Abstract
In clinical settings, there is a high comorbidity between substance use disorders, psychiatric disorders, and traumatic stress. As such, transdiagnostic therapies are needed to address these co-occurring issues efficiently. The aim of the present study was to conduct a pragmatic randomized controlled trial comparing Mindfulness-Oriented Recovery Enhancement (MORE) to group Cognitive-Behavioral Therapy (CBT) and treatment-as-usual (TAU) for previously homeless men residing in a therapeutic community. Men with co-occurring substance use and psychiatric disorders, as well as extensive trauma histories, were randomly assigned to 10 weeks of group treatment with MORE (n=64), CBT (n=64), or TAU (n=52). Study findings indicated that from pre- to post-treatment MORE was associated with modest yet significantly greater improvements in substance craving, post-traumatic stress, and negative affect than CBT, and significantly greater improvements in post-traumatic stress and positive affect than TAU. A significant indirect effect of MORE on decreasing craving and post-traumatic stress by increasing dispositional mindfulness was observed, suggesting that MORE may target these issues via enhancing mindful awareness in everyday life. This pragmatic trial represents the first head-to-head comparison of MORE against an empirically-supported treatment for co-occurring disorders. Results suggest that MORE, as an integrative therapy designed to bolster self-regulatory capacity, may hold promise as a treatment for intersecting clinical conditions.
Keywords: mindfulness, transdiagnostic, addiction, PTSD, emotion regulation, reappraisal, savoring
Of the estimated 2.5 – 3.5 million homeless individuals in the United States annually (Kilgore, 2013), pooled prevalence estimates suggest that 24% to 38% have substance use disorders (Fazel, Khosla, Doll, & Geddes, 2008), and one study identified a lifetime prevalence rate of 23% for co-occurring substance use and psychiatric disorders (SAMHSA, 2015). Moreover, there is substantial comorbidity of post-traumatic stress disorder (PTSD) and substance use disorders among the homeless, with estimates ranging from 16 to 19% (Torchalla et al., 2014). The co-occurrence of psychiatric and substance use disorders is associated with increased risk of relapse, recurrent psychological symptoms, and poor prognosis (Flynn & Brown, 2008). Despite having significant psychiatric needs, less than half of individuals with co-occurring disorders (COD) in need of treatment receive it (SAMHSA, 2015).
Individuals with COD tend to have high rates of exposure to stressful and traumatic life events with which they often cope through alcohol and drug use as a form of self-medication (Khantzian, 1997; Leeies, Pagura, Sareen, & Bolton, 2010). To the extent that psychoactive agents may temporarily relieve distress, self-medication can become negatively reinforcing (Baker, Piper, McCarthy, Majeskie, & Fiore, 2004), resulting in entrenchment of this coping pattern as an addictive response subject to reactivation by future stressors (Garland, Boettiger, & Howard, 2011). Consequently, substance use becomes compulsive, resulting in a powerful conditioned response mediated by the mesocorticolimbic dopamine system that is subjectively experienced as craving (Skinner & Aubin, 2010). In turn, craving coupled with negative affect may promote chronic substance use, which in turn renders the individual increasingly sensitized to stress and desensitized to pleasure from naturally-rewarding objects and events (Koob, 2008; Koob & Le Moal, 2001). This process, known as allostasis, results in an overall hedonic deficit, manifested in negative affective states which impel the individual to imbibe increasingly higher doses of the substance to achieve a dwindling sense of well-being.
These reciprocally-energizing linkages between psychiatric distress, substance use, and trauma symptoms make COD especially difficult to treat (Najavits, 2002). Though community-based treatment agencies typically adopt a sequential approach to treating these interlocking issues, integrated treatment approaches are heralded as best practices. Despite the prevalence and consequences of COD, few integrated, empirically-supported treatment options are available, and even fewer have been tested as interventions for homeless individuals in randomized controlled trials (RCTs). Among interventions for COD currently employed in the U.S., Seeking Safety (Najavits, 2002; Najavits, Weiss, Shaw, & Muenz, 1998) has perhaps the strongest evidence base. This cognitive-behavioral therapy (CBT), which was specifically designed to target the co-occurrence of PTSD and substance use disorders, has been shown in RCTs to significantly improve PTSD and substance use disorder symptoms (Najavits & Hien, 2013).
Despite the considerable success of Seeking Safety, CBT interventions may not be effective for all homeless individuals with COD and histories of trauma. Indeed, clients who suffer from mood and anxiety disorders (in addition to PTSD symptoms) might benefit from other therapies which target a broad spectrum of cognitive, affective, behavioral, and physiological processes underpinning psychopathology (Garland & Howard, 2013a). In that regard, mindfulness-based interventions (MBIs) may be especially efficacious. Meta-analyses have found MBIs to outperform non-specific active control conditions and produce significant effects on depressive and anxious symptomatology (Goyal et al., 2014). RCTs have revealed significant effects of MBIs on substance use disorders (Bowen et al., 2014; Chiesa & Serretti, 2014). Although less evidence is available with regard to the effects of MBIs on post-traumatic stress symptoms, quasi-experimental (Kearney, McDermott, Malte, Martinez, & Simpson, 2013; King et al., 2013) studies have found significant improvements in post-traumatic stress associated with participation in MBIs, and a recent wait-list RCT found large-effect size reductions in post-traumatic stress and depressive symptoms among female survivors of interpersonal violence following treatment with a trauma-informed MBI (Kelly & Garland, in press). Taken together, these studies suggest that MBIs might be useful for ameloriating COD.
As an exemplar MBI, Mindfulness-Oriented Recovery Enhancement (MORE) was designed to target mechanisms linking stress-related conditions and addiction (Garland, 2013). MORE unites complementary aspects of mindfulness training, CBT, and principles from positive psychology into an integrative treatment approach. MORE differs from other MBIs in that it integrates formal mindfulness meditation practice with cognitive reappraisal and savoring techniques. At present, MORE has been tested in two early-stage RCTs. In the first trial, MORE was tested as a treatment for alcohol dependent adults (N=53) in long-term residential treatment (Garland, Gaylord, Boettiger, & Howard, 2010). Results indicated that compared to a support group control condition, MORE was associated with significantly greater reductions in perceived stress and thought suppression, as well as significantly greater autonomic nervous system recovery from stress and alcohol cue-exposure at post-treatment. In a second trial, a modified version of MORE was tested as a treatment for prescription opioid misuse among chronic pain patients prescribed long-term opioid analgesics (N=115) (Garland, Manusov, et al., 2014). Compared with a support group control condition, participants in MORE evidenced significantly greater reductions in stress arousal and opioid craving, and were significantly more likely to no longer meet criteria for opioid use disorder at post-treatment.
Subsequent mechanistic studies indicated that participation in MORE was associated with significant reductions in attentional bias for emotionally-threatening cues (Garland & Howard, 2013b), significant improvements in autonomic regulation during attention to emotional information (Garland, Froeliger, & Howard, 2014a), and significant increases in cardiac (Garland, Froeliger, et al., 2014a), and electrocortical indices of natural reward processing (Garland, Froeliger, & Howard, 2014b). Further, MORE appears to exert addiction-specific effects, including decreasing the correlation strength between drug craving and addictive behavior (Garland, Manusov, et al., 2014), and reducing drug cue-reactivity (Garland, Froeliger, et al., 2014a). The effects of MORE on these mechanisms indicates its promise as an intervention for COD, yet MORE’s efficacy relative to other treatments for COD has not been established.
