Abstract
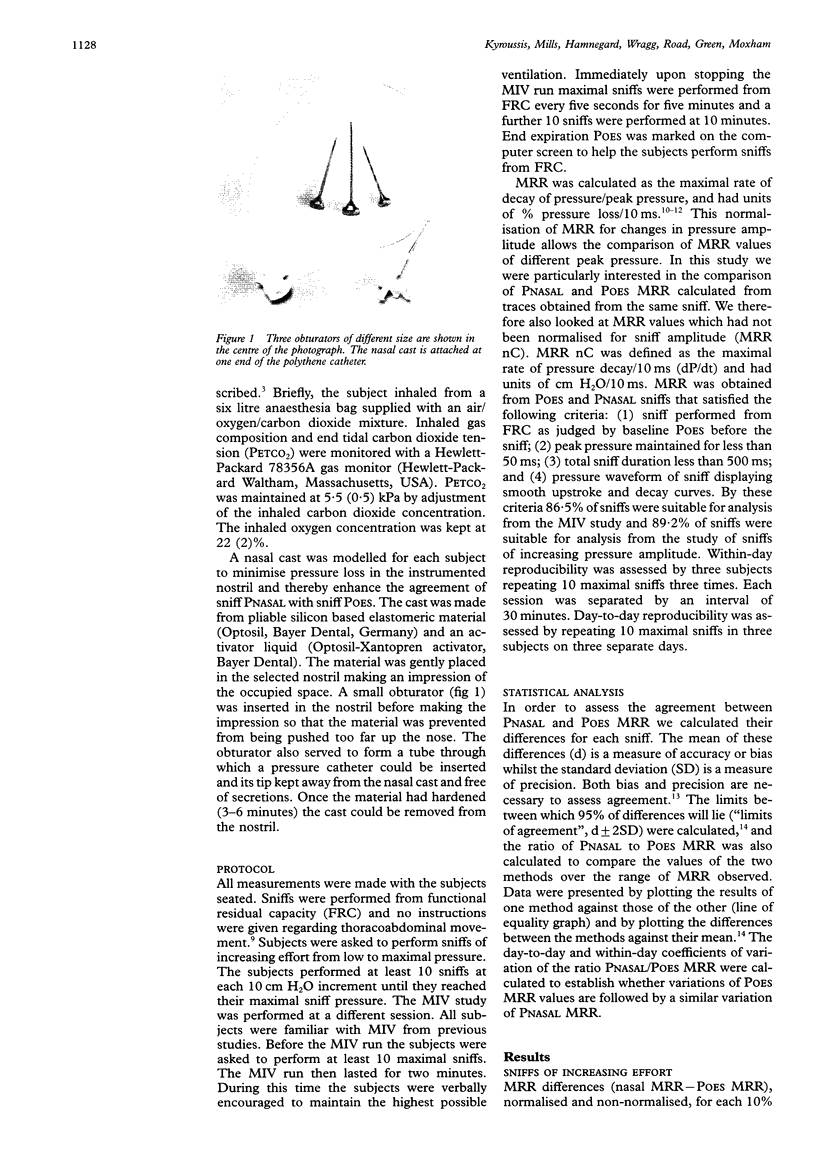
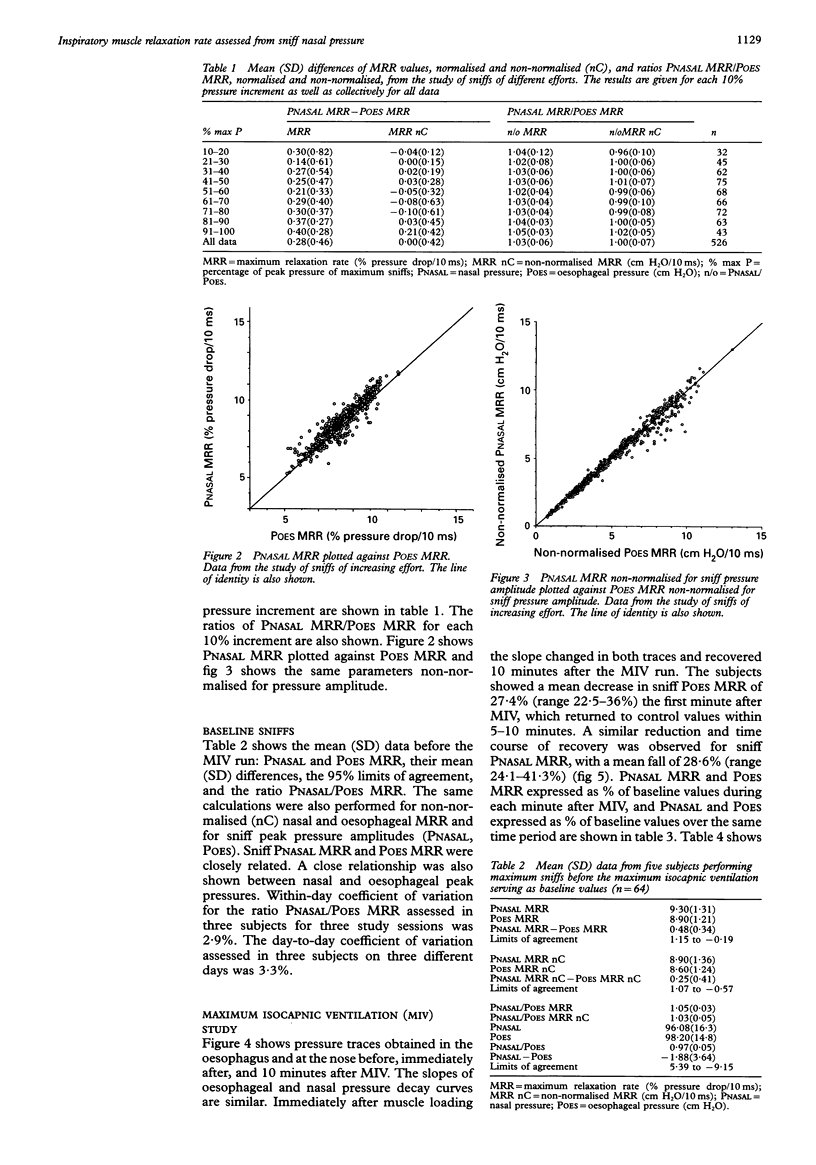
BACKGROUND--Slowing of the maximum relaxation rate (MRR) of inspiratory muscles measured from oesophageal pressure (POES) during sniffs has been used as an index of the onset and recovery of respiratory muscle fatigue. The purpose of this study was to measure MRR at the nose (PNASAL MRR), to investigate its relationship with POES MRR, and to establish whether PNASAL MRR slows with respiratory loading. METHODS--Five normal subjects were studied. Each performed sniffs before and after two minutes of maximal isocapnic ventilation (MIV). In a separate session the subjects performed submaximal sniffs. POES and PNASAL were recorded during sniffs and the MRR (% pressure fall/10 ms) for each sniff was determined. RESULTS--Before MIV mean POES MRR was 8.9 and PNASAL MRR was 9.3. The mean (SD) difference between PNASAL MRR and POES MRR during a maximal sniff was 0.48 (0.34) (n = 64) and during submaximal sniffs was 0.28 (0.46) (n = 526). The subjects showed a mean decrease in sniff POES MRR of 27.4% (range 22.5-36%) after MIV and a similar reduction in sniff PNASAL MRR of 28.5% (range 24.1-41.3%). Both returned to control values within 5-10 minutes. CONCLUSIONS--PNASAL MRR reflects POES MRR over a wide range of sniff pressures, PNASAL MRR of maximal sniffs reflects POES MRR in normal subjects at rest and following MIV, so measurement of PNASAL MRR may be a useful non-invasive method for measuring inspiratory muscle MRR, thereby providing an index of respiratory muscle fatigue.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baydur A., Behrakis P. K., Zin W. A., Jaeger M., Milic-Emili J. A simple method for assessing the validity of the esophageal balloon technique. Am Rev Respir Dis. 1982 Nov;126(5):788–791. doi: 10.1164/arrd.1982.126.5.788. [DOI] [PubMed] [Google Scholar]
- Bland J. M., Altman D. G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986 Feb 8;1(8476):307–310. [PubMed] [Google Scholar]
- Bridger G. P. Physiology of the nasal valve. Arch Otolaryngol. 1970 Dec;92(6):543–553. doi: 10.1001/archotol.1970.04310060015005. [DOI] [PubMed] [Google Scholar]
