Abstract
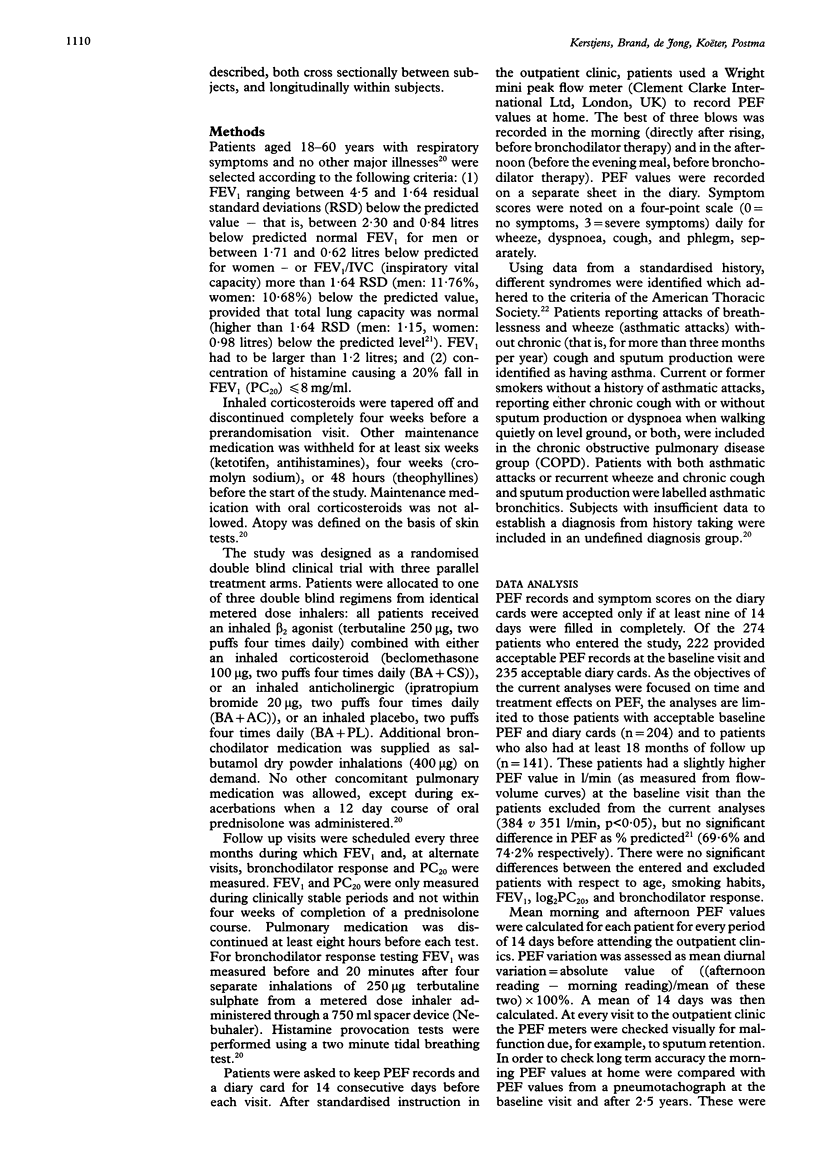
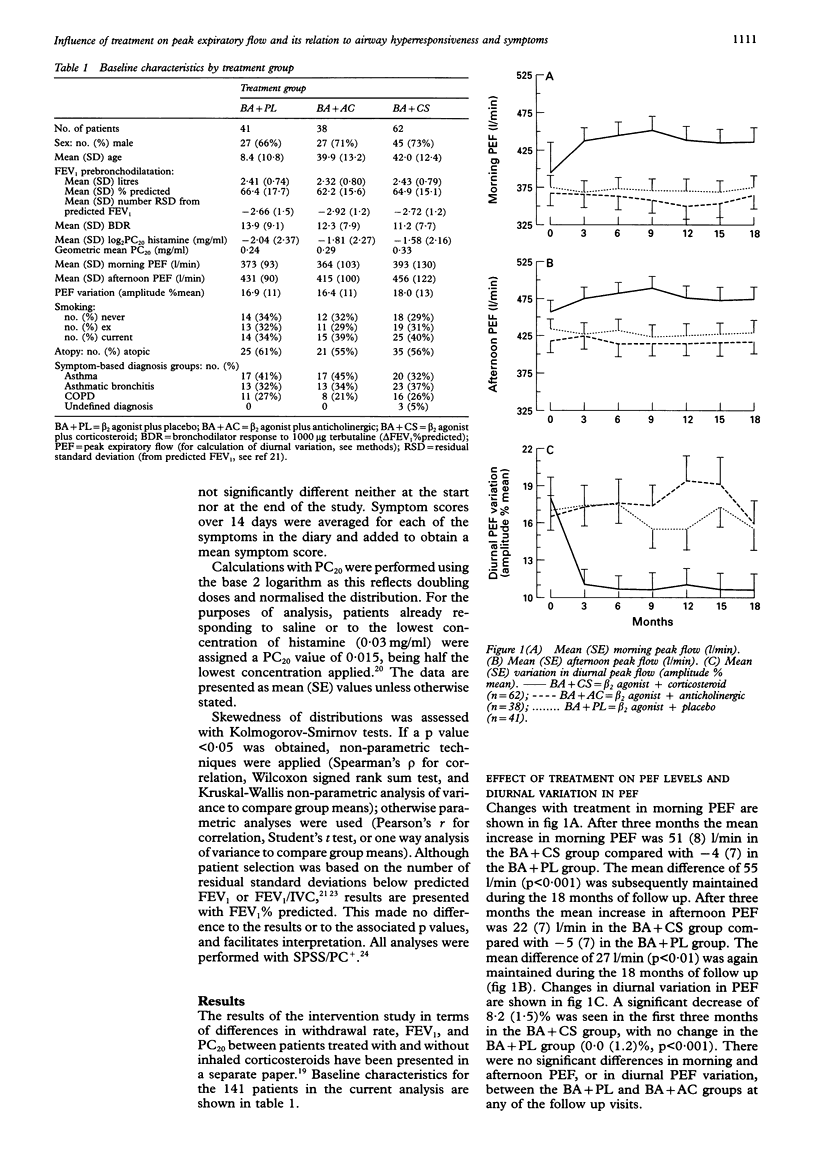
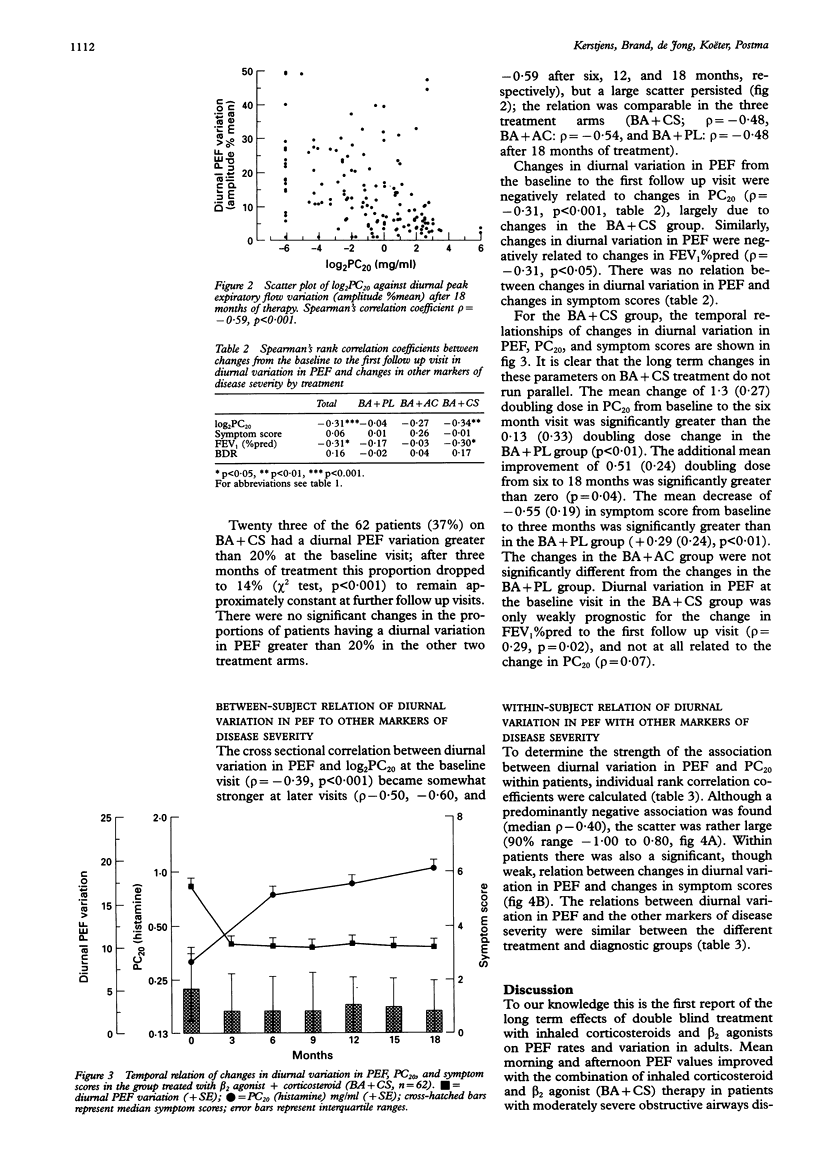
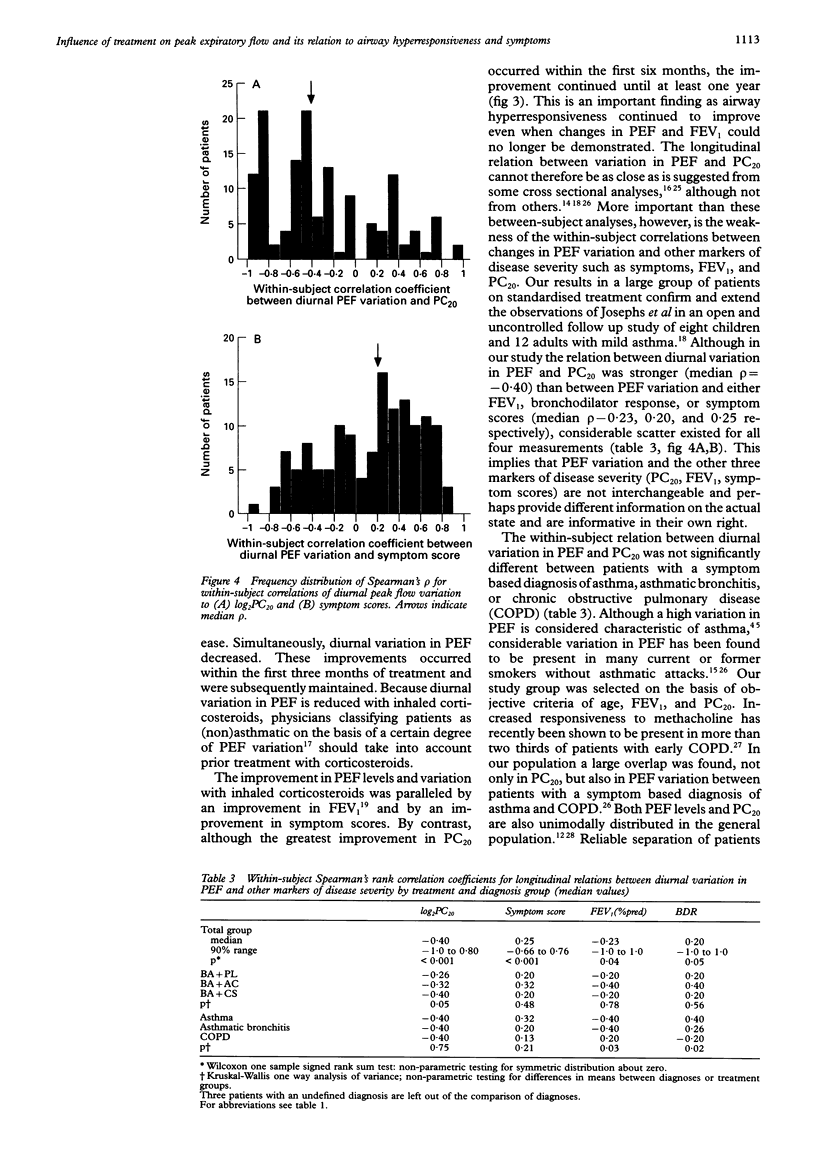
BACKGROUND--Despite effective treatments, the morbidity and mortality of obstructive airways disease (asthma and COPD) remains high. Home monitoring of peak expiratory flow (PEF) is increasingly being advocated as an aid to better management of obstructive airways disease. The few available studies describing effects of treatment on the level and variation of PEF have involved relatively small numbers of subjects and did not use control groups. METHODS--Patients aged 18-60 years were selected with PC20 < or = 8 mg/ml and FEV1 < 95% confidence interval of predicted normal. They were randomised to receive, in addition to a beta 2 agonist, either an inhaled corticosteroid (BA+CS), an anticholinergic (BA+AC), or a placebo (BA+PL). One hundred and forty one of these subjects with moderately severe obstructive airways disease completed seven periods of two weeks of morning and afternoon PEF measurements at home during 18 months of blind follow up. RESULTS--Improvements in PEF occurred within the first three months of treatment with BA+CS and was subsequently maintained: the mean (SE) increase in morning PEF was 51 (8) l/min in the BA+CS group compared with no change in the other two groups. Similarly, afternoon PEF increased by 22 (7) l/min. Diurnal variation in PEF (amplitude %mean) decreased from 18.0% to 10.2% in the first three months of treatment with BA+CS. Within-subject relations between changes in diurnal variation in PEF and changes in PC20 were found to be