As such, we conducted a pragmatic trial to compare MORE as a treatment for substance dependent individuals with trauma histories to a group cognitive-behavioral therapy (CBT) intervention, as well as treatment-as-usual (TAU) in a modified therapeutic community environment. In contrast to explanatory clinical trials which measure treatment efficacy under ideal conditions, pragmatic trials evaluate the benefit of treatments as delivered in routine clinical practice (Roland & Torgerson, 1998). Given its therapeutic mechanisms, we hypothesized that MORE would produce greater improvements in primary outcomes including craving, post-traumatic stress symptoms, and psychiatric distress than CBT or TAU. With regard to secondary outcomes, we hypothesized that MORE would produce greater improvements in dispositional mindfulness and positive and negative affect than CBT or TAU. Because participants varied with regard to their readiness to change, it was important to consider the effect of this factor on treatment outcomes. A meta-analysis including 8238 patients found a clinically significant effect size (d=.46) for the association between stage of change and psychotherapy outcomes, including outcomes directly relevant to PTSD and COD (Norcross, Krebs, & Prochaska, 2011). As such, we controlled for readiness to change in outcome analyses.
METHODS
Participants and procedure
Men with co-occurring substance use and psychiatric disorders were recruited for this study from a modified therapeutic community in an urban area in the Southeastern United States. This modified therapeutic community involved a two-year-long program, in which clients graduate through various phases of treatment and vocational training. Inclusion criteria were: 1) age ≥18 years; 2) current substance use disorder diagnosis and current psychiatric disorder diagnosis as defined by the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; and 3) homelessness prior to entering into the therapeutic community. Individuals were excluded with 1) active psychosis and 2) substance withdrawal during informed consent. Diagnostic criteria were assessed with a semi-structured psychiatric interview similar to the Mini-International Neuropsychiatric Interview (MINI) (Sheehan et al., 1998), which differed in that it included a broader array of DSM-IV TR categories not assessed by the MINI (e.g., dysthymia, specific phobia, etc.). Diagnostic interviews were conducted by a psychiatrist and/or clinical social worker with training in making addiction and psychiatric disorder diagnoses.
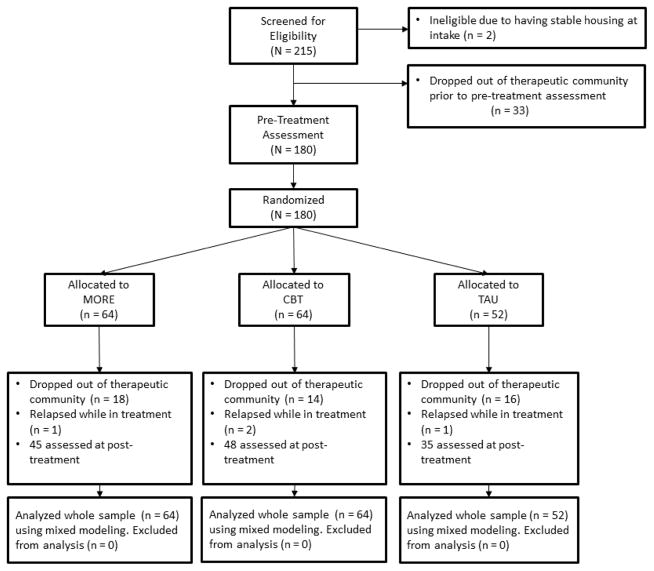
Following admission into the therapeutic community (which entailed an orientation to the program and the diagnostic assessment), potential participants were approached about the study and provided informed consent, after which they completed a series of validated questionnaires in a pre-treatment assessment session administered by a research assistant. Because MORE and CBT were delivered as group therapies in this study, it was necessary to accumulate a cohort of 6 to 12 individuals before the treatment groups could begin. Participants in group cohorts were randomized with simple random assignment to MORE (N=64), CBT (N=64), or TAU (N=52). Simple random assignment was conducted by the first author using Research Randomizer software (Urbaniak & Plous, 2011). The first author, who was blinded to subjects’ identities and uninvolved in research assessments, gave the random assignment table to the study coordinator, who then assigned participants to treatment groups. Over the course of 4 years, 27 cohorts (average N per cohort=7.0±1.3) completed one of the three, 10-week treatment conditions. Following the 10-week intervention conditions, participants completed the same set of questionnaires in a post-treatment assessment session administered by a research assistant who was blinded to treatment allocation, after which they all received TAU. All study procedures were approved by University of North Carolina-Chapel Hill IRB.
Treatment-as-usual
TAU in the modified therapeutic community primarily consisted of: participation in a therapeutic milieu; psychoeducation on topics related to addiction; client-centered, supportive-expressive group therapy; and coping skills groups (Monti & Rohsenow, 1999). TAU was provided for approximately 2 hours each day.
MORE
MORE unites complementary aspects of mindfulness training, third-wave cognitive-behavioral therapy, and principles from positive psychology into an integrative intervention strategy. Techniques drawn from these therapeutic approaches were integrated into a manualized 10-session group intervention designed to address the pathogenic factors implicated in addiction and psychological distress. MORE sessions involved mindfulness training to target automatic habit behavior and foster nonreactivity; positive reappraisal training to regulate negative emotions and foster a sense of meaningfulness in life; and training in savoring pleasant events and emotions to ameliorate deficits in natural reward processing and positive affectivity. Per the MORE treatment manual (Garland, 2013), sessions offered instruction in applying mindfulness and related skills to the following topics: awareness of automaticity in addiction; disrupting the link between negative emotions and addictive behavior through reappraisal; refocusing attention from stress and craving to savor pleasant experiences; regulating craving through mindful attention and awareness; decreasing craving through mindful stress reduction; promoting acceptance instead of suppression of experience; awareness of the impermanence of the body; mindful relationships; interdependence and meaning in life; and developing a mindful recovery plan. Mindfulness training involved mindful breathing and body scan techniques, with an emphasis on developing metacognitive awareness and attentional control. MORE participants were asked to engage in daily 15-minute mindfulness practice on their own. To conform with standard of care at the therapeutic community (i.e., TAU), group sessions were 2 hours in length and were administered by a Masters-level clinical social worker who had practiced mindfulness for >5 years and had clinical experience offering mindfulness training to persons with psychiatric disorders. This individual was supervised weekly by the first author (the developer of MORE).
Cognitive-Behavioral Therapy
We implemented a 10 session group CBT intervention to match the MORE intervention as much as possible in terms of time-in-treatment. This intervention provided training in cognitive, behavioral, and interpersonal coping skills delivered content from the Seeking Safety treatment manual on the following topics (Najavits, 2002): safety; PTSD: taking back your power; detaching from emotional pain; when substances control you; compassion; honesty; recovery thinking; setting boundaries in relationships; healing from anger; termination. To match MORE and TAU sessions in length, CBT group sessions were 2 hours long, and participants were asked to do daily homework to meet “commitments” which they set at the end of each session (Najavits, 2002). The amount of time spent per day on commitments varied considerably depending on the nature of the commitment. CBT was implemented by Master’s-level clinical personnel with experience in treating individuals with addiction, trauma, and psychiatric disorders. Clinical supervision was provided weekly by an experienced licensed psychotherapist with training in CBT.
