Abstract
Background
After endoscopic sinus surgery (ESS), endoscopy is used to gauge surgical success and clinical outcomes. Prior studies have not examined this topic prospectively using validated outcome metrics across multiple institutions.
Methods
A multi-institutional, prospective study of patients with chronic rhinosinusitis (CRS) who underwent ESS completed the SinoNasal Outcome Test (SNOT-22), missed productivity and medication usage questionnaires 6 months postoperatively. Lund-Kennedy endoscopy scoring (LKES) was performed with reviewers blinded to patient-reported data. A control cohort of non-CRS patients was recruited for comparison.
Results
Complete data was available on 183 CRS patients and 48 non-CRS control patients. Approximately 50% of patients achieve perfect or near perfect endoscopy (LKES 0-2) after ESS. Postoperative endoscopy correlated with total SNOT-22 scores (r=0.278, p<0.001), with the strongest correlations to rhinologic and extra-nasal subdomains in the nasal polyp cohort. Improved postoperative endoscopy was associated with decreased antibiotic and oral steroid usage, but had little association with missed productivity. Among patients who achieved near perfect postoperative endoscopy, those with nasal polyps had SNOT-22 scores that were similar to non-CRS control patients (mean SNOT-22 17.7 and 16.3, respectively). However, CRS patients without nasal polyps remained more symptomatic than non-CRS controls and CRS with nasal polyp patients despite nearly perfect endoscopy (mean SNOT-22 21.6).
Conclusions
Postoperative endoscopy correlates with SNOT-22 and medication usage in CRS patients. Polyp patients who achieve near perfect endoscopy have similar symptoms to healthy controls, however, non-polyp patients with near perfect endoscopy still have rhinologic and extra-nasal symptoms that are worse than healthy controls.
Keywords: sinusitis, endoscopy, quality of life, staging, clinical outcomes
Introduction
After endoscopic sinus surgery (ESS) most otorhinolaryngologists use endoscopy to gauge surgical success, determine patient response to adjuvant medical therapy, and discern if any postoperative symptoms are due to sinogenic causes. Endoscopy may also predict the need for revision surgery1. Prior reports on the correlation between postoperative endoscopy and quality of life (QoL) have been conflicting. Several failed to find any correlation between postoperative endoscopy score as measured by the traditional Lund Kennedy Endoscopic Scale (LKES) and total sinus-specific QoL scores2–5. Some correlations become apparent when focusing upon nasal-specific symptom scores3–9, however, it is unclear if these correlations are broadly applicable or are dependent upon polyp status. Others have found correlations between improvements in postoperative endoscopy and sinus specific QoL10; but when faced with a patient in the postoperative period, it may be difficult to recall their preoperative endoscopic score and determine the degree of improvement.
Modifications of the traditional LKES and entirely new endoscopic staging systems have been proposed in attempts to improve correlation with sinus specific symptom scores5,7,9. Most of these modifications eliminate crusting and scarring and may modify assessment of mucosal inflammation and discharge. In general, most of these modifications improve correlation with rhinologic symptoms but may not correlate with systemic manifestations of CRS.
Unfortunately, these issues have not been studied in a multi-institutional, prospective fashion, using validated metrics, and multiple questions remain: How often are we able to achieve a perfect endoscopic appearance? How healthy does a postoperative endoscopic cavity need to be and what does this mean for patient outcomes and medication usage? The first goal of this study was to prospectively follow a large number of patients undergoing ESS by multiple surgeons and determine the distribution of postoperative endoscopy scores. Second, we wanted to determine the correlation between postoperative endoscopy and clinical outcomes, including overall QoL scores, specific symptom subdomain scores, medication usage and productivity. Third, we wanted to compare outcomes in CRS patients who had near perfect postoperative endoscopy with non-CRS control patients to determine if there were persistent symptoms despite a nearly perfect endoscopic exam. Finally, we wished to examine whether modifications of traditional endoscopic scoring improved correlations.
Methods
Study patients
Participants with CRS were prospectively recruited from rhinologic practices at 4 tertiary medical centers across North America (Medical University of South Carolina, Stanford University, University of Calgary, and Oregon Health & Science University) under IRB approval (Pro 12409). All patients had CRS as defined by consensus criteria, including 3 months of at least 2 cardinal symptoms and evidence of inflammation on sinonasal endoscopy and CT scan11,12. All patients had ongoing symptoms after initial attempts at medical treatment, including broad spectrum or culture-directed antibiotics, oral steroids, and topical steroids. Importantly, this cohort does not include those patients with CRS whose symptoms resolve with initial medical therapy. Also excluded were patients with cystic fibrosis, ciliary dyskinesia or other autoimmune disorders, as these are discrete disorders with unique pathophysiologies. Fungus balls or mucoceles were similarly excluded since they are well identified clinical entities with straightforward treatment outcomes.
Research coordinators administered questionnaires that assessed demographic information, medical comorbidities, medication usage over the preceding 90 days, and productivity loss (work days missed in the preceding 90 days). Sinus-specific QoL was assessed using the 22-item Sinonasal Outcome Test (SNOT-22)13. For each subject, CT scans were reviewed in blinded fashion and graded according to Lund-Mackay staging system. Sinonasal endoscopy was performed and grading according to the Lund-Kennedy system with reviewers blinded to patient-reported clinical data. Modified LKES5, eliminating crust and scar scores, was also recorded.