- Bridger G. P., Proctor D. F. Maximum nasal inspiratory flow and nasal resistance. Ann Otol Rhinol Laryngol. 1970 Jun;79(3):481–488. doi: 10.1177/000348947007900308. [DOI] [PubMed] [Google Scholar]
- Dick T. E., van Lunteren E. Fiber subtype distribution of pharyngeal dilator muscles and diaphragm in the cat. J Appl Physiol (1985) 1990 May;68(5):2237–2240. doi: 10.1152/jappl.1990.68.5.2237. [DOI] [PubMed] [Google Scholar]
- Edwards R. H., Hill D. K., Jones D. A. Metabolic changes associated with the slowing of relaxation in fatigued mouse muscle. J Physiol. 1975 Oct;251(2):287–301. doi: 10.1113/jphysiol.1975.sp011093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esau S. A., Bye P. T., Pardy R. L. Changes in rate of relaxation of sniffs with diaphragmatic fatigue in humans. J Appl Physiol Respir Environ Exerc Physiol. 1983 Sep;55(3):731–735. doi: 10.1152/jappl.1983.55.3.731. [DOI] [PubMed] [Google Scholar]
- Haight J. S., Cole P. The site and function of the nasal valve. Laryngoscope. 1983 Jan;93(1):49–55. doi: 10.1288/00005537-198301000-00009. [DOI] [PubMed] [Google Scholar]
- Héritier F., Perret C., Fitting J. W. Esophageal and mouth pressure during sniffs with and without nasal occlusion. Respir Physiol. 1991 Dec;86(3):305–313. doi: 10.1016/0034-5687(91)90102-o. [DOI] [PubMed] [Google Scholar]
- JEWELL B. R., WILKIE D. R. The mechanical properties of relaxing muscle. J Physiol. 1960 Jun;152:30–47. doi: 10.1113/jphysiol.1960.sp006467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaeger M. J. Effect of the cheeks and the compliance of alveolar gas on the measurement of respiratory variables. Respir Physiol. 1982 Mar;47(3):325–340. doi: 10.1016/0034-5687(82)90061-5. [DOI] [PubMed] [Google Scholar]
- Koulouris N., Mulvey D. A., Laroche C. M., Sawicka E. H., Green M., Moxham J. The measurement of inspiratory muscle strength by sniff esophageal, nasopharyngeal, and mouth pressures. Am Rev Respir Dis. 1989 Mar;139(3):641–646. doi: 10.1164/ajrccm/139.3.641. [DOI] [PubMed] [Google Scholar]