Treatment fidelity
Treatment fidelity was monitored in a similar fashion among the MORE and CBT groups. Group facilitators used structured manuals with treatment implementation protocols, completed fidelity assessment checklists after each session, and met weekly with clinical supervisors. Fidelity assessment for the CBT group included an adapted version of the Seeking Safety Adherence Scale (Najavits & Liese, 2000) and fidelity for MORE was assessed with a comparable unpublished fidelity checklist, which tapped the extent to which facilitators: provided information about using mindfulness and reappraisal skills to cope with addiction and psychological distress; followed a common structure across sessions; practiced the application of mindfulness and other skills; displayed empathy; and created a safe and supportive atmosphere in the group. Items tapping intervention adherence and process variables on both fidelity assessment checklists were rated on a 0–3 scale, with higher scores indicating greater adherence. Clinical supervisors debriefed therapists and reviewed audio-recorded sessions to monitor therapist adherence to the MORE and Seeking Safety treatment manuals. Any deviations from the treatment manuals were communicated weekly prior to the next session during clinical supervision and corrected by the therapist in successive sessions. Minor deviations were observed infrequently, and adherence improved over time; no major deviations were noted.
Measures
Trauma history
Participants were asked whether or not they had ever experienced each of 9 traumatic events in their lifetime, including: “witnessed someone severely injured or killed in person”; “having been badly hurt or in danger of being badly hurt”; “had something very bad or terrifying happen to you”; “hit by someone who was trying to hurt you”; “been mugged by with a weapon or by force”; “attacked with a weapon or by someone trying to hurt or kill you”; “witnessed someone be severely beaten”; “been sexually touched against your will”; and “forced to do sex acts against your will.” These question items have been used to assess trauma history in individuals with substance use disorders in prior studies (Garland & Roberts-Lewis, 2013).
Craving
Substance craving was assessed with an adapted version of the Penn Alcohol Craving Scale (PACS) (Flannery, Volpicelli, & Pettinati, 1999), modified to assess craving for alcohol and other psychoactive substances. The original PACS includes five question items that assess the duration, frequency and intensity of craving for alcohol on a 7-point scale. In the version adapted for this study the item structure was maintained for the original five items but an additional five items were rephrased to inquire about craving for drugs other than alcohol. For Example item 1 of PACS “How often have you thought about drinking or how good a drink would make you feel?” was modified to “How often have you thought getting high, or about how good getting high would make you feel?” These adapted items were summed to create a total drug craving score. Then the adapted drug craving items were summed with the alcohol craving items to compute a total substance craving score across all 10 items (α = .93). This substance craving version of the PACS has been validated in several studies (Garland & Roberts-Lewis, 2013; Garland, Roberts-Lewis, Kelley, Tronnier, & Hanley, 2014; Witkiewitz & Bowen, 2011).
Post-traumatic stress symptoms
Post-traumatic stress symptoms were assessed with the 17-item PTSD Checklist-Civilian version (PCL-C) (Weathers et al., 1993). Participants rated how much they had been bothered by PTSD criterion symptoms as outlined by the DSM-IV over the past month. A total post-traumatic stress symptom score was calculated by summing responses to each item (3=.92). Responses on the PCL-C reflected post-traumatic stress symptoms resulting from the experience of traumatic events endorsed on the abovementioned measure of trauma history. The PCL was also used to determine partial PTSD diagnosis, as evidenced by meeting criteria for 2 out of 3 PTSD symptom clusters assessed on this scale.(Mylle & Maes, 2004) Lastly, the PCL was used to establish the presence of subthreshold PTSD symptoms, defined as the presence of some PTSD symptoms, but with too few to meet criteria for a full or partial PTSD diagnosis (Cukor, Wyka, Jayasinghe, & Difede, 2010).
Psychiatric distress
The depression (α = .87) and anxiety subscales (α = .88) of the Brief Symptom Inventory (BSI) (Derogatis & Melisaratos, 1983) were used to measure to what degree participants were currently distressed by symptoms like “Feeling fearful” and “Feelings of guilt.”
Dispositional mindfulness
The Five Facet Mindfulness Questionnaire was used to measure dispositional mindfulness (Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006). This scale is comprised of 39 items tapping to what extent participants endorse experiencing various facets of mindfulness: nonreactivity to inner experience (tapped by items such as “I watch my feelings without getting lost in them”), observing and attending to experience (“I pay attention to sensations, such as the wind in my hair or the sun on my face”), describing and discriminating emotional experiences (“I’m good at finding words to describe my feelings”), nonjudging of experience (“I tell myself I shouldn’t be feeling the way that I am feeling”), and acting with awareness (“I find myself doing things without paying attention”). Items are summed to produce a total dispositional mindfulness score (α = .92).
Positive and negative affect
The positive (α = .94) and negative affect subscales (α = .93) from the 20-item Positive and Negative Affect Schedule (PANAS) (Watson, Clark, & Tellegen, 1988) were used to assess the frequency of positive and negative affect “over the past week.” Responses on these items were summed to compute global positive and negative affect scores.
Readiness to change
Readiness to change was measured with the 32-item version of the University of Rhode Island Change Assessment (URICA; α = .72) (DiClemente, Schlundt, & Gemmell, 2004). Following DiClemente et al., the readiness score was computed by calculating means for the precontemplation, contemplation, action, and maintenance items, and then subtracting the precontemplation mean from the summation of other items. Readiness to change was assessed at the pre-treatment and used as a covariate in outcome analyses.
Statistical analysis
Intention-to-treat (ITT) analyses were conducted on the entire randomized sample (N=180). Outcome data were missing for 28.9% of participants due to study attrition (there were no significant between-groups differences in dropout rate). Non-significant t-tests and chi-square statistics indicated there were no significant differences between participants who dropped out vs. those who completed the study across demographic or clinical variables. To analyze patterns of missing data in study outcome variables, we performed Little’s MCAR test (Little, 1988). The non-significant chi-square value and the pattern of missing data were consistent with being missing completely at random (MCAR). To reduce potential bias resulting from listwise deletion or last-observation carried forward techniques, hypothesis testing was conducted using a repeated-measures linear mixed model approach, which is considered preferable to other methods of dealing with missing data (Singer & Willett, 2003). All models were estimated with maximum likelihood methods, which estimate the variance-covariance matrix for all available data, including data from cases assessed at only one time point.
Repeated-measures mixed models were computed to test our hypotheses that MORE would outperform Seeking Safety and TAU. These mixed models accounted for the variability associated with the nesting of multiple observations (i.e., pre- and post-intervention assessments; Level 1) within participants (Level 2) within group cohorts (Level 3). The random effects aspect of these models affords the structure necessary to account for clustering that may exist between individuals nested within each group cohort. In analysis models, we treated treatment condition (dummy coded into two planned contrasts of MORE vs. CBT and MORE vs. TAU), time, and cohort as fixed effects. Primary analyses modeled time as a repeated measure, treatment condition, and a treatment X time interaction term, with the interaction term being the main parameter of interest. We controlled for readiness to change because participants had a wide range of motivations for entering treatment. Some participants had been in prison following being homeless, and thus were adjudicated and sent to the therapeutic community on an involuntary basis (either compelled to enroll in treatment or face a longer prison sentence). Other participants entered into treatment because they had nowhere to seek long-term shelter other than the treatment facility. Others were compelled by their families to seek treatment. Still others entered treatment out of a desire to pursue recovery from addiction and mental health disorders. Given the wide range of motivations and the great variation in readiness to change (see Table 1), we used pre-intervention readiness to change as a covariate in subsequent analyses.
