Abstract
Background:
Tumor necrosis factor receptor-associated factor 6 (TRAF6) has been reported to be highly expressed in many tumor tissues, but it is still of value to detect its expression in patients with colon cancer and to clarify its clinical significance.
Objectives:
To study the expression and clinical significance of TRAF6 in patients with colon cancer.
Patients and Methods:
A total of 135 patients with colon cancer who underwent surgery at our hospital from February 2008 to March 2013 were selected. The expression levels of TRAF6 protein in tumor and paracancerous tissues were detected with the immunohistochemical method to evaluate their clinical significance.
Results:
The positive expression rate of TRAF6 in tumor tissues was 66.7%, which was significantly higher than in normal paracancerous tissues (18.5%). The positive expression rate of TRAF6 was significantly correlated with Dukes’ staging, degree of differentiation, and lymphatic metastasis (P < 0.05), but not gender or age (P > 0.05). The expression level of TRAF6 was negatively correlated with the 5-year survival rate; patients with high TRAF6 expression levels had significantly decreased survival compared to those with low levels (P < 0.05).
Conclusions:
TRAF6 plays an important role in the onset of colon cancer; therefore, drugs targeting it may have great clinical significance in the treatment of this disease.
Keywords: Receptors, Tumor Necrosis Factor, Gene Expression, Colonic Neoplasms
1. Background
Colon cancer has become the third most common malignancy worldwide, with a morbidity rate that is continuously increasing as the population ages (1). Although novel treatment protocols have been developed, the prognosis for colon cancer remains poor, with a 5-year survival rate lower than 40%. Patients with colon cancer mainly die of metastasis and recurrence (2). Despite numerous experimental and clinical studies on the pathogenesis of colon cancer, its mechanisms have not yet been elucidated, though they are of great clinical significance for the diagnosis and treatment of this cancer. Tumor necrosis factor receptor-associated factor 6 (TRAF6) has been reported to be highly expressed in many tumor tissues (3), but it is still of value to detect its expression in patients with colon cancer and to clarify its clinical significance (4, 5).
2. Objectives
The aim of this study was to detect the expression levels of TRAF6 protein in tumor and paracancerous tissues using immunohistochemical methods, to identify correlations between the clinicopathological characteristics and prognosis of colon cancer, and to provide evidence for future prognostic determinations and target therapies.
3. Patients and Methods
3.1. General Information
A total of 135 patients with primary colon cancer, who underwent surgery at our hospital from February 2008 to March 2013, were selected. The study was approved by the hospital’s ethics committee. Informed consent was obtained from each patient, and the study protocol conformed to the ethical guidelines of the 1975 declaration of Helsinki. All patients included in this study had complete medical records. Patients who had received radiotherapy, chemotherapy, or biological immunotherapy before surgery, or who were lost to follow-up, were excluded.
The sample size Equation is:
| (1) |
Where N is the sample size, Z is the confidence interval (for a level of confidence of 95% in this study, Z = 1.96), P is the probability value, and E is the error value.
3.2. Immunohistochemical and HE Staining
Double staining was used in this study. Tumor and paracancerous tissues resected during surgical procedures were immersed in neutral formalin at 4°C for 2 days, and embedded with paraffin into 6-μm-thick sections (Leica Biosystems, USA), which were then deparaffinized with dimethyl benzene and hydrated with ethanol solutions at gradient concentrations. After antigen retrieval (Beijing Zhongshan Golden Bridge Biotechnology Co., Ltd., China) and blocking with rabbit immune serum (Beijing Zhongshan Golden Bridge Biotechnology Co., Ltd., China), the sections were incubated with TRAF6 antibody (Santa Cruz, 1: 50) in a 37°C incubator for 2 hours, washed with PBS, incubated with secondary antibody for 1 hour, washed again with PBS, and incubated with horseradish peroxidase-labeled streptavidin (Beijing Zhongshan Golden Bridge Biotechnology Co., Ltd., China) for another 15 minutes. Afterwards, the sections were washed with PBS, colored with DAB (Beijing Zhongshan Golden Bridge Biotechnology Co., Ltd., China), counterstained with haematoxylin, and observed under a microscope. PBS was used to replace primary antibody as the negative control.
