Abstract
Background
Despite widespread implementation of compulsory treatment modalities for drug dependence, there has been no systematic evaluation of the scientific evidence on the effectiveness of compulsory drug treatment.
Methods
We conducted a systematic review of studies assessing the outcomes of compulsory treatment. We conducted a search in duplicate of all relevant peer-reviewed scientific literature evaluating compulsory treatment modalities. The following academic databases were searched: PubMed, PAIS International, Proquest, PsycINFO, Web of Science, Soc Abstracts, JSTOR, EBSCO/Academic Search Complete, REDALYC, SciELO Brazil. We also searched the Internet, and article reference lists, from database inception to July 15th, 2015. Eligibility criteria are as follows: peer-reviewed scientific studies presenting original data. Primary outcome of interest was post-treatment drug use. Secondary outcome of interest was post-treatment criminal recidivism.
Results
Of an initial 430 potential studies identified, nine quantitative studies met the inclusion criteria. Studies evaluated compulsory treatment options including drug detention facilities, short (i.e. 21-day) and long-term (i.e., 6 months) inpatient treatment, community-based treatment, group-based outpatient treatment, and prison-based treatment. Three studies (33%) reported no significant impacts of compulsory treatment compared with control interventions. Two studies (22%) found equivocal results but did not compare against a control condition. Two studies (22%) observed negative impacts of compulsory treatment on criminal recidivism. Two studies (22%) observed positive impacts of compulsory inpatient treatment on criminal recidivism and drug use.
Conclusion
There is limited scientific literature evaluating compulsory drug treatment. Evidence does not, on the whole, suggest improved outcomes related to compulsory treatment approaches, with some studies suggesting potential harms. Given the potential for human rights abuses within compulsory treatment settings, non-compulsory treatment modalities should be prioritized by policymakers seeking to reduce drug-related harms.
BACKGROUND
Globally, dependence to illicit and off-label drugs remains a key source of morbidity and mortality, and is implicated in criminal recidivism. For instance, 1.7 million of the world’s estimated 13 million people who inject drugs (PWID) are believed to be HIV-positive while more than 60% of PWID globally are estimated to be hepatitis C (HCV) positive.1 Illicit drug dependence is also estimated to have contribute to 20.0 million disability-adjusted life years in 2010,2 while, the United Nations Office on Drugs and Crime (UNODC) estimated that there were as many as 231,400 drug-related deaths in 2013, the majority of which were the result of drug overdoses.1 Additionally, a UNODC review found that between 56% and 90% of PWID reported imprisonment since initiating injection drug use.3
An increasing range of evidence-based treatment modalities have been found to be effective in improving outcomes from substance use disorder and attendant harms. For example, among individuals addicted to opioids, opioid substitution therapies (OST) including methadone and buprenorphine maintenance have been shown to reduce negative drug-related outcomes and to stabilize individuals suffering from opioid dependence.4–6 In a recent review, use of Suboxone (a combination of buprenorphine and naloxone) was demonstrated to be effective for opioid withdrawal.7–10 Evidence of effectiveness for pharmacotherapies for stimulant use disorder remains mixed.11,12 However, a large set of psychosocial tools have shown promise for a range of substance use disorders.13–18
In many settings, compulsory treatment modalities have been in place or are being implemented. For instance, a recent international review found that as of 2009, 69% of a sample of countries (n = 104) had criminals laws allowing for compulsory drug treatment.19 Compulsory drug treatment can be defined as the mandatory enrolment of individuals, who are often but not necessarily drug-dependent, in a drug treatment program.20 While most often consisting of forced inpatient treatment (i.e., individuals are placed under the care and supervision of treatment institutions), compulsory treatment can nevertheless be designed as outpatient treatment as well, either using an individualized treatment or group-based model that can include psychological assessment, medical consultation, and behavioral therapy to reduce substance use disorder.21 Compulsory drug treatment (particularly in inpatient settings) is often abstinence-based, and it is generally nested within a broader criminal justice-oriented response to drug-related harms.22 Compulsory treatment is distinct from coerced treatment, wherein individuals are provided with a choice, however narrow, to avoid treatment.23 Perhaps the most widely known example of coerced treatment is the drug treatment court model, which provides individuals charged with a drug-related crime with therapeutic measures in addition to criminal justice interventions under the auspices of the criminal justice system.24 While no systematic evaluation of the effectiveness of compulsory treatment approaches has been undertaken, observers have cited concerns regarding human rights violations within compulsory drug treatment centers.25,26 Further, while overviews as well as reviews on related topics (i.e., quasi-compulsory treatment) exist,27,28 no recent systematic assessments of the efficacy or effectiveness of compulsory or forced addiction treatment have been undertaken. This represents a critical gap in the literature given the implementation and scale up of compulsory treatment in a range of settings, including Southeast Asia, Latin America, and Australia.29–31
Observers have also noted that while the overall number of countries that employ compulsory drug treatment approaches is declining, the mean duration of care is increasing, as is the number of cases of individuals sentenced to compulsory drug treatment.19 Relatedly, observers have expressed concern with evidence that compulsory treatment centers incorporate therapeutic approaches generally unsupported by scientific evidence, and employ punishment for individuals who relapse into drug use.29,32,33 Given the need for scientific evidence to inform effective approaches to drug treatment, we therefore undertook a systematic review of the effectiveness of compulsory drug treatment.
METHODS
We employed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for the development of systematic reviews.34 A full review protocol is available by request to the corresponding author.
Eligibility criteria
Studies were eligible if they were peer-reviewed, and if they evaluated the impact of compulsory drug treatment on illicit drug-related outcomes. The primary outcome of interest was defined as the frequency of post-treatment drug use. The secondary outcome of interest was defined as any post-treatment drug-related criminal recidivism (i.e., post-treatment arrest or incarceration). Randomized control trials (RCTs) and observational studies were both eligible for inclusion. To be eligible, treatment interventions reported had to be compulsory; however, the type of intervention (e.g., inpatient abstinence-based therapy, outpatient group therapy, OST, etc.) could vary. Reviews as well as multi-component studies that did not disaggregate findings between components were not eligible if they did not provide specific data regarding the impact of compulsory treatment. Studies that assessed mandated treatment for legal or licit substances (i.e., alcohol, tobacco) were also not eligible. Further, studies that only evaluated outcomes such as attitudinal or psychosocial change, or psychological functioning related to substance use were excluded. Finally, studies that evaluated coerced or quasi-compulsory treatment (i.e., wherein individuals are provided with a choice between treatment and a punitive outcome such as incarceration such as a drug treatment court model) were excluded.
