Abstract
Empirical evidence has identified several risk factors for panic psychopathology, including smoking and anxiety sensitivity (AS; the fear of anxiety-related sensations). Smokers with elevated AS are therefore a particularly vulnerable population for panic. Yet, there is little knowledge about how to reduce risk of panic among high AS smokers. The present study prospectively evaluated panic outcomes within the context of a controlled randomized risk reduction program for smokers. Participants (N = 526) included current smokers who all received a state-of-the-art smoking cessation intervention with approximately half randomized to the AS reduction intervention termed Panic-smoking Program (PSP). The primary hypotheses focus on examining the effects of a PSP on panic symptoms in the context of this vulnerable population. Consistent with prediction, there was a significant effect of treatment condition on AS, such that individuals in the PSP condition, compared to those in the control condition, demonstrated greater decreases in AS throughout treatment and the follow-up period. In addition, PSP treatment resulted in lower rates of panic-related symptomatology. Moreover, mediation analyses indicated that reductions in AS resulted in lower panic symptoms. The present study provides the first empirical evidence that brief, targeted psychoeducational interventions can mitigate panic risk among smokers.
Keywords: anxiety sensitivity, intervention, panic, prevention, smokers
Empirical evidence suggests that panic attacks and anxiety problems co-occur with smoking at rates that exceed those found in the general non-psychiatric population. For instance, Lasser et al. (2000) found that in an analysis of over 4,000 respondents from the National Comorbidity Survey (NCS), current smoking rates for respondents with panic disorder (PD) in the past month or lifetime were significantly greater than smoking rates among respondents with no mental illness. Moreover, reported rates of smoking were highest among individuals with panic-related problems (i.e., history of panic attacks) and other anxiety disorders where panic attacks are common (i.e., posttraumatic stress disorder and generalized anxiety disorder). In regard to smoking contributing to panic specifically, data suggest that smoking initiation typically precedes the onset of panic-related problems (Breslau, Johnson, Hiripi, & Kessler, 2001). For example, Breslau and Klein (1999) tested the association between daily smoking and risk for panic attacks and PD. Results indicated that there was a significant lifetime association between daily smoking and onset of panic attacks and PD; daily smokers were almost 4 times more apt to experience panic attacks and 13 times more likely to develop PD after controlling for major depression and gender.
An integrated theoretical model has been developed to specify how smoking and panic factors are hypothesized to relate to one another (Zvolensky & Schmidt, 2003). In particular, research suggests that among certain daily smokers, smoking serves important affect regulatory functions. This is particularly true for smokers who fear anxiety such as those high in AS. AS, otherwise known as a fear of fear, is a trait like characteristic reflecting a propensity to fear anxiety-related sensations due to the belief that these symptoms have harmful physical, cognitive, and/or social consequences (Reiss & McNally, 1985). At this point in time, AS is perhaps the best-established cognitive causal risk factor for anxiety and panic-spectrum psychopathology (McNally, 2002). In fact, AS is now recognized in the DSM-V as a risk factor for panic (American Psychiatric Association, 2013). One notable aspect of the AS scientific literature is that it comprises both cross-sectional and laboratory tests that have utilized a diverse array of methodological approaches and assessment modalities. In regard to cross-sectional tests, for example, there is consistent evidence that AS, as measured by preexposure to biological challenge (panic provocation), is a significant predictor of postchallenge anxiety symptoms and panic attacks among nonclinical individuals (McNally & Eke, 1996). These effects are apparent from adolescence through adulthood (Leen-Feldner, Feldner, Bernstein, McCormick, & Zvolensky, 2005; Rabian, Embry, & MacIntyre, 1999; Schmidt, Lerew, & Jackson, 1997; Zvolensky, Feldner, Eifert, & Stewart, 2001).
Prospective investigations similarly suggest AS predicts the future onset of unexpected panic attacks for adolescents (Hayward, Killen, Kraemer, & Taylor, 2000; Weems, Hayward, Killen, & Taylor, 2002) and adults (Schmidt et al., 1997; Schmidt, Lerew, & Jackson, 1999). The prospective studies also suggest that these effects are apparent for other anxiety symptoms (Schmidt et al., 1997, 1999). Though less well-studied, there are two reports that suggest that AS is related to the future development of anxiety psychopathology, with some degree of specificity for panic disorder relative to other anxiety conditions (Maller & Reiss, 1992; Schmidt, Zvolensky, & Maner, 2006). Collectively, extant findings indicate AS is associated concurrently and prospectively with anxiety symptoms, panic attack symptoms, and full-blown panic attacks.
AS is also thought to influence smoking behavior among daily cigarette smokers. Specifically, these individuals expect tobacco use to help alleviate aversive anxiety states and are often motivated to smoke for affect regulation purposes (Zvolensky et al., 2005). As the mood-altering qualities of smoking are complex (Parrott, 1999), it may well be useful to conceptualize these processes at the cognitive level of analysis. Thus, in the absence of other more adaptive coping strategies, panic-vulnerable smokers may learn to rely on smoking to manage anxiety states and fears of bodily sensations in the short-term. Over longer periods of time, however, smoking itself will lead to increased risk of bodily sensations and aversive internal states via a number of routes, including nicotine-based withdrawal symptoms, health impairment, and physical illness. Exposure to these types of aversive stimuli may facilitate learning that internal cues can be personally harmful, dangerous, and anxiety-evoking. Although smokers with pre-morbid vulnerability factors like high AS may be particularly motivated to quit smoking, they are at high risk for problems in quitting (Zvolensky, Stewart, Vujanovic, Gavric, & Steeves, 2009). Specifically, these persons are apt to be particularly fearful of, and emotionally reactive to, internal states that occur during smoking discontinuation; they may therefore experience more distressing emotional experiences in cessation attempts (Farris, Langdon, DiBello, & Zvolensky, 2015). Thus, a forward feedback loop may develop, whereby smoking is used as a coping strategy for managing aversive states among high AS individuals in the short term yet paradoxically confers longer-term risk for panic attacks and other anxiety problems. This perspective suggests daily smokers are an “at risk” population for panic and other anxiety-related problems and it is important to target them for preventative intervention, as it could lead to improvement in both anxiety status and smoking behavior.
Given findings suggesting AS is a risk for panic and related problems (e.g., smoking), researchers have begun to evaluate the relevance of AS to preventative interventions by determining to what extent this cognitive factor can be changed (malleability). For example, a number of clinical trials with anxiety patients indicate that AS can be reduced through cognitive behavioral interventions. Several investigations focused on panic disorder treatment have reported significant reductions in AS following treatment (Barlow, Craske, Cerny, & Klosko, 1989; Schmidt et al., 2000; Telch et al., 1993; Westling & Öst, 1999). This work is complemented by investigations specifically focused on the reduction of AS as a preventative intervention in nonclinical, at risk samples. Successful preventative work on AS has included two-hour psychoeducation groups (Feldner, Zvolensky, Babson, Leen-Feldner, & Schmidt, 2008), through single day workshops (Gardenswartz & Craske, 2001), and six week exercise programs (Broman-Fulks & Storey, 2008).