- Koulouris N., Vianna L. G., Mulvey D. A., Green M., Moxham J. Maximal relaxation rates of esophageal, nose, and mouth pressures during a sniff reflect inspiratory muscle fatigue. Am Rev Respir Dis. 1989 May;139(5):1213–1217. doi: 10.1164/ajrccm/139.5.1213. [DOI] [PubMed] [Google Scholar]
- Levy R. D., Esau S. A., Bye P. T., Pardy R. L. Relaxation rate of mouth pressure with sniffs at rest and with inspiratory muscle fatigue. Am Rev Respir Dis. 1984 Jul;130(1):38–41. doi: 10.1164/arrd.1984.130.1.38. [DOI] [PubMed] [Google Scholar]
- MILIC-EMILI J., MEAD J., TURNER J. M., GLAUSER E. M. IMPROVED TECHNIQUE FOR ESTIMATING PLEURAL PRESSURE FROM ESOPHAGEAL BALLOONS. J Appl Physiol. 1964 Mar;19:207–211. doi: 10.1152/jappl.1964.19.2.207. [DOI] [PubMed] [Google Scholar]
- Mador M. J., Kufel T. J. Effect of inspiratory muscle fatigue on inspiratory muscle relaxation rates in healthy subjects. Chest. 1992 Dec;102(6):1767–1773. doi: 10.1378/chest.102.6.1767. [DOI] [PubMed] [Google Scholar]
- Mador M. J., Kufel T. J. Effect of inspiratory muscle fatigue on inspiratory muscle relaxation rates in healthy subjects. Chest. 1992 Dec;102(6):1767–1773. doi: 10.1378/chest.102.6.1767. [DOI] [PubMed] [Google Scholar]
- Marazzini L., Cavestri R., Gori D., Gatti L., Longhini E. Diffference between mouth and esophageal occlusion pressure during CO2 rebreathing in chronic obstructive pulmonary disease. Am Rev Respir Dis. 1978 Dec;118(6):1027–1033. doi: 10.1164/arrd.1978.118.6.1027. [DOI] [PubMed] [Google Scholar]
- Miller J. M., Moxham J., Green M. The maximal sniff in the assessment of diaphragm function in man. Clin Sci (Lond) 1985 Jul;69(1):91–96. doi: 10.1042/cs0690091. [DOI] [PubMed] [Google Scholar]
- Mulvey D. A., Elliott M. W., Koulouris N. G., Carroll M. P., Moxham J., Green M. Sniff esophageal and nasopharyngeal pressures and maximal relaxation rates in patients with respiratory dysfunction. Am Rev Respir Dis. 1991 May;143(5 Pt 1):950–953. doi: 10.1164/ajrccm/143.5_Pt_1.950. [DOI] [PubMed] [Google Scholar]