predominantly negative (median rho-0.40) but with a large scatter. Relations between diurnal variation in PEF and changes in symptom scores, FEV1, and bronchodilator response were even weaker. CONCLUSIONS--In patients with moderately severe obstructive airways disease, PEF rates and variation are greatly improved by inhaled corticosteroids. Since the relation of diurnal PEF variation with PC20, symptoms, FEV1, and bronchodilator response were all weak, these markers of disease severity may all provide different information on the actual disease state. PEF measurements should be used in addition to the other markers but not instead of them.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brand P. L., Kerstjens H. A., Postma D. S., Sterk P. J., Quanjer P. H., Sluiter H. J., Dijkman J. H., van Herwaarden C. L., Hilvering C., Jansen H. M. Long-term multicentre trial in chronic nonspecific lung disease: methodology and baseline assessment in adult patients. Dutch CNSLD Study Group. Eur Respir J. 1992 Jan;5(1):21–31. [PubMed] [Google Scholar]
- Brand P. L., Postma D. S., Kerstjens H. A., Koëter G. H. Relationship of airway hyperresponsiveness to respiratory symptoms and diurnal peak flow variation in patients with obstructive lung disease. The Dutch CNSLD Study Group. Am Rev Respir Dis. 1991 May;143(5 Pt 1):916–921. doi: 10.1164/ajrccm/143.5_Pt_1.916. [DOI] [PubMed] [Google Scholar]
- Clark N. M., Evans D., Mellins R. B. Patient use of peak flow monitoring. Am Rev Respir Dis. 1992 Mar;145(3):722–725. doi: 10.1164/ajrccm/145.3.722. [DOI] [PubMed] [Google Scholar]