To date, the largest AS focused preventative intervention was conducted by Schmidt and colleagues (2007). Participants (N = 404) with ASI scores 1.5 SDs above the nonclinical mean (Schmidt & Joiner, 2002) were randomly assigned to either the Anxiety Sensitivity Amelioration Training (ASAT) condition or a health and nutrition based control condition. The ASAT condition consisted of a 30-minute computer PowerPoint presentation followed by ten minutes with an experimenter. The presentation explored the following concepts: the nature of stress, AS, myths about the harmfulness of physiological arousal, and interoceptive exercises (IE). Results indicate that both conditions produced a reduction in AS; however, the ASAT condition produced a significantly larger reduction in AS than the control condition (30% vs. 17%, respectively). In terms of the development of psychopathology, those in the ASAT condition showed a lower incidence of Axis I diagnoses during the two-year follow-up period.
Recently, an augmented version of ASAT was developed in an attempt to increase its potency (Keough & Schmidt, 2012). The revised protocol, Anxiety Sensitivity Education and Reduction Training (ASERT), included more interaction with a therapist, more intensive IE exercises, and more rigorous homework requirements. The level of overall AS reduction was substantial in the active ASERT group (close to 60% at one-month follow-up). A six-month follow-up assessment indicated that the treatment group retained the majority of their AS reduction, whereas the control group retained their elevated AS scores. Finally, Schmidt and colleagues (2014) showed that a one session, computer-administered version of ASAT with no therapist involvement was also successful in producing substantial reductions in AS that persisted during a one-month follow-up. In summary, we now have emerging evidence that AS can be effectively mitigated, even with very brief one-session treatments that require minimal therapist or experimenter involvement.
From an intervention standpoint, empirical and theoretical work on smoking and panic problems suggests it may be fruitful to simultaneously and concurrently target these risk factors (i.e., AS and smoking) in one overarching model to reduce panic problems while also stimulating cessation-oriented behavior (e.g., enhance motivation to quit). Because panic factors and smoking interact in clinically meaningful ways, addressing one of these factors without addressing the other in this same context may not result in optimal efficacy regarding intervention goals. For example, simply targeting the cognitive-based fear of anxiety (AS) without a recognition of smoking among those who often manage affect by smoking neglects clinically-relevant self-regulation processes (e.g., escape and avoidant coping for emotionally salient events). Alternatively, because AS is related to poorer success in quitting smoking (Brown, Kahler, Zvolensky, Lejuez, & Ramsey, 2001), a failure to target this cognitive-based affective vulnerability may yield lower rates of success in cessation. Thus, smoking should theoretically be directly targeted within the context of clinical intervention for preventing panic attacks and PD. In terms of addressing smoking and psychological factors, integrative programs are predominant (Brown, Kahler, Niaura, et al., 2001; Cinciripini et al., 1995; Hall, Muñoz, & Reus, 1994). This integrative focus for treatment planning is consistent with the larger literature on systems of integrated, concurrent care for individuals with co-occurring addictive and mental disorders (Mueser & Kavanagh, 2004; Osher, 1996; Pechter & Miller, 1997). Moreover, it is consonant with therapeutic models for anxiety disorders and comorbid addictions that have targeted AS while simultaneously altering drug behavior (Otto et al., 1993).
The present proposal aims to fill an important gap in the existing literature by prospectively evaluating panic outcomes within the context of a controlled randomized risk reduction program for smokers. The risk reduction program, implemented across two sites, targeted two well-established risk factors for the development of panic: smoking and AS. All participants received a state-of-the-art smoking cessation intervention with approximately half randomized to the AS reduction intervention termed Panic-smoking Program (PSP).
The primary hypotheses focus on examining the effects of a PSP on panic symptoms in the context of a vulnerable population (i.e., smokers). We hypothesized that participants in the active treatment (PSP) would show greater reductions in AS as well as reduced severity of panic, compared to those individuals receiving only the standard smoking cessation intervention. Moreover, we expected changes in AS would mediate symptom improvement over time.
Method
Participants
The sample consisted of 529 treatment-seeking adult daily smokers recruited from the community to participate in a large randomized controlled trial examining the efficacy of two smoking cessation interventions. All participants were recruited from two sites (University of Vermont and Florida State University; clinicaltrials.gov #NCT01753141). To be eligible for inclusion participants had to be 18 years of age or older, daily cigarette users (e.g., average ≥ 8 cigarettes per day for at least 1 year), and report a motivation to quit smoking (e.g., at least 5 on a 10-point scale). Additionally, individuals with a psychotic disorder, uncontrolled bipolar disorder, serious suicidal intent that warranted hospitalization or immediate treatment, or those using another smoking cessation program or tobacco product, were excluded.
Participants ages ranged from 18–68 (M = 38.23, SD = 13.56) and gender was fairly evenly distributed (45.9% males). The sample was primarily Caucasian (75.4%) with 9.5% African American, 3.4% Hispanic, .9% Asian, 1.7% Other (e.g., biracial), and 9.1% failed to respond. Regarding level of education, 5.3% completed some high school, 19.8% had a high school diploma or the equivalent, 30.2% completed some college, 9.3% graduated from a 2 year college, 13.4% graduated from a 4 year college, 4.9% completed professional school, 7.9% had a graduate degree, and 9.2% failed to respond. Finally, participants reported smoking 16.56 (SD = 9.55) cigarettes per day and had been smoking for an average of 19.66 years (SD = 13.44)
Assessments
Clinician Administered
Structured Clinical Interview for DSM-IV (SCID)
The SCID is a well-validated and widely used structured interview designed to assess for the presence of DSM-IV Axis I diagnoses (First, Spitzer, Gibbon, & Williams, 1997). All SCIDs were administered by advanced doctoral level therapists who completed extensive training in SCID administration and scoring. Training included reviewing SCID training tapes, observing live SCID administrations, and conducting practice interviews with a trained interviewer. Feedback was provided throughout the training process until all trainees demonstrated high levels of reliability. Additionally, all SCID’s were presented to and reviewed by a licensed clinical psychologist to ensure accurate diagnoses. Interviews were audio-taped and the reliability of a random selection of 12.5% of interviews were checked for accuracy; no cases of (diagnostic coding) disagreement were noted.
Self-report Measures
Demographic and Medical Screening Questionnaire
This scale was created to collect data on participants’ gender, race, educational/occupational level, medical conditions and medications and was administered during the screening to ensure participant eligibility.
Anxiety Sensitivity Index-3 (ASI-3)
The ASI-3 is an 18-item self-report questionnaire designed to measure fears of symptoms associated with anxious arousal (Taylor et al., 2007). The ASI-3 has been demonstrated to be a reliable and valid measure of AS (Farris et al., in press; Taylor et al., 2007) and in the current investigation the ASI-3 total score demonstrated excellent internal consistency at all timepoints (α’s ranged from .91 to .93).
Fagerstrom Test for Nicotine Dependence (FTND)
The FTND is a 6-item scale designed to assess gradations in nicotine dependence (Heatherton, Kozlowski, Frecker, & Fagerström, 1991). Previous research found that the FTND has good internal consistency and test-retest reliability (Heatherton et al., 1991). In the present investigation internal consistency was adequate given the low item count (α = .63).
Panic Disorder Severity Scale (PDSS)
The PDSS is a 7-item self-report measure assessing various symptoms of panic including frequency of attacks, fear and avoidance, as well as impairment in social and occupational domains (Shear et al., 1997). The PDSS is both a reliable and valid measure of panic related symptoms (Houck, Spiegel, Shear, & Rucci, 2002). Additionally, in the current study the PDSS demonstrated excellent internal consistency at all timepoints (α’s ranged from .88 to .94).