Table 1.
Description of Study Sample (N = 180).
| MORE (N = 64) | CBT (N = 64) | TAU (N = 52) | |
|---|---|---|---|
| Age | 37.7 (10.4) | 36.5 (11.2) | 38.7 (9.8) |
| Race | |||
| White | 26 (40%) | 28 (44%) | 22 (42%) |
| Black | 29 (45%) | 28 (44%) | 23 (44%) |
| Other | 9 (14%) | 8 (12%) | 7 (14%) |
| Lifetime months incarcerated | 45.4 (59.9) | 38.1 (54.7) | 35.7 (52.8) |
| Readiness to Change | |||
| Pre-contemplation | 11 (17%) | 11 (17%) | 6 (12%) |
| Contemplation | 38 (59%) | 36 (56%) | 29 (56%) |
| Preparation | 15 (23%) | 17 (27%) | 13 (25%) |
| Not answered | 0 (0%) | 0 (0%) | 4 (7%) |
| Substance Use Disorder Diagnosis | |||
| Alcohol dependence | 30 (47%) | 23 (36%) | 28 (40%) |
| Cocaine dependence | 27 (42%) | 26 (41%) | 27 (52%) |
| Opioid dependence | 16 (25%) | 23 (36%) | 10 (19%) |
| Cannabis dependence | 12 (19%) | 19 (30%) | 16 (31%) |
| Sedative dependence | 3 (5%) | 2 (3%) | 0 (0%) |
| Amphetamine dependence | 2 (3%) | 2 (3%) | 1 (2%) |
| Cocaine abuse | 1 (2%) | 4 (6%) | 2 (4%) |
| Alcohol abuse | 3 (5%) | 6 (9%) | 1 (2%) |
| Cannabis abuse | 3 (5%) | 3 (5%) | 0 (0%) |
| Hallucinogen abuse | 0 (0%) | 3 (5%) | 1 (2%) |
| Any drug use disorder dx | 48 (75%) | 55 (85%) | 36 (69%) |
| Number of drug use disorder dx | 1.30 (.50) | 1.46 (.61) | 1.42 (.61) |
| Any alcohol + drug use disorder dx | 24 (38%) | 19 (30%) | 20 (38%) |
| Number of total alcohol + drug use dx | 1.66 (.72) | 1.69 (.74) | 1.70 (.80) |
| Post-Traumatic Stress Diagnosis | |||
| Full post-traumatic stress disorder | 13 (20%) | 17 (27%) | 15 (29%) |
| Partial post-traumatic stress disorder | 19 (30%) | 29 (44%) | 19 (37%) |
| Psychiatric Disorder Diagnosis | |||
| Major depressive disorder | 6 (9%) | 5 (8%) | 9 (17%) |
| Bipolar disorder | 3 (5%) | 4 (6%) | 4 (8%) |
| Generalized anxiety disorder | 5 (8%) | 7 (11%) | 2 (4%) |
| Social phobia | 6 (9%) | 1 (2%) | 6 (12%) |
| Panic disorder | 1 (2%) | 1 (2%) | 2 (4%) |
| Other mood or anxiety disorder | 19 (30%) | 18 (28%) | 11 (21%) |
| Antisocial personality disorder | 4 (6%) | 1 (2%) | 2 (4%) |
| Other | 7 (11%) | 10 (16%) | 1 (2%) |
Note: For the sake of parsimony, multiple diagnoses were collapsed into higher-order categories when appropriate: e.g., major depressive disorder and bipolar disorder categories include all subtypes and specifiers, and the table entry “other mood or anxiety D/O” comprises DSM-IV TR diagnoses 292.84; 292.89; 296.90; 300.00; 300.29; 300.4; and 311.
Two levels of random effects were included: the first level had a random intercept for individuals nested within groups, and the second level had a random intercept for group (for a similar cluster RCT modeling approach, see Schnurr et al., 2003). Denominator degrees of freedom were obtained by a Satterthwaite approximation (Satterthwaite, 1946). Sensitivity analysis of treatment effects on craving controlled for between-groups differences in the number of pre-intervention substance use disorder diagnoses, and sensitivity analysis of treatment effects on traumatic stress symptoms controlled for between-groups differences in pre-intervention PTSD diagnosis. Secondary analyses were conducted to examine within-group change from pre- to post-treatment. Power analysis was conducted Optimal Design software using a medium effect size estimate derived from two earlier trials of MORE compared to an active control group (Garland et al., 2010; Garland, Manusov, et al., 2014) and the median intra-cluster correlation (ICC; ρ = .04) derived from a meta-analysis of cluster RCTs (Eldridge, Ashby, Feder, Rudnicka, & Ukoumunne, 2004). With a medium effect size (d = .50) and 27 clusters (9 per condition), and an ICC of ρ = .04, power is .85.
RESULTS
Participant background characteristics are presented in Table 1. The most prevalent substance use disorders in the sample were alcohol dependence (45%) and cocaine dependence (44%), whereas PTSD was the most common psychiatric disorder − 25% of participants met criteria for full PTSD and 37% met criteria for partial PTSD. Other mood and anxiety disorders were also fairly common. Nearly half (47%) of participants had 2 or more substance use disorders (M = 1.7, SD = 0.8, range 1 – 4). There were no significant between-groups differences in the average number of substance use disorder diagnoses, p = .35. In addition, all participants reported experiencing at least one type of traumatic event in their lives. Participants reported having experienced a wide range of traumatic incidents: 81.1% reported having been struck by someone who had attempted to hurt them; 77% experienced a terrifying event; 76% witnessed someone be beaten; 64% witnessed someone severely injured or killed; 64% had been mugged with a weapon; 64% had been attacked by a weapon by someone trying to hurt or kill them; and 25% had been sexually assaulted or raped. On average, participants had experienced 5.2 (SD = 1.7) different categories of traumatic life events and there were no significant between-groups differences in trauma exposure (p = .17). Many participants also had extensive histories of involvement in the criminal justice system; the mean number of lifetime months spent incarcerated was 40.1 (SD = 55.9).
Primary Outcomes
Table 2 presents descriptive statistics for outcomes by intervention condition and time, whereas Table 3 presents results of linear mixed modeling analyses. Significant fixed effects of time were observed for craving (p = .01), such that across all three treatment conditions, participants improved in craving over the 10 weeks of treatment. The treatment X time interaction term indicated that MORE was associated with significantly greater decreases in craving than CBT (p = .03). There were no significant differences between MORE and TAU on changes in craving (p = .18). However, in a sensitivity analysis controlling for extent of polysubstance use at pre-treatment, participants in MORE reported significantly less craving than Seeking Safety (p = .02) and TAU (p = .04).
Table 2.