Information sources
We searched the following 10 electronic databases: Pubmed, EBSCOhost/Academic Search Complete, Cochrane Central, PAIS International/Proquest, JSTOR, PsycINFO, Soc Abstracts, Web of Science, REDALYC (Spanish language) and Scielo Brazil (Portuguese language). We also searched the internet (Google, Google Scholar), relevant academic conference abstract lists, and scanned the references of potentially eligible studies.
Search
We searched all English-, Spanish- and Portuguese-language studies and abstracts and set no date limits. The following search terms were used: “forced treatment,” “compulsory treatment,” “substance abuse,” “substance use,” “mandated treatment,” “mandatory treatment,” “addiction,” “addiction treatment,” “involuntary treatment,” “involuntary addiction treatment.” The terms were searched as keywords and mapped to database specific subject headings/controlled vocabulary terms when available, including MeSH terms for PubMed searches. Each database was searched from its inception to its most recent update as of June 15th, 2015.
Study selection
Two investigators (MM, CR) conducted the search independently and in duplicate using a predefined protocol. The investigators scanned all abstracts and obtained full texts of articles that potentially met the eligibility criteria. Validity was assessed in duplicate based on eligibility criteria. After all potentially eligible studies were collected, three investigators met to achieve consensus by comparing the two review datasets (MM, CR, DW). Differences were reviewed by three investigators (MM, CR, DW) and a final decision to include or exclude was then made.
Data extraction process
Between September 10th, 2014 and June 15th, 2015, data were extracted using a standardized form soliciting data on study design, setting, sample size, participant characteristics, type of compulsory intervention, measures of effectiveness, and study quality. Given the variance in study methodologies and treatment interventions, we extracted a range of summary measures, including difference in means, risk ratio, and odds ratio. The data were then entered into an electronic database.
Risk of publication bias
Compulsory drug treatment centers have been implemented or brought to scale in a number of settings, including Vietnam, China, and Brazil. However, these settings produce disproportionately less academic scholarship than other settings such as established market economies. For this reason, there is a potential risk of publication bias that may result in a smaller number of peer-reviewed evaluations of compulsory treatment in settings in which these interventions are more widely implemented. This may, in turn, affect the publication of studies relevant to the present systematic review.
Additional analyses
Study quality was assessed using the Downs & Black criteria by two authors independently (MM, CR).35 This scale evaluates five domains: reporting, external validity, risk of bias, confounding, and statistical power.
Given the wide variance in intervention design and reported outcomes, it was not feasible to perform a meta-analysis of findings.
Role of the funding source & Ethics Approval
This study was supported by the Canadian Institutes of Health Research and the Open Society Foundations. At no point did any external funder play a role in the collection, analyses, or interpretation of data, writing of the manuscript or decision to publish. All authors had complete access to all data, and all had final responsibility to submit the manuscript for publication. No ethics approval was required for this review.
RESULTS
Study selection and characteristics
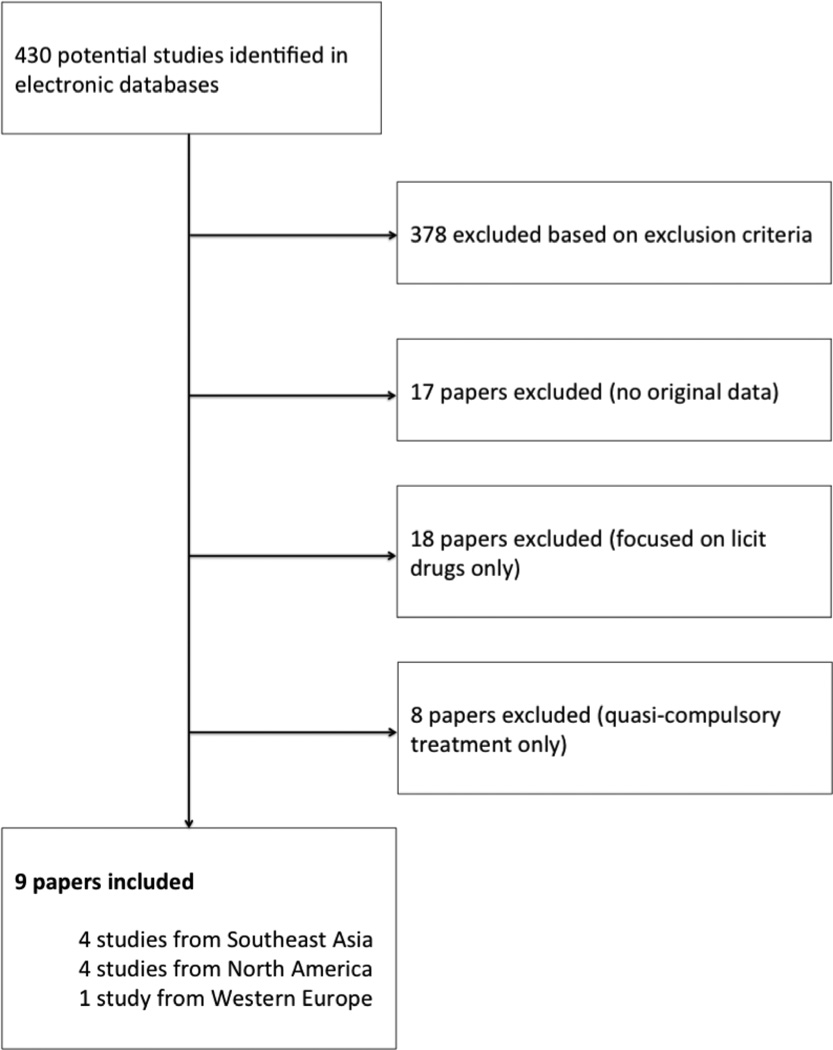
Overall, as seen in Figure 1, 430 studies were initially identified, of which 378 were excluded because they did not present primary and/or specific data on compulsory treatment. Of the remaining 52 studies, 17 were excluded because they constituted reviews or editorials, 18 were excluded because they did not focus on illicit drug use (i.e., they focused on alcohol treatment), and 8 studies were excluded because they evaluated quasi-compulsory treatment rather than compulsory treatment interventions. Nine studies met the inclusion criteria (combined n = 10,699). Three studies employed longitudinal observational approaches, four studies employed prospective case control designs, one study employed a cross-sectional design, and one study employed a quasi-experimental design. Six studies evaluated compulsory inpatient treatment or drug detention, one study evaluated prison/detention-based treatment, and two studies evaluated compulsory community-based treatment.