Procedure
All procedures were approved by the institutional review boards at both universities. Participants responding to study advertisements were scheduled by phone for an in-person baseline assessment session. Upon arriving at the clinic, participants were evaluated by a trained researcher to determine the inclusion and exclusion criteria listed above. Specifically, participants provided written informed consent and were interviewed using the SCID-NP (Axis I). Following these procedures, participants were randomly assigned to one of the two conditions (see description below) and scheduled for their four 90-min individual treatment sessions as well as each of the 7 follow-up assessment sessions (60–120 minutes).
All therapy sessions were conducted by highly trained clinical psychology doctoral students and were delivered at the respective university psychology clinics. Training included a three-day workshop consisting of 20 hours of didactic instruction that covered study aims and procedures, and treatment protocols. In addition, training included shadowing the principle investigator, watching training tapes, role playing, and completing all four sessions with at least one training participant. Ongoing supervision included reviewing a subset of session videotapes, case discussion, and resolving issues regarding recruitment and eligibility of participants, implementation, and adherence to treatment protocols. A random selection of 20% of the treatment sessions were sampled for adherence by two doctoral-level clinical psychologists not involved in treatment delivery. Adherence ratings were 93%.
Description of the Experimental Conditions
Standard smoking cessation program (SP)
Participants assigned to SP received a smoking cessation intervention based on the most recent clinical practice guideline from the USDHHS, Treating Tobacco Use and Dependence (Fiore et al., 2000) and consensus reports (Abrams & Niaura, 2003). SP was delivered on an individual basis in four 90-minute sessions over a four-week period (1 session per week).
Session 1 focused on the following elements: provision of reinforcement and support for quitting, a discussion of prior quit attempts to identify what strategies contributed to success and what factors hindered success, initiation of self-monitoring cigarette use and noting situational cues for smoking (e.g., times of the day, activities while smoking, and moods). The quit date was set and scheduled to occur on the date of their fourth appointment (upon awakening).
Sessions 2 and 3 focused on the identification of high risk situations that may place them at risk for relapse. For each high-risk situation identified, therapists assisted participants in developing behavioral and cognitive strategies for coping with high-risk situations. Therapists advised all participants to avoid or reduce drinking. Therapists advised participants to enlist social support by telling their friends and family about their quit date. Methods of increasing social support were also discussed. All participants were given a copy of the NCI publication, Clearing the Air USDHHS (1995), which provides strategies for smokers who are trying to quit. Therapists instructed participants in the proper use of the nicotine patch (e.g., placement of patch, use one per day, importance of not smoking while using the patch). Lifestyle changes including stress management, healthy diet, exercise, and increasing pleasant nonsmoking activities were discussed as well to help facilitate participants’ long-term abstinence.
Session 4 (quit day) focused on a discussion of quit experiences, including degree of withdrawal symptoms, strategies used to avoid smoking, and perceived benefits of quitting. Therapists provided support and encouragement for participants who lapse and smoke. Participants who returned to regular smoking were told that a few attempts are often needed before people quit smoking entirely and were asked to set a new quit date and resume use of the patch on that day. Similar to Sessions 2 and 3, the anticipation of high-risk situations, development of social support and lifestyle changes were also discussed as needed.
Panic-Smoking Program (PSP)
The PSP protocol integrated the elements of the SP intervention including nicotine replacement therapy along with the key elements of cognitive-behavioral treatment of AS and panic. Due to the additional intervention content, aspects of the SP intervention were scaled back to equate for contact time (four 90-min sessions). Specifically, the 90 min session included 45 min of SP and 45 min of cognitive-behavioral treatment strategies for AS and panic; however, these components were integrated in a manner that discusses the cyclical types of processes related to both factors (Zvolensky & Bernstein, 2005). In addition to the SP treatment components, sessions included the following components:
Session 1: Therapeutic Rationale and the Process of Anxiety
Participants received a thorough rationale for the PSP intervention focused on the idea that in addition to proven strategies for smoking cessation (SP), the current program will also focus on helping the individual (1) learn and (2) practice strategies that will help them better manage interpreting, coping, and tolerating emergent withdrawal symptoms and anxiety and other negative mood states. Specifically, we introduced the concepts of AS, catastrophizing, and smoking (and other negative affect-based negative-reinforcement behaviors) as a maladaptive way of coping with anxiety-related distress. The process of the forward-feeding anxiety cycle, whereby catastrophic thinking and fears of anxiety sensations can lead to subjective threat evaluations, resulting in panic attacks (presently or in the future) and the exacerbation of interoceptive states like withdrawal symptoms was highlighted. We also indicated such reactions may sensitize a person to the interoceptive and environmental cues that signal such distress in the future, leading to smoking as a way of coping. Finally, we articulated that targeting the fear of anxiety and modifying it via thinking and behavioral exercises is important for enhancing smoking outcomes. In this integrative rationale, we emphasized that practice of exercises in-session and out of session (e.g., IE) would be an important element of the intervention.
Session 2: Psychoeducation about Anxiety, IE, and Cognitive Restructuring
In session 2, we emphasized the benign nature of anxiety/stress in regard to its immediate effects on the body by describing (1) the nature of anxiety/stress, (2) effects of stress on the body, and (3) the relation between stress and physiological arousal. Participants were taught that they may have developed, or be at risk for developing, a conditioned fear to certain internal cues. Interoceptive conditioning processes were explained along with a re-description (relative to Session 1) of behavioral exercises that are designed to recondition and “unlearn” interoceptive cues. IE exercises (e.g., straw-breathing) were then demonstrated and practiced in session. Participants rated their levels of fear/anxiety and level of sensations experienced during each exercise using a 0–10 scale. Additionally, participants were taught to identify and change their cognitive reactions to such aversive sensations by encouraging them to reframe such experiences in more adaptive ways and accept them as “normal” rather than “dysfunctional” reactions. Participants were instructed to practice the IE exercises for homework with the rationale that such practice in symptom regulation before quitting should reduce distress that occurs upon cessation.
Session 3: Interoceptive Exposure Practice and Cognitive Restructuring
In session 3, we discussed each patient’s practice and reaction to the homework IE exercises and their ability to identify and alter catastrophic thinking about aversive internal states. IE exercises were again practiced in-session. Discussion about changes in their responses relative to Session 2 were highlighted. In line with components from SP, there was an additional focus on the upcoming quit day and the importance of continuing with selected activities during this difficult time. Participants were, again, asked to practice IE exercises and to monitor their performance using an exposure monitoring record card for homework.
Session 4 (Quit Week): Maintenance
Session 4 focused on the quit experience itself with reminders about the importance of utilizing anxiety-relevant therapeutic coping strategies in helping one deal effectively with cessation. In this session, we paid particular attention to drawing explicit connections between affective distress, withdrawal symptoms, and the urge to smoke. Such therapeutic activities were designed to encourage the participant to become more self-aware of the interactive role of affect-related experiences in their smoking behavior and urge to smoke. In addition, we emphasized the importance of integrating anxiety management skills with their non-smoking lifestyle. That is, we underscored the importance of integrating self-exposure, non-catastrophic thinking, and education regarding anxiety-related experiences as a way to maintain abstinence and build a healthier lifestyle more generally.