Control participants were recruited at Medical University of South Carolina from spouses, family members and friends of participants with CRS in order to enhance likelihood of having a control cohort matched for age, gender and environmental exposures under IRB approval (Pro 16334). Control subjects were excluded if they had any history of chronic or recurrent sinusitis. All control subjects completed basic demographic information as well as the SNOT-22 survey.
Statistical analysis
Statistical analyses were performed using a commercially available software application (SPSS v.22, IBM Corporation, Armonk, NY). Descriptive statistics are reported using means, standard deviations, and frequency. The mean clinically important difference (MCID) of the SNOT-22 was defined at a change of 8.9 or greater from preoperative SNOT-22 score14. Pearson correlations were used to evaluate linear associations between continuous study variables. Analysis of variance (ANOVA) and subsequent Bonferroni multiple comparison testing was performed with more than two continuous variables. Pearson chi-square tests were used to test proportions and exact tests were used when cells had an expected count of less than 5. Numeric discrete variables were compared using Mann-Whitney U Tests between two groups and Kruskal-Wallis between more than two groups. Comparisons of paired proportions were done using McNemar’s test. All tests were assessed using a significance level of 0.05.
Results
Baseline demographic characteristics
Six month follow up was available on 183 CRS patients with a mean age of 51.5 ± 14.9 years. Just over half (52%) were female. Racial breakdown was white (85%), African American (4%), Asian (3%) and other (8%). Forty percent of patients had CRSwNP and had undergone more prior surgeries than CRSsNP patients. Demographics for all CRS and non-CRS control patients are listed in Table 1. Control subjects were similar in age and gender to CRS cohorts, but did have more African Americans, fewer Hispanics and as expected, a lower incidence of asthma, aspirin intolerance and atopy.
Table 1.
Demographics of patient cohorts
| CRSsNP (n=110) | CRSwNP (n=73) | Control (n=48) | p | |||||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | N (%) | Mean (SD) | N (%) | Mean (SD) | N (%) | |||
| Age (years) | 50.4 (14.4) | 53.2 (15.7) | 55.2(18.5) | 0.182 | ||||
| Gender | Female | 63 (57.3%) | 33 (45.2%) | 17 (35.4%) | 0.089 | |||
| Male | 47 (42.7%) | 40 (54.8%) | 31 (64.6%) | |||||
| Race | African-American | 2 (1.8%) | 5 (6.8%) | 12 (25%) | <0.001 | |||
| White | 97 (88.2%) | 59 (80.8%) | 36 (75%) | |||||
| Asian | 2 (1.8%) | 4 (5.5%) | 0 (0%) | |||||
| Other | 9 (8.2%) | 5 (6.8%) | 0 (0%) | |||||
| Ethnicity (Hispanic/Latino) | 5 (4.5%) | 6 (8.2%) | 0 (0%) | <0.001 | ||||
| Asthma | 29 (26.4%) | 41 (56.2%) | 3 (6.3%) | <0.001 | ||||
| ASA Intolerance | 3 (2.7%) | 13 (17.8%) | 0 (0%) | <0.001 | ||||
| Allergy By Testing | 42 (38.2%) | 33 (45.2%) | 10 (20.8%) | 0.023 | ||||
| COPD | 3 (2.7%) | 5 (6.8%) | 0 (0%) | 0.165 | ||||
| Depression | 18 (16.4%) | 8 (11.0%) | 2 (4.2%) | 0.091 | ||||
| Fibromyalgia | 6 (5.5%) | 2 (2.7%) | 1 (2.1%) | 0.674 | ||||
| OSA By Testing | 10 (10.4%) | 3 (5.0%) | 4 (8.3%) | 0.550 | ||||
| Prior sinus surgeries (N) | 0.8 (1.4) | 1.2 (1.2) | NA | NA | 0.030 | |||
CRSsNP = Chronic rhinosinusitis without nasal polyps; CRSwNP = Chronic rhinosinusitis with nasal polyps; ASA = Aspirin; COPD = Chronic obstructive pulmonary disease; OSA = Obstructive sleep apnea