Figure 1.
Screening and study selection process
Methodological quality assessment
The Downs & Black scale has a possible score of 0 to 18, with 18 being a perfect score (highest quality). The median score for eligible studies was 12 (Interquartile Range: 9.5 – 15). All studies failed to undertake adequate steps to mitigate all risk of bias; eight studies (89%) did not optimally address risk of confounding, and five studies (56%) did not report all relevant study characteristics, methods, or findings. One study36 (11%) was only available as an abstract.
Results of individual studies
Three studies reported no significant impacts of compulsory treatment on substance use compared with control interventions.36–38 Two studies found equivocal results but did not compare against a control condition (e.g., voluntary drug treatment).39,40 Two studies observed negative impacts of compulsory treatment on criminal recidivism.41,42 Two studies found positive outcomes: one study observed a small significant impact of compulsory inpatient treatment on criminal recidivism,43 and a retrospective study found improved drug use outcomes within the first week of release after treatment.40
Six studies evaluated compulsory inpatient treatment or drug detention.36–39,41,43 Huang and colleagues examined the impact of mandatory inpatient drug treatment on post-treatment drug use patterns over the period of a year among participants in Chongquing, China (n = 177).41 As the authors note, Chinese police are given authority over mandatory drug treatment facilities, and have the power to detain individuals within these facilities for a period of weeks to several months.41 While the allocation of treatment varies by facility, treatment modalities commonly offered include “physical exercise, moral and legal education, drug and health education, and skill training (e.g., computer skills).”41 The authors do not, however, provide specific data on the content of any of these activities. The authors did not specify what type of treatment participants received, referring only to treatment and counseling. However, 46% of respondents reported using illicit drugs within a month to six months after release from mandatory treatment; a further 10% relapsed within one year.
Sun and colleagues compared relapse into drug use among a sample of heroin users in China (n = 615) enrolled in mandatory detoxification, volunteer detoxification, and detoxification with ‘re-education through labor’ (i.e., compulsory drug detention).36 Overall relapse within a year among the sample was 98%; 22% relapsed within three days, and 52% relapsed within one month. There was no significant difference between rates of relapse between sample participants enrolled in mandatory detoxification, volunteer detoxification, or detoxification in a compulsory drug detention center.36
Hiller and colleagues investigated the impact of a mandated six-month residential addiction treatment intervention on post-treatment criminal recidivism.43 Participants in Dallas, Texas (n = 506) were mandated to participate in a modified therapeutic community (TC), defined as addiction treatment provided within a controlled environment within which supervision is maximized.43 All participants were probationers or individuals arrested for drug-related crimes in Dallas county. Three groups were compared: a graduate group (n = 290; participants who successfully completed six months of the TC treatment process), a dropout group (n = 116; participants who failed to complete six months within the TC), and a comparison group (n = 100) comprised of a random sample of probationers from the Dallas county probationers list. The authors then compared the 1-year and 2-year incarceration rates across the three comparison groups, and found no significant differences after 1-year across all three groups (20% of the dropout group, 17% of the graduate group, and 13% of the comparison group were re-arrested and incarcerated; p > 0.05). The proportion of participants incarcerated within 2 years did not differ significantly between the graduate and comparison groups (21% vs. 23%, p > 0.05), though the dropout group had a significantly higher proportion of participants incarcerated compared with the other two groups (30%, p < 0.05).43
Jansson and colleagues investigated the long-term impact of compulsory residential care among drug-using individuals in Sweden (n = 132).39 This included supervision and care from psychologists, a psychiatrist, nurses, social workers, and treatment attendants. Across 642 observation years after compulsory residential care, 232 observation years (37%) included a criminal justice record, despite the fact that all participants were assigned to treatment.39 Further, in a longitudinal multivariate analysis, use of opiates was significantly associated with subsequent criminal recidivism.
A five-year longitudinal study compared treatment outcomes among American veterans across 15 Veterans Affairs Medical Centers in the United States (n = 2,095) who either had justice system involvement and were voluntarily enrolled in treatment (JSI); were mandated by the justice system to receive treatment (JSI-M); or had no involvement in the justice system and were enrolled in treatment (No-JSI).37 The treatment provided was an abstinence-based, 12-step program.44 Kelly and colleagues compared one- and five-year substance use and criminal recidivism outcomes among participants in each group and adjusted for a range of sociodemographic and dependence-related variables.37 The authors noted that the JSI-M (mandated) group had a significantly lower-risk clinical profile compared with the comparison groups at baseline, which necessitated adjustment via the multivariate analyses. After one year, participants in the JSI-M group had the highest reported level of abstinence from illicit drugs (61.0%), significantly higher than the JSI or No-JSI groups (48.1% vs. 43.8%, respectively).37 However, after five years no significant differences in the proportion of those in remission from drug use were detected across groups (JSI-M=45.4%; JSI=49.8%; No-JSI=46.4%).37 With respect to criminal recidivism, the JSI group reported a significantly higher proportion of individuals rearrested (32.3%) compared with the JSI-M or No-JSI groups (20.6% vs. 18.3%, respectively, p > 0.05). There were no significant differences in the proportion of participants rearrested after five years (JSI-M=23.6%; JSI=32.3%; No-JSI=18.3%). The authors concluded that, while JSI-M participants had a more favourable clinical profile at baseline, they did not have significantly improved therapeutic gains compared with the other groups after five years.37
Fairbairn and colleagues sought to determine whether detainment in a compulsory drug detention was associated with subsequent cessation of injection drug use among a sample of PWID in Bangkok (n = 422).38 Thailand has a large system of compulsory drug detention centers that seeks to promote drug abstinence through punishment, physical labor, and training among individuals charged with drug possession and other minor drug crimes.38 Generally, detainees undergo a 45 day assessment period, followed by four months of detention and two months of vocational training.45 The authors found that 50% of participants reported a period of injection cessation of at least one year (i.e., ‘long term cessation’). In multivariate logistic regression analysis, incarceration and voluntary drug treatment were both associated with long-term cessation, though compulsory drug detention was only associated with short-term cessation (i.e., ceasing injection drug use for less than a year) and subsequent relapse into injecting.38 The authors concluded that strategies to promote long-term cessation are required to address ongoing relapse among Thai PWID.38