With regard to standards for the determination of immunohistochemical staining, TRAF6 was determined to be positively expressed in the case of brownish-yellow precipitates in the cytoplasm. The procedure was completed by two experienced pathologists. By using the double-blind method, 15 fields of vision were selected for each section with a high-powered lens (× 400), and the ratio of the number of TRAF6-positive cells to 100 average cells was calculated as the positive rate. Positive results of immunohistochemical staining were determined according to the following two aspects: 1) percentage of TRAF6-positive cells: < 1%, 0; 1% - 10%, 1 point; 10% - 30%, 2 points; 30% - 60%, 3 points; > 60%, 4 points, and 2) staining results of TRAF6-positive cells: negative, 0; yellowish, 1 point; yellow, 2 points; brownish yellow, 3 points. For the determination of results, 0 - 2 points were negative and 3 - 7 points were positive.
3.3. Detection of TRAF6 mRNA Expression in Tumor and Normal Tissues by RT-PCR
Tumor and paracancerous tissues resected during surgical procedures were immediately stored in liquid nitrogen, from which total RNA was extracted by using TRIzol reagent according to the kit’s instructions.
Upstream primer for TRAF6: 5’-GAATCACTTGGCACGACACTT-3’, downstream primer for TRAF6: 5’-GAGTTTCCATTTTGGCAGTCA-3’ and length of amplified fragment: 227 bp. GAPDH was used as an internal reference. Upstream primer for GAPDH: 5’-ACCACAGTCCATGCCATCAC-3’, downstream primer for GAPDH: 5’-TGCTGTAGCCAAATTCGTTG-3’ and length of amplified fragment: 450 bp.
RT-PCR was performed under the following conditions: reverse transcription at 50°C for 30 minutes, reaction at 95°C for 15 minutes (cycling was started), denaturation at 94°C for 30 d, annealing at 57°C for 30 seconds, and extension at 72°C for 30 seconds, for a total of 30 cycles. After final extension at 72°C for another 10 minutes, the PCR products were subjected to agarose gel electrophoresis.