Postoperative endoscopy
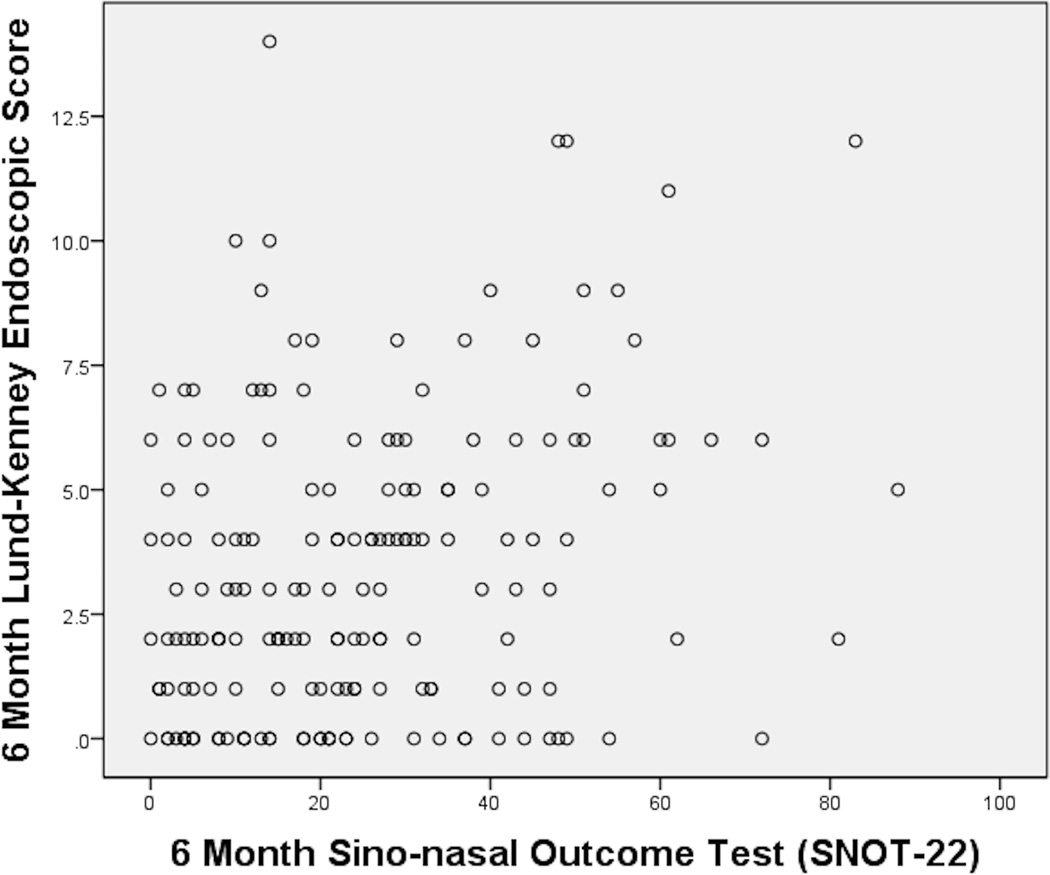
For the overall cohort, baseline LKES was 6.6 ± 3.9 and baseline total SNOT-22 was 53.2 ± 19.3. Mean 6 month LKES was 3.4 ± 3.0 and mean 6 month SNOT-22 score was 24.7 ± 18.7. Patients fell evenly into 4 endoscopic categories based upon 6 month postoperative LKES, with approximately 25% each with perfect endoscopy (LKES 0), mild endoscopy (LKES 1–2), moderate endoscopy (LKES 3–5) and poor endoscopy (LKES ≥ 6). Mean SNOT-22 scores were worse in the poor endoscopy group when compared to those with LKES of 0 or 1–2. Approximately 85% of patients experienced an MCID across all endoscopy groups (no statistical difference, Table 2). The perfect endoscopy group actually had slightly worse SNOT-22 scores than the mild endoscopy group (LKES 1–2). However, these differences were not statistically significant, therefore we collapsed these 2 groups from this point forward for analysis and labeled them “near perfect” endoscopy. This near perfect group had a mean SNOT-22 of 20.4 ± 16.8 which was still better than the poor endoscopy group. Overall, 6 month LKES correlated with total SNOT-22 at 6 months (Figure 1).
Table 2.
Distribution of postoperative endoscopy and outcomes
| Endoscopy Score |
N (%) | Mean SNOT-22 (SD) | MCID (%) |
|---|---|---|---|
| 0 | 40 (22%) | 20.9 (17.4) | 83 |
| 1–2 | 48 (26%) | 20.0 (16.5) | 88 |
| 3–5 | 51 (28%) | 25.5 (16.9) | 82 |
| ≥6 | 44 (24%) | 32.4 (21.9) | 86 |
ANOVA demonstrated differences in mean SNOT-22 scores among groups. (p= 0.006) Post hoc Bonferroni demonstrated endoscopy groups with scores of 0 or 1–2 were significantly different from those with endoscopy ≥6 (p≤0.027). There were no differences in percent experiencing MCID among the four groups (p=0.703).
SNOT-22 = SinoNasal Outcomes Test-22; MCID = Minimal Clinically Important Difference
Figure 1.
6 month total SNOT-22 correlates with 6 month postoperative LKES (r=0.278, p<0.001)
Correlation with SNOT-22 subdomains
SNOT-22 subdomains were analyzed to determine which symptoms correlated most strongly with postoperative LKES. Rhinologic and extra-nasal subdomains correlated most strongly and were the main drivers in overall SNOT-22 correlations (Table 3). Modified LKES (MLKES) correlations varied slightly from LKES correlations.
Table 3.
Correlation of postoperative endoscopy score with SNOT-22 subdomains
| LKES | MLKES | |||
|---|---|---|---|---|
| r | p | r | p | |
| 6 Month SNOT-22 Rhinologic Symptoms | 0.345 | <0.001 | 0.353 | <0.001 |
| 6 Month SNOT-22 Extra-nasal Symptoms | 0.311 | <0.001 | 0.303 | <0.001 |
| 6 Month SNOT-22 Ear Facial Symptoms | 0.227 | 0.002 | 0.199 | 0.007 |
| 6 Month SNOT-22 Psychological Dysfunction | 0.164 | 0.027 | 0.183 | 0.013 |
| 6 Month SNOT-22 Sleep Dysfunction | 0.130 | 0.079 | 0.149 | 0.044 |
| 6 Month SNOT-22 Total Score | 0.278 | <0.001 | 0.285 | <0.001 |
SNOT-22 = SinoNasal Outcomes Test-22; LKES = Lund Kennedy Endoscopy Score; MLKES = Modified Lund Kennedy Endoscopy Score
Impact of nasal polyps
CRSsNP
Mean postoperative LKES in CRSsNP patients was 2.9 ± 2.9 and just over half of CRSsNP patients achieve near perfect postoperative endoscopy. Among CRSsNP patients, as endoscopy worsened, there were trends in worsening SNOT-22 scores, increasing numbers of patients with missed productivity and increasing number of days missed; however, none of these trends were statistically significant (Table 4).
