Abstract
Background:
Migraine is one of the most common and debilitating neurological problems. Although numerous preventive drugs are used to treat migraine, their complications are unavoidable. Application of herbal medicine, especially well-known medicinal plants, to treatment of chronic diseases, like migraine, could be effective. Coriandrum sativum L. (C. sativum) fruit is one of the most commonly prescribed herbs in Persian medicine, which has been used to treat headache.
Objectives:
This study was designed to evaluate the effects of C. sativum syrup on duration, severity and frequency of migraine.
Patients and Methods:
A total of 68 migraineurs, who had the eligibility criteria, according to international headache society diagnostic criteria, were randomly assigned to intervention group (n = 34) or control group (n = 34). In addition to 500 mg of sodium valproate per day, in intervention group, they received 15 mL of Coriander fruit syrup and 15 mL of placebo syrup, in control group, three times a day, during a month. The subjects were followed for clinical efficacy at weeks 1, 2, 3 and 4. The number of migraine attacks per week, as well as the duration and severity of attacks, were evaluated.
Results:
Of 68 patients randomized, 66 were included in analysis. The generalized estimating equations analysis showed that the Coriander fruit syrup decreased duration, severity and frequency of migraine, in the intervention group (P < 0.001). To be more precise, the mean migraine duration, severity and frequency, in the intervention group, were 5.7 hours, 3.65 units and about 50% less than control group, respectively.
Conclusions:
Results of this study showed that C. sativum fruit is efficient in reduction of the duration and frequency of migraine attacks and in diminishing pain degree.
Keywords: Migraine Disorders, Coriandrum, Herbal Medicine, Headache
1. Background
Migraine is a chronic and debilitating neurological disorder, with a significant burden on the migraineurs and the society (1). It is the third most common disorder, as well as the seventh highest specific reason of disability, throughout the world (2). Prevalence rate of migraine is various, in different studies (3), and is estimated between 10 to 33% in women and five to 13.3% in men (4-7). Also, the intensity of pain, in approximately 90% of patients, is moderate to severe (8). Numerous preventive treatments are used to reduce the frequency and severity of pain. Although tricyclic antidepressants, anticonvulsants and beta-blockers are used widely (9, 10), their complications like constipation (11), tremor, weight gain (12), depression and orthostatic hypotension (13) are unavoidable and they are the main difficulties in preventive treatment of migraine (14).
The world health organization has been encouraging countries to employ the traditional medicine, in unresolved diseases (15). Therefore, there is a rising propensity toward application of herbal medicine, in chronic diseases (16). In the Persian medicine, treatment of neurological disorders, like headache, has been described in detail and medicinal plants have been applied to treatment of headache (17). Coriander [Coriandrum sativum L. (C. sativum)] fruit is one of the most commonly prescribed herbs in Persian medicine, which has been used to treat headache (18), despite curing other diseases, like anxiety and insomnia (19-21).
C. sativum is a species belonging to the Apiaceae (Umbelliferae) family, whose habitat is the Middle Eastern and Mediterranean regions (22). It is an annual herb, with small spherical fruits (23). Several of its proven effects are antianxiety (19), antioxidant (24) and antibacterial activities (25). Also, it has potential antitumor effects (26).
2. Objectives
Since there was no available clinical evidence, with regard to its effect on migraine headache, in human, this study was designed to evaluate the effect of Coriander fruit on migraine.
3. Patients and Methods
3.1. Study Design
This study was designed as a prospective, two-arm, randomized, triple-blind, placebo-controlled trial and used a parallel design. Sixty-eight patients were randomly assigned into two groups of intervention (n = 34) and control (n = 34). The study sample was calculated from the formula suggested by Diggle et al. (27), for comparing a continuous response between two parallel groups, in a longitudinal study:
| (1) |
With α = 0.05, β = 0.2 and m = 5 (number of measurements for each person under study) and considering the results of a pilot study, which led to ρ = 0.4 (process correlation), d = 1.5 (least significant difference to be detected for severity of pain) and σ2 = 9 (process variance), at least a sample size of 33 was needed for each study group. Randomization was achieved using the random permuted blocks of size 4, in a ratio of 1:1. As a triple blind style, the patients, physicians and data analyst were not aware of the treatment groups. Initially, the protocol was approved by the ethics committee of the Shahid Beheshti university of medical sciences (approval number: 400/876). Furthermore, it was registered in the Iranian registry of clinical trials and received the registration number: IRCT 2012122511876N1. At first, subjects were informed about the aim of the study, and, before recruiting, they signed an informed consent form. In addition to 500 mg of sodium valproate per day, the patients received either 15 mL of coriander fruit syrup or 15 mL of placebo syrup, three times a day, for a month, according to the code provided by the department of traditional pharmacy in the Tehran university of medical sciences, Tehran, Iran. The subjects were followed at weeks 1, 2, 3 and 4. However, all subjects were free to withdraw at any moment during the intervention. The sealed codes were kept by the study pharmacist and were not decoded until all the experimental process of the last patient was completed and statistical analysis was done.
