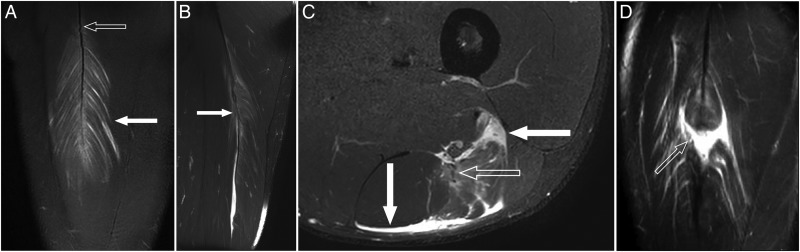
MRI of the disrupted intramuscular tendon demonstrates a wavy retracted appearance as opposed to the normal taut cord-like appearance (figure 2A). Sometimes, as the tendon fails, the tendon strands unravel and give way similar to a piece of intertwined rope. The tendon consequently loses its taut appearance, but there is no gap in the tendon, despite it losing its tensile strength (figure 2B). In some cases, there is longitudinal delamination and splitting of the intramuscular tendon (figure 2C), which otherwise appears continuous. In other cases, the tendon may retract and create a gap (figure 2D).
Figure 2.
Tendon failure. (A) Coronal fat suppressed image of a 23-year-old footballer with sudden onset of anterior thigh pain when sprinting for the ball, demonstrates myofibril tearing (solid arrow) on either side of the intramuscular tendon rachis of the rectus femoris to create a feather-like appearance. The intramuscular tendon is intact but has a wavy contour (open arrow) suggesting the rachis has begun to fail.(B) Coronal fat-saturated sequence of a 19-year-old footballer with sudden hamstring failure when running, demonstrates failure of the proximal intramuscular tendon rachis (arrow) with tendon strands unravelling. However, given that the tendon remained broadly contiguous (with no tendon gap), the athlete was treated in a conservative manner with return to competition 6 weeks later. (C) Axial fat-suppressed image demonstrates longitudinal delamination and splitting of the biceps femoris intramuscular tendon (open arrow). However, no gap is seen. Note haemorrhage surrounding the muscle (solid arrows).(D) A 29-year-old footballer with a history of a rectus femoris strain returns to competition only to sustain another injury. On examination, there is a palpable defect in the anterior thigh at the junction of the middle and distal thirds of the thigh. Coronal fat suppressed image demonstrates failure of the intramuscular tendon rachis of rectus femoris with tendon retraction filled with blood products to create a ‘bull's eye’ or ‘target’ lesion (arrow). Note the torn adjacent muscle fibres with no connective scaffold to hang on to. The defect will take some time for granulation tissue to fill, and indeed may never completely do so, leaving the athlete with a residual defect.
The role of intramuscular tendon tears
Two examples of the important role these intramuscular tendons play are in the hamstring and quadriceps muscles.
Hamstring muscle injuries
Hamstring injuries are a major cause of time loss injuries in sport and particularly in the various football codes.2 The anatomical issues highlighted in this paper may contribute to the inconsistent outcomes of hamstring injury management.
Garrett et al3 observed in a CT study that the proximal biceps femoris tendon and its muscle-tendon junction extend 60% of the muscle length, while the distal tendon and its muscle-tendon junction extend 66% of the muscle length. Thus, the regions of muscle-tendon junction extend the full length of the muscle belly on either the proximal or distal portion (figure 3).
Figure 3.