One study evaluated mandatory prison-based addiction treatment. Vaughn and colleagues evaluated Taiwan’s compulsory prison-based addiction treatment program.42 This program, implemented in 1997, required individuals arrested for illicit drug use to undergo a one-month detoxification regime upon incarceration. At that point, a medical doctor determined whether offenders were drug dependent; such individuals were then sentenced to 12 months in prison and enrolment in a three-month drug abuse treatment program. The treatment was abstinence-based and included physical labor, psychological counseling, career planning, religious meditation, and civil education (no further details regarding the content of the psychological counseling, career planning, and civil education was provided by study authors). If offenders did not satisfactorily complete the program, they were forced to repeat it until successful completion.42 Once released, individuals were required to pay the cost of treatment. The authors employed a quasi-experimental design wherein individuals who undertook the three-month drug treatment program (n = 109) were compared with individuals who were not enrolled in the program as a result of being incarcerated prior to the program’s implementation (n = 99). Individuals were interviewed during pre-release and after 12 months of release from prison. Multivariate logistic regression analyses were used to identify any significant differences in post-treatment drug use and criminal recidivism. The authors found that offenders enrolled in the mandatory prison-based drug treatment program were significantly more likely to engage in post-release drug use and criminal recidivism. As such, they concluded that Taiwan’s mandatory drug treatment system requires reform.42
Two studies evaluated mandatory outpatient or community-based treatment. Strauss and colleagues sought to determine the short-term impact of a compulsory community-based treatment intervention on substance use among a sample of drug-using female offenders in Portland, Oregon (n = 165).40 Participants were mandated to receive either treatment from ‘ASAP’ (Alcohol and Substance Abuse Prevention Program) or VOA (Volunteers of America). Both programs are community-based treatment interventions that include both mandated and voluntary clients, and are intended to last six months. ASAP is an outpatient program that employs an abstinence-based approach with individual counseling sessions and therapeutic group sessions,40 while VOA provides a residential program focused on the therapeutic community model, with an emphasis on structured activities, individual counseling, and building skills to reduce domestic violence and abuse risk.40 In a retrospective analysis focused on the first week after release from treatment, the authors found that women offenders who were in treatment longer were less likely to use drugs within the first week.40
In 2003, the American state of Kansas implemented SB 123, a state senate bill legislating mandatory community-based treatment of up to 18 months for nonviolent offenders convicted of a first or second offense of drug possession.46 Rengifo and colleagues compared criminal recidivism among individuals convicted of drug possession who were mandated to treatment (n = 1,494) vs. those on regular probation, sent to court services, or sent to prison (n = 4,359), though they do not describe the community-based treatment that individuals received. Data were collected between 2001 and 2005. Findings suggested that there was no significant impact on criminal recidivism among participants mandated to treatment compared to those mandated to regular probation. Of concern, participants mandated to treatment had a significantly increased risk of criminal recidivism compared to participants mandated to court services. The authors concluded that offenders mandated to treatment were not recidivating at a lower rate compared with offenders in alternative programs.46
CONCLUSION
Summary of evidence
While a limited literature exists, the majority of studies (78%) evaluating compulsory treatment failed to detect any significant positive impacts on drug use or criminal recidivism over other approaches, with two studies (22%) detecting negative impacts of compulsory treatment on criminal recidivism compared with control arms. Further, only two studies (22%) observed a significant impact of long-term compulsory inpatient treatment on criminal recidivism: one reported a small effect size on recidivism after two years, and one found a lower risk of drug use within one week of release from compulsory treatment.40 As such, and in light of evidence regarding the potential for human rights violations within compulsory treatment settings, the results of this systematic review do not, on the whole, suggest improved outcomes in reducing drug use and criminal recidivism among drug-dependent individuals enrolled in compulsory treatment approaches, with some studies suggesting potential harms.
These results are of high relevance given the reliance on compulsory drug detention among policymakers in a range of settings. Indeed, compulsory drug treatment approaches have been implemented in southeast Asia,29,45 the Russian Federation,47 North America,46 Latin America,30,47–49 Europe,39 Australia,31 and elsewhere.19 However, experts have noted that little evidence exists to support compulsory treatment modalities, and that the onus is therefore on advocates of such approaches to provide scientific evidence that compulsory treatment is effective, safe, and ethical.32 The results of the present systematic review, which fails to find sufficient evidence that compulsory drug treatment approaches are effective, appears to further confirm these statements.25 Human rights violations reported at compulsory drug detention centers include forced labour, physical and sexual abuse, and being held for up to five years without a clinical determination of drug dependence.25,29,33,45 Governments should therefore seek alternative, evidence-based policies to address drug dependence.
The evidence presented herein also supports the joint statement on drug detention centers released by a range of United Nations-affiliated institutions declaring that, “[t]here is no evidence that these centres represent a favorable or effective environment for the treatment of drug dependence”, and that “United Nations entities call on States to close compulsory drug detention and rehabilitation centres and implement voluntary, evidence-informed and rights-based health and social services in the community.”50 It is noteworthy in this regard that, while compulsory approaches appear ineffective, evidence suggests that a large body of scientific evidence supports the effectiveness of voluntary biomedical approaches such as OST in reducing drug-related harms.4,5 China, Vietnam and Malaysia, for example, all previously scaled up compulsory drug detention centers, but are increasingly moving towards voluntary methadone maintenance and needle and syringe distribution systems to reduce the risk of blood-borne disease transmission from PWID sharing injecting equipment.51–57 Emerging evidence suggests that expanded OST dispensation in these settings has been effective in reducing drug use.54,56–58 This scale up of evidence-based biomedical and harm reduction interventions is occurring despite China’s previous investment in a compulsory treatment infrastructure; as such, tensions remain between voluntary, public health-oriented approaches and compulsory detainment,59 as they do in settings that include both compulsory and voluntary approaches, such as Mexico.60,61 This may result in suboptimal treatment outcomes given that ongoing interactions with law enforcement and the threat of detainment within compulsory drug detention centers may cause drug-dependent individuals to avoid harm reduction services or engage in risky drug-using behaviors out of a fear of being targeted by police,59 as has been observed in a range of settings.62–66 We also note that this is likely the case in settings seeking to control the harms of non-opioid substance use disorders such as cocaine use disorder, given that available interventions that have been shown to be effective have been undertaken using voluntary treatment approaches.11,12,16 Governments seeking to implement or bring to scale harm reduction interventions that include OST and needle and syringe distribution will therefore likely be required to reduce their reliance on compulsory and law enforcement-based approaches in order to ensure treatment effectiveness.