Data Analytic Procedure
Piecewise latent growth curve analysis was conducted to examine the effects of the intervention on growth of AS (i.e., ASI-3 scores), as well as panic symptoms (i.e., PDSS scores), from Baseline to Year 1 Follow-Up. This approach extends beyond traditional latent growth curve analysis by allowing for multiple slope parameters, reflecting different treatment stages (i.e., active treatment versus follow-up; Chou, Yang, Pentz, & Hser, 2004; Cudeck & Harring, 2010). The first slope (i.e., Intervention Slope) modeled the effects of the intervention on outcomes during the active treatment period (i.e., from Baseline to Quit Week). The second slope (i.e., Follow-up Slope) modeled post-treatment effects (i.e., from Week 1 to Year 1 Follow-Up) on outcomes during the follow-up period. For each model, the intercept was centered on Baseline scores and intercept and slope parameters were allowed to freely covary. Treatment condition (0 = Smoking Program [SP], 1 = Panic/Smoking Program [PSP]) was included as a predictor of the Intervention Slope and the Follow-up Slope. Models were fit in Mplus version 5.1 (Muthen & Muthen, 1998–2008) using Full Information Maximum Likelihood (FIML) and the Yuan-Bentler scaled chi-square index (Y-B χ2) to adjust the standard errors for nonnormality in the data. Overall model fit was determined using the Y-B χ2 and additional χ2-based fit indices, including the comparative fit index (CFI) and the root mean square error of approximation (RMSEA). A nonsignificant χ2 value indicates excellent model fit to the data. Additionally, CFI values from .90 to .95 indicate adequate fit and values greater than .95 indicate good fit. RMSEA values between .08 and .05 indicate adequate fit and values less than .05 indicate good fit. A 90% confidence interval is provided for the RMSEA, with .05 and below indicating that close fit cannot be dismissed and .10 and above indicating that poor fit cannot be ruled out (Hu & Bentler, 1999; Kline, 2011; MacCallum, Browne, & Sugawara, 1996). There was substantial missing data. However, all individuals who attended at least one treatment session were included in the data because FIML is robust to missing data, more so than other methods of handling missing data, including multiple imputation, pairwise deletion, and listwise deletion (Graham, 2009; Wothke, 2000).
A secondary aim of the current study was to examine whether the effects of the AS intervention on PDSS scores were mediated by the effects of the intervention on AS. Mediation analyses were conducted in Mplus to examine the effects of treatment on PDSS scores at two time points, immediately following the last treatment session (i.e., Quit Week), and at Year 1 Follow-Up. It was expected that the treatment would influence PDSS scores through a decrease in AS scores across treatment (i.e., Intervention Slope). PDSS scores at Baseline were included to control for initial PDSS levels. The mediation model was conducted using bias-corrected bootstrapped confidence intervals (CIs) with 1,000 bootstrap samples to provide consistent and replicable results (Preacher & Hayes, 2008). This method is preferred to other approaches using standard errors because asymmetric CIs can optimally balance power and Type I error (MacKinnon, Lockwood, & Williams, 2004).
Results
Sample and Preliminary Analysis
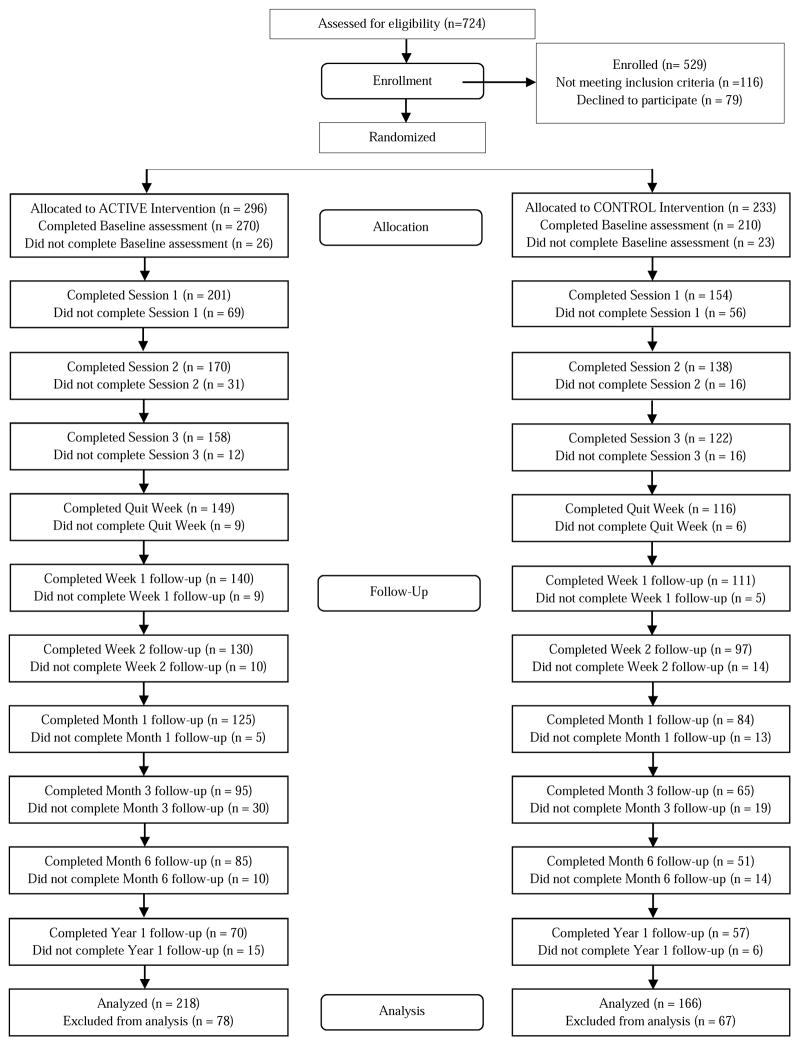
The final sample included 529 individuals randomized to treatment conditions, 296 (56%) assigned to the PSP condition, and 233 (44%) assigned to the SP condition. At baseline assessment, only 1 individual, from the PSP condition, was missing diagnostic information. Of the 529 individuals assigned to the intervention, 218 (74%) of the individuals in the PSP condition, and 166 (71%) of the individuals in the SP condition attended at least one treatment session, and were therefore included in the final sample to be analyzed. Comparisons across demographic and outcome variables between those who were assigned to participate but failed to complete a treatment session and those who completed at least a single treatment session indicated no significant differences across age, gender, drop-out across treatment condition, or across baseline levels of ASI-3, FTND (i.e., smoking severity). or PDSS scores.
Diagnostic data for individuals who participated in at least one treatment session are provided in Table 1. Of the 218 individuals in the PSP condition who attended at least one treatment session, 121 (55.5%) attended all four sessions, 37 (17.0%) attended at least three sessions, 23 (10.6%) attended at least two sessions, and 37 (17.0%) attended only a single session. Of the 166 individuals in the SP condition, 92 (55.4%) attended all sessions, 33 (19.9%) attended three sessions, 22 (13.3%) attended two sessions, and 19 (11.4%) attended only a single session. Means of demographics as well as baseline ASI-3 and PDSS scores were compared across treatment condition to examine the effectiveness of randomization. There were significant differences in ASI-3 scores, F (1, 382) = 3.89, p < .05, and PDSS scores, F (1, 382) = 6.61, such that individuals in the PSP condition had initially higher levels across these variables.
Table 1.