3.2. Study Population
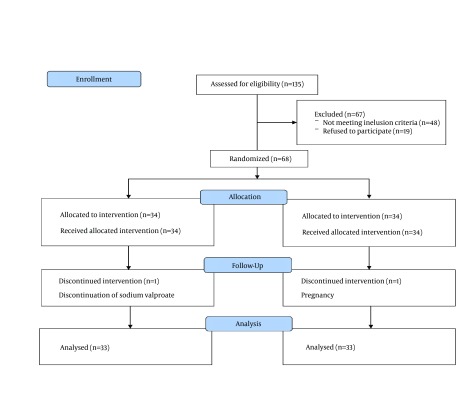
In general, of 135 patients with migraine, who referred (from 14 January to 28 September, 2013) to the neurology clinic of Shohadaye-Tajrish hospital, Tehran, Iran, 87 patients with inclusion criteria were considered and 48 persons were excluded. Among these 87 patients, 19 individuals refused participation and 68 individuals were finally recruited, to this study. A neurologist examined all the patients and assessed the inclusion and exclusion criteria, based on the study protocol.
All patients were adults, aged 18 - 45 years old, who had migraine according to the international headache society diagnostic criteria, for at least 1 year, with at least four attacks per month. They were evaluated by the Beck inventory, in order to rule out depression. Also, pregnant or lactating females were not allowed to attend. Patients with serious concomitant medical problems and concurrent treatment (herbal and chemical medicine) were not included in the study. Females, with a positive test for pregnancy or the decision to become pregnant, were excluded from the intervention. Other exclusion criteria were serious medical problems, such as cardiac disease or diabetes. Also, patients that had other headaches, like secondary headache, daily and analgesic overuse headache, with migraine, were excluded.
3.3. Plant Material
Dried C. sativum fruits were purchased from a local herbal store, in Tehran bazaar, Iran, in 2012. They were authenticated in the faculty of pharmacy, Tehran university of medical sciences, Tehran, Iran. Afterwards, for future reference, a voucher specimen (#PMP-308) was deposited at the herbarium of the faculty of pharmacy, Tehran university of medical sciences, Tehran, Iran. The dried C. sativum fruits were used for extraction of total essential oil, using a Clevenger-type apparatus and yielded 0.5 mL percent (v/w) of dried fruits. Analysis of total essential oil, using gas chromatography (GC) and GC-mass spectrometry (GC-MS) methods, showed several major component, as linalool (82%), geraniol (6%), α-pinene (5%), β-pinene (3%) and thymol (1.48%). Total evaporated ethanol extract of C. sativum fruits was used for preparation of syrup, while each 5 mL of syrup contained 100 mg evaporated ethanol extract, in the base of sucrose pharmacopoeial syrup. The placebo was prepared in the same appearance and packaging, on pharmacopoeia syrup formula, without C. sativum fruits extract. Finally, the medication was supplied in bottles of 250 mL, containing either drug or placebo.
3.4. Intervention
In addition to 500 mg/day sodium valproate, the participants were given bottles of either coriander or placebo syrup. Dosage of syrup was 15 mL, three times a day, monthly. To make sure of the compliance of patients, they were asked to return the given bottles upon every follow-up visit.