Table 4.
Impact of NP status upon postop endoscopy and clinical outcomes
| LKES | CRSsNP | CRSwNP | ||||||
|---|---|---|---|---|---|---|---|---|
| N (%) | Mean SNOT- 22 (SD) |
% of those missing any days of productivity in past 90 days |
Average days of missed productivity among those missing days |
N (%) | Mean SNOT- 22 (SD) |
% of those missing any days of productivity in past 90 days |
Average days of missed productivity among those missing days |
|
| 0–2 | 61 (56%) | 21.6 (17.5) | 27% | 18.6 | 27 (37%) | 17.7 (15.0) | 12% | 5.3 |
| 3–5 | 29 (26%) | 25.0 (19.4) | 31% | 7.0 | 22 (30%) | 26.2 (13.3) | 14% | 35.7 |
| ≥6 | 20 (18%) | 31.7 (21.6) | 47% | 26.0 | 24 (33%) | 33.0 (22.6) | 14% | 18.3 |
Among CRSsNP patients, there were no significant differences between endoscopy groups in SNOT-22 scores, % of patients with missed productivity or days of missed productivity (p≥0.120). Among CRSwNP patients, those who had LKES of 0–2 had SNOT-22 scores that were statistically significantly lower than those with LKES ≥6 (p=0.010). There were no other statistically significant differences in % of patients with missed productivity or days of missed productivity (p≥0.43). When comparing CRSsNP to CRSwNP groups with identical LKES categories, CRSwNP patients were less likely to achieve near perfect endoscopy (p=0.014). Among patients with poor endoscopy, those with CRSsNP were more likely to have missed days of productivity (47% vs 14%, p=0.023). There were no other differences based upon polyp status.
CRSsNP = Chronic rhinosinusitis without nasal polyps; CRSwNP = Chronic rhinosinusitis with nasal polyps; SNOT-22 = SinoNasal Outcomes Test-22; LKES = Lund Kennedy Endoscopy Score.
CRSwNP
Mean postoperative LKES in CRSwNP patients was 4.1 ± 3.1 and just over one third of CRSwNP patients achieve near perfect postoperative endoscopy, but when they do, their mean SNOT-22 scores are significantly better than CRSwNP patients with poor endoscopy. Similar to CRSsNP patients, postoperative LKES did not impact percent of patients missing days of productivity or days of missed productivity (Table 4).
Comparing CRSsNP to CRSwNP
When comparing diagnostic groups, some differences become apparent. CRSsNP patients are more likely to achieve near perfect endoscopy (56% vs 37%, p=0.014, Table 4). Among patients with poor endoscopy, CRSwNP patients are less likely to have missed productivity than CRSsNP patients with similar LKES (14% vs 47%, p=0.023). There were no significant differences in other variables when comparing diagnostic groups.
Subdomain analysis was performed to determine the impact of nasal polyp status upon various symptoms. CRSsNP patients had statistically significant, but relatively weak correlations between postoperative LKES and rhinologic, extranasal and ear facial subdomains. In contrast, endoscopy in CRSwNP patients had a moderate correlation with rhinologic and extra nasal subdomains (Table 5). MLKES provided little additional benefit.
Table 5.
Correlation of postop endoscopy with subdomains of SNOT-22 stratified by NP status
| CRSsNP | CRSwNP | |||||||
|---|---|---|---|---|---|---|---|---|
| LKES | MLKES | LKES | MLKES | |||||
| r | p | r | p | r | p | r | p | |
| 6 Month SNOT-22 Rhinologic Symptoms | 0.230 | 0.016 | 0.254 | 0.007 | 0.467 | <0.001 | 0.443 | <0.001 |
| 6 Month SNOT-22 Extra-nasal Symptoms | 0.277 | 0.003 | 0.288 | 0.002 | 0.389 | 0.001 | 0.359 | 0.002 |
| 6 Month SNOT-22 Ear Facial Symptoms | 0.207 | 0.030 | 0.200 | 0.037 | 0.274 | 0.019 | 0.220 | 0.061 |
| 6 Month SNOT-22 Psychological Dysfunction | 0.131 | 0.173 | 0.154 | 0.108 | 0.218 | 0.064 | 0.232 | 0.048 |
| 6 Month SNOT-22 Sleep Dysfunction | 0.104 | 0.278 | 0.094 | 0.331 | 0.164 | 0.165 | 0.220 | 0.062 |
| 6 Month SNOT-22 Total Score | 0.220 | 0.021 | 0.230 | 0.016 | 0.366 | 0.001 | 0.364 | 0.002 |
CRSsNP = Chronic rhinosinusitis without nasal polyps; CRSwNP = Chronic rhinosinusitis with nasal polyps; SNOT-22 = SinoNasal Outcomes Test-22; LKES = Lund Kennedy Endoscopy Score; MLKES = Modified Lund Kennedy Endoscopy Score
Medication usage
We then examined the relationship between postoperative endoscopy and medication usage to determine if additional medications, oral antibiotics and oral steroids in particular, were used differentially among endoscopy groups. In CRSsNP patients, there were no baseline differences in any medication category among the endoscopy groups. Postoperatively, however, patients with near perfect endoscopy used oral antibiotics and oral steroids less often than those with poor endoscopy and they used oral antibiotics, oral steroids, nasal steroid spray, antihistamines and decongestants less often than at baseline (Table 6).