Descriptive Statistics for Pre-Intervention Measures by Treatment Condition
| Active Control | Treatment | ||
|---|---|---|---|
| Axis I Disorders | Percentage | Percentage | χ2 |
| Major Depressive Disorder | 7% | 7% | .01 |
| Dysthymia | 6% | 3% | 2.50 |
| Bipolar I | 1% | 0% | 1.31 |
| Bipolar II | 0% | 1% | .77 |
| Seasonal Depression | 1% | 0% | 1.31 |
| MDD NOS | 0% | 1% | 2.31 |
| Alcohol Use Disorders | 7% | 8% | .20 |
| Substance Use Disorders | 5% | 6% | .06 |
| Social Anxiety Disorder | 15% | 12% | .77 |
| Specific Phobia | 8% | 11% | .51 |
| Obsessive Compulsive | 2% | 3% | .73 |
| Post-Traumatic Stress Disorder | 4% | 5% | .03 |
| Generalized Anxiety Disorder | 8% | 10% | .60 |
| Anxiety NOS | 2% | 1% | 2.77 |
| Body Dysmorphic Disorder | 0% | 1% | .77 |
| Anorexia Nervosa | 1% | 0% | 1.31 |
| Bulimia | 0% | 1% | .77 |
N = 384. MDD = Major Depressive Disorder. NOS = Not Otherwise Specified.
At Year 1 follow-up, 70 individuals from the PSP condition and 57 individuals from the SP condition remained. Although the estimation methods used are robust to attrition, differential attrition between treatment and control condition could compromise the Year 1 findings. As a proxy test of differential attrition, comparisons were made, on demographic and baseline variables, between individuals in the PSP condition who attrited (N = 148) and individuals in the SP condition who attrited (N = 109). For these analyses, there was only one significant difference and that was for PDSS scores, F (1, 256) = 6.06, p < .05, indicating that individuals who dropped out from the SP condition had higher mean levels of PDSS scores (M = 4.72, SD = 4.30) than those from the PSP condition (M = 3.38, SD = 4.33).
Piecewise Latent Growth Curve Analysis of the Effects of Intervention on ASI-3 and PDSS Scores
A piecewise latent growth curve analysis was fit for the ASI-3. Treatment condition was included as a covariate. This model demonstrated adequate fit to the data (Y-B χ2 = 127.44, p < .05, CFI = .97, RMSEA = .05, 90% CI [.04, .06]). Unstandardized model parameters as well as the effect of treatment status on the intervention and follow-up slopes are provided in Table 3. There was a significant negative Intervention Slope (B = −.76, p < .001) indicating that ASI-3 scores decreased across treatment sessions. Further, treatment condition significantly predicted this slope (B = −.52, p < .05), such that individuals in the PSP condition demonstrated greater decreases in ASI-3 scores than did individuals in the SP condition. The effect size, d, calculated according to Feingold’s (2009) formula for calculating effect sizes using the baseline standard deviation, was in the small range (d = .18). The Follow-Up Slope was non-significant (B = −.02, p > .05), indicating that any gains made during treatment were maintained over the follow-up sessions. There was no effect of condition on the Follow-Up Slope.1
Table 3.
Parameters for Piecewise Latent Growth Curve Analysis of ASI-3 and PDSS Scores Including Treatment Condition Predicting Growth
| ASI-3 | PDSS | |||
|---|---|---|---|---|
|
| ||||
| Parameters | Estimate | SE | Estimate | SE |
| Intercept | 14.91*** | .61 | 4.08*** | .22 |
| Variance | 130.17*** | 12.54 | 16.89*** | 1.75 |
| Intervention Slope | −.76*** | .12 | −.26*** | .05 |
| Variance | 2.83*** | .50 | .24*** | .07 |
| Follow-up Slope | −.02 | .02 | −.01 | .01 |
| Variance | .02*** | .01 | .001 | .001 |
| Intercept/Intervention Slope Covariance | −9.69*** | 1.96 | −1.02*** | .31 |
| Intercept/Follow-Up Slope Covariance | −.47* | .19 | −.07** | .19 |
| Intervention/Follow-Up Slopes Covariance | −.01 | .03 | .01 | .004 |
|
| ||||
| Treatment Condition Effects (SP = 0, PSP = 1) | B | SE | B | SE |
|
| ||||
| Int Slope | −.52* | .21 | −.16* | .08 |
| FU Slope | .01 | .02 | .00 | .01 |
Note. ASI-3 = Anxiety Sensitivity Index-3. PDSS = Panic Disorder Severity Scale. SE = Standard Error.
p < .001,
p < .01,
p < .05.
A piecewise latent growth curve model for the PDSS demonstrated adequate fit to the data (Y-B χ2 = 134.81, p < .05, CFI = .93, RMSEA = .05, 90% CI [.04, .07]). Unstandardized model parameters as well as the effect of treatment status on the Intervention Slope and Follow-Up Slope are provided in Table 4. For PDSS, there was a significant negative Intervention Slope (B = −.26, p < .001) indicating that PDSS scores decreased across treatment sessions. Further, treatment condition significantly predicted this slope (B = −.16, p < .05), such that individuals in the PSP condition demonstrated greater decreases in PDSS scores than did individuals in the SP condition (d = .16).
Table 4.
Treatment Effects on PDSS Scores Mediated by ASI-3 Intervention Slopes
| Quit Week | Year 1 | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| B | 95% CI | B | 95% CI | |||
| LL | UL | LL | UL | |||
| PDSS | ||||||
| Baseline | .67 | .56 | .76 | .52 | .37 | .67 |
| Treatment Condition | .46 | −.18 | 1.11 | 1.08 | .23 | 1.90 |
| ASI-3 Slope | .50 | .19 | .83 | .46 | .05 | .87 |
| Indirect Effect | −.24 | −.56 | −.05 | −.22 | −.62 | −.02 |
Note. LL = Lower Limit. UL = Upper Limit. PDSS = Panic Disorder Severity Scale. ASI-3 Slope = ASI-3 Intervention Slope. Significant confidence intervals (i.e., those not including zero) are in bold.
Mediation Analyses Examining Effects of Treatment on PDSS Scores through ASI-3 Slope
Mediation analyses were conducted to examine the effects of treatment condition, through ASI-3 Slope (i.e., Intervention Slope), on PDSS scores at Quit Week and at Year 1. These analyses were conducted controlling for Baseline PDSS scores. Because bias-corrected bootstrapped CIs are not provided when the Y-B χ2 correction is used in Mplus, analyses were conducted without this correction. In order to limit the effect of skew on the analyses, outliers for the PDSS scale were corrected to within +/− 3 standard deviations of the mean. Model fit statistics indicated that the Quit Week mediation model fit the data adequately (Y-B χ2 = 317.41, p < .05, CFI = .93, RMSEA = .09, 90% CI [.08, .11]) as did the Year 1 mediation model (Y-B χ2 = 299.51, p < .05, CFI = .94, RMSEA = .08, 90% CI [.07, .09]).
Unstandardized parameters with bias corrected CIs for mediation effects at Quit Week and at Year 1 are provided in Table 4. For the Quit Week model, the ASI-3 slope significantly predicted PDSS scores (B = .50, 95% CI [.19, .83]). The effect of treatment condition was mediated by ASI-3 Slope (B = −.24, 95% CI [−.56, −.05]). For the Year 1 model, treatment condition significantly predicted PDSS scores (B = 1.08, 95% CI [.23, 1.90]) as did the ASI-3 Slope (B = .46, 95% CI [.05, .87]). The effect of treatment condition was also mediated by the ASI-3 Slope (B = −.22, 95% CI [−.62, −.02]).