3.5. Main Outcomes and Other Registered Characteristics
Initially, the basic characteristics and demographic information were registered for each patient. In addition, the baseline frequency, duration and severity of migraine were recorded. To do this, the patients were asked to express the frequency of attacks and mean duration of pain, in a week. All statements were added to the patients’ files. Then, the mean severity of pain was evaluated, by a ten-point visual analog scale (VAS). Eventually, the patients were requested to write down the number of their migraine attacks, per week, as well as the duration and severity of each attack, separately. At the end of each week, patients were referring to the neurology clinic to report the requested items.
3.6. Statistical Analysis
For describing the data, the frequency distributions and percent were reported for qualitative variables. In addition, quantitative variables were described using the mean (and SD) or median (and interquartile range). In univariate analyses, comparison of demographic characteristics and baseline variables, of the patients in the two groups, were performed by the chi-square test and independent samples t-test (or Mann-Whitney test, for non-normal variables). Moreover, the marginal models, with identity link function for duration and severity, and log link, for frequency, as well as the generalized estimating equations (GEE) approach, were used to assess the effect of intervention on duration, severity and frequency of migraine, during the time, adjusting for demographic characteristics and baseline variables of the patients. The SPSS software version 16.0 (SPSS Inc. Chicago, IL, USA) was utilized for data analysis and P < 0.05 were considered statistically significant.
4. Results
Our study was started with 135 migraineurs and ended with 33 patients, in the intervention group, and 33 patients, in the control group. The subjects with uncompleted therapy were equal, in both groups. The reason for dropping out, in one of them, was due to pregnancy. Another participant was excluded from the study because of discontinuation of sodium valproate, in the mid-intervention. Figure 1 shows the flowchart of the study. The mean ± SD age of participants was 32.06 ± 7.37. Among them, 51 persons (77.3%) were female and 15 persons (22.7%) were male. Table 1 compares the characteristics of the subjects, in the two groups. The descriptive statistics, for the outcome variables, represented a decreasing trend over time, with different slope for two groups, especially regarding migraine severity. Table 2 displays the trend of the outcome variables under study, at different times.
Figure 1. Flowchart of the Study.
Table 1. Demographic Characteristics and Baseline Variables of the Patients in the Two Groupsa.
| Variable | Intervention | Control | P Value |
|---|---|---|---|
| Gender | .769 | ||
| Female | 26 (78.8) | 25 (75.8) | |
| Male | 7 (21.2) | 8 (24.2) | |
| Marital status | .125 | ||
| Single | 9 (27.3) | 15 (45.5) | |
| Married | 24 (72.7) | 18 (54.5) | |
| Type of migraine | .741 | ||
| Without aura | 27 (81.8) | 28 (84.8) | |
| With aura | 6 (18.2) | 5 (15.2) | |
| Age, y | 33.09 ± 7.50 | 31.03 ± 7.20 | .259b |
| Baseline duration | 24.0 (14.0)c | 10.0 (18.0)c | .019d |
| Baseline severity | 8.42 ± 1.17 | 6.63 ± 2.01 | < .001b |
| Baseline frequency | 3.0 (2.0)c | 2 (2.0)c | .149d |
aData are presented as No. (%) or mean ± SD.
bFrom independent samples t-test.
cMedian (IQR).
dFrom Mann-Whitney test.
Table 2. Descriptive Statistics for Trend of Outcomes During the Time in Two Groupsa.
| Time | Intervention Group | Control Group | ||||
|---|---|---|---|---|---|---|
| Duration | Severity | Frequency | Duration | Severity | Frequency | |
| First week | 8.03 ± 0.85 | 5.09 ± 1.72 | 1.79 ± 0.86 | 10.70 ± 7.88 | 5.60 ± 1.81 | 2.12 ± 0.96 |
| Second week | 3.57 ± 2.53 | 2.73 ± 1.56 | 1.27 ± 0.71 | 8.40 ± 5.24 | 4.99 ± 1.89 | 1.85 ± 0.79 |
| Third week | 0.98 ± 1.27 | 0.80 ± 0.86 | 0.60 ± 0.55 | 6.84 ± 4.80 | 4.09 ± 2.40 | 1.30 ± 0.77 |
| Fourth week | 0.15 ± 0.34 | 0.21 ± 0.48 | 0.18 ± 0.39 | 4.17 ± 3.74 | 3.70 ± 2.53 | 1.03 ± 0.73 |
aData are presented as mean ± SD.