Primary and Secondary Outcomes as a Function of Treatment and Time of Measurement: Intention-to-Treat Analysis (N = 180).
| MORE (N=64) | CBT (N=64) | TAU (N=52) | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| Outcome | Pre | Post | es | Pre | Post | es | Pre | Post | es |
| PACS Craving | 25.06 (1.97) | 19.66 (1.78) | 0.4** | 22.82 (1.88) | 22.36 (1.76) | 0.0 | 25.68 (2.18) | 23.59 (2.03) | 0.1 |
| PCL-C PTSD | 36.07 (1.98) | 31.56 (1.99) | 0.3* | 36.59 (1.89) | 36.54 (1.96) | 0.0 | 39.81 (2.19) | 39.53 (2.26) | 0.0 |
| BSI Depression | 12.91 (.79) | 10.52 (.78) | 0.4* | 12.59 (.77) | 10.78 (.83) | 0.3* | 13.95 (.85) | 12.54 (.85) | 0.2 |
| BSI Anxiety | 11.20 (.82) | 9.65 (.76) | 0.3* | 10.78 (.78) | 9.92 (.81) | 0.1 | 12.27 (.89) | 10.95 (.83) | 0.2 |
| FFMQ Mindfulness | 125.30 (3.29) | 138.79 (3.04) | 0.5*** | 130.14 (3.06) | 129.92 (2.91) | 0.0 | 126.81 (3.64) | 129.25 (3.49) | 0.1 |
| PANAS Positive Affect | 34.16 (1.70) | 40.08 (1.54) | 0.5** | 34.39 (1.59) | 37.53 (1.52) | 0.3* | 31.49 (1.79) | 32.82 (1.75) | 0.1 |
| PANAS Negative Affect | 34.40 (1.88) | 30.23 (1.74) | 0.3* | 32.60 (1.79) | 32.88 (1.77) | 0.0 | 36.37 (1.99) | 36.05 (1.95) | 0.0 |
Data are given as mean (SE). ES = within-group effect size (Hedge’s g).
p< .05 vs. pre-treatment within a treatment group
p≤.01 vs. pre-treatment within a treatment group
p≤.001 vs. pre-treatment within a treatment group
Table 3.
Results of Linear Mixed Models on Primary and Secondary Outcomes (N = 180).
| Outcome | Time | Time X MORE vs. CBT | Time X MORE vs. TAU | Time X CBT vs. TAU |
|---|---|---|---|---|
| PACS Craving | 6.21,101.9, p=.01 | 4.81,101.1, p=.03 | 1.81,101.2, p=.18 | 0.51,103.2, p=.49 |
| PCL-C PTSD | 2.61,104.2, p=.10 | 4.51,103.8, p=.04 | 3.711,103.8, p=.05 | 0.01,104.6, p=.99 |
| BSI Depression | 18.51,79.6, p< .001 | 0.31,79.4, p=.56 | 1.51,79.2, p=.23 | 0.41,80.2, p=.55 |
| BSI Anxiety | 7.21,81.9, p=.009 | 0.61,81.0, p=.44 | 0.41,81.9, p=.54 | 0.01,82.6, p=.88 |
| FFMQ Mindfulness | 11.31,82.9, p=.001 | 17.31,81.9, p < .001 | 8.71,82.3, p=.004 | 0.71,84.0, p=.42 |
| PANAS Positive Affect | 13.31,95.1, p<.001 | 2.11,95.4, p=.15 | 4.31,94.3, p=.04 | 0.51,95.5, p=.43 |
| PANAS Negative Affect | 1.51,88.8, p=.23 | 4.21,89.1, p =.04 | 2.91,87.3, p =.09 | 0.11,89.6, p=.78 |
MORE = Mindfulness-Oriented Recovery Enhancement. CBT = Cognitive-Behavioral Therapy. TAU = Treatment-As-Usual. Note: All results are presented as F-values (Fdf1,df2). All linear mixed models included a fixed effect of time, treatment group, cohort, and custom contrast coded time X treatment interactions (depicted here), and were adjusted for pre-intervention levels of readiness to change. Exact p-values are reported.
While the fixed effect of time was non-significant for post-traumatic stress symptoms, significant treatment X time interactions were observed, such that MORE was associated with greater decreases in post-traumatic stress than CBT (p = .04), and TAU (p = .05). Controlling for presence vs. absence of PTSD diagnosis at pre-treatment, MORE was associated with significantly greater decreases in post-traumatic stress symptoms in this subsample than CBT (p = .04), but not TAU (p = .06). Additional subanalyses of the sample meeting full PTSD criteria revealed the same pattern of results – MORE was associated with significantly greater reduction in PTSD symptoms than CBT, but not TAU.
Significant fixed effects of time were observed for symptoms of depression (p < .001) and anxiety (p = .01), such that across all three treatment conditions, participants improved in these domains of psychiatric distress over the 10 weeks of treatment. However, there were no significant between-group differences in symptoms of depression and anxiety over time. Furthermore, CBT and TAU did not significantly differ with regard to changes in craving or post-traumatic stress symptoms.
Secondary Outcomes
Significant treatment X time interactions were observed for dispositional mindfulness, such that MORE was associated with greater increases in dispositional mindfulness than CBT (p < .001) and TAU (p = .004). Participants in MORE also reported significantly greater increases in positive affect than TAU (p = .04). Similarly, MORE was associated with significantly greater decreases in negative affect than CBT (p = .04).
With regard to the comparison of MORE and CBT, 4/7 outcomes were significantly different, and 3/7 outcomes were significantly different between MORE and TAU. Additional analyses examined change from pre- to post-treatment within each treatment condition (Table 2). Among MORE participants, there were significant improvements in craving, post-traumatic stress, symptoms of depression and anxiety, mindfulness, and positive and negative affect.
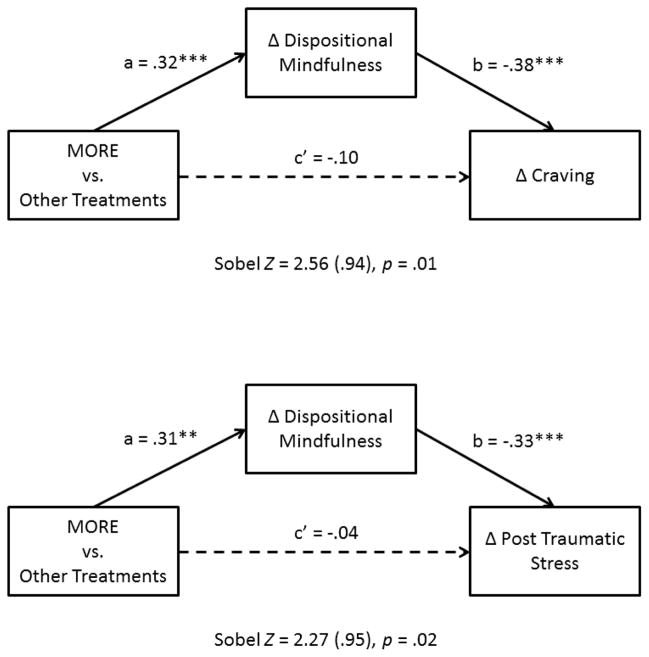
Changes in Mindfulness as Therapeutic Mechanism
Changes in dispositional mindfulness were significantly negatively correlated with changes in craving (r = −.43, p <.001) and post-traumatic stress symptoms (r = −.37, p < .001). To examine mindfulness as a therapeutic mechanism, two path analyses were conducted with a dummy coded treatment variable (MORE vs. other treatments) as the independent variable, changes in craving and PTSD as dependent variables, and changes in mindfulness as a mediator (see Figure 2). Sobel test statistics (craving Sobel p = .01; post-traumatic stress Sobel p = .02) indicated the presence of a significant indirect effect of changes in mindfulness on these clinical outcomes (see Figure 2a and 2b).
Figure 2.
The indirect effect of Mindfulness-Oriented Recovery Enhancement on craving (Figure 2a) and post-traumatic stress symptoms (Figure 2b) through increasing dispositional mindfulness was statistically significant.