Limitations
This systematic review has limitations. Primarily, risk of publication bias is present given political support for law enforcement-oriented strategies to controlling drug-related harms, particularly in Southeast Asia, where compulsory drug detention centers have been implemented by many national governments.29,45 In certain settings, such as Thailand, the scale up of drug detention centers has been accompanied by high-profile ‘war on drugs’ campaigns promoting enforcement- and military-based responses to drug harms.38 Within such political climates, undertaking or publishing peer-reviewed research critical of compulsory drug treatment may be disincentivized. Further, while drug detention centers are more numerous in southeast Asia, this region has a limited infrastructure for scientific research on drug use, which may also increase the risk of publication bias.
Conclusions
Based on the available peer-reviewed scientific literature, there is little evidence that compulsory drug treatment is effective in promoting abstention from drug use or in reducing criminal recidivism. It is noteworthy that this systematic review includes evaluations of not only drug detention centers, but of a range of compulsory inpatient and outpatient treatment approaches. Additionally, the reductions in drug use and criminal recidivism as a result of compulsory drug treatment interventions were generally short-term or of low clinical significance. In light of the lack of evidence suggesting that compulsory drug treatment is effective, policymakers should seek to implement evidence-based, voluntary treatment modalities in order to reduce the harms of drug use.
| Author/ Year |
Location | n | Study period |
Study design |
Participant characteristics |
Intervention | Changes in substance use |
Changes in recidivism |
Summary of outcomes |
Quality score |
|||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean age (range) | Female | Ethnicity | Drug use | ||||||||||
| Sun 2001 |
China | 615 | NR | Cross- sectional |
NR | NR | NR | NR | Mandatory detoxification vs. volunteer detoxification vs. Detoxification and compulsory drug detention |
98% relapsed within one year |
NR | Almost all participants relapsed within a year. No significant difference between participants enrolled in different interventions |
8 |
| Huang 2011 |
Chongqing, China |
177 | 2009 | Longitudinal observational |
16% 18–25; 43.4% 26–35; 31.4% 36– 45; 9.1% 46+ |
21.6% | Asian (Chinese) |
87.5% alcohol; 69.4% heroin; 62.8% meth; 40.7% Manguo |
Mandatory inpatient treatment |
10.3% relapsed in less than a month; 35.5% 1–6 months; 10.3% 7–12 months; 43.9% >13 months |
N/A | 65% placed in mandatory treatment by police in past 12 months; 46% used drugs within 6 months of their release and 10% relapsed in 7–12 months |
8 |
| Rengifo 2010 |
Kansas | 1,494; 4,359 in control group |
2001– 2005 |
Prospective case control |
SB 123 group: 14–25 = 38.9% 26–35 = 28.2% >35 = 32.9% Control groups: >35 = 33.0–45.0% |
SB 123: 29% Control groups: 19.3%– 26.5% |
SB 123 group: 81.6% white Control groups: 75.5– 78.2% white |
NR | 18 months of mandatory community based drug treatment |
NA | No difference in recidivism |
No significant impact on recidivism compared to community corrections; increase compared to court services |
15 |
| Fairbairn 2014 |
Bangkok, Thailand |
422 | N/A | Cross- sectional observational |
38 (34–48) | 18% | 100% Thai |
Heroin, methamph etamine, midazolam; proportions not reported |
Compulsory drug detention vs. voluntary addiction treatment vs. MMT |
Voluntary addiction treatment associated with sustained cessation; compulsory drug detention associated with short-term cessation |
N/A | Compulsory drug detention not associated with long-term cessation |
16 |
| Jansson 2009 |
Sweden | 132 | Treated between 1997– 2000; 5 year follow up |
Longitudinal observational |
Youth: 18.7 (16–20), Adults: 26.7 (18–43) |
100% | NR | NR | Compulsory residential care |
NA | Of 642 observation years, 232 (37%) contained a criminal justice record. |
Recidivism was associated with use of opiates |
12 |
| Hiller 2006 |
Dallas, TX | 506 | 1997– 1999 |
Longitudinal observational |
32.2 (SD: 9.2) | 30% | 10% Hispanic |
NR | Mandated residential 6- month treatment |
N/A | No significant differences in 1-year arrest rates. Significantly fewer graduates arrested in 2nd year than dropouts. |
Treatment graduates slightly less likely to be arrested within 2 years of leaving the program |
13 |
| Kelly 2005 |
US | 2,095 | 5 year follow up (dates not reported) |
Prospective case control |
JSI-M = 42 (9.4) JSI = 40.7 (8.0) None = 42.9 (9.2) (p<0.01) |
None | 49% African American; 45% White; 6% other |
JSI-M: 44.7%; JSI: 58.3%; None: 57.5% (p=0.01) |
21- or 28-day SUD residential treatment programs from Veterans Affairs |
1-year remission: JSI-M 61.0%; JSI 48.1%; None 43.8%; (p<0.01) 5-year remission: JSI-M 45.4%; JSI 49.8%; None 46.4%; (p=0.32) |
1-year rearrest: JSI-M 20.6%; JSI 32.3%; Other 18.3%; (p<0.05) 5-year rearrested: JSI-M 23.6%; JSI 27.7%; None 19.0%; (p=0.24) |
Mandated patients had less severe clinical profile at treatment intake; no differences in therapeutic gains during treatment. |
15 |
| Vaughn 2002 |
Taiwan | 700 | 1999– 2000 |
Quasi- experimental |
NR | 25% of 700 pre- release intervie ws |
Asian | NR | Compulsory prison based treatment for drug using offenders |
Treatment sample: 44% amphetamine, 26.6% heroin; Non-treatment sample: 9.1% amphetamine, 7.1% heroin |
33% of treatment sample reincarcerat ed, 5% of non- treatment reincarcerat ed |
Treatment group had worse outcomes than non-treatment group |
11 |
| Strauss 2001 |
Oregon | 165 | 1995– 1999 |
Prospective case control |
ASAP: 30.9 VOA: 34.0 |
100% | African American: ASAP = 25–29.7% VOA = 13.8– 20.5% |
NR | Community based treatment programs |
45 used drugs in first week after treatment (27%), 120 did not |
NA | Those not using drugs in first week after mandated treatment more likely to have been in treatment longer and had individual and group support |
11 |
Note: NA = Not applicable; NR = Not reported; SD = Standard deviation; Meth = Methamphetamine MMT = Methadone maintenance therapy; SB 123 = Kansas’ mandatory drug treatment policy; QCT = Quasi-compulsory treatment; JSI = Justice system involved individuals; JSI-M = Justice system involved and mandated individuals; SUD = Substance use disorder; ASAP = ASAP treatment services, Inc; VOA = Volunteers of America residential program;
Acknowledgments
DW had full access to all the data in the study and had final responsibility for the decision to submit for publication. MM and CR conducted the systematic search, with assistance from DW. DW drafted the manuscript. EW provided guidance on the systematic review and meta-analysis methodology. BF, AK, SS, and EW revised the manuscript substantially. All authors have seen and approved the final version.