Our modeling results, based on GEE analysis, revealed that the duration, severity and frequency of migraine were significantly different between intervention and control groups (P < 0.001), adjusting for demographic characteristics and baseline variables. To be more precise, the estimate of the group variable, for frequency of migraine, in Table 3, can be interpreted using the Exp (b) column. The Exp (b) = 0.509 tells us that the rate of migraine attacks, in the intervention group, was about half of this rate in the control group. Moreover, the obtained estimate of -5.70 for group variable for duration of pain demonstrated that the mean migraine headache duration, in the intervention group, was 5.7 hours less than in control group. Finally, according to the estimation of the group variable (in the same table) for severity of pain, the mean migraine severity, in the intervention group, was about 3.65 units (based on VAS scale) less than the control group.
Table 3. Marginal Modeling (Generalized Estimating Equations Analysis) Analysis) Results for Evaluating the Effect of Treatment on Frequency, Duration and Severity of Migrainez.
| Response Parameters | ba | SE (b)b | P Value | Exp (b)c |
|---|---|---|---|---|
| Frequency | ||||
| Group (intervention/control) | -0.675 | 0.68 | < .001 | 0.509 |
| Gender (female/male) | 0.158 | 0.074 | .034 | 1.171 |
| Type (without aura/with aura) | 0.081 | 0.079 | .311 | 1.084 |
| Marriage (single/married) | -0.019 | 0.084 | .824 | 0.981 |
| Baseline frequency | 0.389 | 0.028 | < .001 | 1.476 |
| Age | 0.002 | 0.008 | .785 | 1.002 |
| Onset | 0.015 | 0.013 | .265 | 1.015 |
| Time | -0.376 | 0.032 | < .001 | 0.687 |
| Duration | ||||
| Group (intervention/control) | -5.70 | 0.72 | < .001 | NA |
| Gender (female/male) | 0.988 | 0.81 | .225 | NA |
| Type (without aura/with aura) | -0.657 | 1.049 | .531 | NA |
| Marriage (single/married) | -0.834 | 0.927 | .368 | NA |
| Baseline duration | 0.127 | 0.029 | < .001 | NA |
| Age | -0.049 | 0.088 | .578 | NA |
| Onset | 0.181 | 0.172 | .293 | NA |
| Time | -2.390 | 0.258 | < .001 | NA |
| Severity | ||||
| Group (intervention/control) | -3.646 | 0.269 | < .001 | NA |
| Gender (female/male) | 0.501 | 0.232 | .031 | NA |
| Type (without aura/with aura) | -0.009 | 0.316 | .978 | NA |
| Marriage (single/married) | 0.024 | 0.315 | .940 | NA |
| Baseline severity | 0.697 | 0.027 | < .001 | NA |
| Age | -0.028 | 0.028 | .309 | NA |
| Onset | 0.056 | 0.057 | .330 | NA |
| Time | -1.144 | 0.091 | < .001 | NA |
zAbbreviation: NA, not available.
aEstimate of the model parameter.
bStandard error of the estimate.
cRate ratio.
There was no report of the events leading to discontinuation of study, or any experience of adverse effects. from the intervention. Instead, several patients declared the desired effects, such as increase of appetite in two persons, sleep quality improvement, in one patient, and lack of nausea, for six patients. Also, four patients had headache (however, not the pulsating type), and two patients got rid of constipation, after 2 weeks.