Treatment Fidelity and Attendance Data
Regarding CBT fidelity scores, adherence was adequate, with means as follows on a 0–3 scale: on intervention items, 2.5 (SD = 0.4); on process items, 2.7 (SD = 0.4). Regarding scores on the MORE fidelity checklist, adherence was also adequate, with means as follows on a 0–3 scale: on intervention items, 2.9 (SD = 0.2); on process items, 2.8 (SD = 0.3). Because attendance of treatment groups was mandatory according to therapeutic community rules, attendance was high and there were no significant between-groups differences observed: CBT participants attended on average 9.1 (SD = 1.9) sessions, whereas MORE participants attended on average 9.0 (SD = 2.0) sessions.
DISCUSSION
This pragmatic trial represents the first head-to-head comparison of MORE against CBT for co-occurring psychiatric and substance use disorders. Results from this trial indicate that MORE was associated with modest yet statistically significant improvements in craving, post-traumatic stress symptoms, and positive and negative affect from pre- to post-treatment. Importantly, we identified a significant indirect effect of MORE on craving and post-traumatic stress through increased dispositional mindfulness, suggesting that this intervention produced therapeutic effects by virtue of its ability to enhance mindful awareness in everyday life. Though the observed effect sizes ranged from small to moderate, these positive outcomes are notable, in that participants suffered from multiple vulnerabilities, including psychiatric disturbance, trauma, addiction, incarceration, and homelessness. Also, people residing in therapeutic communities often evidence improvements in mental health and addiction symptoms (Magor-Blatch, Bhullar, Thomson, & Thorsteinsson, 2014), so demonstrating effects over and above TAU is often difficult in this population; nonetheless, MORE outperformed TAU across several domains.
In this clinically-complex sample of individuals with COD, participation in MORE was associated with reduced craving for drugs and alcohol. MORE provides training in a twofold technique for coping with craving. First, patients are instructed to cultivate metacognitive awareness of the craving experience, using mindfulness to deconstruct the experience into its constituent sensorial, affective, and cognitive subcomponents. If craving becomes too intense, patients are instructed to reorient attention to the sensation of breathing, as a means of disrupting rumination and engaging parasympathetic regulation. Once arousal has been titrated to a more manageable level, the individual is taught to refocus attention back to the experience of craving. Following this attentional process, patients are taught to consciously contemplate the negative consequences of satiating the craving, as well as to anticipate the positive consequences of remaining abstinent. This this dual-stage procedure may engage top-down, conscious cognitive control over bottom-up, automatic addictive impulses, subserved by activation of prefrontal-striatal brain circuits (Garland, Froeliger, & Howard, 2013).
MORE provides a similar approach to regulate negative thoughts and emotions in the context of stress, whereby individuals are instructed to first become aware of distressing mental contents, and then to re-orient attention to the breath as a means of disrupting perseverative cognition (e.g., catastrophizing and ruminating) on the stressor. Once the automatic emotional reaction is interrupted, the cognitive flexibility afforded by the practice of mindfulness may increase access to an expanded set of information regarding the meaning of the stressor from which alternative appraisals can be generated. Participants are taught to oscillate between mindfully disengaging from negative automatic appraisals and generating positive reappraisals to reduce psychological distress and motivate healthy coping behavior. In this sense, MORE uses mindfulness training to facilitate cognitive reappraisal; this potentially synergistic “mindful reappraisal” approach may have led to the observed reduction in post-traumatic stress. In that regard, more frequent use of cognitive reappraisal predicts attenuated PTSD symptoms (Boden, Bonn-Miller, Kashdan, Alvarez, & Gross, 2012), and theory and empirical evidence indicate that mindfulness promotes positive reappraisals of life adversity to enhance post-traumatic growth and eudaimonic well-being (Garland, Farb, Goldin, & Fredrickson, in press). To that latter point, MORE was associated with significant within-group improvements in positive and negative affect, as well as in symptoms of depression and anxiety. The affective benefits of MORE may stem from its integration of mindfulness and reappraisal, as well as from its emphasis on mindful savoring, the process of attending to and appreciating pleasant events and the positive emotions that flow from them (Bryant & Veroff, 2007). Future studies should measure reappraisal and savoring as potential treatment mediators.
It should be noted that the observed clinical outcomes were measured after 10 weeks of treatment. The duration of these therapeutic benefits is unknown. It is quite possible that the observed significant-between groups differences might have dissipated at a later time point, or that CBT and/or TAU might have had more pronounced treatment effects at a later follow-up. Contrary to our expectations, in the present study, CBT was not found to significantly improve craving or post-traumatic stress symptoms. However, these null results are consistent with a recent meta-analysis of RCTs for people with co-occurring substance use disorders and PTSD which found that on average, non-trauma focused group CBT interventions (those that do not directly process trauma memories) do not produce statistically significant effects on traumatic stress or drug-related outcomes in this population, and even for efficacious treatments, effect sizes are small (Roberts, Roberts, Jones, & Bisson, 2015). However, this meta-analysis did not take patient complexity into account, and when doing so, findings are highly divergent with regard to what treatments work best (Gerger, Munder, & Barth, 2014). It is also possible that the low-dose provision of coping skill training to TAU may have obscured differences between the CBT and TAU groups. It should be noted that though MORE outperformed CBT on PTSD symptom reduction, the observed between-groups differences were quite small, and statistical power for assessing this outcome may have been somewhat limited given that only 62% of the sample met criteria for full or partial PTSD. Also, the psychometrics of the trauma history measure used in the present study have not been evaluated.
In addition, the present study was limited by a lack of biochemical measures of abstinence. To assess effects of the study interventions on drug and alcohol use, it would have been ideal if biochemical verification of abstinence was conducted consistently at regular time intervals. However, self-reports of abstinence were corroborated by random urinalyses conducted at the TC on an as needed basis, as well as through daily observation by program staff. According to this data, 98% of participants remained abstinent over the course of the study. The high rate of abstinence may have been due to the fact that participants (who had been previously homeless) were residents in a long-term therapeutic community which provided housing, vocational training, and an array of supports to those who remained abstinent. Study findings may not be generalizable to individuals with COD with lower levels of motivation who would not be willing to enroll in such an extensive, long-term treatment program. Future studies should quantify distal outcomes through biochemical confirmation of abstinence and structured diagnostic interviews at 12- and 24-month follow-ups, to determine the impact of treatment of substance use and psychiatric disorder status.
In spite of these limitations, the present study, which compared MORE to an empirically-supported CBT intervention for formerly homeless individuals with severe substance use and psychiatric disorders, provides evidence that MORE is associated with modest but statistically significant therapeutic effects on factors integral to the co-occurrence of addiction, emotional distress, and trauma. Thus, study findings suggest that MORE, as an integrative therapy designed to enhance self-regulatory capacity, may be a promising treatment for some of the most vulnerable and marginalized individuals in our society: those afflicted by poverty, violence, and a range of complex, intersecting clinical conditions.
Figure 1.
Study flow diagram.