3.4. Statistical Analysis
All data were analyzed by SPSS 13.0. The numerical data were compared by χ2 test, and the survival rates were estimated by the Kaplan-Meier method. P < 0.05 was considered statistically significant.
4. Results
4.1. TRAF6 Expression in Tumor and Paracancerous Tissues
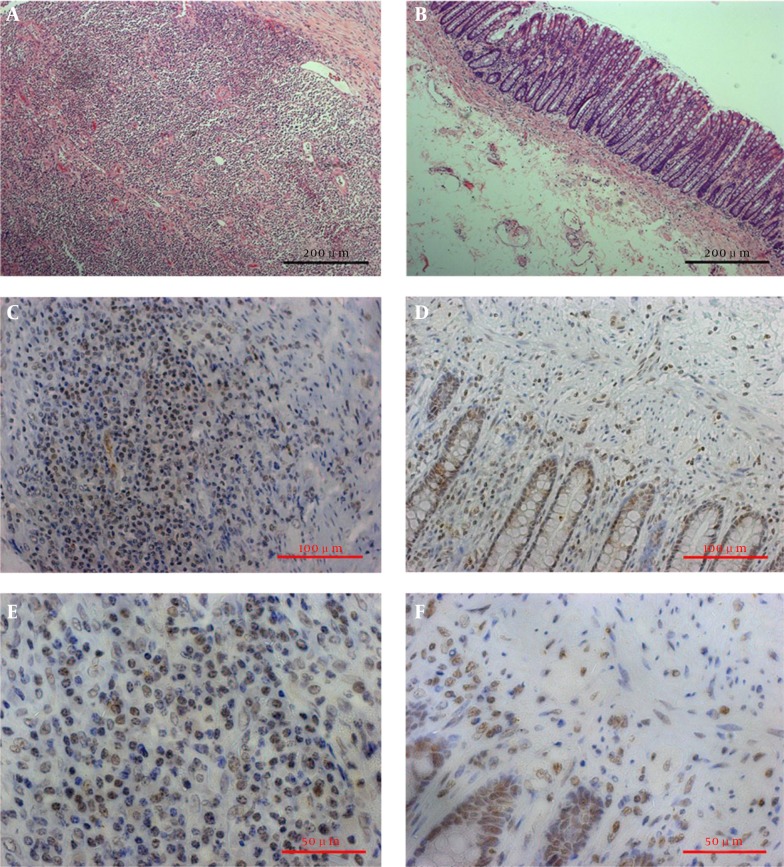
The HE staining results for the tumor and paracancerous tissues are shown in Figure 1. Significantly more TRAF6 protein was expressed in tumor tissues than in paracancerous tissues. In tumor tissues (Figure 1 A - C), TRAF6 protein was mainly expressed in the cytoplasm, showing dark brown particles. Meanwhile, tumor stromal cells were also positively stained. In paracancerous tissues (Figure 1 D - F), however, TRAF6 protein was mainly scattered in the cytoplasm, exhibiting light brown particles. In the meantime, the stroma was slightly positively stained. TRAF6 was weakly positively expressed in the cytoplasm of normal tissues (positive rate: 33.3%), which was significantly less than in tumor tissues (positive rate: 66.7%; P < 0.05) (Table 1).
Figure 1. TRAF6 Expression.
A - C, TRAF6 expression in tumor; and D - F, paracancerous tissues. A and D (× 100): HE staining; B and E (× 200), C and F (× 400immunohistochemical staining.
Table 1. TRAF6 Expression in Tumor and Paracancerous Tissues.
| Group | TRAF6 Expressiona,b | |
|---|---|---|
| Proportion of Positive Expression | Proportion of Negative Expression | |
| Tumor tissue | 90 (66.7) | 45 (33.3) |
| Paracancerous tissue | 25 (18.5) | 110 (81.5) |
aP value < 0.0001.
bValues are expressed as No. (%).
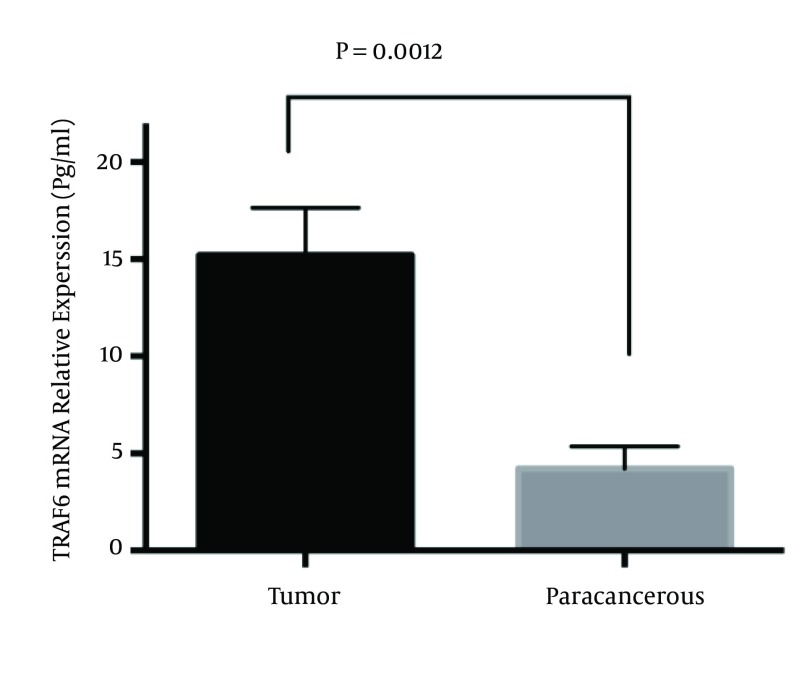
4.2. RT-PCR Results
Tumor and paracancerous tissues all expressed TRAF6 mRNA. The TRAF6 mRNA expression level in tumor tissues (15.21 ± 2.43) was significantly higher than in paracancerous tissues (4.23 ± 1.13; P < 0.01) (Figure 2).