5. Discussion
The aim of this trial was to evaluate the efficacy of C. sativum on migraine headache. Therefore, concomitant consumption of coriander syrup, with sodium valproate, in the intervention group, was designed in comparison with control group, who received sodium valproate and placebo syrup. Previous animal studies have already shown analgesic and anti-inflammatory activity of C. sativum fruits. Indeed, Pathan et al. demonstrated that injection of 50 - 200 mg/kg of coriander fruit, in mice, has central analgesic activity (28). In consistence with the previous study, results of formalin test on mice, which is used in neurogenic and inflammatory pain researches, indicated that coriander extract has dose-dependent analgesic effect and it can delay both neurogenic and inflammatory phase of pain (29). Additionally, results of a study on mice illustrated that linalool is effective in chronic pain, via the inhibition of evoked inflammatory mediators (30). In our study, several major components, which were obtained from the analysis of coriander, were linalool (82%), geranial (6%), α-pinene (5%), β-pinene (3%) and thymol (1.48%). Also, linalool is one of the components of lamiaceae family and various investigations have confirmed the analgesic and anti-inflammatory effects of several species, belonging to this family. The study of Hajhashemi et al. on mice and rats, demonstrated that the polyphenolic fraction and essential oil of Lavandula angustifolia have significant analgesic activity; moreover, its essential oil possesses anti-inflammatory effect (31). Since linalool is the main component of coriander (22) and neurogenic inflammation is one of the numerous mechanism, which have been hypothesized to migraine (32, 33), perhaps it can be concluded that influence of coriander on migraine is secondary to linalool. Since the severity and frequency of attacks were reduced significantly, in the intervention group, compared with the control group, one may be conclude that coriander syrup would be effective in the prophylactic treatment of migraine. Therefore, we suggest other trials for the evaluation of this aim.
Although this trial was unique in its field, with no observed and recorded adverse events, its limitations should be mentioned. Firstly, the subjects received syrup, only for one month; therefore, we could not comment on any long-term efficacy of coriander syrup. Also, the patients were not followed-up after finishing the study, and, therefore, the long-lasting effects are not clear to us. Undoubtedly, the results of long-term studies, with a larger sample size, would be more generalizable and efficient. Also, the follow-up period would specify durability of drug effects. Finally, more assessments to identify the mechanism involved in the decrease of pain are suggested.
Overall, according to the findings of this investigation, it can be concluded that C. sativum fruit has short-term considerable effects on migraine, and it is efficient in reduction the duration and frequency of migraine attacks and in diminishing pain degree, in a month. Therefore, its use, as a medicine, to treat migraine, is very probable.
Acknowledgments
This article is based on PhD thesis of Dr. Zahra Ghorbanifar (Number: 133), department of traditional medicine, school of traditional medicine, Shahid Beheshti university of medical sciences, Tehran, Iran. We thank all the study participants for their participation. The authors gratefully acknowledge the help of Dr. Lawrence George and Dr. Elders Greg (regional family practice, Baxter regional medical center, Baxter, UK) for the English editing of the article.
Footnotes
Authors’ Contribution:Study concept and design: Zahra Ghorbanifar, Hosein Delavar Kasmaei, Hossein Rezaeizadeh and Farid Zayeri; acquisition of data: Zahra Ghorbanifar and Hosein Delavar Kasmaei; analysis and interpretation of data: Zahra Ghorbanifar and Farid Zayeri; drafting of the manuscript: Zahra Ghorbanifar, Seyed Hamid Kamali, Ali Ghobadi and Hossein Rezaeizadeh; critical revision of the manuscript for important intellectual content: Zahra Ghorbanifar, Hosein Delavar Kasmaei, Hossein Rezaeizadeh, Seyed Hamid Kamali, Farid Zayeri and Ali Ghobadi; statistical analysis: Farid Zayeri; technical and material support: Gholamreza Amin, Ali Ghobadi and Zohreh Mirzaei; study supervision: Hosein Delavar Kasmaei, Bagher Minaei and Gholamreza Amin.