There is a high comorbidity between substance use and psychiatric disorders
CBT interventions may efficiently target co-occurring disorders
Mindfulness-Oriented Recovery Enhancement (MORE) is a novel treatment
MORE reduced craving and traumatic stress symptoms more than CBT
Therapeutic effects of MORE were statistically mediated by mindfulness
MORE holds promise as a treatment for co-occurring disorders
Acknowledgments
This study was funded by grant TI 020489 from the Substance Abuse and Mental Health Services Administration (SAMHSA) awarded to ARL. ELG was also supported by grant R34DA037005 from the National Institute on Drug Abuse (NIDA) during the preparation of this manuscript. Neither SAMHSA nor NIDA had any role in the interpretation of the data and preparation, review, or approval of the manuscript.
Footnotes
Conflict of interest: The first author (ELG) developed the Mindfulness-Oriented Recovery Enhancement (MORE) intervention, and has received income from the MORE treatment manual (Garland, 2013) and therapist trainings.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Eric L. Garland, University of Utah
Amelia Roberts-Lewis, University of North Carolina at Chapel Hill.
Christine D. Tronnier, Smith College
Rebecca Graves, Triangle Residential Options for Substance Abusers, Inc.
Karen Kelley, Triangle Residential Options for Substance Abusers, Inc.
References
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13:27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: an affective processing model of negative reinforcement. Psychological Review. 2004;111:33–51. doi: 10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- Boden MT, Bonn-Miller MO, Kashdan TB, Alvarez J, Gross JJ. The interactive effects of emotional clarity and cognitive reappraisal in posttraumatic stress disorder. Journal of Anxiety Disorders. 2012;26(1):233–238. doi: 10.1016/j.janxdis.2011.11.007. [DOI] [PubMed] [Google Scholar]
- Bowen S, Witkiewitz K, Clifasefi SL, Grow J, Chawla N, Hsu SH, et al. Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders: a randomized clinical trial. JAMA Psychiatry. 2014;71(5):547–556. doi: 10.1001/jamapsychiatry.2013.4546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant FB, Veroff J. Savoring: A new model of positive experience. Lawrence Erlbaum Associates Publishers; 2007. Retrieved from http://psycnet.apa.org/psycinfo/2006-11872-000. [Google Scholar]
- Chiesa A, Serretti A. Are mindfulness-based interventions effective for substance use disorders? A systematic review of the evidence. Substance Use & Misuse. 2014;49(5):492–512. doi: 10.3109/10826084.2013.770027. [DOI] [PubMed] [Google Scholar]
- Cukor J, Wyka K, Jayasinghe N, Difede J. The nature and course of subthreshold PTSD. Journal of Anxiety Disorders. 2010;24(8):918–923. doi: 10.1016/j.janxdis.2010.06.017. http://doi.org/10.1016/j.janxdis.2010.06.017. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol Med. 1983;13:595–605. [PubMed] [Google Scholar]
- DiClemente CC, Schlundt D, Gemmell L. Readiness and stages of change in addiction treatment. American Journal on Addictions. 2004;13(2):103–119. doi: 10.1080/10550490490435777. [DOI] [PubMed] [Google Scholar]
- Eldridge SM, Ashby D, Feder GS, Rudnicka AR, Ukoumunne OC. Lessons for cluster randomized trials in the twenty-first century: a systematic review of trials in primary care. Clinical Trials. 2004;1(1):80–90. doi: 10.1191/1740774504cn006rr. http://doi.org/10.1191/1740774504cn006rr. [DOI] [PubMed] [Google Scholar]
- Fazel S, Khosla V, Doll H, Geddes J. The Prevalence of Mental Disorders among the Homeless in Western Countries: Systematic Review and Meta-Regression Analysis. PLoS Med. 2008;5(12):e225. doi: 10.1371/journal.pmed.0050225. http://doi.org/10.1371/journal.pmed.0050225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flannery BA, Volpicelli JR, Pettinati HM. Psychometric properties of the Penn alcohol craving scale. Alcoholism: Clinical and Experimental Research. 1999;23(8):1289–1295. [PubMed] [Google Scholar]
- Flynn PM, Brown BS. Co-occurring disorders in substance abuse treatment: Issues and prospects. Journal of Substance Abuse Treatment. 2008;34(1):36–47. doi: 10.1016/j.jsat.2006.11.013. http://doi.org/10.1016/j.jsat.2006.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland E, Froeliger B, Howard M. Mindfulness training targets neurocognitive mechanisms of addiction at the attention-appraisal-emotion interface. Name: Frontiers in Psychiatry. 2013;4:173. doi: 10.3389/fpsyt.2013.00173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL. Mindfulness-Oriented Recovery Enhancement for Addiction, Stress, and Pain. Washington, D.C: NASW Press; 2013. [Google Scholar]
- Garland EL, Boettiger CA, Howard MO. Targeting cognitive-affective risk mechanisms in stress-precipitated alcohol dependence: An integrated, biopsychosocial model of allostasis, automaticity, and addiction. Medical Hypotheses. 2011;76:745–754. doi: 10.1016/j.mehy.2011.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Farb NA, Goldin PR, Fredrickson BL. Mindfulness broadens awareness and builds eudaimonic meaning: A process model of mindful positive emotion regulation. Psychological Inquiry. doi: 10.1080/1047840X.2015.1064294. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Froeliger B, Howard MO. Effects of Mindfulness-Oriented Recovery Enhancement on reward responsiveness and opioid cue-reactivity. Psychopharmacology. 2014a;231(16):3229–3238. doi: 10.1007/s00213-014-3504-7. http://doi.org/10.1007/s00213-014-3504-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Froeliger B, Howard MO. Neurophysiological evidence for remediation of reward processing deficits in chronic pain and opioid misuse following treatment with Mindfulness-Oriented Recovery Enhancement: exploratory ERP findings from a pilot RCT. Journal of Behavioral Medicine. 2014b;38(2):327–336. doi: 10.1007/s10865-014-9607-0. http://doi.org/10.1007/s10865-014-9607-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Gaylord SA, Boettiger CA, Howard MO. Mindfulness training modifies cognitive, affective, and physiological mechanisms implicated in alcohol dependence: Results of a randomized controlled pilot trial. Journal of Psychoactive Drugs. 2010;42(2):177–192. doi: 10.1080/02791072.2010.10400690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Howard MO. A transdiagnostic perspective on cognitive, affective, and neurobiological processes underlying human suffering. Research on Social Work Practice. 2013a 1049731513503909. [Google Scholar]
- Garland EL, Howard MO. Mindfulness-oriented recovery enhancement reduces pain attentional bias in chronic pain patients. Psychotherapy and Psychosomatics. 2013b;82(5):311–318. doi: 10.1159/000348868. [DOI] [PubMed] [Google Scholar]
- Garland EL, Manusov EG, Froeliger B, Kelly A, Williams JM, Howard MO. Mindfulness-oriented recovery enhancement for chronic pain and prescription opioid misuse: Results from an early-stage randomized controlled trial. Journal of Consulting and Clinical Psychology. 2014;82(3):448. doi: 10.1037/a0035798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Roberts-Lewis A. Differential roles of thought suppression and dispositional mindfulness in posttraumatic stress symptoms and craving. Addictive Behaviors. 2013;38(2):1555–1562. doi: 10.1016/j.addbeh.2012.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Roberts-Lewis A, Kelley K, Tronnier C, Hanley A. Cognitive and Affective Mechanisms Linking Trait Mindfulness to Craving Among Individuals in Addiction Recovery. Substance Use & Misuse. 2014;49(5):525–535. doi: 10.3109/10826084.2014.850309. http://doi.org/10.3109/10826084.2014.850309. [DOI] [PubMed] [Google Scholar]