Funding: Dan Werb is supported by a US National Institute on Drug Abuse Avenir Award (DP2 DA040256-01) and the Canadian Institutes of Health Research (MOP 79297). Further support was provided by the Open Society Foundations through an operating grant for the International Centre for Science in Drug Policy. Benedikt Fischer acknowledges funding support from a CIHR/PHAC Applied Public Health Chair. Steffanie Strathdee acknowledges funding support from the National Institutes of Health (R37 DA019829). Meredith Meacham acknowledges funding support from the National Institutes of Health (T32 DA023356). Claudia Rafful acknowledges funding from the Fogarty International Center (D43 TW008633) and CONACyT (209407/313533). This research was undertaken, in part, thanks to funding for a Tier 1 Canada Research Chair in Inner City Medicine, which supports Evan Wood. The funders had no role in the decision to initiate the study; the design and conduct of the study; the collection, management, analysis, and interpretation of the data; and the preparation, review, or approval of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest: All authors declare that they have no conflicts of interest.
References
- 1.UNODC. World Drug Report 2015. Vienna: United Nations Office on Drugs and Crime; 2015. [Google Scholar]
- 2.Degenhardt L, Whiteford HA, Ferrari AJ, et al. Global burden of disease attributable to illicit drug use and dependence: findings from the Global Burden of Disease Study 2010. The Lancet. 2013;382(9904):1564–1574. doi: 10.1016/S0140-6736(13)61530-5. [DOI] [PubMed] [Google Scholar]
- 3.Jurgens R. Effectiveness of interventions to address HIV in prisons. Geneva: World Health Organization (WHO), United Nations Office on Drugs and Crime (UNODC), and Joint United Nations Programme on HIV/AIDS (UNAIDS; 2007. [Google Scholar]
- 4.Mattick RP, Breen C, Kimber J, Davoli M. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database Syst Rev. 2009;(2):CD002209. doi: 10.1002/14651858.CD002209. [DOI] [PubMed] [Google Scholar]
- 5.Amato L, Davoli M, Ferri M, Ali R. Methadone at tapered doses for the management of opioid withdrawal. Cochrane Database Syst Rev. 2002;(1):CD003409. doi: 10.1002/14651858.CD003409. [DOI] [PubMed] [Google Scholar]
- 6.Gowing L, Ali R, White J. Buprenorphine for the management of opioid withdrawal. Cochrane database of systematic reviews (Online) 2004;(4) doi: 10.1002/14651858.CD002025.pub2. [DOI] [PubMed] [Google Scholar]
- 7.As S, Young J, Vieira K. Long-term suboxone treatment and its benefit on long-term remission for opiate dependence. J Psychiatry. 2014;17(1000174):2. [Google Scholar]
- 8.Krupitsky E, Nunes EV, Ling W, Illeperuma A, Gastfriend DR, Silverman BL. Injectable extended-release naltrexone for opioid dependence: A double-blind, placebo-controlled, multicentre randomised trial. Lancet. 2011;377(9776):1506–1513. doi: 10.1016/S0140-6736(11)60358-9. [DOI] [PubMed] [Google Scholar]
- 9.Wolfe D, Carrieri MP, Dasgupta N, Wodak A, Newman R, Bruce RD. Concerns about injectable naltrexone for opioid dependence. Lancet. 2011;377(9776):1468–1470. doi: 10.1016/S0140-6736(10)62056-9. [DOI] [PubMed] [Google Scholar]
- 10.Ferri M, Davoli M, Perucci CA. Pharmaceutical heroin for heroin maintenance in chronic heroin dependents. Cochrane Database of Systematic Reviews. 2011;(12) doi: 10.1002/14651858.CD003410.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Castells X, Casas M, Perez-Maña C, Roncero C, Vidal X, Capellà D. Efficacy of psychostimulant drugs for cocaine dependence. Cochrane Database Syst Rev. 2010;2 doi: 10.1002/14651858.CD007380.pub3. [DOI] [PubMed] [Google Scholar]
- 12.Fischer B, Blanken P, Da Silveira D, et al. Effectiveness of secondary prevention and treatment interventions for crack-cocaine abuse: A comprehensive narrative overview of English-language studies. Int J Drug Pol. 2015 doi: 10.1016/j.drugpo.2015.01.002. [DOI] [PubMed] [Google Scholar]
- 13.Shearer J, Wodak A, Van Beek I, Mattick RP, Lewis J. Pilot randomized double blind placebo- controlled study of dexamphetamine for cocaine dependence. Addiction. 2003;98(8):1137–1141. doi: 10.1046/j.1360-0443.2003.00447.x. [DOI] [PubMed] [Google Scholar]
- 14.Mooney ME, Herin DV, Schmitz JM, Moukaddam N, Green CE, Grabowski J. Effects of oral methamphetamine on cocaine use: a randomized, double-blind, placebo-controlled trial. Drug Alc Depend. 2009;101(1):34–41. doi: 10.1016/j.drugalcdep.2008.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grabowski J, Rhoades H, Schmitz J, et al. Dextroamphetamine for cocaine-dependence treatment: a double-blind randomized clinical trial. J Clin Psychopharmacol. 2001;21(5):522–526. doi: 10.1097/00004714-200110000-00010. [DOI] [PubMed] [Google Scholar]
- 16.Hofmann SG, Asnaani A, Vonk IJ, Sawyer AT, Fang A. The efficacy of cognitive behavioral therapy: A review of meta-analyses. Cognitive Therapy and Research. 2012;36(5):427–440. doi: 10.1007/s10608-012-9476-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dutra L, Stathopoulou G, Basden SL, Leyro TM, Powers MB, Otto MW. A meta-analytic review of psychosocial interventions for substance use disorders. Am J Psychiatry. 2008;165(2):179–187. doi: 10.1176/appi.ajp.2007.06111851. [DOI] [PubMed] [Google Scholar]
