Abstract
Rationale
Due to the rising costs of drug development especially in the field of neuropsychiatry there is increasing interest in efforts to identify new clinical uses for existing approved drugs (i.e., drug repurposing).
Objectives
The purpose of this work was to evaluate in animals the smoking cessation agent, varenicline, a partial agonist at α4β2 and full agonist at α7 nicotinic acetylcholine receptors, for its potential as a repurposed drug for disorders of cognition.
Methods
Oral doses of varenicline ranging from 0.01 to 0.3 mg/kg were evaluated in aged and middle aged monkeys for effects on: working/short term memory in a delayed match to sample (DMTS) task, distractibility in a distractor version of the DMTS (DMTS-D), and cognitive flexibility in a ketamine-impaired reversal learning task.
Results
In dose-effect studies in the DMTS and DMTS-D tasks, varenicline was not associated with statistically significant effects on performance. However, individualized “optimal doses” were effective when repeated on a separate occasion (i.e., improving DMTS accuracy at long delays and DMTS-D accuracy at short delays by approximately 13.6 and 19.6 percentage points above baseline, respectively). In reversal learning studies, ketamine impaired accuracy and increased perseverative responding, effects that were attenuated by all three doses of varenicline that were evaluated.
Conclusions
While the effects of varenicline across the different behavioral tasks were modest, these data suggest that varenicline may have potential as a repurposed drug for disorders of cognition associated with aging (e.g., Alzheimer’s disease), as well as those not necessarily associated with advanced age (e.g., schizophrenia).
Keywords: Alzheimer’s disease, schizophrenia, Mild Cognitive Impairment, attention deficit hyperactivity disorder (ADHD), repurposing, repositioning, working memory, cognitive flexibility, reversal learning, cholinergic
Introduction
The enormous costs and time investments required to develop new drugs (i.e., from the discovery phase to clinical approval) combined with frequent failures in clinical trials has resulted in several large pharmaceutical companies abandoning or severely restricting their research and development programs for neuropsychiatric disorders (Kaitin et al. 2011; Riordan and Cutler 2011). This dilemma has led to an increased interest in alternative approaches to the drug discovery process such as drug repurposing or repositioning (i.e., identifying new clinical uses for existing approved drugs, see Ashburn and Thor 2004; Merino et al. 2010; Medina-Franco et al. 2013). Drug repurposing can potentially reduce the time, costs and safety risks associated with clinical approval for a new indication, since, most repurposed candidates have already been assessed in phase I or II clinical trials for their original indications (Ashburn and Thor 2004). There are multiple examples in the past where clinical observations and off-label prescribing eventually led to the approval of drugs for purposes other than what they were originally approved for (e.g., anticonvulsants for pain disorders and bipolar disease, antihypertensive beta blockers for congestive heart failure and migraine prophylaxis). However, this “clinical observation” and “off-label prescribing” approach to drug discovery is not an efficient mechanism and there is a critical need for prospective (scientifically-based) repurposing studies both in the preclinical and clinical trials setting.
Due to observations over 25 years ago that the tobacco alkaloid nicotine has pro-cognitive effects in non-smokers and animal models (see Levin 2006), numerous preclinical studies have been conducted to assess the potential of nicotine and nicotine-like compounds as therapeutic agents for conditions as diverse as Alzheimer’s disease (AD), ADHD, schizophrenia, Parkinson disease and depression (see Powledge 2014 for review). Currently, the only nicotinic ligands available either by prescription or over the counter (and thus potentially available for repurposing) are nicotine itself (as a gum or transdermal patch) and the 4 2 nAChR partial agonist/α7 nAChR full agonist, varenicline, both currently used to improve smoking cessation. Despite prior concerns regarding potential side effects of nicotine, there have been several encouraging (albeit small) clinical trials with nicotine for AD (Newhouse et al. 1988; Sahakian et al. 1991; Jones et al. 1992; Wilson et al. 1995 White and Levin 1999) and one encouraging study in Mild Cognitive Impairment (MCI, Newhouse et al. 2012).
There is also some preclinical and clinical evidence to suggest that varenicline might be worth evaluating for repurposing in conditions where cognitive function is impaired. For example, in rats varenicline has been shown to improve sustained attention in a signal detection task, to enhance sensorimotor gating in a prepulse inhibition task, and to improve recognition memory in a novel object recognition task (Rollema et al. 2009), thus indicating its potential for conditions such as AD and schizophrenia. Moreover, varenicline significantly improved delayed match to sample performance in both cocaine-naive and cocaine-experienced monkeys (Gould et al. 2013) indicating a potential for is use as a pro-cognitive agent in drug addiction as well as other disorders. There has been a small number of clinical studies designed to evaluate the effect of varenicline in healthy, non-smoking adults (Mocking et al. 2013), in abstinent smokers (Loughead et al. 2010), schizophrenia and schizoaffective disorder (Smith et al., 2009), mild to moderate AD (Kim et al. 2014), and adjunctively with antipsychotics for cognitive impairments in schizophrenia (Shim et al. 2012). Most of these studies (with the exception of the Kim study cited above) have had promising results, although they were typically short in duration with a relatively small sample size. Based on these encouraging findings, the purpose of the experiments described in this report study was, to further evaluate varenicline as a potential pro-cognitive agent in monkeys in tasks designed to assess working/short term memory, attention/distractibility, and cognitive flexibility.
Materials and Methods
All procedures employed during this study were approved by the Georgia Regents University Institutional Animal Care and Use Committee and are consistent with AAALAC guidelines. Measures were taken to minimize pain and discomfort in accordance with the National Institutes of Health Guide for the Care and Use of Laboratory Animals (NIH Publications No. 80-23) revised 1996. Significant efforts were also made to minimize the total number of animals used while maintaining statistically valid group numbers.
Test Subjects
The subjects in this study included a total of 20 male and female rhesus (Macaca mulatta) and pigtail (Macaca nemestrina) macaques designated as aged (≥19 years old) and young/middle-aged (≤18 years old) divided into 3 cohorts (see Table 1 for additional details). The designation of aged at ≥19 years old is based on previous studies in rhesus monkeys where cognitive impairments (and accompanying neuroanatomical changes) began to emerge late in the second decade of life, becoming prominent by the mid 20’s (see Price and Sisodia 1994 for review). The monkeys were individually housed in double stainless steel cages composed of two 127 x 71 x 66 cm units in rooms with up to five other monkeys. To promote psychological well-being, a variety of enrichment devices including perch bars, toys, foraging tubes, and a variety of food treats were provided routinely and the monkeys were allowed to observe television programs each afternoon after behavioral testing. At certain times when animals were not being tested routinely (e.g., during prolonged washout periods from drug studies, and after the semi-annual physical exams) they are allowed access to an enclosed outdoor exercise facility.
Table 1.