Table 6.
Percentage of CRSsNP patients on medications in previous 90 days at baseline and postoperatively
| Postoperative Endoscopy Group (CRSsNP) | p | |||
|---|---|---|---|---|
| 0–2 (n=61) % (mean days) |
3–5 (n=29) % (mean days) |
≥6 (n=20) % (mean days) |
||
| Baseline Oral Antibiotic | 61% (30.6) | 75% (30.1) | 50% (39.0) | 0.209 |
| Six Month Oral Antibiotic | 17% (22.5) | 46% (36.3) | 45% (43.3) | 0.005 |
| Baseline vs. Six Month p value | <0.001 | 0.146 | 1.000 | |
| Baseline Oral Steroid | 55% (19.4) | 75% (19.8) | 47% (31.6) | 0.110 |
| Six Month Oral Steroid | 10% (35.3) | 12% (8.0) | 35% (12.0) | 0.021 |
| Baseline vs. Six Month p value | <0.001 | <0.001 | 0.581 | |
| Baseline Steroid Drops/Irrigations | 15% (64.2) | 21% (77.5) | 35% (74.3) | 0.162 |
| Six Month Steroid Drops/Irrigations | 28% (73.0) | 31% (70.9) | 63% (64.2) | 0.017 |
| Baseline vs. Six Month p value | 0.096 | 0.453 | 0.070 | |
| Baseline Steroid Spray | 78% (61.9) | 78% (54.1) | 74% (70.3) | 0.949 |
| Six Month Steroid Spray | 61% (74.1) | 58% (59.6) | 60% (62.0) | 0.967 |
| Baseline vs. Six Month p value | 0.013 | 0.070 | 0.375 | |
| Baseline Antihistamine | 48% (50.8) | 43% (66.3) | 42% (40.6) | 0.836 |
| Six Month Antihistamine | 28% (50.0) | 46% (50.8) | 35% (53.0) | 0.275 |
| Baseline vs. Six Month p value | 0.007 | 1.000 | 0.727 | |
| Baseline Decongestants | 47% (32.9) | 61% (55.1) | 50% (53.7) | 0.469 |
| Six Month Decongestant | 28% (21.8) | 42% (49.9) | 21% (30.0) | 0.257 |
| Baseline vs. Six Month p value | 0.035 | 0.289 | 0.070 | |
| Baseline Leukotriene Modifier | 13% (75.0) | 29% (65.0) | 26% (78.0) | 0.196 |
| Six Month Leukotriene Modifier | 18% (82.1) | 23% (62.0) | 15% (90.0) | 0.838 |
| Baseline vs. Six Month p value | 0.625 | 0.625 | 0.625 | |
| Baseline Saline | 85% (61.5) | 75% (59.8) | 84% (63.8) | 0.515 |
| Six Month Saline | 90% (73.7) | 92% (56.0) | 95% (75.0) | 0.898 |
| Baseline vs. Six Month p value | 0.508 | 0.289 | 0.625 | |
CRSsNP = Chronic rhinosinusitis without nasal polyps
In CRSwNP patients, there were no major differences in oral antibiotic use between endoscopy groups at baseline or postoperatively. When evaluating postoperative oral antibiotic use, all endoscopic groups decreased their use, but this only achieved statistical significance in the moderate LKES group. Oral steroid usage decreased postoperatively as LKES category improved and within each LKES category when comparing baseline to postoperative usage. In general, use of steroid irrigations/drops increased postoperatively and other maintenance medications remained relatively stable (Table 7).
Table 7.
Percentage of CRSwNP patients on medications in previous 90 days at baseline and postoperatively.
| Postoperative Endoscopy Group (CRSwNP) | p | |||
|---|---|---|---|---|
| 0–2 (n=27) % (mean days) |
3–5 (n=22) % (mean days) |
≥6 (n=24) % (mean days) |
||
| Baseline Oral Antibiotic | 44% (18.9) | 64% (22.6) | 52% (21.7) | 0.404 |
| Six Month Oral Antibiotic | 24% (32.7) | 29% (32.5) | 35% (37.1) | 0.712 |
| Baseline vs. Six Month p value | 0.180 | 0.039 | 0.508 | |
| Baseline Oral Steroid | 32% (25.3) | 59% (22.2) | 91% (24.5) | <0.001 |
| Six Month Oral Steroid | 8% (10.5) | 23% (56.0) | 44% (37.9) | 0.016 |
| Baseline vs. Six Month p value | 0.039 | 0.008 | 0.004 | |
| Baseline Steroid Drops/Irrigations | 8% (75.0) | 9% (60.0) | 50% (61.4) | <0.001 |
| Six Month Steroid Drops/Irrigations | 52% (76.5) | 59% (81.5) | 52% (82.5) | 0.861 |
| Baseline vs. Six Month p value | 0.001 | 0.001 | 1.000 | |
| Baseline Steroid Spray | 54% (63.2) | 59% (68.5) | 67% (43.1) | 0.673 |
| Six Month Steroid Spray | 39% (66.9) | 55% (72.1) | 48% (62.4) | 0.532 |
| Baseline vs. Six Month p value | 0.289 | 1.000 | 0.289 | |
| Baseline Antihistamine | 27% (46.6) | 86% (47.4) | 46% (40.3) | <0.001 |
| Six Month Antihistamine | 20% (48.0) | 46% (66.2) | 46% (63.5) | 0.107 |
| Baseline vs. Six Month p value | 0.500 | 0.004 | 1.000 | |
| Baseline Decongestants | 42% (15.9) | 50% (57.3) | 55% (35.8) | 0.691 |
| Six Month Decongestant | 12% (39.3) | 36% (38.9) | 44% (33.7) | 0.043 |
| Baseline vs. Six Month p value | 0.039 | 0.508 | 0.687 | |
| Baseline Leukotriene Modifier | 16% (90.0) | 32% (50.6) | 50% (75.2) | 0.044 |
| Six Month Leukotriene Modifier | 12% (80.0) | 41% (59.4) | 48% (73.4) | 0.019 |
| Baseline vs. Six Month p value | 1.000 | 0.687 | 1.000 | |
| Baseline Saline | 50% (63.4) | 86% (54.5) | 91% (59.4) | 0.002 |
| Six Month Saline | 88% (80.7) | 100% (75.5) | 91% (78.3) | 0.360 |
| Baseline vs. Six Month p value | 0.008 | 0.250 | 1.000 | |
CRSwNP = Chronic rhinosinusitis with nasal polyps
Comparison to healthy controls
CRS patients with near perfect postoperative endoscopy were then compared to non-CRS controls of similar age and gender. When comparing near perfect CRSwNP patients to healthy controls, there were no differences in total SNOT-22 or any of the subdomains. In contrast, CRSsNP patients who had near perfect postoperative endoscopy still had rhinologic and extra-nasal symptoms that were worse than non-CRS controls (Table 8).