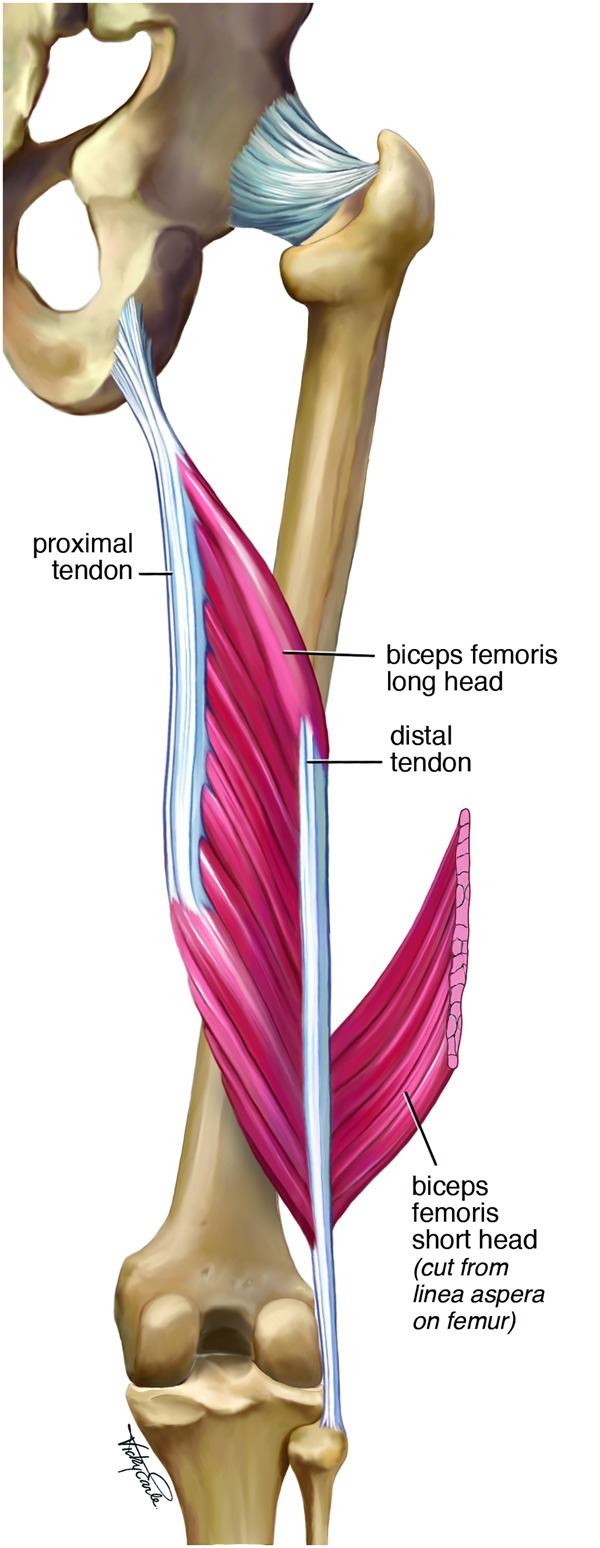
Proximal and distal tendons extending into the muscle belly of biceps femoris.
Similarly in the semimembranosus muscle, the proximal tendon extended 78% and the distal 52% into the muscle.3 4
A number of MRI studies5–7 confirmed that the majority of hamstring muscle injuries occurred at the myotendinous junction of the intramuscular tendon and described the characteristic appearance on MRI of a feather-like pattern of oedema shown previously in figures 1 and 2.
Comin et al8 noted that the appearance of the central tendon in these injuries is variable. On some occasions, the tendon maintains its structural integrity despite disruption of surrounding muscle fibres, whereas in other cases this integrity appears to be lost and the tendon takes on an irregular or wavy contour, or is frankly disrupted.
They then reviewed 62 hamstring injuries among elite Australian Rules footballers. Of the 62 injuries, 45 (72%) involved the biceps femoris, and of these 45, 12 (27%) had intramuscular tendon disruption on MRI.
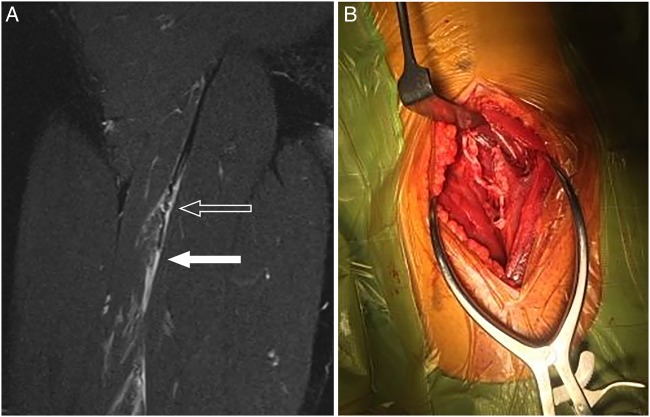
Three of the 12 participants with biceps femoris intramuscular tendon injuries had surgery to repair the disrupted tendon. The median recovery time of these three patients, including postsurgical recovery, was 91 days (IQR 84–91). These cases were excluded from further analysis. An example of a case which required surgery is shown in figure 4A, B.