Monkey Subject Information
| DMTS Delay Intervals (sec) | ||||||
|---|---|---|---|---|---|---|
| Subject ID | Species | Gender | Age | Wt (kg) | Short | Long |
|
|
|
|
|
|
|
|
| Cohort 1 | ||||||
| 281 | Rhesus | M | 27 | 12.0 | 3 | 100 |
| 51 | Rhesus | M | 26 | 13.1 | 5 | 75 |
| 23 | Rhesus | M | 29 | 12.2 | 5 | 40 |
| 993 | Rhesus | M | 21 | 13.3 | 8 | 40 |
| p73 | Rhesus | F | 24 | 7.7 | 3 | 50 |
| 979 | Rhesus | F | 35 | 9.4 | 5 | 45 |
| 987 | Rhesus | M | 20 | 10.8 | 10 | 100 |
| 573 | Rhesus | M | 31 | 13.7 | 4 | 100 |
|
|
||||||
| Mean | 26.6 | 11.5 | 5.4 | 68.8 | ||
| SEM | 1.8 | 0.8 | 0.9 | 10.6 | ||
|
| ||||||
| Cohort 2 | ||||||
| 808 | Rhesus | F | 18 | 12.2 | 4 | 30 |
| NA8 | Rhesus | M | 18 | 11.1 | 7 | 90 |
| 77F | Rhesus | F | 10 | 10.8 | 3 | 40 |
| 147 | Rhesus | M | 16 | 14.8 | 5 | 45 |
| 86F | Rhesus | F | 11 | 6.9 | 15 | 60 |
| K1E | Rhesus | F | 14 | 13.6 | 4 | 30 |
| Mean | 14.5 | 11.6 | 6.3 | 49.2 | ||
| SEM | 1.4 | 1.1 | 1.8 | 9.3 | ||
|
| ||||||
| Cohort 3 | ||||||
| V6T | Pigtail | M | 15 | 16.7 | NA | NA |
| 119 | Pigtail | F | 24 | 9.1 | NA | NA |
| C8R | Pigtail | M | 15 | 11.7 | NA | NA |
| PA1 | Pigtail | M | 20 | 17 | NA | NA |
| P2J | Pigtail | M | 17 | 13.7 | NA | NA |
| 770 | Pigtail | F | 25 | 7.8 | NA | NA |
| Mean | 19.3 | 12.7 | ||||
| SEM | 1.8 | 1.6 | ||||
Subjects were maintained on tap water (unlimited) and standard laboratory monkey chow (Harlan Teklad Laboratory monkey diet, Madison, WI) supplemented with fruits and vegetables. Food was removed from cages at about 0630 hours, and replaced after behavioral testing of all subjects for the day (at about 1630 hours). Additional nourishment was derived from 300 mg reinforcement food pellets (composition of standard monkey chow and banana flakes, Noyes Precision food pellets, P.J. Noyes Co., Lancaster, NH) obtained during behavioral test sessions. On weekends animals were fed without time restrictions. Room temperature and humidity were maintained at 22 ± 0.6°C and 52 ± 2%, respectively.
Each test subject had previously participated in one or more short-term studies assessing the effects of reversible drugs on Delayed Match to Sample performance (see below). Prior drug experience produced no observable untoward effects, and each subject received at least a 4-week washout period (with continued weekday DMTS testing) prior to the beginning of this study.
Delayed Match to Sample (DMTS) Testing
DMTS testing was conducted in monkey Cohort 1 (see Table 1) using a modification of the procedure we have described previously (Terry et al. 2005; Webster et al. 2011). Briefly, computer-automated test panels with touch-sensitive screens (15 in. AccuTouch LCD Panelmount TouchMonitor) and pellet dispenser units (Med Associates) were mounted in lightweight aluminum chasses and attached to each animal’s home cage prior to DMTS testing. The visual stimuli presented for matching included rectangles of various colors (e.g., red, blue, yellow). A trial was initiated by the presentation of a sample square composed of one of three colors. The sample rectangle remained in view until the monkey touched within its borders to initiate a pre-programmed delay (retention) interval. Following the delay interval, the two choice rectangles located below where the sample had been were presented. One of the two choice colors was presented with the color matching the stimulus (correct), whereas the other (incorrect) color was presented as one of the two remaining colors. A correct (matching) choice was rewarded with a banana flavored food pellet (see above). Non-matching choices were neither reinforced nor punished. The inter-trial interval was 5 sec and each session consisted of 96 trials. The presentation of stimulus colors, choice colors, and choice positions were fully counterbalanced so as to relegate non-matching strategies to chance levels of accuracy. Five different presentation sequences were rotated through each daily session to prevent the subjects from memorizing the first several trials. Delay intervals were established during numerous non-drug or vehicle sessions prior to initiating the study.
Training sessions
The duration for each delay interval was adjusted for each subject until three levels of group performance accuracy were approximated: zero delay (85–100% of trials answered correctly); short delay interval (70–84% correct); and long delay interval (50–65% correct). The assignment of retention intervals based upon an individual’s baseline task accuracy is necessary to avoid ceiling effects in the most proficient animals during drug studies, while also serving to insure that each animal begins testing at relatively the same level of task difficulty. In addition to session accuracy, two response latencies also were measured: the “sample latency”, which is the time between presentation of the sample color and the animal pressing in sample rectangle; and the “choice latency”, which is the time between presentation of the choice colors and the animal pressing one of the choice rectangles. Each animal was well trained (>100 individual sessions) in the delayed matching-to-sample (DMTS) task.
When the duration for each delay interval was adjusted and stabilized so that performances of the monkeys were within the ranges of accuracy described above, pharmacological studies were initiated. The standard weekly regimen for each drug administration included, Monday: the administration of vehicle followed by DMTS testing; Tuesday: drug administration followed by DMTS test session; Wednesday: DMTS testing (in the absence of drug or vehicle) initiated 24 hours after Tuesday’s dosing; Thursday and Friday: same as Tuesday and Wednesday. This timing of administration (i.e., the particular day of drug and/or placebo administration) could be modified in response to some (husbandry or housing-related) constraints and adapted to each monkey.
DMTS with Distractor (DMTS-D) Trials
In a separate group of monkeys (Cohort 2, see Table 1) a “distractor’ version of the DMTS task was conducted using a modification of a previously published procedure (see Terry et al. 2002). Distractor stimuli (interference trials) were presented to the test subject on 24 of the 96 trials completed during distractor DMTS sessions. The stimuli were presented simultaneously on the sample and choice keys for 3 sec and they consisted of a random pattern of three colored rectangles flashing in an alternating manner. The distractor rectangles were comprised of the same 3 colors used for sample and choice stimuli presentation. The total duration of presentation for a given colored light was 0.33 sec. Immediately as one colored light was extinguished, a different colored light was presented. Thus, during presentation of the distractor, each color was presented in random order on each key 3 separate times. Distractor stimuli (24) were presented an equal number of times on trials with Short and Long delay intervals. The remaining trials were completed with no delay interval or distractor and they were randomly inserted throughout the test session. The following parameters were recorded during all test sessions: % correct on distractor and non-distractor trials with Short, and Long delay intervals, and latency of response to sample and choice stimuli.
Distractor DMTS sessions were administered no more frequently than three times every two weeks to avoid the animals becoming tolerant to the impairing effects of the distractor. For each two-week block, the sequence for distractor sessions generally was Wednesday of the first week, and Monday and Thursday of the subsequent week. For all other weekdays, animals were administered the standard DMTS task with no pre-test intervention.
Reversal Learning-Spatial (Left-Right) Response Strategy Task
In a third group of monkeys (Cohort 3, see Table 1) reversal learning studies were conducted using a ketamine-impairment model (see under Drug Administration)
Apparatus
Behavioral testing was performed using a custom-designed Wisconsin General Test Apparatus (WGTA) that was attached directly to the monkey’s home cage in the colony room (Taylor et al. 1990). The WGTA (constructed at the Laboratory Equipment Services Division at Georgia Regents University) consisted of an opaque panel that could be raised and lowered manually and it separated the monkey from the metal test tray (25.4 cm long x 10.16 cm wide) that contained 3 equally spaced food wells with hinged Plexiglas lids (8.25 cm long x 5.08 cm wide). A slot in the lid top allowed the experimenter to insert distinctive, colored pictures (Microsoft Clip Art) and the monkey was able to easily open the lids to retrieve the hidden food reward (Reese’s Pieces, The Hershey Company, Hershey PA). Initially, all monkeys were habituated to the apparatus and trained to open the lid to retrieve the food reward once the panel was raised. The monkey was allowed to open only one lid per trial and each trial lasted until the subject opened a lid or 2 min had lapsed. Subjects were given 20 trials per session with an inter-trial interval (ITI) of 10 sec. Testing occurred on Monday, Wednesday and Friday between 11 A.M. and 2 P.M.