Table 8.
Comparison of CRS patients with near perfect endoscopy to healthy, non-CRS controls
| Healthy non-CRS control |
CRSwNP post ESS endoscopy 0–2 |
CRSsNP post ESS endoscopy 0–2 |
|||
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | p vs control |
Mean (SD) | p vs control |
|
| 6 Month SNOT-22 Rhinologic Symptoms | 3.9 (4.2) | 4.7 (5.24) | 0.445 | 6.4 (5.56) | 0.009 |
| 6 Month SNOT-22 Extra-nasal Symptoms | 2.0 (2.4) | 2.4 (2.45) | 0.490 | 4.0 (3.51) | 0.001 |
| 6 Month SNOT-22 Ear Facial Symptoms | 2.4 (2.8) | 2.9 (3.26) | 0.487 | 3.5 (3.82) | 0.078 |
| 6 Month SNOT-22 Psychological Dysfunction | 5.5 (5.8) | 5.2 (5.56) | 0.852 | 6.3 (7.12) | 0.530 |
| 6 Month SNOT-22 Sleep Dysfunction | 5.7 (5.3) | 6.3 (6.05) | 0.672 | 6.1 (6.17) | 0.731 |
| 6 Month SNOT-22 Total Score | 16.3 (13.4) | 17.7 (15.0) | 0.672 | 21.6 (17.5) | 0.082 |
CRSsNP = Chronic rhinosinusitis without nasal polyps; CRSwNP = Chronic rhinosinusitis with nasal polyps; SNOT-22 = SinoNasal Outcomes Test-22
Discussion
Postoperatively, sinus surgeons perform endoscopy with the goal of achieving a well healed sinus cavity, due largely to the belief that a healthy postoperative cavity is associated with fewer symptoms and improved outcomes. In our overall cohort, we were able to achieve perfect or near perfect 6 month endoscopy scores in nearly half of our patients (46%). The remainder of our patients were evenly divided between moderate endoscopy (3–5) and poor endoscopy (≥6). When examining the impact of NP status upon likelihood of achieving perfect endoscopy, we found that CRSsNP patients are much more likely to achieve a near perfect cavity (56%) when compared to CRSwNP patients (37%). This is comparable to other series that have reported perfect endoscopy ranging from 51% in a CRSsNP series8 to 21% in a series with unknown percentage of CRSwNP patients3. The highest report of perfect cavities was 63%. However, this series used non-validated endoscopy, the patient population included only 22% CRSwNP patients and surgical indications included headache and nasal obstruction15. It is also important to note that CRSwNP patients in our series had a number of significant differences from CRSsNP patients, including number of prior surgeries, asthma prevalence and aspirin tolerance (Table 1). In order to compare our findings to prior reports, we chose to compare our patients based upon polyp status and did not examine the impact of all demographic and patient specific factors that could impact postoperative endoscopy, but this is an important consideration for future studies.
Other series have reported mean postoperative LKES rather than categorizing the distribution of patients. In CRSsNP patients, mean LKES as low as 1.46 have been reported, while in CRSwNP mean LKES as high as 7.9 are reported7. Our cohort had mean LKES of 2.9 in CRSsNP patients and 4.1 in CRSwNP patients. Obviously postoperative endoscopy is influenced by multiple factors including nasal polyp status, adjuvant medical therapy, patient compliance and possibly postoperative debridement. Wright7 demonstrated that using perioperative prednisone in CRSwNP patients can improve LKES at 6 months from 7.9 to 4.7. Similarly, Snidvongs4 reported a mean LKES at 1 year of 2.9 in CRSwNP patients using postoperative steroid irrigations. We found that systemic medication use was actually greater in our poor endoscopy groups. Of particular interest, CRSsNP patients with poor endoscopy used more oral antibiotics and oral steroids and CRSwNP patients with poor endoscopy used more oral steroids, so near perfect endoscopy was not the result of increased postoperative medications, but was associated with less systemic medication usage. Thus achieving near perfect postoperative endoscopy is indicative of better overall control of CRS, ie fewer symptoms and less systemic medications. Perioperative and postoperative therapies in our series were at the discretion of the treating surgeon and were not standardized, thus, variations in these practices may have impacted endoscopic outcomes and is an area for future study.