Figure 4.
Longitudinal tear in the intramuscular biceps femoris tendon. (A) MRI. The open arrow demonstrates a wavy appearance of the intramuscular tendon of biceps femoris in the proximal third of the thigh, while the closed arrow show a fluid-filled defect created by rupture and retraction of the tendon. Oedema and blood fluid products also dissect along the torn myofibrils. (B) Intraoperative appearance showing the tear in the tendon.
The remaining nine biceps femoris injuries with tendon disruption treated non-operatively had a mean recovery time of 72 days. In comparison, the biceps femoris injuries without intramuscular tendon disruption had a recovery time of 21 days.
In a prospective study of 18 elite sprinters with hamstring muscle injures by Askling et al,9 the subgroup in which the injury involved the proximal tendon (n=6) had a significantly (p=0.009) longer time back to preinjury level (mean: 34.8, range 16–49) compared with the subgroup with no proximal tendon involvement (n=12, mean:13.0, range 6–26).
Pollock et al10 reviewed 65 hamstring injuries in 44 elite track and field athletes. They classified the injuries according to the British Athletics Muscle Injury Classification System11 in which injuries are graded numerically by severity (1=small, 2=moderate, 3=extensive) and alphabetically by site (a=myofascial, b=myotendinous, c=intratendinous). The study compared time to return to full training and recurrence rates between the different types of injury.
The study demonstrated that injuries that extend into the tendon were associated with a substantial increased risk of recurrence of injury and an increased time to return to full training.
There was a significant difference within classifications 1a–3c for time to return to full training. Separate linear regression analysis of grade and site demonstrated that grade 3 severity (p<0.001) and intratendinous (c) site (p=0.008) were associated with an increase in the time to return to full training. Grade 3c injuries (N=7) had a mean return time of 84 days (SD 49.4, range 40–128) compared with grade 2b injuries (N=17) with return time of 21 days (SD 10.2, range 12–49) and 2c injuries (N=8) of 27 days (SD 49.4, range 40–128). No significant differences were found between grades 1 and 2 (t=−1.138, p=0.263) or between classifications (a) and (b) (t=−0.240, p=0.812).
There was also a significant difference within classifications 1a–3c with respect to injury recurrence. Separate binary logistic analysis of grade and site suggested that grade was not associated with recurrence (p=0.133–0.968), but that intratendon injuries (c) were associated with a higher risk of recurrence (p=0.002). This significantly increased repeat injury rate was 63% in 2c injuries and 57% in 3c injuries. In comparison, the repeat injury rate in 2b injuries was only 6% (p<0.001) and there were no recurrences in any myofascial (a) injury class.
Prolonged recovery time and higher rate of injury recurrence both have enormous clinical implications especially for the elite athlete. There is a vigorous debate about the utility of MRI in hamstring strain.12 In this clinical setting, we argue that high-quality MRI is indicated to identify possible tendon disruption that accompany biceps femoris injuries. A positive diagnosis would influence management.
Quadriceps muscle injuries
Hasselman et al13 described the appearance of the rectus femoris muscle at cadaveric dissection. The proximal tendon of the rectus femoris muscle has two components (superficial and deep) rather than being a single, superficial tendon as previously described. The tendon of the straight head arises from the anterior inferior iliac spine and forms the superficial anterior tendon that covers the ventral aspect of the proximal third of the muscle length.
The tendon of the indirect head arises from the superior acetabular ridge and travels deep to the tendon of the straight head. It is initially rounded and lies in the most medial aspect of the muscle; however, as it progresses along the muscle, it flattens out, rotates laterally, and migrates to the middle of the muscle belly. In the distal third of the muscle, the deep tendon of the indirect head is flat, twisted 90° to a nearly vertical position, and lies intramuscularly in the anterior aspect of the distal muscle belly.
The ‘bulls eye’ and intrasubstance tendon tear
Hughes et al14 described a series of intrasubstance quadriceps strain injuries resulting from a tear of those fibres originating on the tendon of the indirect head of the muscle. They hypothesised that the strain injury that occurs in the mid-muscle belly involves disruption of the muscle fibres at the deep myotendinous junction of the indirect head with distal retraction of these fibres.