Spatial (Left-Right) Response
Training- All monkeys were trained to perform a spatial (left-right) response location strategy task in a between-session design. A trial began by placing the reward under the right lid location with the panel lowered so the subject could not see the placement of the reward. The panel was raised and the subject was allowed to make one choice by lifting either the right, center or left lid; each lid top contained a red card that was irrelevant to correct response location. Once the subject made a choice the panel was lowered and the experimenter scored the response as either correct or incorrect before proceeding to the next trial. Thus, the animals were trained to select one well location per trial and to determine, solely by trial and error, that the right lid location contained the reward. For each training session, the subject was given 20 trials with an ITI of 10 sec; if the subject did not make a choice selection within 2 min the trial ended, scored as “no response” and a new trial began. Training continued with the right response location strategy until each monkey reached a predetermined performance accuracy criterion of ≥90% correct for 3 consecutive training sessions. Once the right spatial response strategy was achieved, training began with the left response location until all animals met the predetermined accuracy criterion (above). Each response strategy was presented consecutively for 3-9 sessions prior to switching to the other strategy. Training continued for each spatial response location until all monkeys were performing each location strategy at a consistent and competent level prior to performing any pharmacological assessment.
Reversal Tests
Once all monkeys achieved stable reversal learning performance, pharmacological testing began. During this phase of testing, animals were presented with 3 consecutive spatial response sessions (20 trials each; ITI=10 sec) to ensure 90% accuracy prior to the presentation of the reversal trial (i.e., switching to the other rewarded response location). The reversal trial was given 24–48 hrs after the initial learned response location strategy. Response locations were pseudo-randomized across all subjects and drug treatments. If a subject failed to maintain accuracy at any time during pharmacological testing it was given additional training. During the reversal test session the following dependent response measures were determined: 1) performance accuracy (% correct of the total responses); 2) perseverative errors (choosing the previously rewarded response location strategy; 3) regressive errors (once the subject made 4 correct responses under the new spatial location strategy all subsequent errors were no longer considered as perseverative errors, because at this point the subject was using an alternative strategy (Ragozzino et al., 1999); 4) never-reinforced errors (choosing the center location).
Drug Administration
DMTS and DMTS-D Tasks
Varenicline tartrate (Chantix® Pfizer Laboratories, NY, NY) was obtained through the hospital pharmacy at Georgia Regents Medical Center, Augusta Georgia. All drug doses were calculated based on the weight of the salt. In each of the behavioral studies described below, varenicline was administered orally in an ascending dose series one hour before testing in a solid formulation composed of a mixture of peanut butter and PRIMA-Burgers® (Bio Serv, Frenchtown, NJ). This formulation (without varenicline) was administered as the vehicle on non-drug days before, during, and after the varenicline dose-effect studies to obviate any confounding effects of training on DMTS performance that could be perceived as a varenicline-related effect.
Reversal Learning Task
To avoid potential pharmacological carryover effects (particularly for ketamine, see below), in the reversal learning studies, drug testing occurred no more than once per week. Subjects were first tested under vehicle conditions by administering the peanut butter and PRIMA-Burgers combination described above (orally) one hour before testing. Vehicle tests were performed 4–5 times over the course of the study to ensure stable task performance. Next, subjects were administered increasing doses of ketamine (Ketaset HCI, Fort Dodge Animal Health, Overland Park, Kansas) to determine a sufficient dose that would impair reversal learning performance compared to their vehicle performance without producing overt (non-specific) changes in behavior (e.g., sedation, motor incoordination). Ketamine doses (1.0–3.0 mg/kg, administered by intramuscular injection, 45 min pretreatment) were prepared from a 10 mg/ml stock solution using sterile, injection-grade saline. From this dose-effect evaluation, the 3.0 mg/kg dose of ketamine was selected (See Fig 3). Varenicline in an ascending dose series was subsequently administered orally 60 minutes before testing followed by the injection of ketamine 15 minutes later (i.e., 45 minutes before behavioral testing).
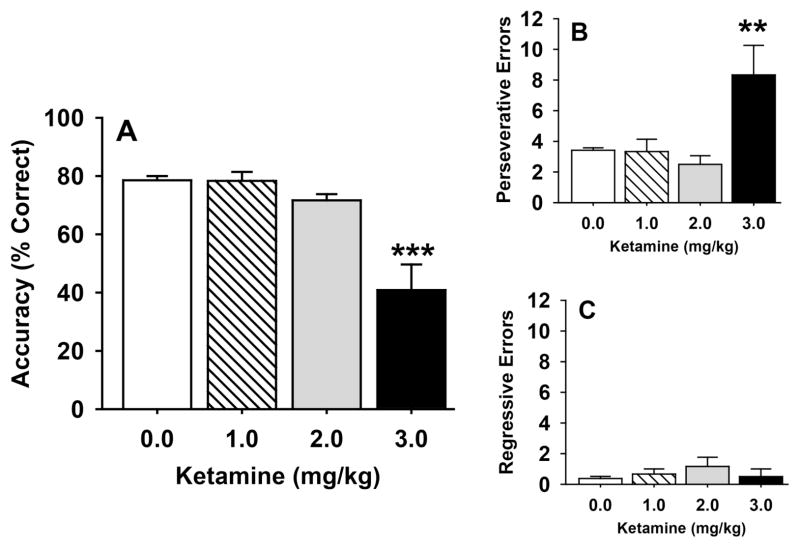
Fig. 3.
The effect of ketamine on performance of a reversal learning task in middle-aged/aged pigtail monkeys. (A) Dose-related effects on accuracy 45 min after the i.m. injection of ketamine or vehicle (saline). (B) Dose related effects on the number of perseverative errors 45 min after the i.m. injection of ketamine or vehicle (saline). (C) Dose related effects on the number of regressive errors 45 min after the i.m. injection of ketamine or vehicle (saline). Each bar represents the mean ± S.E.M. **p<0.01, ***p<0.001 = significant difference from vehicle-related response. N=6.
Statistical Analyses
For all one and two factor comparisons, analysis of variance (with repeated measures) was used followed by the Student Newman Keuls method for post hoc analysis (SigmaPlot 11.2). For each figure presented, error values denoted by ± indicate the standard error of the mean. Differences between means were considered significant at the p<0.05 level. Trends toward significance were considered at the p<0.10.