In our overall cohort, postoperative LKES did correlate with total postoperative SNOT-22 score. This was driven largely by rhinologic and extra nasal subdomains in both CRSsNP and CRSwNP patients, with much weaker correlations to ear/facial and psychological domains. This is not particularly surprising given that nasal endoscopy is an assessment of sinonasal burden of disease and may not accurately assess non-rhinologic, systemic manifestations of CRS. It can be seen that CRSwNP patients have a much stronger correlation between their postoperative endoscopy and rhinologic and extranasal symptoms than CRSsNP patients. This strong correlation to nasal specific symptoms, especially in CRSwNP patients may explain the conflicting information noted in other series. Several showed weak or no correlations to overall sinus specific QOL, but correlations improve when examining the relationship between endoscopy and nasal specific symptoms2,3,5,6 or when examining CRSwNP patients7. We failed to find a significant benefit to using a modified LKES. Correlations were similar, so modified systems that eliminate crust and scar may be quicker, but in our study it did not improve the magnitude of correlation. Additional limitations to our study are the somewhat subjective nature of endoscopic grading and the tertiary nature of the practices that contributed. Thus our results may not be broadly applicable to general practices.
While endoscopic appearance is an important, surgeon defined outcome, ultimately it is critical to understand the impact of improved postoperative endoscopy upon patient symptoms. Among CRSwNP patients, SNOT-22 scores improve as postoperative endoscopy improves and in the 37% of CRSwNP patients who achieve near perfect endoscopy, their SNOT-22 scores reach normative values. In contrast, while CRSsNP patients with poor endoscopy had worse SNOT-22 scores, they were not significantly different from CRSsNP patients with near perfect endoscopy. As shown in Table 3, SNOT-22 scores among CRSsNP patients with moderate and poor endoscopy paralleled CRSwNP patients, thus the lack of differences among the CRSsNP cohort is likely due to failure of those with near perfect endoscopy to achieve “normal” SNOT-22 scores. These near perfect CRSsNP patients had a mean SNOT-22 score of 21.6, which was 4 to 5 points worse than non-CRS controls and CRSwNP patients with near perfect endoscopy (Table 7). Previous studies have reported normative data for the SNOT-22 in non-CRS patients with a mean as low as 716, however these studies typically examined medical students or other populations that were not matched for age, gender, co-morbidities and environmental exposures17,18–20. When we compared our CRS cohort to a matched non-CRS cohort, we found that a “normal” SNOT-22 is approximately 16, thus this should realistically be the goal for our CRS patients, rather than a “perfect” score of 0. CRSwNP patients who achieve near perfect endoscopy achieve normal symptom levels in all domains of the SNOT-22, however, CRSsNP patients with near perfect endoscopy still have significantly worse sinus specific QoL, in particular rhinologic and extra-nasal symptoms. It is possible that CRSsNP patients have some underlying rhinologic or extra-nasal condition that endoscopy does not adequately assess and which we did not account for. While atopy and OSA were not significantly higher in the CRSwNP group, they may have had non-allergic rhinitis, laryngopharyngeal reflux or some other undetected condition. While the explanation for persistent sinonasal symptoms in the near perfect CRSsNP patients is unclear, it may be useful to inform these patients that even if surgery and medical treatments get them to a perfect sinus cavity, it is likely they will still experience sinonasal symptoms that are worse than CRSwNP patients and non-CRS controls.
Conclusion
Achieving near perfect postoperative endoscopy is an indicator of better control of CRS, with improved symptoms and decreased systemic medication use. When faced with a CRSwNP patient, surgeons can counsel them that they can get back to “normal” endoscopy about one third of the time and their rhinologic and systemic symptoms will then be similar to healthy non-CRS patients. CRSsNP patients will also experience clinical improvement regardless of postoperative endoscopy, but even if they get to a near perfect state, they will still experience rhinologic and extra nasal symptoms that are worse than otherwise healthy patients.
Acknowledgment
Dr. R. J. Schlosser is consultant for Olympus and Arrinex and received grant support from Intersect ENT, Entellus and Optinose. Dr. T. L. Smith, Dr. Z. M. Soler, and J. C. Mace are supported by a grant from the National Institutes of Health (NIH; R01 DC005805). The NIH had no role in the preparation, review, or approval of this article or decision to submit it for publication. Dr. T. L. Smith is consultant for Intersect ENT. Dr. Z.M. Soler is consultant for Olympus and received grant support from Intersect ENT, Entellus and Optinose.
Footnotes
The authors have no other funding, financial relationships, or conflicts of interest to disclose.