References
- 1.Krymchantowski AV, da Cunha Jevoux C, Bigal ME. Topiramate plus nortriptyline in the preventive treatment of migraine: a controlled study for nonresponders. J Headache Pain. 2012;13(1):53–9. doi: 10.1007/s10194-011-0395-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu R, Yu S, He M, Zhao G, Yang X, Qiao X, et al. Health-care utilization for primary headache disorders in China: a population-based door-to-door survey. J Headache Pain. 2013;14:47. doi: 10.1186/1129-2377-14-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oztora S, Korkmaz O, Dagdeviren N, Celik Y, Caylan A, Top MS, et al. Migraine headaches among university students using ID Migraine test as a screening tool. BMC Neurol. 2011;11:103. doi: 10.1186/1471-2377-11-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lipton RB, Serrano D, Holland S, Fanning KM, Reed ML, Buse DC. Barriers to the diagnosis and treatment of migraine: effects of sex, income, and headache features. Headache. 2013;53(1):81–92. doi: 10.1111/j.1526-4610.2012.02265.x. [DOI] [PubMed] [Google Scholar]
- 5.Diener HC, Montagna P, Gacs G, Lyczak P, Schumann G, Zoller B, et al. Efficacy and tolerability of diclofenac potassium sachets in migraine: a randomized, double-blind, cross-over study in comparison with diclofenac potassium tablets and placebo. Cephalalgia. 2006;26(5):537–47. doi: 10.1111/j.1468-2982.2005.01064.x. [DOI] [PubMed] [Google Scholar]
- 6.Shahbeigi S, Fereshtehnejad SM, Mohammadi N, Golmakani MM, Tadayyon S, Jalilzadeh G, et al. Epidemiology of headaches in Tehran urban area: a population-based cross-sectional study in district 8, year 2010. Neurol Sci. 2013;34(7):1157–66. doi: 10.1007/s10072-012-1200-0. [DOI] [PubMed] [Google Scholar]
- 7.Balaban H, Semiz M, Senturk IA, Kavakci O, Cinar Z, Dikici A, et al. Migraine prevalence, alexithymia, and post-traumatic stress disorder among medical students in Turkey. J Headache Pain. 2012;13(6):459–67. doi: 10.1007/s10194-012-0452-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lipton RB, Bigal ME, Diamond M, Freitag F, Reed ML, Stewart WF, et al. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007;68(5):343–9. doi: 10.1212/01.wnl.0000252808.97649.21. [DOI] [PubMed] [Google Scholar]
- 9.Barbanti P, Aurilia C, Egeo G, Fofi L. Migraine prophylaxis: what is new and what we need? Neurol Sci. 2011;32 Suppl 1:S111–5. doi: 10.1007/s10072-011-0526-3. [DOI] [PubMed] [Google Scholar]
- 10.Afshinmajd S, Davati A, Akbari F. The effects of body mass index on the treatment of the patients with migraine headaches. Iran J Neurol. 2011;10(3-4):35–8. [PMC free article] [PubMed] [Google Scholar]
- 11.Uher R, Farmer A, Henigsberg N, Rietschel M, Mors O, Maier W, et al. Adverse reactions to antidepressants. Br J Psychiatry. 2009;195(3):202–10. doi: 10.1192/bjp.bp.108.061960. [DOI] [PubMed] [Google Scholar]
- 12.Ramakrishnappa SK, Belhekar MN. Serum drug level-related sodium valproate-induced hair loss. Indian J Pharmacol. 2013;45(2):187–8. doi: 10.4103/0253-7613.108315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miller S. The acute and preventative treatment of episodic migraine. Ann Indian Acad Neurol. 2012;15(Suppl 1):S33–9. doi: 10.4103/0972-2327.99998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tajmirriahi M, Sohelipour M, Basiri K, Shaygannejad V, Ghorbani A, Saadatnia M. The effects of sodium valproate with fish oil supplementation or alone in migraine prevention: A randomized single-blind clinical trial. Iran J Neurol. 2012;11(1):21–4. [PMC free article] [PubMed] [Google Scholar]
- 15.Pal SK, Shukla Y. Herbal medicine: current status and the future. Asian Pac J Cancer Prev. 2003;4(4):281–8. [PubMed] [Google Scholar]
- 16.Kamali SH, Khalaj AR, Hasani-Ranjbar S, Esfehani MM, Kamalinejad M, Soheil O, et al. Efficacy of 'Itrifal Saghir', a combination of three medicinal plants in the treatment of obesity; A randomized controlled trial. Daru. 2012;20(1):33. doi: 10.1186/2008-2231-20-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hamedi A, Zarshenas MM, Sohrabpour M, Zargaran A. Herbal medicinal oils in traditional Persian medicine. Pharm Biol. 2013;51(9):1208–18. doi: 10.3109/13880209.2013.777462. [DOI] [PubMed] [Google Scholar]