Results
Delayed Match to Sample (DMTS)
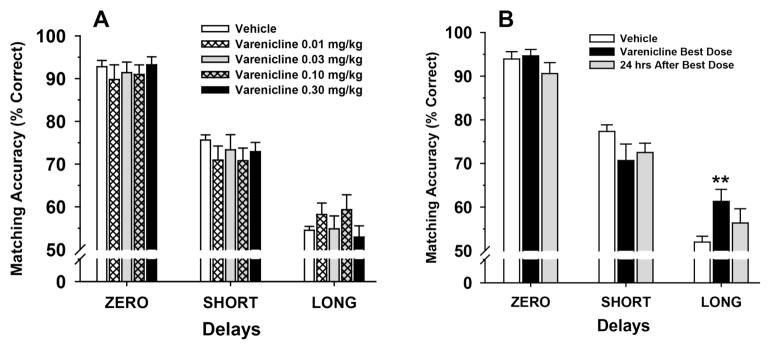
Vehicle (peanut butter & PRIMA-Burgers®) was administered on several occasions during the varenicline DMTS study (pseudorandomized with doses of varenicline) to cohort 1 (see Table 1). The data obtained from these sessions were averaged and used for comparison with varenicline treatment sessions. As a group the mean performance accuracies in the aged animals in the DMTS task after vehicle administration met the performance criteria set forth above (see Methods): Zero delay, 92.8%, Short delay, 75.6%, and Long delay, 54.5% trials correct and always followed a significant (p<0.001) delay-dependent decline in accuracy (see Fig. 1A). Oral administration of varenicline was not associated with statistically significant effects on DMTS accuracy; main effect of dose [F(4,28)=0.27, p=0.90]; delay [F(2,56)=134.6, p<0.001]; dose x delay interaction [F(8,56)=1.00, p=0.45]. A Best (optimal) dose was subsequently selected for each subject that was based on the highest overall (averaged) accuracy attained among the four doses tested. These selected doses were repeated in each subject on a separate occasion along with additional vehicle administrations. The best doses selected for each subject were as follows, monkeys #23 and 573 (0.01 mg/kg); monkeys #281, 993, p73, and 979 (0.1 mg/kg); monkeys #51 and 987 (0.3 mg/kg). In this (optimal dose) analysis (see Fig 1B), there were statistically significant improvements by varenicline of DMTS task accuracy (i.e., by approximately 13.6 percentage points above baseline), main effect of treatment, [F2,14=2.05, p=0.17]; delay, [F2,28=145.6, p<0.001]; treatment x delay interaction, [F4,28=2.68, p=0.05]. Post hoc analysis indicated that a significant (p=0.014) improvement in accuracy occurred at the long delay interval (when compared to vehicle performance).
Fig 1.
The effect of varenicline on performance of a Delayed Match to Sample (DMTS) task in aged rhesus monkeys. (A) Dose-effect relationship on accuracy for each delay interval in the DMTS task, 60 min after the oral administration of varenicline or vehicle. (B) Accuracy for each delay interval of the DMTS task 1 h after oral administration of the individualized and repeated optimal dose of varenicline or vehicle. Each bar represents the mean (% correct) ± S.E.M. over 96 trials per session. ** p<0.01= significant difference from vehicle response. N=8
Delayed Match to Sample with Distractor (DMTS-D)
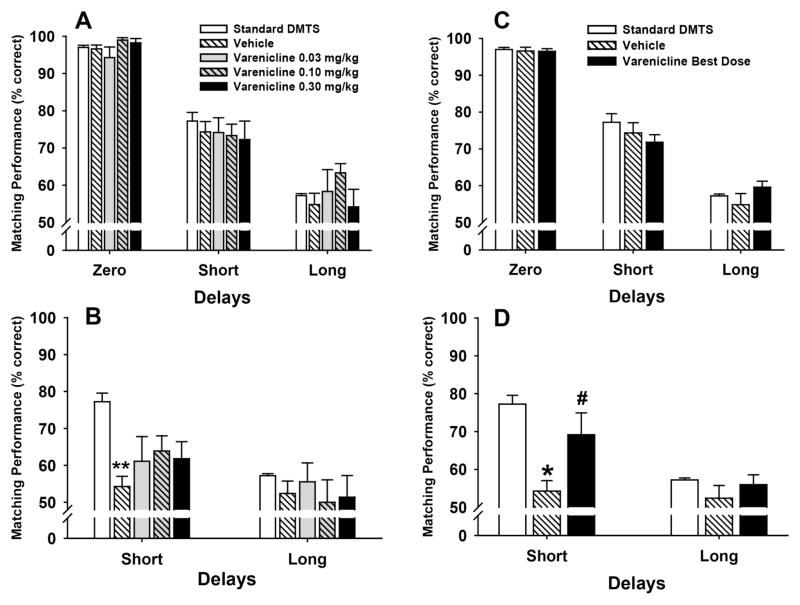
DMTS-D studies were conducted in Cohort 2 (see Table 1) on specific days of the week, and standard DMTS sessions were conducted on the other days. As in the case of the aged monkeys in Cohort 1, mean task accuracies in standard DMTS test sessions (i.e., under vehicle conditions) in the young/middle aged subjects in Cohort 2 also met the performance criteria set forth in the methods: zero delay, 97.0%, short delay, 77.2%, and long delay, 57.2% trials correct (see Fig 2A). On days when distractor sessions were incorporated (DMTS-D sessions), performance (under vehicle conditions) was not significantly different between the non-distractor trials and the standard DMTS trials (see Fig 2A), effect of trial type [F(1,5)=1.40, p=0.29]. Conversely, the presence of the distractor (see Fig 2B) produced a significant decrease in task accuracy relative to standard DMTS [F(1,5)=24.00, p=0.004]. Post hoc analysis indicated that task accuracy during short (but not long) delay distractor trials was significantly decreased (p<0.001) compared to standard DMTS test sessions (see Fig. 2B). Similarly, the presence of the distractor produced a significant decrease in task accuracy relative to non-distractor test sessions in the DMTS-D studies, effect of trial type [F(1,5)=13.30, p=0.015]. Post hoc analysis indicated that task accuracy during short (but not long) delay distractor trials was significantly decreased (p<0.001) compared to non-distractor test sessions.
Fig. 2.
The effect of varenicline on performance of the distractor version of the DMTS task (DMTS-D) in young/middle-aged monkeys. (A) Dose-effect relationship on accuracy for each delay in the DMTS-D task (non-distractor trials) in monkeys 60 min after the oral administration of varenicline. (B) Dose-effect relationship on accuracy for each delay in the DMTS-D task (distractor trials) in monkeys 60 min after the oral administration of varenicline. (C) Accuracy for each delay interval of the DMTS-D task (non-distractor trials) 60 mi after oral administration of the individualized and repeated optimal dose of varenicline or vehicle. (D) Accuracy for each delay interval of the DMTS-D task (distractor trials) 60 mi after oral administration of the individualized and repeated optimal dose of varenicline or vehicle. In each figure, mean accuracies associated with the standard DMTS task (under vehicle conditions) are included for comparison. Each bar represents the mean ± S.E.M. * p<0.05; **p<0.01= significant difference from standard DMTS task performance (under vehicle conditions). #p<0.05 = significant difference between the varenicline optimal dose performance and vehicle related performance during distractor trials. N=6
In the varenicline dose effect studies there was a clear trend toward a positive effect of varenicline, main effect of dose [F(4,20)=4.65, p=0.06] on DMTS-D (distractor trial) performance at short delay intervals (Fig 2B), however there were no statistically significant effects other that the effect of delay interval, [F(1,20)=10.68, p=0.02]. Likewise, there were no statistically significant effects of varenicline on DMTS-D (non-distractor) trials (p value for dose and dose x delay interaction were >0.05, Fig 1A).
After analysis of the DMTS-D dose-effect results, the optimal (best) dose was selected for each monkey (based on the best performance at short delay intervals) and repeated on a separate occasion (at least 2 weeks after the dose-effect studies) and randomized with additional vehicle distractor and standard DMTS test sessions. The best doses selected for each subject were as follows, monkeys #77F, 147, and 86F (0.03 mg/kg); monkeys #808, na8, and K1E (0.1 mg/kg). In these studies there was a clear (statistically significant) improvement by varenicline (i.e., by approximately 19.6 percentage points above baseline), of distractor trial performance (Fig 1D), main effect of treatment, [F(2,10)=0.97, p=0.45], delay, [F(1,10)=13.50, p=0.01], dose x delay interaction, [F(2,00)=7.36, p=0.01]. Post hoc analysis indicated that varenicline treatment significantly (p <0.035) improved task accuracy at the short delays compared to vehicle. There were no statistically significant effects of varenicline on non-distractor trial performance (p>0.05 for treatment, treatment x delay interaction, Fig 2C).