Figure 2. TRAF6 mRNA Expression in Tumor and Paracancerous Tissues (P < 0.01).
4.3. Correlation Between TRAF6 Expression and Clinicopathological Characteristics, Staging of Colon Cancer
The positive expression rate of TRAF6 was not correlated with the age or gender of the patients (P > 0.05), whereas it was correlated with Dukes’ staging, degree of differentiation, and lymphatic metastasis (P < 0.05). TRAF6 was highly expressed in patients with later stages, lower degrees of differentiation, and lymphatic metastases (Table 2).
Table 2. Correlation Between TRAF6 and Clinicopathological Characteristics.
| Group | N | TRAF6 Expression | P Value | |
|---|---|---|---|---|
| Positive | Negative | |||
| Gender | 0.81 | |||
| Male | 71 | 48 | 23 | |
| Female | 64 | 42 | 22 | |
| Age, y | 0.61 | |||
| < 60 | 49 | 34 | 15 | |
| ≥ 60 | 86 | 56 | 30 | |
| Degree of differentiation | < 0.001 | |||
| Low | 55 | 39 | 16 | |
| Medium | 69 | 41 | 28 | |
| High | 11 | 5 | 6 | |
| Dukes’ stage | < 0.001 | |||
| A + B | 57 | 20 | 37 | |
| C + D | 78 | 70 | 8 | |
| Lymphatic metastasis | 0.0002 | |||
| Yes | 102 | 74 | 28 | |
| None | 33 | 12 | 21 | |
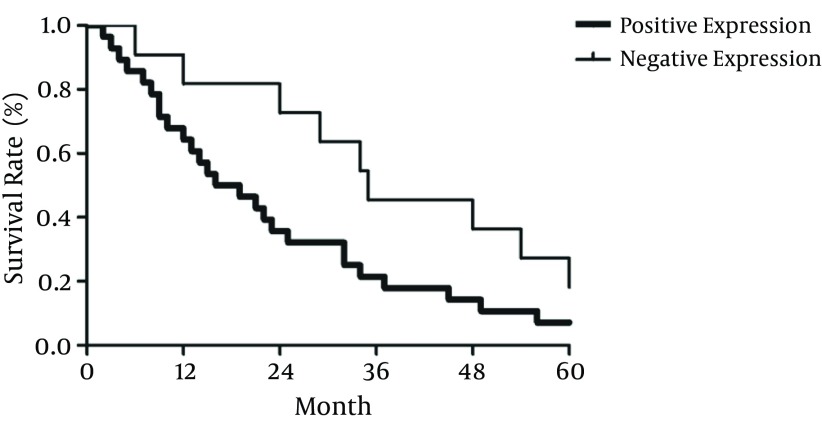
4.4. Correlation Between TRAF6 Expression and 5-Year Survival Rate
The expression of TRAF6 was negatively correlated with the 5-year survival rate (Figure 3); the patients in whom more TRAF6 was expressed survived longer.
Figure 3. Correlation Between TRAF6 Expression and 5-Year Survival Rate.