They described the typical MRI appearance of this injury as a ‘bulls eye’ appearance which refers to an injury associated with enhancement of signal about the central tendon on T1-weighted scans after intravenous gadolinium.
Cross et al15 examined the clinical and MRI appearance of 25 quadriceps injuries of which 15 were rectus femoris injuries. Seven of the 15 rectus femoris injuries involved the central (intramuscular) tendon. They described a typical MRI appearance (figure 2D) showing a feather-like pattern of injury in the coronal T2 view.
The clinical importance of this intramuscular tendon involvement is shown by the prolonged rehabilitation time in this group (27 days) compared with the remainder of the rectus femoris injuries (9 days).
Balius et al16 published a ultrasound study of 35 cases of rectus femoris injuries involving the central tendon (aponeurosis). The injuries involving the tendon had longer time to return to play (RTP) than the 13 peripheral rectus femoris injuries (15 days) in their cohort. Most of the distal central tendon injuries were grade I (14) or II (20) with only one complete tendon tear. The average RTP for grade I injuries was 28 days and the grade II injuries 46 days. These injuries were equally distributed between proximal and distal, with the proximal injuries having a longer time to RTP (49 vs 32 days).
Tears involving the intramuscular tendon of rectus femoris follow a similar pattern to those of biceps femoris, although these typically involve a kicking rather than running mechanism of injury. Some tears involving the intramuscular tendon result in disruption of the myofibrils from the central tendon to create the feather-like appearance, but the central tendon retains its integrity.
This central tendon can also fail and retract to create a fluid-filled defect. It is common for the myofibril attachments to initially fail, but for the central tendon to remain in continuity. There is a resultant increase in stress load transferred to the intramuscular tendon which leads to injury.
Our clinical experience indicates that athletes with this injury typically appear to recover quite quickly and RTP, only to sustain a reinjury, this time with failure of the intramuscular tendon.
Hughes et al14 postulated that the indirect (central tendon) and direct heads of the proximal tendon begin to act independently, creating a shearing phenomenon in contrast to what occurs in the normal rectus femoris. This hypothesis was then used15 as a potential explanation for the longer rehabilitation associated with acute injuries involving the central (intramuscular) tendon.
Summary
A number of thigh muscles including the biceps femoris and rectus femoris have significant intramuscular tendons. These tendons are a common site of myotendinous muscle strains.
There is some research evidence to support our clinical experience that injuries involving significant intramuscular tendon injury require prolonged rehabilitation time and may be more prone to recurrence. Therefore, it is important that they are recognised early, especially in the elite athlete. Injuries involving the intramuscular tendon can best be identified on MRI.
At present, optimal management of these injuries that involve a significant tear of the intramuscular tendon is unclear. There may be a role for surgical repair, and this warrants further investigation specifically addressing RTP and reinjury rates in comparison to conservative care.
Conclusion
Thigh muscle injuries involving significant injury to the intramuscular tendon may be associated with prolonged RTP times and an increased incidence of recurrence.
Future research should aim at better understanding the involvement of the intramuscular tendon in muscle injuries, and investigating appropriate treatment interventions for this particular group of muscle injuries.
What are the findings?
Injuries involving the quadriceps or hamstring intramuscular tendon have prolonged rehabilitation and return to play times—they must be treated differently to ‘muscle strains’.
Differentiation of these intramuscular tendon injuries seems particularly important in injuries to the biceps femoris and rectus femoris muscles.
If injury to these tendons is suspected, MRI is indicated for accurate diagnosis and athlete/player and coach/agent education.
There may be a role for surgical repair of the tendon in injuries with significant damage of the intramuscular tendon.
How might it impact on clinical practice in the future?
Improved recognition of injury of the intramuscular tendon may allow more accurate prediction of time to return to sport and thus, reduce risk of recurrence. This needs to be investigated further.
The role of surgical repair versus conservative management in some of these injuries is not clear. The options need to be weighed carefully and discussed appropriately (shared decision-making) until more data provide a basis for clear recommendations.
Footnotes
Contributors: PB wrote the original draft of the manuscript. DC provided the images and reviewed the manuscript.