Reversal Learning Studies
In the ketamine dose-effect analysis in the reversal learning studies (see Fig 3A), there was a clear (dose-dependent) impairment of accuracy [F(3,15)=16.68, p<0.001]. Post hoc analysis indicated that ketamine 3.0 mg/kg treatment significantly (p<0.001) impaired task accuracy compared to vehicle control. Likewise, ketamine increased the number of perseverative errors, [F(3,15)=7.28, p=0.003], post hoc (p=0.003 for the ketamine 3.0 mg/kg versus vehicle comparison, see Fig 3B). There were no significant effects of ketamine on regressive errors (Fig 3C) or errors associated with the never-reinforced wells (data not shown).
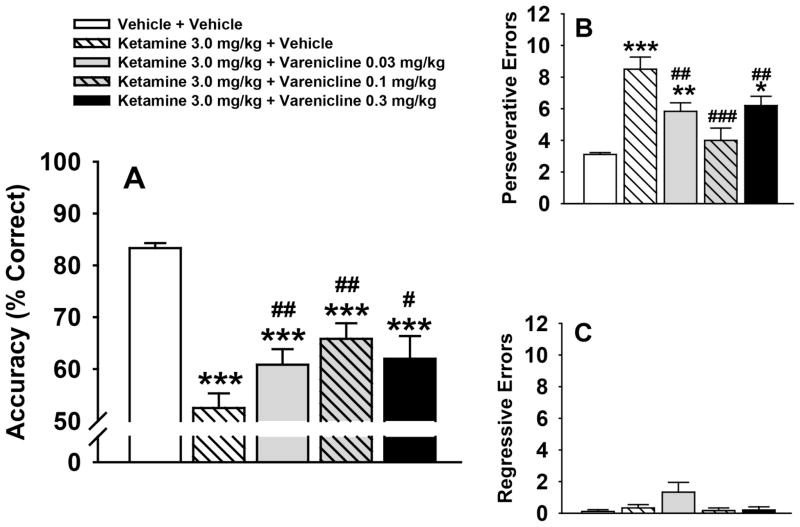
In the varenicline dose effect analysis (i.e., for the ability to reverse the negative effects of ketamine 3.0 mg/kg), the follow results were obtained: In the accuracy assessment (Fig 4A), there were highly significant effects of treatment [F(4,19)=26.36, p<0.001], post hoc analysis indicated that ketamine 3.0 mg/kg significantly impaired accuracy (p<0.001), and that all three dose of varenicline partially (but significantly) attenuated, the effects of ketamine on accuracy (p=0.015, p=0.002, and p=0.010, for the 0.03, 0.1, and 0.3 mg/kg doses of varenicline, respectively). Likewise, in the assessment of perseverative errors (Fig 4B), there was a significant effect of treatment, [F(4,19)=13.20, p<0.001], post hoc analysis indicated that ketamine 3.0 mg/kg significantly increased perseverative errors (p<0.001), and that all three dose of varenicline partially (but significantly) attenuated, the effects of ketamine on perseverative errors (p=0.010, p<0.001, and p=0.008, for the 0.03, 0.1, and 0.3 mg/kg doses of varenicline, respectively). There were no significant effects of any of the drug treatments on regressive errors (Fig 4C) or errors associated with the never-reinforced wells (data not shown).
Fig 4.
The effects of varenicline on the ketamine-related impairments in performance of a reversal learning task in middle-aged/aged pigtail monkeys. (A) Effects of different doses of varenicline or vehicle when combined with ketamine on accuracy. B) Effects of different doses of varenicline or vehicle when combined with ketamine on the number of perseverative errors. (C) Effects of different doses varenicline or vehicle when combined with ketamine on the number of regressive errors. In these studies, varenicline was administered orally 60 min before testing and ketamine was administered by i.m. injection 45 min before testing. Each bar represents the mean ± S.E.M. *p<0.05, **p<0.01, ***p<0.001 = significant difference from vehicle-related response. #p<0.05, ##p<0.01, ###p<0.001 = significant difference from the ketamine alone response. N=6.
Additional Observations
There were no visible signs of side effects noted with any of the doses of varenicline (when administered alone) that were evaluated. The animals’ behaviors appeared normal throughout the study, they were alert, they moved and climbed around their cages normally, and they ate all of their regular food later in the afternoon after DMTS testing. The research technicians also noted that all of the test subjects took (and consumed) food treats throughout the study period. In the reversal learning studies, there were two cases (both in the same monkey, #V6T) where vomiting occurred after ketamine and varenicline combinations were administered. In the first instance, this occurred 3 hr after the ketamine injection (and did not interfere with behavioral testing) and in the second instance vomiting occurred approximately 1 hr after the ketamine injection and it prevented completion of testing on that particular day.
Discussion
The results of this study can be summarized as follows: 1) In both the old monkeys in Cohort 1 and the young/middle-aged monkeys in Cohort 2, there was a delay-dependent decrease in accuracy (under vehicle conditions) when standard DMTS trials (or non-distractor trials in the DMTS-D) were presented and the subjects met the predetermined performance criteria for matching accuracy at each of the three assigned delays, 2) In the DMTS-D, a task-relevant distractor clearly impaired performance at the short delay intervals, in fact, accuracy was decreased to near chance levels of performance. 3) In the DMTS and DMTS-D tasks the doses of varenicline that were evaluated were not associated with statistically significant effects on performance; however, individualized “optimal doses” (based on the best overall performance in each animal in the dose-effect series) were effective when repeated on a separate occasion. 3). In reversal learning studies, ketamine 3.0 mg/kg significantly impaired task accuracy and increased perseverative responding, effects that were attenuated by all three doses of varenicline.
For preclinical evaluations of varenicline for repurposing in disorders of cognition, we chose monkeys (specifically macaques) due to their unique translational value and similarities to humans (genetic homology, brain anatomy, behavioral repertoire, etc.). The fact that many of the monkeys we used were aged or middle-aged has relevance to conditions where older age is a major factor (e.g., AD, MCI). Importantly, as macaques age, like humans, their performance across multiple domains of cognition declines and they exhibit a variety of age-related changes in the brain that are similar to humans (e.g., neuronal loss, amyloid plaques, reactive glia, decreased neurotransmitters, etc.). Please see a more detailed discussion of the translational value of macaques and the effects of aging in our previous manuscript, Callahan et al. 2013.
For the behavioral assessments of varenicline we chose the delay-dependent DMTS test as a working/short term memory task that employs several mnemonic processes (stimulus discrimination, encoding, retention, etc.) that are critical to human attention, memory for recent events, executive function, etc. (see review, Paule et al. 1998). Various versions of the DMTS procedure have been used in humans to assess the effects of aging as well as a variety of illnesses on cognitive function including AD, Lewy Body Dementia, Korsakoff’s Disease, unipolar depression, and alcoholism, (Oscar-Berman and Bonner 1985; Irle et al. 1987; Aggleton et al. 1988; Sahgal et al. 1992; Perryman and Fitten 1993; Elliott et al. 1996). The distractor version of the DMTS (DMTS-D) was employed in Cohort 2 to increase task difficulty and to evaluate the animals’ susceptibility to distraction (a factor that is also relevant to many disorders of cognition). It is believed that the presentation of distractors during the delay or recall interval (i.e., a time during which selective attention and rehearsing are thought to be important), disrupts the cognitive processes that subserve working memory (see Rodriguez and Paule 2009). The results of our studies using the DMTS and DMTS-D paradigms, therefore, suggest that varenicline has the potential to improve working/short term memory and to reduce distractibility in conditions where these domains of cognition are impaired. Here it is important to note that these conclusions should be viewed with some caution since they are based on selected (albeit replicated) optimal doses. We have used this approach in multiple studies due to the heterogeneity of the test subjects available and the consequent variability in the degree (and dose-range) of drug efficacy, pharmacokinetics, and other factors that are not often encountered in rodents and other animal subjects (i.e., where the age, gender, and weight, can be tightly controlled and the numbers available are not a major challenge). As a general comparison of drug efficacy we have provided the “best dose” results across several nAChR ligands that we have evaluated in DMTS and DMTS-D studies (including varenicline). The criteria for inclusion of a drug in the in the table were that a minimum of 6 animals were tested, and that the most improved delay was “long” for DMTS and “Short” for DMTS-D (as we have most often observed with nAChR agonists in the past). It should be noted that there were some differences across the studies (i.e., number of delays presented, the brand of the touch panels used, the drug route of administration, and the species of macaque evaluated ( i.e., rhesus versus pigtail).