5. Discussion
As a member of the TRAF family, TRAF6 consists of 530 amino acids, including a highly conservative TRAF6 domain at the C terminus and an activated coiled-coil domain at the N terminus. In particular, the activated domain comprises a RING finger and five zinc fingers (6). Out of all of the TRAFs, TRAF6 is the only member that directly binds to interleukin receptor-associated kinases, NF-κB receptor activator, and CD40. Through the signaling pathways mediated by membrane surface receptors, such as LPS, IL-1, TLR4, and CD40, TRAF6 is able to finally activate NF-κB, activator protein 1, and PKB/Akt. Since TRAF6 can activate several signaling pathways simultaneously, it plays a crucial role in the growth, proliferation, differentiation, and death of cells (7). It was previously reported that TRAF6 dominantly controlled the onset, progression, invasion, and metastasis of tumors (3, 8, 9). TRAF6 has also controlled the proliferation and invasion of tumor cells in lung cancer and esophagus cancer tissues by regulating the activity of NF-κB (3, 10), and it has been shown that inhibiting the activity of TRAF6 in multiple myeloma cells could suppress their proliferation and promote apoptosis (11). The expression of Akt was shown to be significantly elevated in colon cancer tissues (12), and inhibiting the activity of the Akt enzyme could promote the apoptosis of tumor cells and suppress their proliferation (13). Moreover, NF-κB is highly expressed in 40% of colon cancer tissues, which is closely associated with the infiltration and metastasis of these tissues. However, inhibiting the activity of NF-κB could suppress the proliferation of these cells. Therefore, we postulated that TRAF6, as the key enzyme for the activation of Akt and NF-κB, may be highly expressed in colon cancer tissues. Indeed, the outcomes herein have verified this assumption. Compared with paracancerous tissues, the expression of TRAF6 in tumor tissues was significantly increased, suggesting that TRAF6 may play a critical role in the onset, development, invasion, and metastasis of colon cancer.
The correlations between TRAF6 expression and various clinicopathological characteristics were also studied. The expression of TRAF6 was closely associated with Dukes’ staging and lymphatic metastasis. Patients with Dukes’ stage C or D, and those with lymphatic metastases, had significantly higher TRAF6 expression levels than those with stage A or B disease, and those without colon cancer. In addition, the 5-year survival rate of the patients with positive TRAF6 expression was significantly lower than in those with negative expression. Hence, it is of value to detect the expression level of TRAF6 in colon cancer tissues in clinical practice. With regard to the mechanism behind the regulatory effect of TRAF6 on the onset and progression of colon cancer cells, Sun et al. found that after binding to HIF-1α, TRAF prevented it from degradation by polyubiquitination linked with Lys63 (14). As a result, HIF-1α protein was destabilized and induced to accumulate in cells, which controlled the proliferation of tumor cells and angiogenesis by regulating the expression of many genes. Although primarily the effects of TRAF6 on colon cancer have been studied, this disease’s pathogenesis, and the possibility of treating it by down-regulating the expression of TRAF6, should be further evaluated in animal models in order to provide valuable theoretical evidence for colon cancer therapy using TRAF6 interventions.
In summary, TRAF6 was abnormally expressed in colon cancer tissues, which was closely associated with the prognosis. Targeted TRAF6 therapy, as a novel protocol, may be effective for mitigating colon cancer.
Footnotes
Authors’ Contribution:Tao Zhang: study concept and design, and critical revision of the manuscript for important intellectual content. Hui Wang and Liang Han: acquisition of data, analysis and interpretation of data, and drafting of the manuscript.