- 18.Prendergast M, Podus D, Finney J, Greenwell L, Roll J. Contingency management for treatment of substance use disorders: A meta- analysis. Addiction. 2006;101(11):1546–1560. doi: 10.1111/j.1360-0443.2006.01581.x. [DOI] [PubMed] [Google Scholar]
- 19.Israelsson M, Gerdner A. Compulsory commitment to care of substance misusers: International trends during 25 Years. Eur Addict Res. 2011;18(6):302–321. doi: 10.1159/000341716. [DOI] [PubMed] [Google Scholar]
- 20.Wild TC. Compulsory substance-user treatment and harm reduction: A critical analysis. Substance use & misuse. 1999;34(1):83–102. doi: 10.3109/10826089909035637. [DOI] [PubMed] [Google Scholar]
- 21.Hiller ML, Knight K, Broome KM, Simpson DD. Compulsory community-based substance abuse treatment and the mentally ill criminal offender. The Prison Journal. 1996;76(2):180–191. [Google Scholar]
- 22.WHO Regional Office for the Western Pacific. Assessment of compulsory treatment of people who use drugs in Cambodia, China, Malaysia and Viet Nam: Application of selected human rights principles. Geneva: World Health Organization; 2009. [Google Scholar]
- 23.Bright DA, Martire KA. Does coerced treatment of substance- using offenders lead to improvements in substance use and recidivism? A review of the treatment efficacy literature. Australian Psychologist. 2012 [Google Scholar]
- 24.Werb D, Elliott R, Fischer B, Wood E, Montaner J, Kerr T. Drug treatment courts in Canada: An evidence-based review. HIV/AIDS Policy & Law Review. 2007;126(2/3) [PubMed] [Google Scholar]
- 25.Hall W, Babor T, Edwards G, et al. Compulsory detention, forced detoxification and enforced labour are not ethically acceptable or effective ways to treat addiction. Addiction. 2012;107(11):1891–1893. doi: 10.1111/j.1360-0443.2012.03888.x. [DOI] [PubMed] [Google Scholar]
- 26.Jurgens R, Csete J. In the name of treatment: ending abuses in compulsory drug detention centers. Addiction. 2012;107(4):689–691. doi: 10.1111/j.1360-0443.2011.03738.x. [DOI] [PubMed] [Google Scholar]
- 27.Wild TC, Roberts AB, Cooper EL. Compulsory substance abuse treatment: An overview of recent findings and issues. European Addiction Research. 2002;8(2):84–93. doi: 10.1159/000052059. [DOI] [PubMed] [Google Scholar]
- 28.Stevens A, Berto D, Heckmann W, et al. Quasi-compulsory treatment of drug dependent offenders: An international literature review. Substance use & misuse. 2005;40(3):269–283. doi: 10.1081/ja-200049159. [DOI] [PubMed] [Google Scholar]
- 29.Amon JJ, Pearshouse R, Cohen J, Schleifer R. Compulsory drug detention centers in China, Cambodia, Vietnam, and Laos: Health and human rights abuses. Health and Human Rights. 2013;15(2) [PubMed] [Google Scholar]
- 30.Malta M, Beyrer C. The HIV epidemic and human rights violations in Brazil. J Int AIDS Soc. 2013;16(1) doi: 10.7448/IAS.16.1.18817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Birgden A, Grant L. Establishing a compulsory drug treatment prison: Therapeutic policy, principles, and practices in addressing offender rights and rehabilitation. International Journal of Law and Psychiatry. 2010;33(5):341–349. doi: 10.1016/j.ijlp.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 32.Hall W, Carter A. Advocates need to show compulsory treatment of opioid dependence is effective, safe and ethical. Bulletin of the World Health Organization. 2013;91(2):146. doi: 10.2471/BLT.12.115196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pearshouse R. " Patients, not criminals"? An assessment of Thailand's compulsory drug dependence treatment system. HIV/AIDS policy & law review/Canadian HIV/AIDS Legal Network. 2009;14(1):11. [PubMed] [Google Scholar]
- 34.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. Journal of Epidemiology and Community Health. 1998;52(6):377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sun B, Ye Y, Qin L. An analysis of relapse factors of 615 heroin addicts. Chin J Drug Depend. 2001;10(3):214–216. [Google Scholar]
- 37.Kelly J, Finney J, Moos R. Substance use disorder patients who are mandated to treatment: Characteristics, treatment process, and 1-and 5-year outcomes. J Subst Abuse Treat. 2005;28(3):213–223. doi: 10.1016/j.jsat.2004.10.014. [DOI] [PubMed] [Google Scholar]
- 38.Fairbairn N, Hayashi K, Ti L, et al. Compulsory drug detention and injection drug use cessation and relapse in Bangkok, Thailand. Drug and Alcohol Review. 2014 doi: 10.1111/dar.12206. [DOI] [PubMed] [Google Scholar]
- 39.Jansson I, Hesse M, Fridell M. Influence of personality disorder features on social functioning in substance-abusing women five years after compulsive residential treatment. European addiction research. 2008;15(1):25–31. doi: 10.1159/000173006. [DOI] [PubMed] [Google Scholar]
- 40.Strauss S, Falkin G. The first week after drug treatment: The influence of treatment on drug use among women offenders. Am J Drug Alc Abuse. 2001;27(2):241–264. doi: 10.1081/ada-100103708. [DOI] [PubMed] [Google Scholar]
- 41.Huang K, Zhang L, Liu J. Drug problems in contemporary China: a profile of Chinese drug users in a metropolitan area. Int J Drug Pol. 2011;22(2):128–132. doi: 10.1016/j.drugpo.2010.09.010. [DOI] [PubMed] [Google Scholar]
- 42.Vaughn M, Deng F, Lee L-J. Evaluating a prison-based drug treatment program in Taiwan. J Drug Issues. 2003;33(2):357–383. [Google Scholar]
- 43.Hiller M, Knight K, Simpson D. Recidivism following mandated residential substance abuse treatment for felony probationers. The Prison Journal. 2006;86(2):230–241. [Google Scholar]