- Corrigan C. J., Brown P. H., Barnes N. C., Szefler S. J., Tsai J. J., Frew A. J., Kay A. B. Glucocorticoid resistance in chronic asthma. Glucocorticoid pharmacokinetics, glucocorticoid receptor characteristics, and inhibition of peripheral blood T cell proliferation by glucocorticoids in vitro. Am Rev Respir Dis. 1991 Nov;144(5):1016–1025. doi: 10.1164/ajrccm/144.5.1016. [DOI] [PubMed] [Google Scholar]
- Cross D., Nelson H. S. The role of the peak flow meter in the diagnosis and management of asthma. J Allergy Clin Immunol. 1991 Jan;87(1 Pt 1):120–128. doi: 10.1016/0091-6749(91)90223-b. [DOI] [PubMed] [Google Scholar]
- Griffin E., Håkansson L., Formgren H., Jörgensen K., Peterson C., Venge P. Blood eosinophil number and activity in relation to lung function in patients with asthma and with eosinophilia. J Allergy Clin Immunol. 1991 Feb;87(2):548–557. doi: 10.1016/0091-6749(91)90014-f. [DOI] [PubMed] [Google Scholar]
- Guidelines for management of asthma in adults: I--Chronic persistent asthma. Statement by the British Thoracic Society, Research Unit of the Royal College of Physicians of London, King's Fund Centre, National Asthma Campaign. BMJ. 1990 Sep 29;301(6753):651–653. doi: 10.1136/bmj.301.6753.651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haahtela T., Järvinen M., Kava T., Kiviranta K., Koskinen S., Lehtonen K., Nikander K., Persson T., Reinikainen K., Selroos O. Comparison of a beta 2-agonist, terbutaline, with an inhaled corticosteroid, budesonide, in newly detected asthma. N Engl J Med. 1991 Aug 8;325(6):388–392. doi: 10.1056/NEJM199108083250603. [DOI] [PubMed] [Google Scholar]