References
- 1.Senior BA, Kennedy DW, Tanabodee J, Kroger H, Hassab M, Lanza D. Long-term results of functional endoscopic sinus surgery. Laryngoscope. 1998;108:151–157. doi: 10.1097/00005537-199802000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Kaplan BA, Kountakis SE. Role of nasal endoscopy in patients undergoing endoscopic sinus surgery. Am J Rhinol. 2004;18:161–164. [PubMed] [Google Scholar]
- 3.Ryan WR, Ramachandra T, Hwang PH. Correlations between symptoms, nasal endoscopy, and in-office computed tomography in post-surgical chronic rhinosinusitis patients. Laryngoscope. 2011;121:674–678. doi: 10.1002/lary.21394. [DOI] [PubMed] [Google Scholar]
- 4.Snidvongs K, Pratt E, Chin D, Sacks R, Earls P, Harvey RJ. Corticosteroid nasal irrigations after endoscopic sinus surgery in the management of chronic rhinosinusitis. International forum of allergy & rhinology. 2012;2:415–421. doi: 10.1002/alr.21047. [DOI] [PubMed] [Google Scholar]
- 5.Psaltis AJ, Li G, Vaezeafshar R, Cho KS, Hwang PH. Modification of the Lund-Kennedy endoscopic scoring system improves its reliability and correlation with patient-reported outcome measures. Laryngoscope. 2014;124:2216–2223. doi: 10.1002/lary.24654. [DOI] [PubMed] [Google Scholar]
- 6.Toros SZ, Bolukbasi S, Naiboglu B, et al. Comparative outcomes of endoscopic sinus surgery in patients with chronic sinusitis and nasal polyps. Eur Arch Otorhinolaryngol. 2007;264:1003–1008. doi: 10.1007/s00405-007-0301-5. [DOI] [PubMed] [Google Scholar]
- 7.Wright ED, Agrawal S. Impact of perioperative systemic steroids on surgical outcomes in patients with chronic rhinosinusitis with polyposis: evaluation with the novel Perioperative Sinus Endoscopy (POSE) scoring system. Laryngoscope. 2007;117:1–28. doi: 10.1097/MLG.0b013e31814842f8. [DOI] [PubMed] [Google Scholar]
- 8.Giger R, Dulguerov P, Quinodoz D, et al. Chronic panrhinosinusitis without nasal polyps: long-term outcome after functional endoscopic sinus surgery. Otolaryngol Head Neck Surg. 2004;131:534–541. doi: 10.1016/j.otohns.2004.03.030. [DOI] [PubMed] [Google Scholar]
- 9.Snidvongs K, Dalgorf D, Kalish L, Sacks R, Pratt E, Harvey RJ. Modified Lund Mackay Postoperative Endoscopy Score for defining inflammatory burden in chronic rhinosinusitis. Rhinology. 2014;52:53–59. doi: 10.4193/Rhino13.056. [DOI] [PubMed] [Google Scholar]
- 10.Mace JC, Michael YL, Carlson NE, Litvack JR, Smith TL. Correlations between endoscopy score and quality of life changes after sinus surgery. Arch Otolaryngol Head Neck Surg. 2010;136:340–346. doi: 10.1001/archoto.2010.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fokkens WJ, Lund VJ, Mullol J, et al. EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology. 2012;50:1–12. doi: 10.4193/Rhino12.000. [DOI] [PubMed] [Google Scholar]
- 12.Rosenfeld RM. Clinical practice guideline on adult sinusitis. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2007;137:365–377. doi: 10.1016/j.otohns.2007.07.021. [DOI] [PubMed] [Google Scholar]
- 13.DeConde AS, Bodner TE, Mace JC, Smith TL. Response shift in quality of life after endoscopic sinus surgery for chronic rhinosinusitis. JAMA otolaryngology-- head & neck surgery. 2014;140:712–719. doi: 10.1001/jamaoto.2014.1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Browne JP, Hopkins C, Slack R, Cano SJ. The Sino-Nasal Outcome Test (SNOT): can we make it more clinically meaningful? Otolaryngol Head Neck Surg. 2007;136:736–741. doi: 10.1016/j.otohns.2007.01.024. [DOI] [PubMed] [Google Scholar]
- 15.Vleming M, de Vries N. Endoscopic paranasal sinus surgery: Results. American Journal of Rhinology. 1990;4:13–17. [Google Scholar]
- 16.Jalessi M, Farhadi M, Kamrava SK, et al. The reliability and validity of the persian version of sinonasal outcome test 22 (snot 22) questionnaires. Iranian Red Crescent medical journal. 2013;15:404–408. doi: 10.5812/ircmj.7937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vaitkus S, Padervinskis E, Balsevicius T, et al. Translation, cross-cultural adaptation, and validation of the sino-nasal outcome test (SNOT)-22 for Lithuanian patients. Eur Arch Otorhinolaryngol. 2013;270:1843–1848. doi: 10.1007/s00405-012-2282-2. [DOI] [PubMed] [Google Scholar]
- 18.Lachanas VA, Tsea M, Tsiouvaka S, Hajiioannou JK, Skoulakis CE, Bizakis JG. The sino-nasal outcome test (SNOT)-22: validation for Greek patients. Eur Arch Otorhinolaryngol. 2014;271:2723–2728. doi: 10.1007/s00405-014-2969-7. [DOI] [PubMed] [Google Scholar]
- 19.Kosugi EM, Chen VG, Fonseca VM, Cursino MM, Mendes Neto JA, Gregorio LC. Translation, cross-cultural adaptation and validation of SinoNasal Outcome Test (SNOT): 22 to Brazilian Portuguese. Brazilian journal of otorhinolaryngology. 2011;77:663–669. doi: 10.1590/S1808-86942011000500021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gillett S, Hopkins C, Slack R, Browne JP. A pilot study of the SNOT 22 score in adults with no sinonasal disease. Clinical otolaryngology : official journal of ENT-UK; official journal of Netherlands Society for Oto-Rhino-Laryngology & Cervico-Facial Surgery. 2009;34:467–469. doi: 10.1111/j.1749-4486.2009.01975.x. [DOI] [PubMed] [Google Scholar]