Discussion
The current study was designed to develop knowledge about reducing risk for panic among an at risk sample of high AS smokers. Consistent with initial prediction there was a significant effect of treatment condition on AS, such that individuals in the PSP condition, compared to those in the SP condition, demonstrated greater decreases in AS throughout treatment which persisted throughout the follow-up period. Expanding upon prior AS intervention research (Barlow et al., 1989; Feldner et al., 2008; Keough & Schmidt, 2012; Schmidt et al., 2007), we now have evidence that an integrated smoking/AS reduction treatment is effective at decreasing risk, even among an at risk sample.
Also consistent with initial prediction, results revealed a significant effect of treatment condition on reductions in panic-related symptomatology. Despite the plethora of literature attesting to the associations between AS and panic (Ehlers, 1995; Schmidt et al., 1997; Taylor, 2014), we are aware of only two studies that have evaluated whether an AS intervention reduced later diagnoses. (Schmidt et al., 2007) as well as (Gardenswartz & Craske, 2001) found that intervening on AS reduced the risk for all Axis I diagnoses (Schmidt et al., 2007) or panic disorder (Gardenswartz & Craske, 2001). The current report adds to this limited literature in showing that relatively brief, psychoeducational interventions can significantly impact the incidence of later psychopathology.
Further, based on the mediation analyses conducted in the current study, panic symptoms were largely reduced through reductions in AS, occurring throughout the intervention. These findings are consistent with several recent studies demonstrating that AS interventions reduce anxiety symptoms via reductions in AS (Allan, Short, Albanese, Keough, & Schmidt, in press; Norr, Allan, Macatee, Keough, & Schmidt, 2014). Norr and colleagues further demonstrated that reductions in AS and not an associated risk factor (distress tolerance) uniquely mediated intervention effects on anxiety symptoms. Consistent with work from intervention studies on panic disorder (Smits, Powers, Cho, & Telch, 2004), these findings highlight the role of AS in panic-relevant outcomes.
Unlike prior AS intervention research utilizing at risk treatment-seeking samples in which effect sizes were found to be medium to large (Broman-Fulks & Storey, 2008; Feldner et al., 2008; Keough & Schmidt, 2012; Schmidt et al., 2007), effect sizes for AS reduction within the current investigation were small. These differences could be explained by a host of study specific factors, including differing baseline levels of AS, follow-up periods, measures of AS, and intensity of treatment. It is also possible that differences in the nature of the population across the various AS trials contributed to these disparate findings. The majority of AS reduction studies to date have utilized anxiety patient samples or highly anxious undergraduates (Gardenswartz & Craske, 2001; Keough & Schmidt, 2012; Schmidt et al., 2014). Given the complex nature of the relations between AS, smoking, and panic pathology (Zvolensky & Bernstein, 2005) targeting this cognitive risk factor within the context of smoking populations may require more intensive AS interventions than would typically be delivered to an anxiety-based population. Alternatively, it is also possible that the control condition used in the present investigation acted somewhat as an active control. In particular, individuals in the SP were taught to monitor and fade their cigarette consumption prior to quit day. This continual exposure to withdrawal symptoms that typically occur during smoking discontinuation could have subsequently lowered ones sensitivity to such sensations (AS) thereby attenuating overall effect sizes between conditions.
Findings from the current study should be considered in light of its limitations and opportunities for future research. Although the sample size was quite large at the start of the study, there were high levels of attrition throughout. In particular, only a little over 50% of the sample received the full intervention. While this rate of attrition is not uncommon within the smoking cessation literature (see Prochaska, Delucchi, & Hall, 2004 for a review), it could have obviously diminished the effects of this brief intervention. Future studies should seek to replicate these findings in larger samples while also examining variables that could influence treatment outcomes including co-morbid psychiatric diagnoses. Finally, although valid and reliable measures were used, all were assessed using self-report methods. Future investigations could benefit from multi-modal assessments including biological challenge paradigms to assess for fearful responding to panic-related symptomotology (Schmidt et al., 2007).
Despite these limitations, the investigation provides important information regarding the amelioration of a well-established individual difference variable within the context of an at risk sample of smokers. Consistent with initial prediction, individuals in the PSP compared to those in the SP evidenced significantly lower AS scores post-intervention. These effects were maintained through follow-up, one year later, for those who continued to participate in the study. The current study also demonstrated reductions in panic symptoms, through AS reductions, providing support for the effectiveness of this and similar interventions in reducing panic symptoms.
Figure 1.
CONSORT chart of participants detailing patient flow, assignment, and dropout. CONSORT = consolidated standards of reporting trials.
Table 2.
Descriptive Statistics for Baseline Measures by Treatment Condition
| SP Condition | PSP Condition | ||||
|---|---|---|---|---|---|
|
| |||||
| Mean | SD | Mean | SD | F | |
| ASI-3 Total | 12.91 | 11.46 | 15.31 | 12.04 | 3.89* |
| PDSS | 3.41 | 4.04 | 4.57 | 4.60 | 6.61* |
| Age | 39.65 | 12.98 | 37.89 | 14.16 | 1.55 |
|
| |||||
| Percentage | Percentage | χ2 | |||
| Sex | .84 | ||||
| Male | 52% | 48% | |||
| Female | 48% | 52% | |||
| Race | 8.40 | ||||
| Caucasian | 79% | 87% | |||
| African American | 13% | 9% | |||
| Hispanic | 4% | 2% | |||
| Asian | 2% | 0% | |||
| Other | 2% | 2% | |||
Note. SP Condition = Smoking Program Condition. PSP Condition = Panic/Smoking Program Condition. ASI-3 = Anxiety Sensitivity Index-3. PDSS = Panic Disorder Severity Scale.
p < .01,
p < .05.
Highlights.
Risk factors for panic include smoking and anxiety sensitivity (AS).
Yet, little is known about how to reduce risk of panic in high AS smokers.
Current study evaluated panic outcomes in among high AS smokers.
Significant main effect of treatment condition on AS and panic related symptoms.
Mediation analyses indicated that reductions in AS resulted in lower panic symptoms.
Acknowledgments
This research was funded by the National Institute of Mental Health (grant R01 MH076629-0). It should be noted that the funding agency had no role in the study design, collection of data, analysis or interpretation of data, in the writing of the report, or in the decision to submit the article for publication.