- Hetzel M. R., Clark T. J. Comparison of normal and asthmatic circadian rhythms in peak expiratory flow rate. Thorax. 1980 Oct;35(10):732–738. doi: 10.1136/thx.35.10.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins B. G., Britton J. R., Chinn S., Cooper S., Burney P. G., Tattersfield A. E. Comparison of bronchial reactivity and peak expiratory flow variability measurements for epidemiologic studies. Am Rev Respir Dis. 1992 Mar;145(3):588–593. doi: 10.1164/ajrccm/145.3.588. [DOI] [PubMed] [Google Scholar]
- Higgins B. G., Britton J. R., Chinn S., Jones T. D., Jenkinson D., Burney P. G., Tattersfield A. E. The distribution of peak expiratory flow variability in a population sample. Am Rev Respir Dis. 1989 Nov;140(5):1368–1372. doi: 10.1164/ajrccm/140.5.1368. [DOI] [PubMed] [Google Scholar]
- Josephs L. K., Gregg I., Mullee M. A., Holgate S. T. Nonspecific bronchial reactivity and its relationship to the clinical expression of asthma. A longitudinal study. Am Rev Respir Dis. 1989 Aug;140(2):350–357. doi: 10.1164/ajrccm/140.2.350. [DOI] [PubMed] [Google Scholar]
- Kerstjens H. A., Brand P. L., Hughes M. D., Robinson N. J., Postma D. S., Sluiter H. J., Bleecker E. R., Dekhuijzen P. N., de Jong P. M., Mengelers H. J. A comparison of bronchodilator therapy with or without inhaled corticosteroid therapy for obstructive airways disease. Dutch Chronic Non-Specific Lung Disease Study Group. N Engl J Med. 1992 Nov 12;327(20):1413–1419. doi: 10.1056/NEJM199211123272003. [DOI] [PubMed] [Google Scholar]
- Kerstjens H. A., Overbeek S. E., Schouten J. P., Brand P. L., Postma D. S. Airways hyperresponsiveness, bronchodilator response, allergy and smoking predict improvement in FEV1 during long-term inhaled corticosteroid treatment. Dutch CNSLD Study Group. Eur Respir J. 1993 Jun;6(6):868–876. [PubMed] [Google Scholar]