- Mulvey D. A., Koulouris N. G., Elliott M. W., Laroche C. M., Moxham J., Green M. Inspiratory muscle relaxation rate after voluntary maximal isocapnic ventilation in humans. J Appl Physiol (1985) 1991 May;70(5):2173–2180. doi: 10.1152/jappl.1991.70.5.2173. [DOI] [PubMed] [Google Scholar]
- Murciano D., Aubier M., Bussi S., Derenne J. P., Pariente R., Milic-Emili J. Comparison of esophageal, tracheal, and mouth occlusion pressure in patients with chronic obstructive pulmonary disease during acute respiratory failure. Am Rev Respir Dis. 1982 Nov;126(5):837–841. doi: 10.1164/arrd.1982.126.5.837. [DOI] [PubMed] [Google Scholar]
- Remmers J. E., deGroot W. J., Sauerland E. K., Anch A. M. Pathogenesis of upper airway occlusion during sleep. J Appl Physiol Respir Environ Exerc Physiol. 1978 Jun;44(6):931–938. doi: 10.1152/jappl.1978.44.6.931. [DOI] [PubMed] [Google Scholar]
- Rodenstein D. O., Stănescu D. C., Francis C. Demonstration of failure of body plethysmography in airway obstruction. J Appl Physiol Respir Environ Exerc Physiol. 1982 Apr;52(4):949–954. doi: 10.1152/jappl.1982.52.4.949. [DOI] [PubMed] [Google Scholar]
- Van Lunteren E., Vafaie H. Force potentiation in respiratory muscles: comparison of diaphragm and sternohyoid. Am J Physiol. 1993 Jun;264(6 Pt 2):R1095–R1100. doi: 10.1152/ajpregu.1993.264.6.R1095. [DOI] [PubMed] [Google Scholar]
- Wiles C. M., Young A., Jones D. A., Edwards R. H. Relaxation rate of constituent muscle-fibre types in human quadriceps. Clin Sci (Lond) 1979 Jan;56(1):47–52. doi: 10.1042/cs0560047. [DOI] [PubMed] [Google Scholar]
- van Lunteren E., Salomone R. J., Manubay P., Supinski G. S., Dick T. E. Contractile and endurance properties of geniohyoid and diaphragm muscles. J Appl Physiol (1985) 1990 Dec;69(6):1992–1997. doi: 10.1152/jappl.1990.69.6.1992. [DOI] [PubMed] [Google Scholar]
- van Lunteren E., Salomone R. J., Manubay P., Supinski G. S., Dick T. E. Contractile and endurance properties of geniohyoid and diaphragm muscles. J Appl Physiol (1985) 1990 Dec;69(6):1992–1997. doi: 10.1152/jappl.1990.69.6.1992. [DOI] [PubMed] [Google Scholar]
- van Lunteren E., Strohl K. P. The muscles of the upper airways. Clin Chest Med. 1986 Jun;7(2):171–188. [PubMed] [Google Scholar]