References
- 1.Edwards BK, Ward E, Kohler BA, Eheman C, Zauber AG, Anderson RN, et al. Annual report to the nation on the status of cancer, 1975-2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer. 2010;116(3):544–73. doi: 10.1002/cncr.24760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chang GJ, Rodriguez-Bigas MA, Skibber JM, Moyer VA. Lymph node evaluation and survival after curative resection of colon cancer: systematic review. J Natl Cancer Inst. 2007;99(6):433–41. doi: 10.1093/jnci/djk092. [DOI] [PubMed] [Google Scholar]
- 3.Starczynowski DT, Lockwood WW, Delehouzee S, Chari R, Wegrzyn J, Fuller M, et al. TRAF6 is an amplified oncogene bridging the RAS and NF-kappaB pathways in human lung cancer. J Clin Invest. 2011;121(10):4095–105. doi: 10.1172/JCI58818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Naderi M, Yaghootkar H, Tara F, Tavakkol Afshari J, Farid Hosseini R, Ghayour Mobarhan M, et al. Tumor necrosis factor-alpha polymorphism at position -238 in preeclampsia. Iran Red Crescent Med J. 2014;16(1):e23931. doi: 10.5812/ircmj.11195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fouad SA, Elsaaid NH, Mohamed NA, Abutaleb OM. Diagnostic Value of Serum Level of Soluble Tumor Necrosis Factor Receptor IIalpha in Egyptian Patients With Chronic Hepatitis C Virus Infection and Hepatocellular Carcinoma. Hepat Mon. 2014;14(9):e23931. doi: 10.5812/hepatmon.19346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Landstrom M. The TAK1-TRAF6 signalling pathway. Int J Biochem Cell Biol. 2010;42(5):585–9. doi: 10.1016/j.biocel.2009.12.023. [DOI] [PubMed] [Google Scholar]
- 7.Walsh MC, Kim GK, Maurizio PL, Molnar EE, Choi Y. TRAF6 autoubiquitination-independent activation of the NFkappaB and MAPK pathways in response to IL-1 and RANKL. PLoS One. 2008;3(12):e23931. doi: 10.1371/journal.pone.0004064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mu Y, Sundar R, Thakur N, Ekman M, Gudey SK, Yakymovych M, et al. TRAF6 ubiquitinates TGFbeta type I receptor to promote its cleavage and nuclear translocation in cancer. Nat Commun. 2011;2:330. doi: 10.1038/ncomms1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lin Y, Qiu Y, Xu C, Liu Q, Peng B, Kaufmann GF, et al. Functional role of asparaginyl endopeptidase ubiquitination by TRAF6 in tumor invasion and metastasis. J Natl Cancer Inst. 2014;106(4):dju012. doi: 10.1093/jnci/dju012. [DOI] [PubMed] [Google Scholar]
- 10.Ma T, Wang N, Su Z, Chen L, Zhu N, Ma C, et al. Characterization of apoptosis and proliferation in esophageal carcinoma EC109 cells following siRNA-induced down-regulation of TRAF6. Mol Cell Biochem. 2011;352(1-2):77–85. doi: 10.1007/s11010-011-0741-5. [DOI] [PubMed] [Google Scholar]
- 11.Liu H, Tamashiro S, Baritaki S, Penichet M, Yu Y, Chen H, et al. TRAF6 activation in multiple myeloma: a potential therapeutic target. Clin Lymphoma Myeloma Leuk. 2012;12(3):155–63. doi: 10.1016/j.clml.2012.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roy HK, Olusola BF, Clemens DL, Karolski WJ, Ratashak A, Lynch HT, et al. AKT proto-oncogene overexpression is an early event during sporadic colon carcinogenesis. Carcinogenesis. 2002;23(1):201–5. doi: 10.1093/carcin/23.1.201. [DOI] [PubMed] [Google Scholar]
- 13.Itoh N, Semba S, Ito M, Takeda H, Kawata S, Yamakawa M. Phosphorylation of Akt/PKB is required for suppression of cancer cell apoptosis and tumor progression in human colorectal carcinoma. Cancer. 2002;94(12):3127–34. doi: 10.1002/cncr.10591. [DOI] [PubMed] [Google Scholar]
- 14.Sun H, Li XB, Meng Y, Fan L, Li M, Fang J. TRAF6 upregulates expression of HIF-1alpha and promotes tumor angiogenesis. Cancer Res. 2013;73(15):4950–9. doi: 10.1158/0008-5472.CAN-13-0370. [DOI] [PubMed] [Google Scholar]