- Lane S. J., Lee T. H. Glucocorticoid receptor characteristics in monocytes of patients with corticosteroid-resistant bronchial asthma. Am Rev Respir Dis. 1991 May;143(5 Pt 1):1020–1024. doi: 10.1164/ajrccm/143.5_Pt_1.1020. [DOI] [PubMed] [Google Scholar]
- Miller M. R., Pincock A. C. Predicted values: how should we use them? Thorax. 1988 Apr;43(4):265–267. doi: 10.1136/thx.43.4.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molema J., van Herwaarden C. L., Folgering H. T. Effects of long-term treatment with inhaled cromoglycate and budesonide on bronchial hyperresponsiveness in patients with allergic asthma. Eur Respir J. 1989 Apr;2(4):308–316. [PubMed] [Google Scholar]
- Quackenboss J. J., Lebowitz M. D., Krzyzanowski M. The normal range of diurnal changes in peak expiratory flow rates. Relationship to symptoms and respiratory disease. Am Rev Respir Dis. 1991 Feb;143(2):323–330. doi: 10.1164/ajrccm/143.2.323. [DOI] [PubMed] [Google Scholar]
- Ramsdale E. H., Morris M. M., Hargreave F. E. Interpretation of the variability of peak flow rates in chronic bronchitis. Thorax. 1986 Oct;41(10):771–776. doi: 10.1136/thx.41.10.771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rijcken B., Schouten J. P., Weiss S. T., Meinesz A. F., de Vries K., van der Lende R. The distribution of bronchial responsiveness to histamine in symptomatic and in asymptomatic subjects. A population-based analysis of various indices of responsiveness. Am Rev Respir Dis. 1989 Sep;140(3):615–623. doi: 10.1164/ajrccm/140.3.615. [DOI] [PubMed] [Google Scholar]