- Gerger H, Munder T, Barth J. Specific and Nonspecific Psychological Interventions for PTSD Symptoms: A Meta-Analysis With Problem Complexity as a Moderator. Journal of Clinical Psychology. 2014;70(7):601–615. doi: 10.1002/jclp.22059. http://doi.org/10.1002/jclp.22059. [DOI] [PubMed] [Google Scholar]
- Goyal M, Singh S, Sibinga EM, Gould NF, Rowland-Seymour A, Sharma R, et al. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Internal Medicine. 2014;174(3):357–368. doi: 10.1001/jamainternmed.2013.13018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kearney DJ, McDermott K, Malte C, Martinez M, Simpson TL. Effects of participation in a mindfulness program for veterans with posttraumatic stress disorder: a randomized controlled pilot study. Journal of Clinical Psychology. 2013;69(1):14–27. doi: 10.1002/jclp.21911. [DOI] [PubMed] [Google Scholar]
- Kelly A, Garland EL. Trauma-Informed Mindfulness-Based Stress Reduction for Female Survivors of Interpersonal Violence: Results from a Stage I RCT. Journal of Clinical Psychology. doi: 10.1002/jclp.22273. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khantzian EJ. The self-medication hypothesis of substance use disorders: a reconsideration and recent applications. Harv Rev Psychiatry. 1997;4:231–44. doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- Kilgore PE. Epidemiology of Homelessness in the United States. Annals of Epidemiology. 2013;23(9):594. [Google Scholar]
- King AP, Erickson TM, Giardino ND, Favorite T, Rauch SA, Robinson E, Liberzon I. A pilot study of group mindfulness-based cognitive therapy (MBCT) for combat veterans with posttraumatic stress disorder (PTSD) Depression and Anxiety. 2013;30(7):638–645. doi: 10.1002/da.22104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koob GF. Alcoholism, corticotropin-releasing factor, and molecular genetic allostasis. Biol Psychiatry. 2008;63:137–8. doi: 10.1016/j.biopsych.2007.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koob GF, Le Moal M. Drug addiction, dysregulation of reward, and allostasis. Neuropsychopharmacology. 2001;24:97–129. doi: 10.1016/S0893-133X(00)00195-0. [DOI] [PubMed] [Google Scholar]
- Leeies M, Pagura J, Sareen J, Bolton JM. The use of alcohol and drugs to self-medicate symptoms of posttraumatic stress disorder. Depression and Anxiety. 2010;27(8):731–736. doi: 10.1002/da.20677. [DOI] [PubMed] [Google Scholar]
- Little RJ. A test of missing completely at random for multivariate data with missing values. Journal of the American Statistical Association. 1988;83:1198–1202. [Google Scholar]
- Magor-Blatch L, Bhullar N, Thomson B, Thorsteinsson E. A systematic review of studies examining effectiveness of therapeutic communities. Therapeutic Communities: The International Journal of Therapeutic Communities. 2014;35(4):168–184. [Google Scholar]
- Monti PM, Rohsenow DJ. Coping-skills training and cue-exposure therapy in the treatment of alcoholism. Alcohol Res Health. 1999;23:107–15. [PMC free article] [PubMed] [Google Scholar]
- Mylle J, Maes M. Partial posttraumatic stress disorder revisited. Journal of Affective Disorders. 2004;78(1):37–48. doi: 10.1016/s0165-0327(02)00218-5. [DOI] [PubMed] [Google Scholar]
- Najavits LM. Clinicians’ views on treating posttraumatic stress disorder and substance use disorder. Journal of Substance Abuse Treatment. 2002;22(2):79–85. doi: 10.1016/s0740-5472(02)00219-2. http://doi.org/10.1016/S0740-5472(02)00219-2. [DOI] [PubMed] [Google Scholar]
- Najavits LM. Seeking safety: A treatment manual for PTSD and substance abuse. Guilford Press; 2002. [DOI] [PubMed] [Google Scholar]
- Najavits LM, Hien D. Helping vulnerable populations: a comprehensive review of the treatment outcome literature on substance use disorder and PTSD. Journal of Clinical Psychology. 2013;69(5):433–479. doi: 10.1002/jclp.21980. [DOI] [PubMed] [Google Scholar]
- Najavits LM, Liese BS. Unpublished Measure. Harvard Medical School/McLean Hospital; Boston, MA: 2000. Seeking Safety Adherence Scale (revised) [Google Scholar]
- Najavits LM, Weiss RD, Shaw SR, Muenz LR. “Seeking safety”: Outcome of a new cognitive-behavioral psychotherapy for women with posttraumatic stress disorder and substance dependence. Journal of Traumatic Stress. 1998;11(3):437–456. doi: 10.1023/A:1024496427434. [DOI] [PubMed] [Google Scholar]
- Norcross JC, Krebs PM, Prochaska JO. Stages of change. Journal of Clinical Psychology. 2011;67(2):143–154. doi: 10.1002/jclp.20758. [DOI] [PubMed] [Google Scholar]
- Roberts NP, Roberts PA, Jones N, Bisson JI. Psychological interventions for posttraumatic stress disorder and comorbid substance use disorder: A systematic review and meta-analysis. Clinical Psychology Review. 2015;38:25–38. doi: 10.1016/j.cpr.2015.02.007. [DOI] [PubMed] [Google Scholar]
- Roland M, Torgerson DJ. Understanding controlled trials: What are pragmatic trials? BMJ. 1998;316(7127):285. doi: 10.1136/bmj.316.7127.285. http://doi.org/10.1136/bmj.316.7127.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satterthwaite FE. An approximate distribution of estimates of variance components. Biometrics Bulletin. 1946;2(6):110–114. [PubMed] [Google Scholar]
- Schnurr PP, Friedman MJ, Foy DW, Shea MT, Hsieh FY, Lavori PW, Bernardy NC. Randomized trial of trauma-focused group therapy for posttraumatic stress disorder: Results from a Department of Veterans Affairs cooperative study. Archives of General Psychiatry. 2003;60(5):481–489. doi: 10.1001/archpsyc.60.5.481. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. quiz 34–57. [PubMed] [Google Scholar]
- Singer J, Willett J. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. Oxford University Press; 2003. [Google Scholar]
- Skinner MD, Aubin HJ. Craving’s place in addiction theory: Contributions of the major models. Neuroscience & Biobehavioral Reviews. 2010;34(4):606–623. doi: 10.1016/j.neubiorev.2009.11.024. http://doi.org/16/j.neubiorev.2009.11.024. [DOI] [PubMed] [Google Scholar]
- Torchalla I, Strehlau V, Li K, Aube Linden I, Noel F, Krausz M. Posttraumatic stress disorder and substance use disorder comorbidity in homeless adults: Prevalence, correlates, and sex differences. Psychology of Addictive Behaviors. 2014;28(2):443–452. doi: 10.1037/a0033674. http://doi.org/10.1037/a0033674. [DOI] [PubMed] [Google Scholar]
- Urbaniak GC, Plous S. Research randomizer (version 3.0)[Computer software] 2011. Retrieved on April 22, 2011. [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54:1063–70. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM, et al. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility 1993 [Google Scholar]
- Witkiewitz K, Bowen S. Depression, craving, and substance use following a randomized trial of mindfulness-based relapse prevention. J Consult Clin Psychol. 2011;78:362–74. doi: 10.1037/a0019172. [DOI] [PMC free article] [PubMed] [Google Scholar]