We employed a reversal learning task with ketamine impairment in Cohort 3 for several reasons. Successful reversal learning requires “cognitive flexibility” which is commonly impaired in neurological and psychiatric disorders including AD, Parkinson’s disease, Huntington disease, autism, Rett syndrome, Tourette syndrome, and schizophrenia (Baddeley et al. 2001; Elliott et al. 1995; Gauntlett-Gilbert et al. 1999; Hill 2004; Josiassen et al. 1983; Pantelis et al. 1999; Traykov et al. 2007; Verte et al. 2005). Reversal learning requires the inhibition of a previously successful (learned) response strategy to a specific set of contingencies and the acquisition of a different response strategy to a new set of contingencies during the reversal phase (Pisa and Cyr 1990; Dias et al. 1997; Watson et al 2006). The inability to suppress the previously successful response is characterized by an increase in response perseveration (i.e., perseverative errors), whereas the inability to acquire the new, competing rule is characterized by an increase in regressive errors (i.e., errors observed later in the reversal session after the initial perseveration period has ended, see Palencia and Ragozzino 2004). Our use of ketamine to impair reversal learning in this study was based on the well-established literature where NMDA receptor antagonists, including ketamine, phencyclidine (PCP), and MK-801 lead to symptoms that resemble schizophrenia including impairments in cognition (Gilmour et al. 2012). Notably, the use of NMDA antagonists in reversal learning paradigms is now a common approach to modelling the deficits in cognitive flexibility in schizophrenia (see Jentsch and Taylor 2001; Neill et al. 2010; Gastambide et al. 2013a,b). The results of our reversal learning studies, therefore suggest that varenicline has the potential to improve cognitive flexibility in conditions such as schizophrenia where it is often impaired.
Finally, we chose varenicline as a potential drug to be repurposed for disorders of cognition based on its receptor pharmacology and the large body of evidence that nicotine and other ligands at nicotinic acetylcholine receptors (nAChRs) have pro-cognitive effects and other properties that would potentially be useful in neuropsychiatric conditions (reviewed Levin et al. 2006). Both α4β2 and α7 nAChRs are considered viable targets of pro-cognitive agents and varenicline is a potent partial agonist at α4β2 nAChRs as well as a potent full agonist at α7 nAChRs (Mihalak et al. 2006). As noted in the Introduction, varenicline has been shown to improve sustained attention, recognition memory, and sensorimotor gating in rats (Rollema et al. 2009), as well as to improve working memory in monkeys that self-administer cocaine (Gould et al., 2013). Collectively, these data combined with our results in aged and middle-aged monkeys (indicating improvements in working/short term memory, distractibility, and cognitive flexibility) suggest that varenicline might have therapeutic potential for the impairments of information processing and cognition observed in age-related illness such as AD and MCI as well as neuropsychiatric illnesses that are not necessarily associated with advanced aged (e.g. schizophrenia, drug dependence).
Table 2.
Comparison of Optimal Doses of nAChR agonists on Matching Accuracy in Monkeys
| Drug
|
nAChR Activity
|
N
|
Task
|
Age
|
Delay
|
Average % Change from Baseline
|
|---|---|---|---|---|---|---|
| nicotine | nonselective agonist | 10 | DMTS | Adult | Long | 15.1 |
| ABT-418 | α4β2 agonist | 6 | DMTS | Aged | Long | 15.7 |
| ABT-089 | α4β2 partial agonist | 6 | DMTS | Aged | Long | 12.7 |
| ABT-594 | α4β2 agonist | 7 | DMTS | Adult | Long | 11.3 |
| A-582941 | α7 agonist | 7 | DMTS | Adult | Long | 22.0 |
| varenicline | α4β2 partial agonist | 8 | DMTS | Aged | Long | 13.6 |
| α7 full agonist | ||||||
| nicotine | nonselective agonist | 8 | DMTS-D | Adult | Short | 17.5 |
| ABT-418 | α4β2 agonist | 8 | DMTS-D | Adult | Short | 17.5 |
| ABT-089 | α4β2 partial agonist | 8 | DMTS-D | Adult | Short | 34.4 |
| ABT-594 | α4β2 agonist | 7 | DMTS-D | Adult | Short | 12.0 |
| varenicline | α4β2 partial agonist | 8 | DMTS-D | Adult | Short | 19.6 |
| α7 full agonist |
Abbreviations: nAChR, nicotinic acetylcholine receptor; DMTS, delayed match to sample; DMTS-D, delayed match to sample with distractors
Adult = 7–18 years old; aged = >19 years old
Acknowledgments
Funding source: This work was supported in part by the National Institute on Drug Abuse [Grant R01-DA029127] and by Prime Behavior Testing Laboratories, Inc., Evans, Georgia
The authors would like to thank Ms. Ashley Davis for her administrative assistance in preparing this article and the Division of Laboratory Animal Services (DLAS) at Georgia Regents University for their dedication to the care, husbandry, and enrichment of the non-human primate subjects used in this study.
Footnotes
Conflict of interest The authors do not declare any conflict of interest.