- 44.Ouimette PC, Finney JW, Moos RH. Twelve-step and cognitive-behavioral treatment for substance abuse a comparison of treatment Effectiveness. Journal of Consulting and Clinical Psychology. 1997;65(2):230–240. doi: 10.1037//0022-006x.65.2.230. [DOI] [PubMed] [Google Scholar]
- 45.Pearshouse R. Compulsory drug treatment in Thailand: Observations on the Narcotic Addict Rehabilitation Act BE 2545 (2002) Canadian HIV/AIDS Legal Network Toronto; 2009. [Google Scholar]
- 46.Rengifo AF, Stemen D. The impact of drug treatment on recidivism: Do mandatory programs make a difference? Evidence from Kansas's Senate Bill. Crime & Delinquency. 2010;123 [Google Scholar]
- 47.Utyasheva L. Russian Federation: Inhumane conditions in drug treatment facilities lead to tragedy. HIV/AIDS Policy & Law Review. 2007;12(1):32–33. [PubMed] [Google Scholar]
- 48.Mendelevich VD. Bioethical differences between drug addiction treatment professionals inside and outside the Russian Federation. Harm Reduct J. 2011;8(1):15. doi: 10.1186/1477-7517-8-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Vecinos del centro de rehabilitación 'Fe y Vida' cuentan lo que escucharon. CNN Mexico. 2010 Jun 13; [Google Scholar]
- 50.Joint statement on compulsory drug detention and rehabilitation centres ILO, OHCHR, UNDP, UNESCO, UNFPA, UNHCR, UNICEF, UNODC, UN Women, WFP, WHO and UNAIDS. Geneva: Unitd Nations Office of the High Commissioner for Human Rights; 2012. [Google Scholar]
- 51.Qian H-Z, Hao C, Ruan Y, et al. Impact of methadone on drug use and risky sex in China. J Subst Abuse Treat. 2008;34(4):391–397. doi: 10.1016/j.jsat.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 52.Sullivan SG, Wu Z. Rapid scale up of harm reduction in China. Int J Drug Pol. 2007;18(2):118–128. doi: 10.1016/j.drugpo.2006.11.014. [DOI] [PubMed] [Google Scholar]
- 53.Wu Z, Sullivan SG, Wang Y, Rotheram-Borus MJ, Detels R. Evolution of China's response to HIV/AIDS. Lancet. 2007;369(9562):679–690. doi: 10.1016/S0140-6736(07)60315-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Baharom N, Hassan MR, Ali N, Shah SA. Improvement of quality of life following 6 months of methadone maintenance therapy in Malaysia. Subst Abuse Treat Prev Policy. 2012;7(1):32. doi: 10.1186/1747-597X-7-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Reid G, Kamarulzaman A, Sran SK. Malaysia and harm reduction: The challenges and responses. Int J Drug Pol. 2007;18(2):136–140. doi: 10.1016/j.drugpo.2006.12.015. [DOI] [PubMed] [Google Scholar]
- 56.Hammett TM, Wu Z, Duc TT, et al. ‘Social evils’ and harm reduction: the evolving policy environment for human immunodeficiency virus prevention among injection drug users in China and Vietnam. Addiction. 2008;103(1):137–145. doi: 10.1111/j.1360-0443.2007.02053.x. [DOI] [PubMed] [Google Scholar]
- 57.Nguyen T, Nguyen LT, Pham MD, Vu HH, Mulvey KP. Methadone maintenance therapy in Vietnam: an overview and scaling-up plan. Advances in preventive medicine. 2012;2012 doi: 10.1155/2012/732484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yin W, Hao Y, Sun X, et al. Scaling up the national methadone maintenance treatment program in China: Achievements and challenges. International journal of epidemiology. 2010;39(suppl 2):i29–ii37. doi: 10.1093/ije/dyq210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Larney S, Dolan K. Compulsory detoxification is a major challenge to harm reduction in China. Int J Drug Pol. 2010;21(3):165–166. doi: 10.1016/j.drugpo.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 60.Garcia A. Serenity: violence, inequality, and recovery on the edge of Mexico City. Med Anthropology Q. 2015 doi: 10.1111/maq.12208. [DOI] [PubMed] [Google Scholar]
- 61.Lozano-Verduzco I, Marín-Navarrete R, Romero-Mendoza M, Tena-Suck A. Experiences of power and violence in Mexican men attending mutual-aid residential centers for addiction treatment. Am J Men's Health. 2015 doi: 10.1177/1557988314565812. 1557988314565812. [DOI] [PubMed] [Google Scholar]
- 62.Bluthenthal RN, Kral AH, Lorvick J, Watters JK. Impact of law enforcement on syringe exchange programs: A look at Oakland and San Francisco. Med Anthropol. 1997;18(1):61. doi: 10.1080/01459740.1997.9966150. [DOI] [PubMed] [Google Scholar]
- 63.Cooper H, Moore L, Gruskin S, Krieger N. The impact of a police drug crackdown on drug injectors' ability to practice harm reduction: A qualitative study. Social Science & Medicine. 2005;61(3):673–684. doi: 10.1016/j.socscimed.2004.12.030. [DOI] [PubMed] [Google Scholar]
- 64.Beletsky L, Lozada R, Gaines T, et al. Syringe confiscation as an HIV risk factor: The public health implications of arbitrary policing in Tijuana and Ciudad Juarez, Mexico. Journal of Urban Health. 2013:1–15. doi: 10.1007/s11524-012-9741-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Beletsky L, Heller D, Jenness SM, Neaigus A, Gelpi-Acosta C, Hagan H. Syringe access, syringe sharing, and police encounters among people who inject drugs in New York City: A community-level perspective. Int J Drug Pol. 2014;25(1):105–111. doi: 10.1016/j.drugpo.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Werb D, Wood E, Small W, et al. Effects of police confiscation of illicit drugs and syringes among injection drug users in Vancouver. Int J Drug Pol. 2008;19(4):332. doi: 10.1016/j.drugpo.2007.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]