Footnotes
To determine whether there were site effects for the intervention, invariance testing was conducted across sites. There were no significant differences in slope values across sites or in the effect of treatment condition on slopes. The only significant difference was in intercept values across sites (χ2 = 12.12, p < .001), indicating that initial ASI-3 scores were higher in individuals seeking treatment at UVM as compared to initial ASI-3 levels at FSU.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abrams DB, Niaura R. The tobacco dependence treatment handbook: A guide to best practices. Guilford Press; 2003. [Google Scholar]
- Allan NP, Short NA, Albanese BJ, Keough ME, Schmidt NB. Direct and mediating effects of an anxiety sensitivity intervention on post-traumatic stress disorder symptoms in trauma exposed individuals. Cognitive Behavior Therapy. doi: 10.1080/16506073.2015.1075227. in press. [DOI] [PubMed] [Google Scholar]
- Association, A. P. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®) American Psychiatric Pub; 2013. [Google Scholar]
- Barlow DH, Craske MG, Cerny JA, Klosko JS. Behavioral treatment of panic disorder. Behavior Therapy. 1989;20(2):261–282. [Google Scholar]
- Breslau N, Johnson EO, Hiripi E, Kessler R. Nicotine dependence in the United States: prevalence, trends, and smoking persistence. Archives of general psychiatry. 2001;58(9):810–816. doi: 10.1001/archpsyc.58.9.810. [DOI] [PubMed] [Google Scholar]
- Breslau N, Klein DF. Smoking and panic attacks: an epidemiologic investigation. Archives of general psychiatry. 1999;56(12):1141–1147. doi: 10.1001/archpsyc.56.12.1141. [DOI] [PubMed] [Google Scholar]
- Broman-Fulks JJ, Storey KM. Evaluation of a brief aerobic exercise intervention for high anxiety sensitivity. Anxiety, Stress, & Coping. 2008;21(2):117–128. doi: 10.1080/10615800701762675. [DOI] [PubMed] [Google Scholar]
- Brown RA, Kahler CW, Niaura R, Abrams DB, Sales SD, Ramsey SE, Miller IW. Cognitive–behavioral treatment for depression in smoking cessation. Journal of consulting and clinical psychology. 2001;69(3):471. doi: 10.1037//0022-006x.69.3.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Kahler CW, Zvolensky MJ, Lejuez CW, Ramsey SE. Anxiety sensitivity: Relationship to negative affect smoking and smoking cessation in smokers with past major depressive disorder. Addictive behaviors. 2001;26(6):887–899. doi: 10.1016/s0306-4603(01)00241-6. [DOI] [PubMed] [Google Scholar]
- Chou C, Yang D, Pentz MA, Hser Y. Piecewise growth curve modeling approach for longitudinal prevention study. Computational Statistics & Data Analysis. 2004;46(2):213–225. [Google Scholar]
- Cinciripini PM, Lapitsky L, Seay S, Wallfisch A, Meyer WJ, Van Vunakis H. A placebo-controlled evaluation of the effects of buspirone on smoking cessation: differences between high-and low-anxiety smokers. Journal of clinical psychopharmacology. 1995;15(3):182–191. doi: 10.1097/00004714-199506000-00006. [DOI] [PubMed] [Google Scholar]
- Cudeck R, Harring JR. Developing a random coefficient model for nonlinear repeated measures data. Statistical methods for modeling human dynamics: An interdisciplinary dialogue. 2010:289–318. [Google Scholar]
- Ehlers A. A 1-year prospective study of panic attacks: clinical course and factors associated with maintenance. Journal of abnormal psychology. 1995;104(1):164. doi: 10.1037//0021-843x.104.1.164. [DOI] [PubMed] [Google Scholar]
- Farris SG, DiBello AM, Allan NP, Hogan J, Schmidt NB, Zvolensky MJ. Evaluation of the Anxiety Sensitivity Index-3 among treatment-seeking smokers. Psychological assessment. doi: 10.1037/pas0000112. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farris SG, Langdon KJ, DiBello AM, Zvolensky MJ. Why Do Anxiety Sensitive Smokers Perceive Quitting as Difficult? The Role of Expecting “Interoceptive Threat” During Acute Abstinence. Cognitive Therapy and Research. 2015;39(2):236–244. [Google Scholar]
- Feingold A. Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychological methods. 2009;14(1):43. doi: 10.1037/a0014699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldner MT, Zvolensky MJ, Babson K, Leen-Feldner EW, Schmidt NB. An integrated approach to panic prevention targeting the empirically supported risk factors of smoking and anxiety sensitivity: Theoretical basis and evidence from a pilot project evaluating feasibility and short-term efficacy. Journal of anxiety disorders. 2008;22(7):1227–1243. doi: 10.1016/j.janxdis.2008.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiore MC, Bailey WC, Cohen SJ, Dorfman SF, Goldstein MG, Gritz ER, Lando HA. Treating tobacco use and dependence: a clinical practice guideline. Publications Clearinghouse; 2000. [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J. User’s guide for the Structured clinical interview for DSM-IV axis I disorders SCID-I: clinician version. American Psychiatric Pub; 1997. [Google Scholar]
- Gardenswartz CA, Craske MG. Prevention of panic disorder. Behavior Therapy. 2001;32(4):725–737. [Google Scholar]
- Graham JW. Missing data analysis: Making it work in the real world. Annual review of psychology. 2009;60:549–576. doi: 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- Hall SM, Muñoz RF, Reus VI. Cognitive-behavioral intervention increases abstinence rates for depressive-history smokers. Journal of consulting and clinical psychology. 1994;62(1):141. doi: 10.1037//0022-006x.62.1.141. [DOI] [PubMed] [Google Scholar]
- Hayward C, Killen JD, Kraemer HC, Taylor CB. Predictors of panic attacks in adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39(2):207–214. doi: 10.1097/00004583-200002000-00021. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström K. The Fagerström test for nicotine dependence: a revision of the Fagerstrom Tolerance Questionnaire. British journal of addiction. 1991;86(9):1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Houck PR, Spiegel DA, Shear MK, Rucci P. Reliability of the self-report version of the panic disorder severity scale. Depression and anxiety. 2002;15(4):183–185. doi: 10.1002/da.10049. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural equation modeling: a multidisciplinary journal. 1999;6(1):1–55. [Google Scholar]
- Keough ME, Schmidt NB. Refinement of a brief anxiety sensitivity reduction intervention. Journal of consulting and clinical psychology. 2012;80(5):766. doi: 10.1037/a0027961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. Guilford press; 2011. [Google Scholar]
- Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: a population-based prevalence study. Jama. 2000;284(20):2606–2610. doi: 10.1001/jama.284.20.2606. [DOI] [PubMed] [Google Scholar]
- Leen-Feldner EW, Feldner MT, Bernstein A, McCormick JT, Zvolensky MJ. Anxiety sensitivity and anxious responding to bodily sensations: A test among adolescents using a voluntary hyperventilation challenge. Cognitive Therapy and Research. 2005;29(5):593–609. [Google Scholar]
- MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychological methods. 1996;1(2):130. [Google Scholar]
- MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate behavioral research. 2004;39(1):99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maller RG, Reiss S. Anxiety sensitivity in 1984 and panic attacks in 1987. Journal of anxiety disorders. 1992;6(3):241–247. [Google Scholar]
- McNally RJ. Anxiety sensitivity and panic disorder. Biological psychiatry. 2002;52(10):938–946. doi: 10.1016/s0006-3223(02)01475-0. [DOI] [PubMed] [Google Scholar]