- Ryan G., Latimer K. M., Dolovich J., Hargreave F. E. Bronchial responsiveness to histamine: relationship to diurnal variation of peak flow rate, improvement after bronchodilator, and airway calibre. Thorax. 1982 Jun;37(6):423–429. doi: 10.1136/thx.37.6.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tashkin D. P., Altose M. D., Bleecker E. R., Connett J. E., Kanner R. E., Lee W. W., Wise R. The lung health study: airway responsiveness to inhaled methacholine in smokers with mild to moderate airflow limitation. The Lung Health Study Research Group. Am Rev Respir Dis. 1992 Feb;145(2 Pt 1):301–310. doi: 10.1164/ajrccm/145.2_Pt_1.301. [DOI] [PubMed] [Google Scholar]
- Waalkens H. J., Gerritsen J., Koëter G. H., Krouwels F. H., van Aalderen W. M., Knol K. Budesonide and terbutaline or terbutaline alone in children with mild asthma: effects on bronchial hyperresponsiveness and diurnal variation in peak flow. Thorax. 1991 Jul;46(7):499–503. doi: 10.1136/thx.46.7.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolcock A. J., Yan K., Salome C. M. Effect of therapy on bronchial hyperresponsiveness in the long-term management of asthma. Clin Allergy. 1988 Mar;18(2):165–176. doi: 10.1111/j.1365-2222.1988.tb02856.x. [DOI] [PubMed] [Google Scholar]
- van Essen-Zandvliet E. E., Hughes M. D., Waalkens H. J., Duiverman E. J., Pocock S. J., Kerrebijn K. F. Effects of 22 months of treatment with inhaled corticosteroids and/or beta-2-agonists on lung function, airway responsiveness, and symptoms in children with asthma. The Dutch Chronic Non-specific Lung Disease Study Group. Am Rev Respir Dis. 1992 Sep;146(3):547–554. doi: 10.1164/ajrccm/146.3.547. [DOI] [PubMed] [Google Scholar]