References
- Aggleton JP, Nicol RM, Huston AE, Fairbairn AF. The performance of amnesic subjects on tests of experimental amnesia in animals: delayed matching-to-sample and concurrent learning. Neuropsychologia. 1988;26(2):265–72. doi: 10.1016/0028-3932(88)90079-6. [DOI] [PubMed] [Google Scholar]
- Ashburn TT, Thor KB. Drug repositioning: identifying and developing new uses for existing drugs. Nat Rev Drug Discov. 2004;3(8):673–83. doi: 10.1038/nrd1468. [DOI] [PubMed] [Google Scholar]
- Baddeley AD. Is working memory still working? American Psychologist. 2001;56(11):851–864. doi: 10.1037/0003-066x.56.11.851. [DOI] [PubMed] [Google Scholar]
- Dias R, Robbins TW, Roberts AC. Dissociable forms of inhibitory control within prefrontal cortex with an analog of the Wisconsin Card Sort Test: restriction to novel situations and independence from "on-line" processing. J Neurosci. 1997;17(23):9285–97. doi: 10.1523/JNEUROSCI.17-23-09285.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott R, McKenna PJ, Robbins TW, Sahakian BJ. Neuropsychological evidence for frontostriatal dysfunction in schizophrenia. Psychol Med. 1995;25(3):619–30. doi: 10.1017/s0033291700033523. [DOI] [PubMed] [Google Scholar]
- Elliott R, Sahakian BJ, McKay AP, Herrod JJ, Robbins TW, Paykel ES. Neuropsychological impairments in unipolar depression: The influence of perceived failure on subsequent performance. Psychol Med. 1996;26:975–89. doi: 10.1017/s0033291700035303. [DOI] [PubMed] [Google Scholar]
- Gastambide F, Mitchell SN, Robbins TW, Tricklebank MD, Gilmour G. Temporally distinct cognitive effects following acute administration of ketamine and phencyclidine in the rat. Eur Neuropsychopharmacol. 2013;23(11):1414–22. doi: 10.1016/j.euroneuro.2013.03.002. [DOI] [PubMed] [Google Scholar]
- Gastambide F, Gilmour G, Robbins TW, Tricklebank MD. The mGlu5 positive allosteric modulator LSN2463359 differentially modulates motor, instrumental and cognitive effects of NMDA receptor antagonists in the rat. Neuropharmacology. 2013;64:240–7. doi: 10.1016/j.neuropharm.2012.07.039. [DOI] [PubMed] [Google Scholar]
- Gauntlett-Gilbert J, Roberts RC, Brown VJ. Mechanisms underlying attentional set-shifting in Parkinson's disease. Neuropsychologia. 1999;37(5):605–16. doi: 10.1016/s0028-3932(98)00049-9. [DOI] [PubMed] [Google Scholar]
- Gilmour G, Dix S, Fellini L, Gastambide F, Plath N, Steckler T, Talpos J, Tricklebank M. NMDA receptors, cognition and schizophrenia--testing the validity of the NMDA receptor hypofunction hypothesis. Neuropharmacology. 2012;62(3):1401–12. doi: 10.1016/j.neuropharm.2011.03.015. [DOI] [PubMed] [Google Scholar]
- Gould RW, Garg PK, Garg S, Nader MA. Effects of nicotinic acetylcholine receptor agonists on cognition in rhesus monkeys with a chronic cocaine self-administration history. Neuropharmacology. 2013;64:479–88. doi: 10.1016/j.neuropharm.2012.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill K, Mann L, Laws KR, Stephenson CM, Nimmo-Smith I, McKenna PJ. Hypofrontality in schizophrenia: a meta-analysis of functional imaging studies. Acta Psychiatr Scand. 2004;110(4):243–56. doi: 10.1111/j.1600-0447.2004.00376.x. [DOI] [PubMed] [Google Scholar]
- Irle E, Kessler J, Markowitsch HJ, Hofmann W. Primate learning tasks reveal strong impairments in patients with presenile or senile dementia of the Alzheimer type. Brain Cogn. 1987;6(4):429–49. doi: 10.1016/0278-2626(87)90138-2. [DOI] [PubMed] [Google Scholar]
- Jentsch JD, Taylor JR. Impaired inhibition of conditioned responses produced by subchronic administration of phencyclidine to rats. Neuropsychopharmacology. 2001;24(1):66–74. doi: 10.1016/S0893-133X(00)00174-3. [DOI] [PubMed] [Google Scholar]
- Jones GM, Sahakian BJ, Levy R, Warburton DM, Gray JA. Effects of acute subcutaneous nicotine on attention, information processing and short-term memory in Alzheimer's disease. Psychopharmacology (Berl) 1992;108(4):485–94. doi: 10.1007/BF02247426. [DOI] [PubMed] [Google Scholar]
- Josiassen RC, Curry LM, Mancall EL. Development of neuropsychological deficits in Huntington's disease. Arch Neurol. 1983;40(13):791–6. doi: 10.1001/archneur.1983.04050120041005. [DOI] [PubMed] [Google Scholar]
- Kaitin KI, DiMasi JA. Pharmaceutical innovation in the 21st century: new drug approvals in the first decade, 2000–2009. Clin Pharmacol Ther. 2011;89(2):183–8. doi: 10.1038/clpt.2010.286. [DOI] [PubMed] [Google Scholar]
- Kim SY, Choi SH, Rollema H, Schwam EM, McRae T, Dubrava S, Jacobsen J. Phase II crossover trial of varenicline in mild-to-moderate Alzheimer's disease. Dement Geriatr Cogn Disord. 2014;37(3–4):232–45. doi: 10.1159/000355373. [DOI] [PubMed] [Google Scholar]
- Levin ED, Lawrence S, Petro A, Horton K, Seidler FJ, Slotkin TA. Increased nicotine self-administration following prenatal exposure in female rats. Pharmacol Biochem Behav. 2006;85(3):669–74. doi: 10.1016/j.pbb.2006.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loughead J, Ray R, Wileyto EP, Ruparel K, Sanborn P, Siegel S, Gur RC, Lerman C. Effects of the alpha4beta2 partial agonist varenicline on brain activity and working memory in abstinent smokers. Biol Psychiatry. 2010;67(8):715–21. doi: 10.1016/j.biopsych.2010.01.016. [DOI] [PubMed] [Google Scholar]
- Medina-Franco JL, Giulianotti MA, Welmaker GS, Houghten RA. Shifting from the single to the multitarget paradigm in drug discovery. Drug Discov Today. 2013;8(9–10):495–501. doi: 10.1016/j.drudis.2013.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merino A, Bronowska AK, Jackson DB, Cahill DJ. Drug profiling: knowing where it hits. Drug Discov Today. 2010;15(17–18):749–56. doi: 10.1016/j.drudis.2010.06.006. [DOI] [PubMed] [Google Scholar]
- Mihalak KB, Carroll FI, Luetje CW. Varenicline is a partial agonist at alpha4beta2 and a full agonist at alpha7 neuronal nicotinic receptors. Mol Pharmacol. 2006;70(3):801–5. doi: 10.1124/mol.106.025130. [DOI] [PubMed] [Google Scholar]
- Mocking RJ, Patrick Pflanz C, Pringle A, Parsons E, McTavish SF, Cowen PJ, Harmer CJ. Effects of short-term varenicline administration on emotional and cognitive processing in healthy, non-smoking adults: a randomized, double-blind, study. Neuropsychopharmacology. 2013;38(3):476–84. doi: 10.1038/npp.2012.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neill JC, Barnes S, Cook S, Grayson B, Idris NF, McLean SL, Snigdha S, Rajagopal L, Harte MK. Animal models of cognitive dysfunction and negative symptoms of schizophrenia: focus on NMDA receptor antagonism. Pharmacol Ther. 2010;128(3):419–32. doi: 10.1016/j.pharmthera.2010.07.004. [DOI] [PubMed] [Google Scholar]
- Newhouse PA, Sunderland T, Tariot PN, Blumhardt CL, Weingartner H, Mellow A, Murphy DL. Intravenous nicotine in Alzheimer's disease: a pilot study. Psychopharmacology (Berl) 1988;95(2):171–5. doi: 10.1007/BF00174504. [DOI] [PubMed] [Google Scholar]