Competing interests: PB is the co-author of the textbook ‘Brukner & Khan's Clinical Sports Medicine’ and receives royalties from the publisher McGraw-Hill. He is currently Australian cricket team doctor.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Garrett WE. Muscle strain injuries. Am J Sports Med 1996;24(6 Suppl):S2–8. [PubMed] [Google Scholar]
- 2.Brukner P. Hamstring injuries: prevention and treatment—an update. Br J Sports Med 2015;49:1241–4. 10.1136/bjsports-2014-094427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garrett WE Jr, Rich FR, Nikolaou PK, et al. . Computed tomography of hamstring muscle strains. Med Sci Sports Exerc 1989;21:506–14. 10.1249/00005768-198910000-00004 [DOI] [PubMed] [Google Scholar]
- 4.Woodley SJ, Mercer S. Hamstring muscles: architecture and innervation. Cells Tissues Organs (Print) 2005;179:125–41. 10.1159/000085004 [DOI] [PubMed] [Google Scholar]
- 5.Connell DA, Schneider-Kolsky ME, Hoving JL, et al. . Longitudinal study comparing sonographic and MRI assessments of acute and healing hamstring injuries. AJR Am J Roentgenol 2004;183:975–84. 10.2214/ajr.183.4.1830975 [DOI] [PubMed] [Google Scholar]
- 6.De Smet AA, Best TM. MR imaging of the distribution and location of acute hamstring injuries in athletes. AJR Am J Roentgenol 2000;174:393–9. 10.2214/ajr.174.2.1740393 [DOI] [PubMed] [Google Scholar]
- 7.Slavotinek JP, Verrall GM, Fon GT. Hamstring injury in athletes: using MR imaging measurements to compare extent of muscle injury with amount of time lost from competition. AJR Am J Roentgenol 2002;179:1621–8. 10.2214/ajr.179.6.1791621 [DOI] [PubMed] [Google Scholar]
- 8.Comin J, Malliaras P, Baquie P, et al. . Return to competitive play after hamstring injuries involving disruption of the central tendon. Am J Sports Med 2013;41:111–15. 10.1177/0363546512463679 [DOI] [PubMed] [Google Scholar]
- 9.Askling CM, Tengvar M, Saartok T, et al. . Acute first-time hamstring strains during high-speed running: a longitudinal study including clinical and magnetic resonance imaging findings. Am J Sports Med 2007;35:197–206. 10.1177/0363546506294679 [DOI] [PubMed] [Google Scholar]
- 10.Pollock N, Patel A, Chakraverty J, et al. . Time to return to full training is delayed and recurrence rate is higher in intratendinous (‘c’) acute hamstring injury in elite track and field athletes: clinical application of the British Athletics Muscle Injury Classification. Br J Sports Med 2015; ▪▪▪. Published Online First: July 17, 2015 10.1136/bjsports-2015-094657 [DOI] [PubMed] [Google Scholar]
- 11.Pollock N, James SLJ, Lee JC, et al. . British Athletics muscle injury classification: a new grading system. Br J Sports Med 2014;48:1347–51. 10.1136/bjsports-2013-093302 [DOI] [PubMed] [Google Scholar]
- 12.Reurink G, Whiteley R, Tol JL. Hamstring injuries and predicting return to play “bye bye MRI?” Br J Sports Med 2015;49:1162–3. 10.1136/bjsports-2015-094771 [DOI] [PubMed] [Google Scholar]
- 13.Hasselman CT, Best TM, Hughes C, et al. . Explanation for various rectus femoris strain injuries using previously described muscle architecture. Am J Sports Med 1995;23:493–9. 10.1177/036354659502300421 [DOI] [PubMed] [Google Scholar]
- 14.Hughes C, Hasselman CT, Best TM, et al. . Incomplete, intrasubstance strain injuries of the rectus femoris muscle. Am J Sports Med 1995;23:500–6. 10.1177/036354659502300422 [DOI] [PubMed] [Google Scholar]
- 15.Cross TM, Gibbs N, Houang MT, et al. . Acute quadriceps muscle strains: magnetic resonance imaging features and prognosis. Am J Sports Med 2004;32:710–19. 10.1177/0363546503261734 [DOI] [PubMed] [Google Scholar]
- 16.Balius R, Maestro A, Pedret C, et al. . Central aponeurosis tears of the rectus femoris: practical sonographic prognosis. Br J Sports Med 2009;43:818–24. 10.1136/bjsm.2008.052332 [DOI] [PubMed] [Google Scholar]