- McNally RJ, Eke M. Anxiety sensitivity, suffocation fear, and breath-holding duration as predictors of response to carbon dioxide challenge. Journal of abnormal psychology. 1996;105(1):146. doi: 10.1037//0021-843x.105.1.146. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Kavanagh D. Treating comorbidity of alcohol problems and psychiatric disorder. The essential handbook of treatment and prevention of alcohol problems. 2004:139. [Google Scholar]
- Muthen LK, Muthen BO. Mplus User’s Guide. 5. Los Angeles, CA: 1998–2008. [Google Scholar]
- Norr AM, Allan NP, Macatee RJ, Keough ME, Schmidt NB. Effect of a computerized anxiety sensitivity intervention on anxiety, depression, and worry: Mediation through affect tolerances. Behaviour research and therapy. 2014;59:12–19. doi: 10.1016/j.brat.2014.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osher FC. A vision for the future: Toward a service system responsive to those with co-occurring addictive and mental disorders. American Journal of Orthopsychiatry. 1996;66(1):71. doi: 10.1037/h0080156. [DOI] [PubMed] [Google Scholar]
- Otto M, Pollack M, Sachs G, Reiter S, Meltzer-Brody S, Rosenbaum J. Discontinuation of benzodiazepine treatment: efficacy of cognitive-behavioral therapy for patients with panic disorder. Am J Psychiatry. 1993;150(10):1485–1490. doi: 10.1176/ajp.150.10.1485. [DOI] [PubMed] [Google Scholar]
- Parrott AC. Does cigarette smoking cause stress? American Psychologist. 1999;54(10):817. doi: 10.1037//0003-066x.54.10.817. [DOI] [PubMed] [Google Scholar]
- Pechter BM, Miller NS. Psychopharmacotherapy for addictive and comorbid disorders: Current studies. Journal of addictive diseases. 1997;16(4):23–40. doi: 10.1080/10550889709511141. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior research methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Prochaska JJ, Delucchi K, Hall SM. A meta-analysis of smoking cessation interventions with individuals in substance abuse treatment or recovery. Journal of consulting and clinical psychology. 2004;72(6):1144. doi: 10.1037/0022-006X.72.6.1144. [DOI] [PubMed] [Google Scholar]
- Rabian B, Embry L, MacIntyre D. Behavioral validation of the Childhood Anxiety Sensitivity Index in children. Journal of Clinical Child Psychology. 1999;28(1):105–112. doi: 10.1207/s15374424jccp2801_9. [DOI] [PubMed] [Google Scholar]
- Reiss S, McNally RJ. Expectancy model of fear. In: Reiss S, Bootzin RR, editors. Theoretical issues in behavior therapy inside. San Diego, CA: Academic Press; 1985. [Google Scholar]
- Schmidt NB, Capron DW, Raines AM, Allan NP. Randomized clinical trial evaluating the efficacy of a brief intervention targeting anxiety sensitivity cognitive concerns. Journal of consulting and clinical psychology. 2014;82(6):1023. doi: 10.1037/a0036651. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Eggleston AM, Woolaway-Bickel K, Fitzpatrick KK, Vasey MW, Richey A. Anxiety Sensitivity Amelioration Training (ASAT): a longitudinal primary prevention program targeting cognitive vulnerability. Journal of anxiety disorders. 2007;21(3):302–319. doi: 10.1016/j.janxdis.2006.06.002. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Joiner TE. Structure of the Anxiety Sensitivity Index psychometrics and factor structure in a community sample. Journal of anxiety disorders. 2002;16(1):33–49. doi: 10.1016/s0887-6185(01)00087-1. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Lerew DR, Jackson RJ. The role of anxiety sensitivity in the pathogenesis of panic: prospective evaluation of spontaneous panic attacks during acute stress. Journal of abnormal psychology. 1997;106(3):355. doi: 10.1037//0021-843x.106.3.355. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Lerew DR, Jackson RJ. Prospective evaluation of anxiety sensitivity in the pathogenesis of panic: replication and extension. Journal of abnormal psychology. 1999;108(3):532. doi: 10.1037//0021-843x.108.3.532. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Woolaway-Bickel K, Trakowski J, Santiago H, Storey J, Koselka M, Cook J. Dismantling cognitive–behavioral treatment for panic disorder: Questioning the utility of breathing retraining. Journal of consulting and clinical psychology. 2000;68(3):417. doi: 10.1037//0022-006x.68.3.417. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Zvolensky MJ, Maner JK. Anxiety sensitivity: Prospective prediction of panic attacks and Axis I pathology. Journal of psychiatric research. 2006;40(8):691–699. doi: 10.1016/j.jpsychires.2006.07.009. [DOI] [PubMed] [Google Scholar]
- Shear MK, Brown TA, Barlow DH, Money R, Sholomskas DE, Woods SW, Papp LA. Multicenter collaborative panic disorder severity scale. American Journal of Psychiatry. 1997 doi: 10.1176/ajp.154.11.1571. [DOI] [PubMed] [Google Scholar]
- Smits J, Powers MB, Cho Y, Telch MJ. Mechanism of change in cognitive-behavioral treatment of panic disorder: evidence for the fear of fear mediational hypothesis. Journal of consulting and clinical psychology. 2004;72(4):646. doi: 10.1037/0022-006X.72.4.646. [DOI] [PubMed] [Google Scholar]
- Taylor S. Anxiety sensitivity: Theory, research, and treatment of the fear of anxiety. Routledge; 2014. [Google Scholar]
- Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR, Stewart SH. Robust dimensions of anxiety sensitivity: development and initial validation of the Anxiety Sensitivity Index-3. Psychological assessment. 2007;19(2):176. doi: 10.1037/1040-3590.19.2.176. [DOI] [PubMed] [Google Scholar]
- Telch MJ, Lucas JA, Schmidt NB, Hanna HH, Jaimez TL, Lucas RA. Group cognitive-behavioral treatment of panic disorder. Behaviour research and therapy. 1993;31(3):279–287. doi: 10.1016/0005-7967(93)90026-q. [DOI] [PubMed] [Google Scholar]
- Weems CF, Hayward C, Killen JD, Taylor CB. A longitudinal investigation of anxiety sensitivity in adolescence. Journal of abnormal psychology. 2002;111(3):471. [PubMed] [Google Scholar]
- Westling BE, Öst L. Brief cognitive behaviour therapy of panic disorder. Scandinavian Journal of Behaviour Therapy. 1999;28(2):49–57. [Google Scholar]
- Wothke W. Longitudinal and multigroup modeling with missing data. 2000:219–281. [Google Scholar]
- Zvolensky MJ, Bernstein A. Cigarette smoking and panic psychopathology. Current Directions in Psychological Science. 2005;14(6):301–305. doi: 10.1177/0963721410388642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zvolensky MJ, Feldner MT, Eifert GH, Stewart SH. Evaluating differential predictions of emotional reactivity during repeated 20% carbon dioxide-enriched air challenge. Cognition & Emotion. 2001;15(6):767–786. [Google Scholar]
- Zvolensky MJ, Schmidt NB. Panic disorder and smoking. Clinical Psychology: Science and Practice. 2003;10(1):29–51. [Google Scholar]
- Zvolensky MJ, Schmidt NB, Antony MM, McCabe RE, Forsyth JP, Feldner MT, Kahler CW. Evaluating the role of panic disorder in emotional sensitivity processes involved with smoking. Journal of anxiety disorders. 2005;19(6):673–686. doi: 10.1016/j.janxdis.2004.07.001. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Stewart SH, Vujanovic AA, Gavric D, Steeves D. Anxiety sensitivity and anxiety and depressive symptoms in the prediction of early smoking lapse and relapse during smoking cessation treatment. Nicotine & Tobacco Research. 2009;11(3):323–331. doi: 10.1093/ntr/ntn037. [DOI] [PMC free article] [PubMed] [Google Scholar]