- Newhouse P, Kellar K, Aisen P, White H, Wesnes K, Coderre E, Pfaff A, Wilkins H, Howard D, Levin ED. Nicotine treatment of mild cognitive impairment: a 6-month double-blind pilot clinical trial. Neurology. 2012;78(2):91–101. doi: 10.1212/WNL.0b013e31823efcbb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oscar-Berman M, Bonner RT. Matching- and delayed matching-to-sample performance as measures of visual processing, selective attention, and memory in aging and alcoholic individuals. Neuropsychologia. 1985;23(5):639–51. doi: 10.1016/0028-3932(85)90065-x. [DOI] [PubMed] [Google Scholar]
- Palencia CA, Ragozzino ME. The influence of NMDA receptors in the dorsomedial striatum on response reversal learning. Neurobiol Learn Mem. 2004;82(2):81–9. doi: 10.1016/j.nlm.2004.04.004. [DOI] [PubMed] [Google Scholar]
- Pantelis C, Barber FZ, Barnes TR, Nelson HE, Owen AM, Robbins TW. Comparison of set-shifting ability in patients with chronic schizophrenia and frontal lobe damage. Schizophr Res. 1999;37(3):251–70. doi: 10.1016/s0920-9964(98)00156-x. [DOI] [PubMed] [Google Scholar]
- Paule MG, Bushnell PJ, Maurissen JP, Wenger GR, Buccafusco JJ, Chelonis JJ, Elliott R. Symposium overview: the use of delayed matching-to-sample procedures in studies of short-term memory in animals and humans. Neurotoxicol Teratol. 1998;20(5):493–502. doi: 10.1016/s0892-0362(98)00013-0. [DOI] [PubMed] [Google Scholar]
- Perryman KM, Fitten LJ. Delayed matching-to-sample performance during a double-blind trial of tacrine (THA) and lecithin in patients with Alzheimer's disease. Life Sci. 1993;53(6):479–86. doi: 10.1016/0024-3205(93)90699-4. [DOI] [PubMed] [Google Scholar]
- Pisa M, Cyr J. Regionally selective roles of the rat's striatum in modality-specific discrimination learning and forelimb reaching. Behav Brain Res. 1990;37(3):281–92. doi: 10.1016/0166-4328(90)90140-a. [DOI] [PubMed] [Google Scholar]
- Powledge TM. Nicotine as Therapy. PLoS Biology. 2004;2(11):e404. doi: 10.1371/journal.pbio.0020404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price DL, Sisodia SS. Cellular and molecular biology of Alzheimer's disease and animal models. Annu Rev Med 1994. 1994;45:435–46. doi: 10.1146/annurev.med.45.1.435. [DOI] [PubMed] [Google Scholar]
- Ragozzino ME, Detrick S, Kesner RP. Involvement of the prelimbic-infralimbic areas of the rodent prefrontal cortex in behavioral flexibility for place and response learning. J Neurosci. 1999;19(11):4585–94. doi: 10.1523/JNEUROSCI.19-11-04585.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riordan HJ, Cutler NR. The death of CNS drug development: Overstatement or Omen? J Clin Stud. 2012;3:12–5. [Google Scholar]
- Rodriguez JS, Paule MG. Working Memory Delayed Response Tasks in Monkeys. In: Buccafusco JJ, editor. Methods of Behavior Analysis in Neuroscience. 2. Chapter 12. Boca Raton (FL): CRC Press; 2009. [PubMed] [Google Scholar]
- Rollema H, Hajós M, Seymour PA, Kozak R, Majchrzak MJ, Guanowsky V, Horner WE, Chapin DS, Hoffmann WE, Johnson DE, McLean S, Freeman J, Williams KE. Preclinical pharmacology of the alpha4beta2 nAChR partial agonist varenicline related to effects on reward, mood and cognition. Biochem Pharmacol. 2009;78(7):813–24. doi: 10.1016/j.bcp.2009.05.033. [DOI] [PubMed] [Google Scholar]
- Sahakian BJ, Jones GMM. The effects of nicotine on attention, information processing, and working memory in patients with dementia of the Alzheimer type. In: Adlkofer F, Thruau K, editors. Effects of Nicotine on Biological Systems. Basel: Birkhauser Verlag; 1991. pp. 623–630. [Google Scholar]
- Sahgal A, Galloway PH, McKeith IG, Lloyd S, Cook JH, Ferrier IN, Edwardson JA. Matching-to-sample deficits in patients with senile dementias of the Alzheimer and Lewy body types. Arch Neurol. 1992;49(10):1043–6. doi: 10.1001/archneur.1992.00530340059019. [DOI] [PubMed] [Google Scholar]
- Shim JC, Jung DU, Jung SS, Seo YS, Cho DM, Lee JH, Lee SW, Kong BG, Kang JW, Oh MK, Kim SD, McMahon RP, Kelly DL. Adjunctive varenicline treatment with antipsychotic medications for cognitive impairments in people with schizophrenia: a randomized double-blind placebo-controlled trial. Neuropsychopharmacology. 2012;37(3):660–8. doi: 10.1038/npp.2011.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith RC, Lindenmayer JP, Davis JM, Cornwell J, Noth K, Gupta S, Sershen H, Lajtha A. Cognitive and antismoking effects of varenicline in patients with schizophrenia or schizoaffective disorder. Schizophr Res. 2009;110(1–3):149–55. doi: 10.1016/j.schres.2009.02.001. [DOI] [PubMed] [Google Scholar]
- Taylor JR, Roth RH, Sladek JR, Jr, Redmond DE., Jr Cognitive and motor deficits in the performance of an object retrieval task with a barrier-detour in monkeys (Cercopithecus aethiops sabaeus) treated with MPTP: long-term performance and effect of transparency of the barrier. Behav Neurosci. 1990;104(4):564–76. doi: 10.1037//0735-7044.104.4.564. [DOI] [PubMed] [Google Scholar]
- Terry AV, Jr, Risbrough VB, Buccafusco JJ, Menzaghi F. Effects of (+/−)-4-[[2-(1-methyl-2-pyrrolidinyl)ethyl]thio]phenol hydrochloride (SIB-1553A), a selective ligand for nicotinic acetylcholine receptors, in tests of visual attention and distractibility in rats and monkeys. J Pharmacol Exp Ther. 2002;301(1):284–92. doi: 10.1124/jpet.301.1.284. [DOI] [PubMed] [Google Scholar]
- Terry AV, Jr, Buccafusco JJ, Bartoszyk GD. Selective serotonin 5-HT2A receptor antagonist EMD 281014 improves delayed matching performance in young and aged rhesus monkeys. Psychopharmacology (Berl) 2005;179(4):725–32. doi: 10.1007/s00213-004-2114-1. [DOI] [PubMed] [Google Scholar]
- Traykov L, Raoux N, Latour F, Gallo L, Hanon O, Baudic S, Bayle C, Wenisch E, Remy P, Rigaud AS. Executive functions deficit in mild cognitive impairment. Cogn Behav Neurol. 2007;20(4):219–24. doi: 10.1097/WNN.0b013e31815e6254. [DOI] [PubMed] [Google Scholar]
- Verté S, Geurts HM, Roeyers H, Oosterlaan J, Sergeant JA. Executive functioning in children with autism and Tourette syndrome. Dev Psychopathol. 2005;17(2):415–45. doi: 10.1017/s0954579405050200. [DOI] [PubMed] [Google Scholar]
- Watson DJ, Sullivan JR, Frank JG, Stanton ME. Serial reversal learning of position discrimination in developing rats. Dev Psychobiol. 2006;48(1):79–94. doi: 10.1002/dev.20106. [DOI] [PubMed] [Google Scholar]
- Webster SJ, Wilson CA, Lee CH, Mohler EG, Terry AV, Jr, Buccafusco JJ. The acute effects of dimebolin, a potential Alzheimer's disease treatment, on working memory in rhesus monkeys. Br J Pharmacol. 2011;164(3):970–8. doi: 10.1111/j.1476-5381.2011.01432.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White HK, Levin ED. Four-week nicotine skin patch treatment effects on cognitive performance in Alzheimer's disease. Psychopharmacology (Berl) 1999;143(2):158–65. doi: 10.1007/s002130050931. [DOI] [PubMed] [Google Scholar]
- Wilson AL, Langley LK, Monley J, Bauer T, Rottunda S, McFalls E, Kovera C, McCarten JR. Nicotine patches in Alzheimer's disease: pilot study on learning, memory, and safety. Pharmacol Biochem Behav. 1995;51(2–3):509–14. doi: 10.1016/0091-3057(95)00043-v. [DOI] [PubMed] [Google Scholar]
- Zhang L. Cholinergic Receptor Knockout Mice. In: Levin ED, Buccafusco JJ, editors. Animal Models of Cognitive Impairment. Chapter 11. Boca Raton (FL): CRC Press; 2006. Frontiers in Neuroscience. [Google Scholar]