- 18.Ibn-e-Sina AH. Al-Qanun fit-tib [The Canon of Medicine] (research of ebrahim shamsedine). Beirut, Lebanon: Alaalami Beirut library Press; 2005. [Google Scholar]
- 19.Mahendra P, Bisht S. Anti-anxiety activity of Coriandrum sativum assessed using different experimental anxiety models. Indian J Pharmacol. 2011;43(5):574–7. doi: 10.4103/0253-7613.84975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rakhshandeh H, Sadeghnia HR, Ghorbani A. Sleep-prolonging effect of Coriandrum sativum hydro-alcoholic extract in mice. Nat Prod Res. 2012;26(22):2095–8. doi: 10.1080/14786419.2011.613388. [DOI] [PubMed] [Google Scholar]
- 21.Emamghoreishi M, Khasaki M, Aazam MF. Coriandrum sativum: evaluation of its anxiolytic effect in the elevated plus-maze. J Ethnopharmacol. 2005;96(3):365–70. doi: 10.1016/j.jep.2004.06.022. [DOI] [PubMed] [Google Scholar]
- 22.Burdock GA, Carabin IG. Safety assessment of coriander (Coriandrum sativum L.) essential oil as a food ingredient. Food Chem Toxicol. 2009;47(1):22–34. doi: 10.1016/j.fct.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 23.Sahib NG, Anwar F, Gilani AH, Hamid AA, Saari N, Alkharfy KM. Coriander (Coriandrum sativum L.): a potential source of high-value components for functional foods and nutraceuticals--a review. Phytother Res. 2013;27(10):1439–56. doi: 10.1002/ptr.4897. [DOI] [PubMed] [Google Scholar]
- 24.Tang EL, Rajarajeswaran J, Fung SY, Kanthimathi MS. Antioxidant activity of Coriandrum sativum and protection against DNA damage and cancer cell migration. BMC Complement Altern Med. 2013;13:347. doi: 10.1186/1472-6882-13-347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lo Cantore P, Iacobellis NS, De Marco A, Capasso F, Senatore F. Antibacterial activity of Coriandrum sativum L. and Foeniculum vulgare Miller Var. vulgare (Miller) essential oils. J Agric Food Chem. 2004;52(26):7862–6. doi: 10.1021/jf0493122. [DOI] [PubMed] [Google Scholar]
- 26.Gomez-Flores R, Hernandez-Martinez H, Tamez-Guerra P, Tamez-Guerra R, Quintanilla-Licea R, Monreal-Cuevas E. Antitumor and immunomodulating potential of Coriandrum sativum, Piper nigrum and Cinnamomum zeylanicum. J Natur Produc. 2010;3:54–63. [Google Scholar]
- 27.Diggle P, Heagerty P, Liang KY, Zeger S. Analysis of longitudinal data. second ed. New York: Oxford University Press; 2002. [Google Scholar]
- 28.Pathan AR, Kothawade KA, Logade MN. Anxiolytic and analgesic effect of seeds of Coriandrum sativum Linn. Inte J Res Pham Chem. 2011;1(4):1087–99. [Google Scholar]
- 29.Taherian AA, Vafaei AA, Ameri J. Opiate System Mediate the Antinociceptive Effects of Coriandrum sativum in Mice. Iran J Pharm Res. 2012;11(2):679–88. [PMC free article] [PubMed] [Google Scholar]
- 30.Batista PA, Werner MF, Oliveira EC, Burgos L, Pereira P, Brum LF, et al. The antinociceptive effect of (-)-linalool in models of chronic inflammatory and neuropathic hypersensitivity in mice. J Pain. 2010;11(11):1222–9. doi: 10.1016/j.jpain.2010.02.022. [DOI] [PubMed] [Google Scholar]
- 31.Hajhashemi V, Ghannadi A, Sharif B. Anti-inflammatory and analgesic properties of the leaf extracts and essential oil of Lavandula angustifolia Mill. J Ethnopharmacol. 2003;89(1):67–71. doi: 10.1016/s0378-8741(03)00234-4. [DOI] [PubMed] [Google Scholar]
- 32.Benemei S, De Cesaris F, Fusi C, Rossi E, Lupi C, Geppetti P. TRPA1 and other TRP channels in migraine. J Headache Pain. 2013;14:71. doi: 10.1186/1129-2377-14-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bernstein C, Burstein R. Sensitization of the trigeminovascular pathway: perspective and implications to migraine pathophysiology. J Clin Neurol. 2012;8(2):89–99. doi: 10.3988/jcn.2012.8.2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]